Abstract
Preclinical research suggests that N-methyl-D-aspartate glutamate receptors (NMDA-Rs) have a crucial role in working memory (WM). In this study, we investigated the role of NMDA-Rs in the brain activation and connectivity that subserve WM. Because of its importance in WM, the lateral prefrontal cortex, particularly the dorsolateral prefrontal cortex and its connections, were the focus of analyses. Healthy participants (n=22) participated in a single functional magnetic resonance imaging session. They received saline and then the NMDA-R antagonist ketamine while performing a spatial WM task. Time-course analysis was used to compare lateral prefrontal activation during saline and ketamine administration. Seed-based functional connectivity analysis was used to compare dorsolateral prefrontal connectivity during the two conditions and global-based connectivity was used to test for laterality in these effects. Ketamine reduced accuracy on the spatial WM task and brain activation during the encoding and early maintenance (EEM) period of task trials. Decrements in task-related activation during EEM were related to performance deficits. Ketamine reduced connectivity in the DPFC network bilaterally, and region-specific reductions in connectivity were related to performance. These results support the hypothesis that NMDA-Rs are critical for WM. The knowledge gained may be helpful in understanding disorders that might involve glutamatergic deficits such as schizophrenia and developing better treatments.
Keywords: NMDA, working memory, connectivity, schizophrenia, prefrontal cortex, ketamine
INTRODUCTION
There is substantial interest in understanding the neural basis of working memory (WM), a cognitive resource used for temporary memory storage and guidance of ongoing behavior (Baddeley, 1992). WM deficits are associated with schizophrenia and other neuropsychiatric disorders. Thus, the study of WM in humans has important implications for both basic and clinical neuroscience. Prior studies in non-human primates implicated regions of lateral prefrontal cortex (LPFC) in the component processes that comprise WM (Fuster and Alexander, 1971; Goldman-Rakic, 1995; Wang et al, 2011). This research has concentrated on the WM phases of encoding, maintaining, and using information to guide response and linked them to distinct neuronal populations. Research in humans has confirmed the importance of LPFC in WM and focused attention on WM subprocesses and the network of brain areas that subserve them (Courtney et al, 1998, 1997; D'Esposito et al, 1998; Leung et al, 2002).
Preclinical research studies indicate that N-methyl-D-aspartate glutamate receptors (NMDA-Rs) are critically involved in WM. For example, NMDA-Rs contribute to the recurrent cortical excitation that is thought to model the maintenance of information in WM (Fellous and Sejnowski, 2003; Lisman et al, 1998; Seamans et al, 2003). In awake, behaving rodents, NMDA-R antagonists attenuate PFC neural activity associated with WM maintenance (Homayoun et al, 2004; Jackson et al, 2004). Also, NMDA-R antagonists impair WM performance in both non-human primates (Baron and Wenger, 2001; Frederick et al, 1995; Roberts et al, 2010) and humans (Ghoneim et al, 1985; Krystal et al, 1994; Oye et al, 1992). The authors of a prior functional magnetic resonance imaging (fMRI) study in humans suggested that NMDA-R antagonists alter the brain activation related to the manipulation of information in WM (Honey et al, 2004). However, this has been the only link between WM deficits produced by NMDA-R antagonists in humans and non-human primates and a direct or surrogate measure of brain activity.
In this investigation, we aimed to further establish this link and to characterize the role of NMDA-Rs in LPFC networks in encoding, maintenance, and response. In this way, we hoped to increase our knowledge about the role of NMDA-Rs in WM as well as lay the groundwork for integrated translational research on WM. To achieve this objective, we tested the effects of the uncompetitive NMDA-R antagonist, ketamine, at a dose previously demonstrated to impair WM function and induce transient schizophrenia-like symptoms in humans (Krystal et al, 1994).
To allow detailed examination of prefrontal function under ketamine blockade, we used an event-related fMRI design that incorporated a memory load manipulation and analyzed its time course of activation to help differentiate the initial encoding and early maintenance (EEM), later maintenance (LM), and response phases of WM (Driesen et al, 2008; Leung et al, 2002, 2004). Preclinical research suggests that these stages may, at least partially, be subserved by distinct neuronal populations and neurotransmitters. NMDA and D1 dopamine receptors establish and maintain sustained activity in the prefrontal circuit (Castner and Williams, 2007; Homayoun et al, 2004; Lisman et al, 1998), whereas D2 dopamine receptors are critical for response (Seamans and Yang, 2004; Wang et al, 2004). In addition, initial evidence suggests that AMPA and NMDA currents are involved in encoding (Wang et al, 2013). The paradigm used in this study was developed by Goldman-Rakic and colleagues to assist in separating these stages and thus promote translational WM research. A control task is included that serves as a sensory processing comparator for memory-related features of the WM task (Leung et al, 2002). To reduce the number of statistical comparisons, we restricted our time-course analysis to previously defined anatomical regions of interests (ROIs) in LPFC. We also included an anatomically defined ROI for Heschl's gyrus, a primary auditory region that is activated by scanner noise but not by the visual WM task. This helped us to differentiate broad systemic effects, such as changes in neurovascular coupling, from changes caused by ketamine's effect upon task-related activation.
We extended our study of NMDA-antagonist effects on PFC to the wider cortical network that subserves WM through seed voxel connectivity analysis (Biswal et al, 1995; Hampson et al, 2002; Raichle et al, 2001) and tested for lateralization of these effects with global-based connectivity or GBC (Cole et al, 2012; Cole et al, 2011; Cole et al, 2010). In doing so, we examined whether NMDA-R antagonists disrupt connectivity between a key WM node, namely dlPFC, and the WM network. The seed used in the present analyses was defined in previous studies of the ‘control network,' a brain network encompassing dlPFC and other areas typically involved in WM (Dosenbach et al, 2007; Dosenbach et al, 2006). We hypothesized that ketamine would impair WM performance and reduce WM-related brain activation. In addition, reasoning that an impaired PFC would have difficulty initiating or sustaining network activity, we predicted that ketamine would reduce connectivity in the dlPFC network. We further hypothesized that reductions in connectivity and activation would have implications for WM performance.
MATERIALS AND METHODS
Participants
Our sample was composed of 22 right-handed, healthy volunteers (14 male) between 21 and 44 years old. All subjects denied a history of neurological disorder, substance abuse or dependence, or other psychiatric illness, and did not have a first-degree relative with substance abuse or psychiatric history. Screening procedures are described in Supplementary Information. The protocol was approved by the Yale and Western Institutional Review Boards, and all subjects provided written informed consent.
