Abstract
Objectives. We assessed whether homeless adults entering substance abuse treatment in Massachusetts were less likely than others to enroll in Medicaid after implementation of the MassHealth Medicaid expansion program in 1997.
Methods. We used interrupted time-series analysis in data on substance abuse treatment admissions from the Treatment 0Episode Data Set (1992–2009) to evaluate Medicaid coverage rates in Massachusetts and to identify whether trends differed between homeless and housed participants. We also compared Massachusetts data with data from 17 other states and the District of Columbia combined.
Results. The percentage of both homeless and housed people entering treatment with Medicaid increased approximately 21% after expansion (P = .01), with an average increase of 5.4% per year over 12 years (P = .01). The increase in coverage was specific to Massachusetts, providing evidence that the MassHealth policy was the cause of this increase.
Conclusions. Findings provide evidence in favor of state participation in the Medicaid expansion in January 2014 under the Affordable Care Act and suggest that hard-to-reach vulnerable groups such as substance-abusing homeless adults are as likely as other population groups to benefit from this policy.
Implemented in 1965, Medicaid was designed as publicly funded health insurance coverage for indigent US citizens and legal permanent residents. The program is jointly funded by the state and federal governments, and states are mandated to provide coverage for children younger than 6 years whose family incomes fall below 133%, children between ages 6 and 17 years whose family incomes fall below 100%, and pregnant women whose incomes fall below 133% of the federal poverty level, as defined by the US Department of Health and Human Services1; individuals who are aged, blind, or disabled and who are eligible for Supplemental Security Income; and low-income Medicare beneficiaries. This program has provided health insurance access to a significant number of previously uninsured low-income Americans and continues to be the only route to health care coverage for many people.
Nationwide, Medicaid coverage has been found to be associated with several positive outcomes. Medicaid recipients have greater access to medical treatment than uninsured individuals and, therefore, fewer emergency department visits.2–6 Medicaid enrollees have better overall health and lower mortality rates over time than uninsured persons, likely because they have increased access to treatment.7–10 As a result, their medical care is significantly less costly to society, because health problems are more likely to be addressed before the onset of complications and adverse outcomes.11
Although the implementation of the Medicaid program has been a largely successful attempt to provide medical insurance, a significant number of low-income adults remain uninsured, mainly because childless adults without qualifying disabilities are ineligible.12–14 In response to this disparity, some states have developed programs to broaden eligibility criteria through a Section 1115 waiver. Massachusetts was among the first states to implement such an initiative, establishing the MassHealth program in July 1997. Among other provisions, the program extended Medicaid eligibility to families and childless adults whose incomes fell below 200% and 133% of the federal poverty level, respectively. MassHealth was jointly funded by the federal and state governments, with Massachusetts paying for roughly 46% of the program.15,16
Outcome evaluations of the MassHealth program demonstrated it to be remarkably successful, with significant declines in uninsured rates, particularly among childless adults who would otherwise be ineligible for Medicaid coverage.17,18 Research by Long et al. found that the MassHealth program resulted in a 33% decrease in the rate of uninsured Massachusetts residents.19 Furthermore, Quigley et al. reported that the MassHealth program covers nearly 1 in 6 Massachusetts residents.15 Consequently, it is estimated that only 6% of adults and 3% of children in Massachusetts remained uninsured after implementation of the program.
Although evaluations of MassHealth have provided strong support for the program, some evidence suggests that certain marginalized populations are less affected by Medicaid expansion policies than others.16,20 Despite meeting the income eligibility criteria, many people living in poverty remain uninsured because they don't know they are eligible, they don't know how to obtain coverage, or they lack any form of identification.21,22 Homeless adults are disproportionately affected by lack of insurance and are reportedly difficult to enroll in public insurance programs.23,24 Although Massachusetts developed several approaches for targeting this hard-to-reach population, evidence suggests that the effort to enroll homeless adults and keep them enrolled faces many logistical barriers.16
These challenges are even greater among homeless individuals with substance use disorders. These disorders are common among homeless persons, with prevalence estimates of 40% to 60%.25,26 These individuals generally have significantly greater health care needs, for treatment of, for example, psychiatric disorders, HIV and other sexually transmitted infections, hepatitis, liver disease, lung disease, and wound and skin infections.27–30 The premature mortality rate is significantly higher for homeless individuals than for the general population,27,31 and homeless people with substance use disorders are even more disproportionately affected.31,32 Finally, substance abuse is among the strongest predictors of returning to homelessness among formerly homeless individuals.33–36 Therefore, homeless adults' lack of the Medicaid coverage necessary to obtain treatment is a significant public health concern.