Spatial WM Task
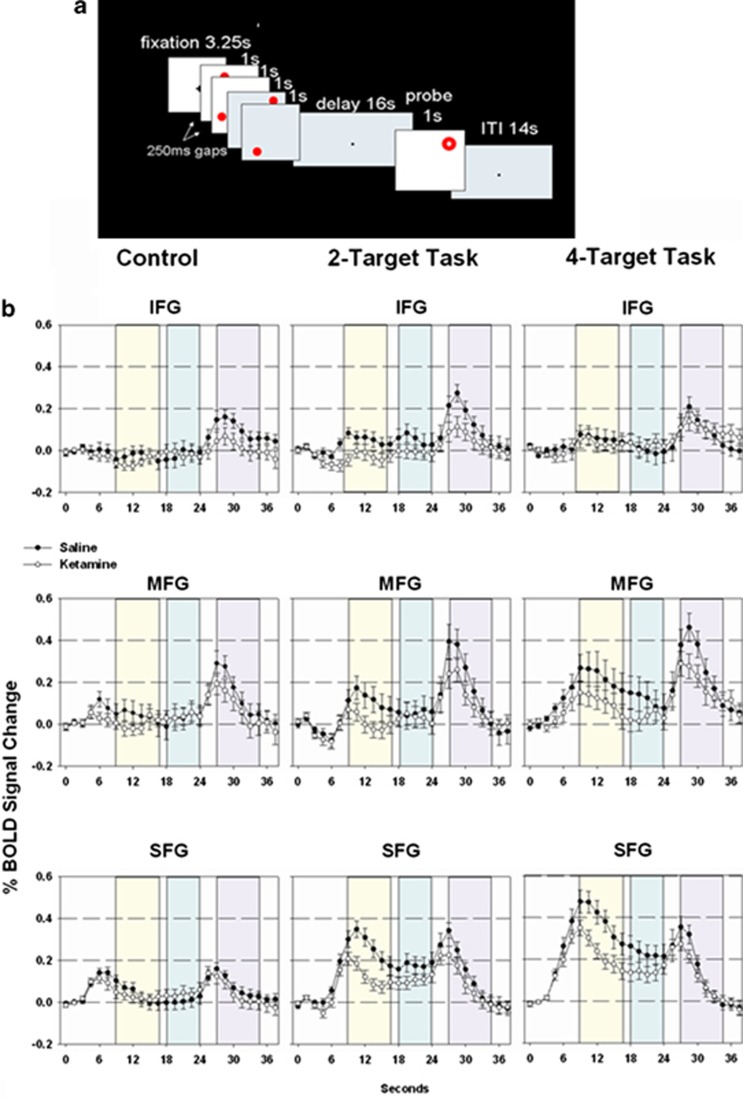
The spatial WM task (Figure 1a) was similar to that previously reported by Driesen et al (2008). There were two memory load conditions. For the high-memory-load (4-target) condition, participants fixated on a dot at the center of the visual field for 3250 ms. Stimuli consisted of four red solid circles at different eccentricities relative to fixation that were presented sequentially. Each circle was presented for 1 s with a 250-ms interstimulus interval. After a 16-s retention interval, a probe (ring) appeared on the screen for 1 s. The subject pressed a button to indicate whether the probe location matched the spatial location of one of the previously presented circles. After subjects responded to the probe, the fixation dot changed to a cross. The subsequent change from a cross to a dot signaled the onset of the next trial. The inter-trial interval was 14 s. The low-memory-load (2-target) condition was the same as the four-item except only two circles were presented. An additional 2500 ms were added to the inter-trial interval to equalize the total length of the 4-target and 2-target trials. The control (no WM) task closely resembled the 4-target task except that the color of the circles was gray and the subject had been instructed to simply attend to the stimuli without attempting to remember. Two high load, two low load, and two control trials alternated in each run in a fixed order. Accuracy (percent correct) and reaction time (RT) were recorded.
Figure 1.
(a) Spatial working memory (WM) task, 4-target version. (b) Regions of interests (ROIs) used for time-course analysis, SFG (blue), MFG (magenta), and IFG (green). Ketamine reduced task-related activation during the encoding and early maintenance (EEM) phase, [F(1,686)=9.48, p=0.0022. EEM (yellow), later maintence (LM) (green), and response (purple) analysis periods indicated by vertical bars. BOLD, blood oxygen level dependent; IFG, inferior frontal gyrus; MFG, middle frontal gyrus; SFG, superior frontal gyrus.
Procedures
Participants who passed screening were scheduled for an experimental session. If possible, female subjects were scheduled so that they were in the follicular phase of their cycle. On the morning of the scan, participants were assessed with the Positive and Negative Syndrome Scale (PANSS; Kay et al, 1986) and received training on the spatial WM task. Two intravenous catheters were placed: one for infusing saline and later ketamine, and another for drawing blood samples. Participants were placed in a 3-Tesla Trio scanner. Each subject's pulse, respiration, oxygen saturation and heart rate were monitored throughout the scanning session.
After acquisition of structural images, functional imaging commenced with a visual fixation scan during which participants looked at a projected cross back-projected onto a mirror. Scan parameters are in Supplementary Information. Seventy-five seconds into the scan, participants received a saline bolus. They then received a constant saline infusion and completed eight scans of the spatial WM task. The task consisted of 4-target, 2-target, and control trials. In the control trials, subjects viewed four targets but were instructed not to memorize their locations. Accuracy (percent correct) and RT were recorded and analyzed in separate repeated-measure MANOVAs.
Following these saline infusion scans, the visual fixation scan and eight spatial WM scans were repeated with ketamine infusion. The initial ketamine bolus was 0.23 mg/kg over 1 min, and the subsequent constant infusion was 0.58 mg/kg/h over the remainder of the scanning session. The volume of the saline bolus and infusion were comparable to that of the ketamine bolus and infusion. Blood samples were taken approximately 5, 25, and 45 min after the start of each bolus and were later analyzed with a previously published method (Krystal et al, 1998). Connectivity alterations during the bolus run were analyzed and will be reported elsewhere.
The entire scanning session lasted approximately 2–2.5 h. Afterward, participants were removed from the scanner and reassessed with the PANSS. Ratings considered their entire ketamine experience and were converted to factor scores for positive, negative, and cognitive symptoms (Bell et al, 1994). ‘Positive' refers to psychotic-like symptoms, ‘negative' to social withdrawal and blunted affect, and ‘cognitive' to thought disorder and poor concentration. Symptom factor scores under saline and ketamine were compared in separate paired t-tests.
Image Analysis
Time-course analysis
Preprocessing and image analysis software are described in Supplementary Information. To calculate time courses, we created spatial ROIs based on our previous experience with the task (Driesen et al, 2008; Leung et al, 2002, 2004). These ROIs had a 10-mm radius and measured activity within the middle frontal gyrus (MFG), inferior frontal gyrus (IFG), and superior frontal gyrus (SFG) in the area of the superior frontal sulcus (see Table 1). The average time course for each ROI and trial type was extracted from the preprocessed data for each scan. Each time point was expressed as a percent signal change from the pre-stimulus baseline, which consisted of three images collected at the beginning of the fixation period. At this stage of the analysis, information about percent signal change at each time point—ie, for each repetition time (TR), ROI, and trial type—were maintained. Based on our earlier work (Driesen et al, 2008), the percent signal change was averaged across sequential time points to represent different WM phases, specifically, EEM (8.75–17.75 s), LM (18–24 s), and response phases (27–34.5 s) as shown in Figure 1b.
Table 1. ROIs Used in Time-course Analyses.
| ROIs |
MNI co-ordinates |
||
|---|---|---|---|
| x | y | z | |
| Inferior frontal gyrus, R | 43 | 38 | −2 |
| Inferior frontal gyrus, L | −43 | 38 | −2 |
| Middle frontal gyrus, R | 48 | 30 | 24 |
| Middle frontal gyrus, L | −42 | 30 | 24 |
| Superior frontal gyrus, R | 24 | 0 | 51 |
| Superior frontal gyrus, L | −24 | −3 | 57 |
These average percent signal change scores were analyzed using mixed models (Brown and Prescott, 1999; Gueorguieva and Krystal, 2004), a statistical technique that allows inter-correlated dependent variables. We fitted a model with four within-subject independent variables: drug (saline, ketamine), task phase (EEM, LM, response), LPFC ROI (IFG, MFG, SFG), and memory load (control, 2-target, 4-target). Significant interactions involving load were followed by separate post-hoc analyses of the WM trials (2-target, 4-target) and the control task.
Each model used the best-fitting correlation structure to account for the correlations within individual subjects and to provide maximum power for detecting effects. For each model employed, the best-fitting variance–covariance structure was selected using Schwartz–Bayesian Information Criterion. Non-significant interactions at the 0.1 level were dropped from the model so that at each step the model was hierarchically well-formulated. Follow-up analyses were reported with uncorrected p-values. Bonferroni correction was applied for multiple comparisons within but not between hypotheses. All analyses reported were statistically significant at the 0.05 level, after correction for multiple comparisons.
A bilateral ROI for Heschl's gyrus from the Harvard-Oxford Cortical Atlas, available in FSL, served as a control region. We chose this area because it is a primary cortical area that receives stimulation during scanning but has no specific role in a visual WM task. Thus, phase and trial type were irrelevant, and all the time points within each drug condition were averaged and compared with a paired t-test.
Connectivity Analysis
Connectivity maps
Cluster correction for all statistical maps is described in Supplementary Information. For the connectivity maps, first-level analyses were completed in two steps. First, we removed the global mean brain signal. Second, we completed two individual analyses, one for the R-dlPFC seed, a voxel located at MNI co-ordinates 43,22,34 and one for the L-dlPFC seed, a voxel located at −43,22,34. This voxel is slightly posterior to the MFG ROI used in the activation analyses. We extracted a time series for each seed (MNI right: 43,22,34; left: −43,22,34) from each subject's MNI-transformed data and also extracted additional time series from a voxel in the lateral ventricle and one in the central white matter of each hemisphere to serve as nuisance regressors. Separate multiple regressions were conducted in FSL for the left and right dlPFC seed, with each using the same nuisance regressors. The resulting statistical maps for each subject represented the positive and negative correlation of each voxel to the right or left dlPFC seed. Individual maps for each scan were combined to produce two second-level individual maps, one for saline and one for ketamine. These maps were then entered into higher-level FSL analyses to calculate group maps depicting the influence of drug condition (saline, ketamine) upon connectivity of these dlPFC seeds.
Testing for lateralization of connectivity effects
Because the L-dlPFC and R-dlPFC seeds were not homologous, we employed global-based connectivity or GBC, a method not biased by seed choice, to assess laterality effects. We first defined the WM network using the anatomical ROIs that our group has developed from previous investigations (Driesen et al, 2008; Leung et al, 2002, 2004). We then completed a GBC that was restricted to this WM network. In this case, GBC would refer to the average correlation of each and every voxel in the WM network with all the other voxels in the network. We then evaluated the average GBC of the left and right dlPFC ROIs under each condition (saline, ketamine) with all the other voxels in the WM network. We performed a drug (saline, ketamine) × hemisphere analysis with the MANOVA approach to repeated measures.
Relating connectivity to WM performance
We investigated this relationship in two ways. First, we evaluated whether overall changes in connectivity, regardless of their location, were associated with performance changes. To accomplish this, we counted the number of voxels in an individual's dlPFC saline and ketamine maps whose z score was higher than 1.96 and subtracted the saline voxel count from the ketamine voxel count. These difference variables were then correlated with performance change scores. Second, we evaluated whether connectivity changes in specific regions were associated with performance changes. To accomplish this, we created a statistical map of correlations between performance and connectivity changes on a voxel-by-voxel basis. The resulting correlation map was then converted to a p-map and cluster-corrected. All clusters were screened for outliers by graphing individuals' average connectivity change score for a cluster against their outcome variable score.
RESULTS
Assessment of movement indicated no significant effects of drug, scan, or their interaction (see Supplementary Information). Mean blood plasma ketamine levels were stable in the participants throughout the scanning session (+5 min: 140.9±58 ng/ml, +25 min: 133.5±30 ng/ml, +45 min: 161.7±33 ng/ml). Performance as measured by percent correct and RT was assessed in separate load (2-target, 4-target) × drug (saline, ketamine) ANOVAs (Table 2). Ketamine reduced performance accuracy (F(1,21)=5.21, p=0.03). Unsurprisingly, performance was lower for the high memory load compared with the low memory load condition (F(1,21)=12.81, p=0.002); however, ketamine and memory load did not interact with respect to behavioral performance. RT was slower at the higher memory load (F(1,21)=12.42, p=0.002), but there were no significant effects of ketamine upon RT. Ketamine increased negative, positive, and cognitive symptoms as measured by the PANSS (Supplementary Information, Supplementary Figure 1). Changes in symptoms did not correlate with performance accuracy.
Table 2. Performance (mean and SD) on Spatial Working Memory Task.
| Measure | Task | Saline | Ketamine |
|---|---|---|---|
| Percent correct | Control | 0.96 (0.06) | 0.97 (0.05) |
| 2-Target | 0.86 (0.09) | 0.83 (0.13) | |
| 4-Target | 0.80 (0.13) | 0.76 (0.13) | |
| Reaction time (ms) | Control | 932 (443) | 824 (406) |
| 2-Target | 1130(442) | 1134 (387) | |
| 4-Target | 1363 (728) | 1363 (584) |
Ketamine reduced performance accuracy (F(1,21)=5.21, p=0.03) as did increased load (2-target vs 4-target), (F(1,20)=11.67, p=0.003).
Values in italic represent standard deviations.
Activation
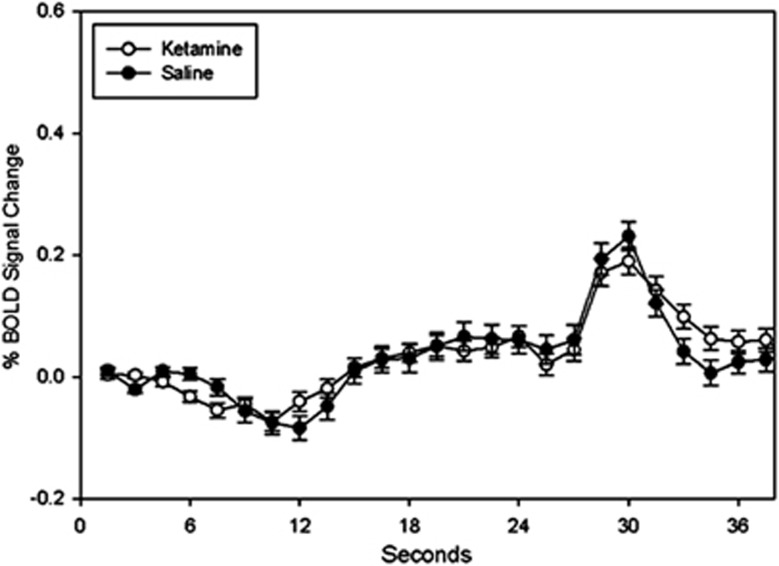
There was a significant interaction between drug, ROI, and load (F(4,1024)=2.67, p=0.03). See Supplementary Information and Supplementary Table 1 for details. During the control task, there were no drug-related differences during any phase (all p-values for post-hoc tests >0.38). During the WM trials (2-target and 4-target), drug treatment interacted with task phase, F(2,686)=11.17, p=0.000 (Supplementary Information, Supplementary Table 2). The difference between ketamine and saline achieved statistical significance during the EEM phase, F(1,686)=9.48, p=0.002, Figure 1b. The difference between ketamine and saline was not significant for the LM or response phases. Auditory time courses during the saline and ketamine condition were quite similar and did not differ statistically (Figure 2). There was no correlation between EEM decreases and positive, negative, or cognitive PANSS symptoms.