Assessing the impact of MassHealth is especially important in the context of national policy initiatives. Currently, many low-income childless adults qualify for Medicaid benefits because of a physical or mental health disability, but substance abuse is not among the conditions that confer eligibility, so many substance-abusing homeless adults who do not have children are ineligible for Medicaid coverage. However, a major provision of the Affordable Care Act is that all individuals with incomes that fall at or below 133% of the federal poverty level will be eligible for Medicaid effective January 2014, irrespective of parental or disability status. Although a Supreme Court ruling in June 2012 rejected a mandate for states to expand coverage,37 it is still expected that a significant portion of individuals with substance use disorders will benefit tremendously from the law's expanded eligibility.
To date, no large-scale quantitative evaluation has attempted to determine whether marginalized population groups, such as homeless substance-abusing adults, still have difficulty obtaining coverage under the Medicaid expansion.16,20–24 Data from state programs such as MassHealth are useful in assessing whether these groups will benefit from Medicaid expansion to the same extent as other population groups or may be in need of targeted interventions to improve their access. We examined administrative data on admissions to substance abuse treatment programs from 1992 to 2009 to assess the uptake of Medicaid coverage by substance-abusing homeless adults after the implementation of MassHealth in 1997. We assessed whether homeless adults entering substance use disorder treatment programs were less likely than housed adults to be covered by Medicaid. To rule out the potential impact of secular trends in national Medicaid coverage, we compared uptake of Medicaid coverage in adults entering substance abuse programs after 1997 in Massachusetts with rates in other states.
METHODS
We obtained data from the admissions files of the Treatment Episode Data Set (TEDS) from 1992 to 2009.38 The TEDS system is operated by the Office of Applied Studies, Substance Abuse and Mental Health Services Administration and consists of national data that is routinely collected by states to monitor their substance abuse treatment systems. Facilities that receive state alcohol or drug agency funds for the provision of substance abuse treatment are most commonly represented by the TEDS system.
Sample
We limited our sample to data from participants aged 18 years and older who had Medicaid or were uninsured and who received treatment in a state that collected data on insurance status at the time of admission. The final sample totaled 958 238 admissions in Massachusetts and 6 504 507 admissions in 17 other states and the District of Columbia. The comparison states were Alaska, Arizona, Colorado, Hawaii, Idaho, Illinois, Maryland, Missouri, Montana, North Dakota, Nebraska, New Hampshire, New Jersey, Nevada, Pennsylvania, Texas, and West Virginia.
States provided information on demographic and socioeconomic characteristics for all clients entering substance abuse treatment, including housing status (homeless, independent living, or dependent living) and insurance status (private, Medicaid, Medicare, or none).
Statistical Analyses
We used interrupted time-series models39,40 to evaluate Medicaid coverage rates over time among Massachusetts adults in substance abuse treatment and to identify whether this trend differed between homeless and housed participants. We used TEDS admissions data to obtain the dependent outcomes of percentage of admissions with Medicaid coverage in each year in Massachusetts and in all comparison states combined (for the comparison of enrollment in Massachusetts vs other states), and within Massachusetts, the percentage of admissions with Medicaid enrollment among the homeless and housed. The independent variables in these models were year, indicator variable for secular trend (year − 1992), before-to-after 1997 (0 if 1997 or earlier; 1 if 1998 or later), and trend after 1997 (0 for 1997 and all years before 1997; year − 1997 for all subsequent years).
Before conducting the time-series analyses, we assessed autocorrelation across years with the Durbin–Watson test and the Newey–West statistic for autocorrelation.41 Presence of such autocorrelation invalidates the use of ordinary least squares regressions and calls for other regression techniques that take such dependency in data into account. The result of the Durbin–Watson test was inconclusive, and the Newey–West statistic did not support the existence of an autocorrelation. Therefore, we used ordinary least squares regression with percentage of participants covered by Medicaid as the dependent variable and secular trend, before-to-after 1997, and trend after 1997 as the independent variables in the model.
We conducted 2 sets of analyses. First, we used model 1 to ensure that the change in Medicaid enrollment was not a result of national changes over this period. We added a new variable, state, set at 1 for Massachusetts and zero for comparison states combined. We included an interaction term, state * before-to-after 1997, in the analysis to indicate whether the effect of the variable before-to-after 1997 on Medicaid enrollment was different for Massachusetts than for other states. We also included 2 other interactions terms in the model: state * secular trend and state * trend after 1997. These interactions tested whether secular trends across the whole 1992 to 2009 period were different for Massachusetts than for other states and whether the trend varied between Massachusetts and other states after 1997.