Figure 2.
Blood oxygen level–dependent (BOLD) percent signal change (mean±SEM) in auditory cortex.
Because ketamine-related decrements in percent signal change were statistically significant during the EEM phase, we examined the relationship between percent signal change and performance accuracy (percent correct) during this phase. In our mixed model, the difference between EEM percent signal change during ketamine and EEM percent signal change during saline served as the dependent variable. Performance accuracy, hemisphere (right vs left), memory load (4-target vs 2-target), and gyrus (MFG, SFG, IFG) were the independent variables. Alterations in EEM percent signal change were related to alterations in performance accuracy, with associative strength varying between load and gyrus, change in accuracy by load by gyrus, F(2,211)=5.48, p=0.005. Post-hoc comparisons were not statistically significant after multiple comparison corrections (see Supplementary Information, Supplementary Table 3).
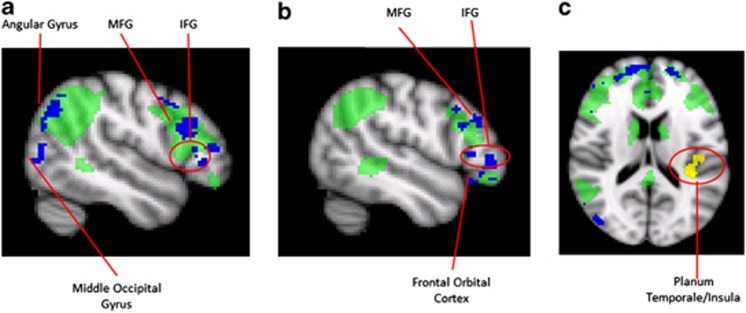
Connectivity
During performance of the WM task, there was a pronounced decrease in connectivity between the R-dlPFC seed and many brain areas under ketamine compared with saline (Figure 3). We refer to this result as hypoconnectivity. Within the frontal lobe, these regions of hypoconnectivity included the MFG extending anteriorly and inferiorly to the IFG, the frontal pole, and frontal orbital cortex, with additional hypoconnected areas in the insula and medial frontal gyrus (not shown). In the parietal lobe, decreased connectivity under ketamine was observed in the angular gyrus, extending inferiorly to the medial temporal and occipital gyri. In the frontal and parietal lobe, hypoconnectivity was mainly noted in areas that were positively correlated with the dlPFC seed time course under saline. The only area of hyperconnectivity observed in this analysis was in the parietal operculum near the border between the planum temporale and the insula.
Figure 3.
R-dlPFC functional connectivity with brain mean time course removed. Green shows task R-dlPFC connectivity under saline, blue are voxels that have higher correlation with R-dlPFC under saline than ketamine, yellow are voxels that have higher correlation with R-dlPFC under ketamine than saline. No other areas of the brain than those shown are significantly increased during ketamine. (a) right lateral saggital, (b) left lateral saggital, (c) axial (z=16).
Hypoconnectivity was also observed with respect to the L-dlPFC seed and there were no clusters where dlPFC connectivity was greater under saline than ketamine. A restricted GBC of the WM network was performed to assess laterality effects (see Materials and Methods). There was a main effect of drug with connectivity being lower under ketamine than saline, F=38.2 (1,21), p<0.001. The effect of hemisphere and the interaction of hemisphere and drug were not statistically significant (p's>0.38).
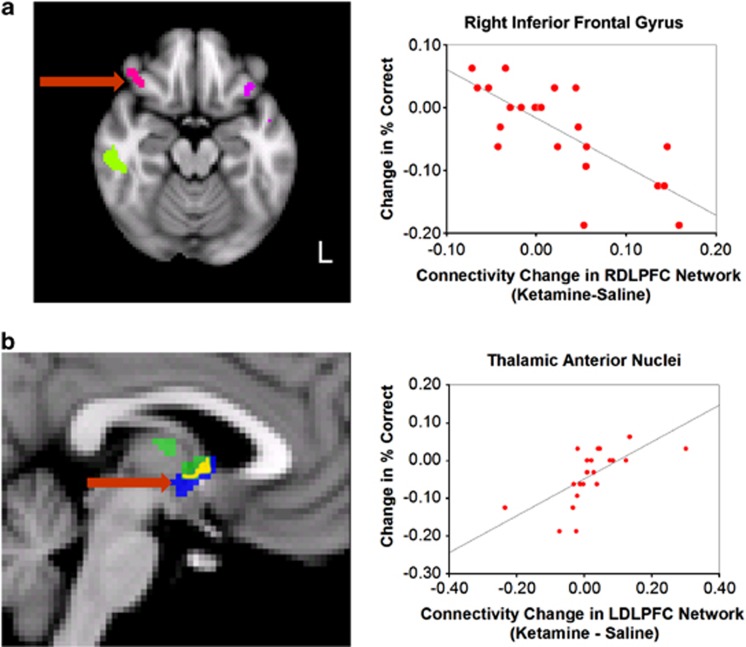
Connectivity and Performance
There was no statistically significant relationship between decreases in the number of voxels significantly correlated with the seed and performance. However, statistical maps correlating performance with connectivity changes indicated that ketamine-associated alterations in dlPFC networks were related to performance. There were moderate correlations (absolute values from 0.64–0.75) between alterations in dlPFC connectivity in specific areas and performance (Figure 4; Supplementary Information, Supplementary Tables 4 and 5). Most of the correlations between these moderating areas and dlPFC were negative, indicating an association between reduced connectivity in these areas and preserved or improved performance under ketamine. Positive correlations occurred mainly in the thalamus.
Figure 4.
Relationship between connectivity alterations and performance (each cluster is depicted with a different color). (a) Relationship between ketamine-related changes in percent correct and connectivity changes in the R-dlPFC network in the IFG observed during task. (b) Relationship between ketamine-related decreases in percent correct and connectivity changes in the thalamus. In blue, thalamic areas (anterior nuclei) correlated with L-dlPFC connectivity changes. In green, thalamic areas (medio-dorsal nucleus and anterior nuclei) correlated with R-dlPFC connectivity changes. In yellow, thalamic areas correlated with both R-dlPFC and L-dlPFC seeds (anterior nuclei). Red arrows indicate area shown in graph. All references to subareas within the thalamus are used for descriptive purposes only and are approximate. All clusters that appear on the slices pictured are shown and their co-ordinates and associated r-values are provided in Supplementary Information, Supplementary Tables 4 and 5.
DISCUSSION
As predicted by our hypotheses, ketamine impaired performance and reduced task-related activation in LPFC during the spatial WM task. Ketamine infusion was also associated with reduced connectivity during task in a network of brain areas involved in WM. Observed reductions in activation and connectivity were related to performance.
Activation During Task
Ketamine reduced task-related activation in the LPFC during the EEM task phase. This finding can be challenged as simply reflecting altered neurovascular coupling. However, previous investigators have reported both increases and decreases in activation under ketamine (Abel et al, 2003; Fu et al, 2005), and the drug did not significantly reduce activation in the control task or in the auditory ROI. This suggests that ketamine's effect on this task was specific to WM. These results parallel those of Wang et al (2013) who show that in the non-human primate, NMDA-R antagonists applied iontophoretically in the dlPFC systemically reduce firing in cue and delay neurons during the EEM phase of WM.
This phase comprises sensory perception, memory encoding, and memory maintenance. Ketamine alters sensory perception (Krystal et al, 1994; Oye et al, 1992; Vollenweider et al, 1997), reduces vigilance (Krystal et al, 1999; Krystal et al, 1994), and increases distractibility (Krystal et al, 2005b; Krystal et al, 1999). However, the effects on perception and attention, even at higher doses, are relatively subtle and do not explain the impairments in WM or declarative memory in prior studies (Newcomer and Krystal, 2001). These findings are consistent with the observation that, in this sample, positive cognitive or negative symptoms as measured by the PANSS did not correlate significantly with WM or with EEM activation deficits. Non-statistically significant trends in the data suggest that activation deficits might persist beyond the EEM, but this will need to be addressed in further experimentation.
Connectivity
To assess connectivity during task, we used a seed known to correlate highly with a group of areas involved in WM and other control processes. Notably, many of the connectivity reductions observed in the WM network during ketamine infusion were in areas that had previously had statistically significant correlations with the seed under saline (Figure 3), suggesting that ketamine produced substantial compromise in the network's ability to function. We further corroborated this hypothesis by using the GBC method and pre-defined anatomical ROIs to demonstrate that the connectivity strength of the left and right dlPFC was reduced during ketamine infusion. No laterality differences were observed in this effect.
Our recent report of increased ketamine-associated global hyperconnectivity during rest (Driesen et al, 2013) might shed light on the current finding of decreased dlPFC connectivity during the WM task. In fact, the same seed used in the current investigation exhibits hyperconnectivity during rest under ketamine (Supplementary Information, Supplementary Figure 2). WM requires an exquisite interplay of brain areas, and much of this co-ordination would be evident in the correlational structure of the blood oxygen level–dependent signal during the WM task. Thus, the combined connectivity findings might suggest that when under ketamine, the brain is still capable of increased functional connectivity, as is observed during rest; but the brain is incapable of generating the coordinated activity required for WM, as is observed during the spatial WM task.
Performance
The observation that ketamine significantly reduced performance on the spatial WM task further supports the view that ketamine produced dysfunction in the dlPFC and its network. This finding, however, was not universal, and some subjects, perhaps in an effort to compensate for perceived and/or actual deficits, improved their performance under ketamine. This performance variability allowed us to further investigate how ketamine-associated functional brain alterations might contribute to WM dysfunction. Ketamine-related changes in activation during the EEM were strongly associated with ketamine-related performance decrements, in a complex manner involving load and gyrus effects. Larger sample sizes might be required to elucidate these relationships.
It was not clear which brain areas would show connectivity alterations that were associated with performance. Accordingly, we took an empirically driven approach that was hypothesis generating rather than hypothesis confirming. In this endeavor, cluster correction was used to guard against false positives. Connectivity alterations in several areas were correlated with performance change under ketamine (Supplementary Information, Supplementary Tables 4 and 5). Correlations in most areas were negative, indicating that, in comparison to other subjects, lower correlations between R-dlPFC and the voxels in the cluster were associated with preserved or even improved performance under ketamine. These negatively correlated areas, with the exception of the bilateral IFG and the supramarginal gyrus, were not areas central to WM (D'Esposito et al, 1998; Leung et al, 2002; Smith et al, 1998) and thus peak functioning may have been unnecessary for the task. The reduced connectivity observed may reflect a sparer, more efficient process for accomplishing the task that promotes successful performance under ketamine challenge.
In this study, improved WM performance was associated with reduced IFG-dlPFC correlation. This finding was surprising as IFG typically activates along with dlPFC during WM (D'Esposito et al, 1998; Leung et al, 2002; Smith et al, 1996). However, IFG-dlPFC functional decoupling, perhaps related to cognitive control, might be a feature of the distracting effects of emotional arousal on WM (Dolcos et al, 2006a; Dolcos and McCarthy, 2006b). Thus, the arousing effects of ketamine might contribute to its disruptive effects on PFC activation during WM.
The finding that subjects who retained or increased connectivity between the anterior thalamus and the R-dlPFC also supports the importance of emotional control in preserving performance under ketamine. The anterior thalamus is closely associated with the limbic system (Fitzgerald et al, 2011). Thus, stronger connectivity between dlPFC and anterior nucleus might indicate greater engagement of control processes in warding off distracting emotions related to the ketamine experience.
Neuronal Basis of Ketamine Effects
The literature suggests that two, potentially complementary, mechanisms could produce the reduced WM-related activation and functional connectivity observed in this study. First, NMDA-R antagonists could directly affect pyramidal neurons in the dlPFC. Establishing and sustaining the recurrent excitation necessary for WM requires D1 and NMDA receptor stimulation (Castner and Williams, 2007). Thus, blocking NMDA-Rs in dlPFC would necessarily impair recurrent excitation in LPFC. This dysfunction would then likely affect the entire WM network. Second, WM networks are tuned by GABA interneurons (Arnsten, 2011; Rao et al, 2000) and there is evidence that NMDA-R antagonists, perhaps preferentially, impair GABA interneurons (Grunze et al, 1996; Homayoun and Moghaddam, 2007; Jackson et al, 2004; Maccaferri and Dingledine, 2002). In reality, these mechanisms are extremely difficult to dissociate because GABA interneurons and pyramidal neurons function in a reciprocal manner.
Limitations
This study has several limitations. First, although ketamine is among the most selective NMDA-R antagonists available for human studies, it has secondary sites of action unrelated to blockade of NMDA glutamate receptors (Cohen et al, 1974; Oye et al, 1992; Oye et al, 1991; Smith et al, 1980). Despite this, investigators have repeatedly shown that, adjusting for potency and pharmacokinetic differences, ketamine's effects closely resemble those of the more selective NMDA-R antagonists used in animal studies (Anis et al, 1983; Moghaddam et al, 1997; Wood et al, 2012). Moreover, research in animal and human models supports the hypothesis that cognitive effects and psychiatric symptoms observed in this study are directly linked to NMDA-R antagonism (Krystal et al, 2005b; Krystal et al, 1999; Moghaddam and Adams, 1998; Roberts et al, 2010).
Second, to avoid possible brain correlates related to error monitoring and subject frustration, we purposely chose a task that subjects would be able to perform fairly well under ketamine. Thus, we do not have enough error trials to perform a separate analysis on error trials alone. However, to determine whether the inclusion of the relatively few error trials influenced the reported analysis, we computed mean time courses for the correct trials only. The ordering of these effects was similar to those reported for the combined correct and incorrect trials (Supplementary Information, Supplementary Figure 3).
Third, although this experimental design does not control for order effects, it is based on our previous out-of-scanner ketamine studies. Of note, we have previously found that data collected in long double sessions are comparable to those collected in single sessions (Krystal et al, 2005a). Also, order of saline and ketamine administration does not affect observed ketamine-related short-term memory deficits (Krystal et al, 2000). In the current study, scan-by-scan analyses of the principal activation and connectivity findings do not suggest fatigue (Supplementary Information, Supplementary Figures 4 and 5). In a subsequent study (n=16), we found that saline (M=3.6, SD=1.2) and ketamine (M=3.5, SD=1.6) self-ratings of sedation were quite similar (Driesen et al, unpublished). However, the small number of trials per scan does not allow us to rule out the possibility that the behavioral results were affected by fatigue. Future studies that better control for order effects could strengthen confidence in the study findings. Finally, the spatial and temporal resolution of fMRI limits this study's ability to identify the cellular bases of the reported findings or to fully resolve subprocesses within WM. Thus, findings reported here need to be qualified by careful, preclinical investigations.
Conclusions
In this study, we have demonstrated that the NMDA-R antagonist ketamine decreases LPFC activation during early WM when percepts are encoded and the resulting WM traces are stored, established, and initially maintained. Ketamine also reduced connectivity within the WM network. These alterations were linked to performance impairment observed under ketamine. The current findings indicate critical roles for NMDA-Rs in WM. Medications that ameliorate the impact of NMDA-R antagonists might have a role in the treatment of cognitive impairments, particularly those observed in schizophrenia.
FUNDING AND DISCLOSURE
Zubin Bhagwagar is employed by Bristol-Myers Squibb and owns stock in the company. Deepak Cyril D'Souza has in the past three years or currently received research grant support administered through Yale University School of Medicine from Astra Zeneca, Abbott Laboratories, Eli Lilly Inc., Forest Laboratories, Organon, Pfizer Inc., and Sanofi. He is a consultant for Bristol Myers Squibb and Johnson & Johnson. John Krystal consults for several pharmaceutical and biotechnology companies, with compensation less than $10 000 per year. These companies include AbbVie, Inc.; Amgen; AstraZeneca Pharmaceuticals; Bristol-Myers Squibb; Eli Lilly and Co.; Janssen Research & Development; Lundbeck Research USA; Otsuka Pharmaceutical, Development & Commercialization, Inc.; Sage Therapeutics, Inc.; Shire Pharmaceuticals; Sunovion Pharmaceuticals, Inc.; Takeda Industries; and Teva Pharmaceutical Industries, Ltd. Dr Krystal is a member of the following scientific advisory boards: CHDI Foundation, Inc.; Lohocla Research Corporation, Mnemosyne Pharmaceuticals, Inc.; Naurex, Inc.; and Pfizer Pharmaceuticals. In addition, Dr Krystal is a board member of the Coalition for Translational Research in Alcohol and Substance Use Disorders, president of the American College of Neuropsychopharmacology, editor of Biological Psychiatry; and an employee of the Yale University School of Medicine and the VA CT Health System. He is an originator on the following patent: Seibyl JP, Krystal JH, and Charney DS; Dopamine and noradrenergic reuptake inhibitors in treatment of schizophrenia; Patent #:5 447 948; 5 September 1995. In addition, he is an originator of the following relevant pending patents: (1) Vladimir, Coric; Krystal, John H, Sanacora, Gerard—Glutamate Agents in the Treatment of Mental Disorders No 11/399 188; 5 April 2006 (Pending). (2) Intranasal Administration of Ketamine to Treat Depression (Pending). The remaining authors declare no conflict of interest.
Acknowledgments
Dr Driesen thanks the following individuals: Dr Amy Arnsten provided helpful comments regarding this manuscript and related topics. Drs Michelle Hampson and Pawel Skudlarski provided advice regarding the connectivity analysis. Cheryl Lacadie helped informally with a number of image processing and software issues. Kathleen Maloney, Julie Holub, Cara Cordeaux, and Nikia McFadden served as research assistants. Nursing care was provided by the Yale Center for Clinical Investigation and the Biostudies Unit, Neurobiological Diagnostic Studies Unit of the VA CT Healthcare System, West Haven, CT, USA. MRI technologists Hedy Sarofin and Karen A Martin supplied expert assistance for this complex MRI protocol. This study was supported by Yale-Pfizer Alliance (NRD); National Alliance for Research on Schizophrenia and Depression-Distinguished Investigator Award (JHK) and Young Investigator Award (ZB); Conte Center Calcium Signaling and Prefrontal Deficits in Schizophrenia, NIMH; National Center for Post-Traumatic Stress Disorder, Clinical Neurosciences Division, West Haven, CT, USA; National Institute on Alcohol Abuse and Alcoholism, 2P50 AA 012870; US Department of Veterans Affairs Alcohol Research Center; NIH National Center for Research Resources CTSA Grant Number UL1 RR024139; NIH Grant Number K23-MH077914; and the State of CT Department of Mental Health and Addiction Services.
Footnotes
Supplementary Information accompanies the paper on the Neuropsychopharmacology website (http://www.nature.com/npp)
Data from this paper were presented at the May 2012 Biological Psychiatry and June 2013 Human Brain Mapping meetings.
Supplementary Material
References
- Abel K, Allin MPG, Kucharska Pietura K, David A, Andrew C, Williams S, et al. Ketamine alters neural processing of facial emotion recognition in healthy men: an fMRI study. Neuroreport. 2003;14:387–391. doi: 10.1097/00001756-200303030-00018. [DOI] [PubMed] [Google Scholar]
- Anis NA, Berry SC, Burton NR, Lodge D. The dissociative anaesthetics, ketamine and phencyclidine, selectively reduce excitation of central mammalian neurones by N-methyl-aspartate. Br J Pharmacol. 1983;79:565–575. doi: 10.1111/j.1476-5381.1983.tb11031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnsten AFT. Prefrontal cortical network connections: key site of vulnerability in stress and schizophrenia. Int J Dev Neurosci. 2011;29:215–223. doi: 10.1016/j.ijdevneu.2011.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baddeley AD. Working memory. Science. 1992;255:556–559. doi: 10.1126/science.1736359. [DOI] [PubMed] [Google Scholar]
- Baron SP, Wenger GR. Effects of drugs of abuse on response accuracy and bias under a delayed matching-to-sample procedure in squirrel monkeys. Behav Pharmacol. 2001;12:247–256. doi: 10.1097/00008877-200107000-00003. [DOI] [PubMed] [Google Scholar]
- Bell M, Lysaker P, Beam-Goulet J, Milstein R, Lindemayer J. Five-component model of schizophrenia: assessing the factorial invariance of the positive and negative syndrome scale. Psychiatry Res. 1994;52:295–303. doi: 10.1016/0165-1781(94)90075-2. [DOI] [PubMed] [Google Scholar]
- Biswal B, Yetkin FZ, Haughton VM, Hyde JS. Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magnetic Resonance in Medicine. 1995;34:537–541. doi: 10.1002/mrm.1910340409. [DOI] [PubMed] [Google Scholar]
- Brown H, Prescott R. Applied Mixed Models in Medicine. John Wiley & Sons, LTD: Chichester; 1999. [Google Scholar]
- Castner S, Williams GV. Tuning the engine of cognition: a focus on NMDA/D1 receptor interactions in prefrontal cortex. Brain Cogn. 2007;63:94–122. doi: 10.1016/j.bandc.2006.11.002. [DOI] [PubMed] [Google Scholar]
- Cohen ML, Chan SL, Bhargava HN, Trevor AJ. Inhibition of mammalian brain acetylcholinesterase by ketamine. Biochem Pharmacol. 1974;23:1647–1652. doi: 10.1016/0006-2952(74)90377-3. [DOI] [PubMed] [Google Scholar]
- Cole M, Yarkoni T, Repovs G, Anticevic A, Braver T. Global connectivity of prefrontal cortex predicts cognitive control and intelligence. J Neurosci. 2012;32:8988–8999. doi: 10.1523/JNEUROSCI.0536-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole MW, Anticevic A, Repovs G, Barch D. Variable Global Dysconnectivity and Individual Differences in Schizophrenia. Biol Psychiatry. 2011;70:43–50. doi: 10.1016/j.biopsych.2011.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole MW, Pathak S, Schneider W. Identifying the brain's most globally connected regions. NeuroImage. 2010;49:3132–3148. doi: 10.1016/j.neuroimage.2009.11.001. [DOI] [PubMed] [Google Scholar]
- Courtney SM, Petit L, Maisog JM, Ungerleider LG, Haxby JV. An area specialized for spatial working memory in human frontal cortex. Science. 1998;279:1347–1351. doi: 10.1126/science.279.5355.1347. [DOI] [PubMed] [Google Scholar]
- Courtney SM, Ungerleider LG, Keil K, Haxby JV. Transient and sustained activity in a distributed neural system for human working memory. Nature. 1997;386:608–611. doi: 10.1038/386608a0. [DOI] [PubMed] [Google Scholar]
- Dolcos F, Kragel P, Wang L, McCarthy G. Role of the inferior frontal cortex in coping with distracting emotions. Neuroreport. 2006a;17:1591–1594. doi: 10.1097/01.wnr.0000236860.24081.be. [DOI] [PubMed] [Google Scholar]
- Dolcos F, McCarthy G. Brain systems mediating cognitive interference by emotional distraction. J Neurosci. 2006b;26:2072–2079. doi: 10.1523/JNEUROSCI.5042-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dosenbach NUF, Fair DA, Miezin FM, Cohen AL, Wenger KK, Dosenbach RAT, et al. Distinct brain networks for adaptive and stable task control in humans. Proc Natl Acad Sci USA. 2007;104:11073–11078. doi: 10.1073/pnas.0704320104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dosenbach NUF, Visscher KM, Palmer ED, Miezin FM, Wenger KK, Kang HC, et al. A core system for the implementation of task sets. Neuron. 2006;50:799–812. doi: 10.1016/j.neuron.2006.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driesen N, Leung H, Calhoun V, Constable R, Gueorguieva R, Hoffman R, et al. Impairment of working memory maintenance and response in schizophrenia: functional magnetic resonance imaging evidence. Biol Psychiatry. 2008;64:1026–1034. doi: 10.1016/j.biopsych.2008.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driesen N, McCarthy G, Bloch M, He G, Morgan P, Krystal JH.(unpublished). Guanfacine moderates activation and connectivity under NMDA blockade.
- Driesen NR, McCarthy G, Bhagwagar Z, Bloch M, Calhoun V, D'Souza DC, et al. 2013Relationship of resting brain hyperconnectivity and schizophrenia-like symptoms produced by the NMDA receptor antagonist ketamine in humans Mol Psychiatry(e-pub ahead of print, 22 January 2013; doi: 10.1038/mp.2012.194 [DOI] [PMC free article] [PubMed]
- D'Esposito M, Aguirre GK, Zarahn E, Ballard D, Shin RK, Lease J. Functional MRI studies of spatial and nonspatial working memory. Brain Res. 1998;7:1–13. doi: 10.1016/s0926-6410(98)00004-4. [DOI] [PubMed] [Google Scholar]
- Fellous J-M, Sejnowski TJ. Regulation of persistent activity by background inhibition in an in vitro model of a cortical microcircuit. Cereb Cortex. 2003;13:1232–1241. doi: 10.1093/cercor/bhg098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgerald M, Gruener G, Mtui E. Clinical Neuroanatomy and Neuroscience. Saunders; 2011. [Google Scholar]
- Frederick DL, Gillam MP, Allen RR, Paule MG. Acute behavioral effects of phencyclidine on rhesus monkey performance in an operant test battery. Pharmacol Biochem Behav. 1995;52:789–797. doi: 10.1016/0091-3057(95)00182-v. [DOI] [PubMed] [Google Scholar]
- Fu CHY, Abel K, Allin MPG, Gasston D, Costafreda S, Suckling J, et al. Effects of ketamine on prefrontal and striatal regions in an overt verbal fluency task: a functional magnetic resonance imaging study. Psychopharmacology. 2005;183:92–102. doi: 10.1007/s00213-005-0154-9. [DOI] [PubMed] [Google Scholar]
- Fuster JM, Alexander GE. Neuron activity related to short-term memory. Science. 1971;173:652–654. doi: 10.1126/science.173.3997.652. [DOI] [PubMed] [Google Scholar]
- Ghoneim MM, Hinrichs JV, Mewaldt SP, Petersen RC. Ketamine: behavioral effects of subanesthetic doses. J Clin Psychopharmacol. 1985;5:70–77. [PubMed] [Google Scholar]
- Goldman-Rakic P. Cellular basis of working memory. Neuron. 1995;14:477–485. doi: 10.1016/0896-6273(95)90304-6. [DOI] [PubMed] [Google Scholar]
- Grunze HC, Rainnie DG, Hasselmo ME, Barkai E, Hearn EF, McCarley RW, et al. NMDA-dependent modulation of CA1 local circuit inhibition. J Neurosci. 1996;16:2034–2043. doi: 10.1523/JNEUROSCI.16-06-02034.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gueorguieva R, Krystal JH. Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the archives of general psychiatry. Arch Gen Psychiatry. 2004;61:310–317. doi: 10.1001/archpsyc.61.3.310. [DOI] [PubMed] [Google Scholar]
- Hampson M, Peterson BS, Skudlarski P, Gatenby JC, Gore JC. Detection of functional connectivity using temporal correlations in MR images. Hum Brain Mapp. 2002;15:247–262. doi: 10.1002/hbm.10022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homayoun H, Moghaddam B. NMDA receptor hypofunction produces opposite effects on prefrontal cortex interneurons and pyramidal neurons. J Neurosci. 2007;27:11496–11500. doi: 10.1523/JNEUROSCI.2213-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homayoun H, Stefani MR, Adams BW, Tamagan GD, Moghaddam B. Functional interaction between NMDA and mGlu5 receptors: effects on working memory, instrumental learning, motor behaviors, and dopamine release. Neuropsychopharmacology. 2004;29:1259–1269. doi: 10.1038/sj.npp.1300417. [DOI] [PubMed] [Google Scholar]
- Honey RAE, Honey GD, O'Loughlin C, Sharar SR, Kumaran D, Bullmore ET, et al. Acute ketamine administration alters the brain responses to executive demands in a verbal working memory task: an fMRI study. Neuropsychopharmacology. 2004;29:1203–1214. doi: 10.1038/sj.npp.1300438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson ME, Homayoun H, Moghaddam B. NMDA receptor hypofunction produces concommitant firing rate potentiation and burst activity reduction in the prefrontal cortex. Neuroscience. 2004;101:8467–8472. doi: 10.1073/pnas.0308455101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay S, Opler L, Fiszbein A. Positive and Negative Syndrome Scale. Multi-Health Systems, Inc.: Toronto, Ontario; 1986. [Google Scholar]
- Krystal J, Abi Saab W, Perry E, D'Souza DC, Liu N, Gueorguieva R, et al. Preliminary evidence of attenuation of the disruptive effects of the NMDA glutamate receptor antagonist, ketamine, on working memory by pretreatment with the group II metabotropic glutamate receptor agonist, LY354740, in healthy human subjects. Psychopharmacology. 2005a;179:303–309. doi: 10.1007/s00213-004-1982-8. [DOI] [PubMed] [Google Scholar]
- Krystal JH, Abi-Saab W, Perry E, D'Souza DC, Liu N, Gueorguieva R, et al. Preliminary evidence of attenuation of the disruptive effects of the NMDA glutamate receptor antagonist, ketamine, on working memory by pretreatment with the group II metabotropic glutamate receptor agonist, LY354740, in healthy human subjects. Psychopharmacology. 2005b;179:303–309. doi: 10.1007/s00213-004-1982-8. [DOI] [PubMed] [Google Scholar]
- Krystal JH, Bennett A, Abi Saab D, Belger A, Karper LP, D'Souza DC, et al. Dissociation of ketamine effects on rule acquisition and rule implementation: possible relevance to NMDA receptor contributions to executive cognitive functions. Biol Psychiatry. 2000;47:137–143. doi: 10.1016/s0006-3223(99)00097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krystal JH, D'Souza DC, Karper LP, Bennett A, Abi-Dargham A, Abi-Saab D, et al. Interactive effects of subanesthetic ketamine and haloperidol in healthy humans. Psychopharmacology. 1999;145:193–204. doi: 10.1007/s002130051049. [DOI] [PubMed] [Google Scholar]
- Krystal JH, Karper LP, Bennett A, D'Souza DC, Abi Dargham A, Morrissey K, et al. Interactive effects of subanesthetic ketamine and subhypnotic lorazepam in humans. Psychopharmacology. 1998;135:213–229. doi: 10.1007/s002130050503. [DOI] [PubMed] [Google Scholar]
- Krystal JH, Karper LP, Seibyl JP, Freeman GK, Delaney R, Bremner JD, et al. Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans: psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry. 1994;51:199–214. doi: 10.1001/archpsyc.1994.03950030035004. [DOI] [PubMed] [Google Scholar]
- Leung HC, Gore JC, Goldman-Rakic PS. Sustained mnemonic response in the human middle frontal gyrus during on-line storage of spatial memoranda. J Cogn Neurosci. 2002;14:659–671. doi: 10.1162/08989290260045882. [DOI] [PubMed] [Google Scholar]
- Leung HC, Seelig D, Gore JC. The effect of memory load on cortical activity in the working memory circuit. Cogn Affect Behav Neurosci. 2004;4:553–563. doi: 10.3758/cabn.4.4.553. [DOI] [PubMed] [Google Scholar]
- Lisman JE, Fellous J-M, Wang X-J. A role for NMDA-receptor channels in working memory. Nat Neurosci. 1998;1:273–276. doi: 10.1038/1086. [DOI] [PubMed] [Google Scholar]
- Maccaferri G, Dingledine R. Control of feedforward dendritic inhibition by NMDA receptor-dependent spike timing in hippocampal interneurons. J Neurosci. 2002;22:5462–5472. doi: 10.1523/JNEUROSCI.22-13-05462.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moghaddam B, Adams B, Verma A, Daly D. Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. J Neurosci. 1997;17:2921–2927. doi: 10.1523/JNEUROSCI.17-08-02921.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moghaddam B, Adams BW. Reversal of phencyclidine effects by a group II metabotropic glutamate receptor agonist in rats. Science. 1998;281:1349–1352. doi: 10.1126/science.281.5381.1349. [DOI] [PubMed] [Google Scholar]
- Newcomer JW, Krystal JH. NMDA receptor regulation of memory and behavior in humans. Hippocampus. 2001;11:529–542. doi: 10.1002/hipo.1069. [DOI] [PubMed] [Google Scholar]
- Oye I, Paulsen O, Maurset A. Effects of ketamine on sensory perception: evidence for a role of N-methyl-D-aspartate receptors. J Pharmacol Exp Ther. 1992;260:1209–1213. [PubMed] [Google Scholar]
- Oye N, Hustvelt O, Moberg ER, Pausen O, Skoglund LS.1991The chiral forms of ketamine as probed for NMDA receptor function in humansIn: Kameyama T, Nabeshima T, Domino E (eds). NMDA Receptor Related Agents: Biochemistry, Pharmacology, and Behavior Vol 381–389.NPP Books: Ann Arbor, MI [Google Scholar]
- Raichle M, MacLeod A, Snyder A, Powers W, Gusnard D, Shulman G. A Default mode of brain function. Proc Natl Acad Sci USA. 2001;98:676–682. doi: 10.1073/pnas.98.2.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao S, Williams G, Goldman-Rakic P. Destruction and creation of spatial tuning by disinhibition: GABAA blockade of prefrontal cortical neurons engaged by working memory. J Neurosci. 2000;20:485–494. doi: 10.1523/JNEUROSCI.20-01-00485.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BM, Shaffer CL, Seymour PA, Schmidt CJ, Williams GV, Castner SA. Glycine transporter inhibition reverses ketamine-induced working memory deficits. Neuroreport. 2010;21:390–394. doi: 10.1097/WNR.0b013e3283381a4e. [DOI] [PubMed] [Google Scholar]
- Seamans J, Yang C. The principal features and mechanisms of dopamine modulation in the prefrontal cortex. Prog Neurobiol. 2004;74:1–57. doi: 10.1016/j.pneurobio.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Seamans JK, Nogueira L, Lavin A. Synaptic basis of persistent activity in prefrontal cortex in vivo and in organotypic cultures. Cereb Cortex. 2003;13:1242–1250. doi: 10.1093/cercor/bhg094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DJ, Westfall DP, Adams JD. Ketamine interacts with opiate receptors as an agonist. Anesthesiology. 1980;53:S5. [Google Scholar]
- Smith EE, Jonides J, Koeppe RA. Dissociating verbal and spatial working memory using PET. Cereb Cortex. 1996;6:11–20. doi: 10.1093/cercor/6.1.11. [DOI] [PubMed] [Google Scholar]
- Smith EE, Jonides J, Marshuetz C, Koeppe RA. Components of verbal working memory: evidence from neuroimaging. Proc Natl Acad Sci USA. 1998;95:876–882. doi: 10.1073/pnas.95.3.876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollenweider F, Leenders K, Scharfetter C, Antonini A, Maguire P, Missimer J, et al. Metabolic hyperfrontality and psychopathology in the ketamine model of psychosis using positron emission tomography (PET) and [18F]fluorodeoxyglucose (FDG) Eur Neuropsychopharmacol. 1997;7:9–24. doi: 10.1016/s0924-977x(96)00039-9. [DOI] [PubMed] [Google Scholar]
- Wang M, Gamo N, Yang Y, Jin L, Wang X-J, Laubach M, et al. Neuronal basis of age-related working memory decline. Nature. 2011;476:210–213. doi: 10.1038/nature10243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M, Vijayraghavan S, Goldman-Rakic PS. Selective D2 receptor actions on the functional circuitry of working memory. Science. 2004;303:853–856. doi: 10.1126/science.1091162. [DOI] [PubMed] [Google Scholar]
- Wang M, Yang Y, Wang C-J, Gamo Nao J, Jin LuE, Mazer James A, et al. NMDA Receptors Subserve Persistent Neuronal Firing during Working Memory in Dorsolateral Prefrontal Cortex. Neuron. 2013;77:736–749. doi: 10.1016/j.neuron.2012.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood J, Kim Y, Moghaddam B. Disruption of prefrontal cortex large scale neuronal activity by different classes of psychotomimetic drugs. J Neurosci. 2012;32:3022–3031. doi: 10.1523/JNEUROSCI.6377-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.