Model 2 assessed whether the trends in Medicaid coverage differed by housing status, and we used the variable homeless, set at 1 if participants were homeless and zero if they were housed. In data limited to Massachusetts, we assessed the association of the interaction term of homelessness with the variable of before-to-after 1997. A statistically significant interaction term would indicate that the impact of change in policy differed between the homeless and the housed in the state of Massachusetts. Again, we included 2 other interaction terms in the model: homeless * secular trend and homeless * trend after 1997. These interactions tested whether secular trends across the whole 1992 to 2009 period differed between the homeless and the housed in Massachusetts and whether the trend varied between these groups after 1997.
We also conducted 2 sensitivity analyses. First, because it was not possible to determine whether individuals were represented multiple times in the TEDS data, we repeated the same analyses in data limited to individuals without a previous treatment episode. Second, because of the high degree of variability between the other states to which we compared Massachusetts, we conducted 3 additional analyses comparing Massachusetts to the 3 states (Illinois, Maryland, and New Jersey) that were most comparable in demographic and economic characteristics,42 as well as in the Medicaid enrollment rate prior to the MassHealth implementation. We performed all statistical analyses with STATA version 10.0.43
RESULTS
Table 1 displays the number of TEDS admissions in Massachusetts and in other states and the District of Columbia combined, as well as the percentage of participants with Medicaid coverage between 1992 and 2009. Before the policy was implemented, 18% to 27% of homeless adults entering substance abuse treatment programs in Massachusetts were covered under Medicaid, and 19% to 35% of housed participants were covered. In the year immediately following MassHealth implementation, the rate of Medicaid coverage remained relatively low, at 29% and 23% for the homeless and housed, respectively, and 24% for all participants in Massachusetts. However, in all years following 1998, the percentage of homeless participants with Medicaid exceeded 50%; it reached 80% in 2009. Among housed participants, the rate of Medicaid coverage was 49% in 1999 and 72% in 2009. By contrast, the percentages were substantially lower in other states, both before and after the implementation of the policy, with percentages ranging from 11% to 20% during the entire period.
TABLE 1—
Medicaid Enrollees Among Adults Entering Substance Use Disorder Treatment Programs in Massachusetts and Other States Before and After 1997 MassHealth Eligibility Expansion: Treatment Episodes Data Set, 1992–2009.
| Massachusetts Homeless |
Massachusetts Housed |
Massachusetts Total |
Comparison Statesa |
|||||
| Year | Total Admissions, No. | Medicaid Enrollees, % | Total Admissions, No. | Medicaid Enrollees, % | Total Admissions, No. | Medicaid Enrollees, % | Total Admissions, No. | Medicaid Enrollees, % |
| Before implementation | ||||||||
| 1992 | 7185 | 23 | 37 140 | 32 | 44 325 | 30 | 309 072 | 15 |
| 1993 | 8236 | 27 | 42 169 | 35 | 50 405 | 34 | 333 783 | 16 |
| 1994 | 8023 | 26 | 43 258 | 32 | 51 281 | 31 | 335 963 | 18 |
| 1995 | 9119 | 23 | 41 716 | 25 | 50 835 | 25 | 330 313 | 18 |
| 1996 | 10 118 | 21 | 40 053 | 22 | 50 171 | 23 | 292 179 | 17 |
| 1997 | 9980 | 18 | 40 314 | 19 | 50 294 | 19 | 285 992 | 12 |
| After implementation | ||||||||
| 1998 | 8524 | 29 | 34 214 | 23 | 42 738 | 24 | 327 167 | 11 |
| 1999 | 11 273 | 55 | 42 697 | 49 | 53 970 | 50 | 348 017 | 12 |
| 2000 | 10 758 | 60 | 44 975 | 55 | 55 733 | 56 | 359 677 | 13 |
| 2001 | 12 226 | 64 | 47 447 | 62 | 59 673 | 62 | 365 603 | 14 |
| 2002 | 12 937 | 67 | 40 547 | 64 | 53 484 | 65 | 390 379 | 15 |
| 2003 | 9536 | 59 | 30 579 | 55 | 40 115 | 56 | 382 924 | 15 |
| 2004 | 10 787 | 70 | 34 052 | 61 | 44 839 | 64 | 408 113 | 17 |
| 2005 | 10 905 | 69 | 33 813 | 58 | 44 718 | 60 | 413 494 | 17 |
| 2006 | 18 198 | 67 | 52 085 | 56 | 70 283 | 59 | 398 574 | 19 |
| 2007 | 18 071 | 69 | 48 983 | 60 | 67 054 | 63 | 380 669 | 20 |
| 2008 | 14 088 | 75 | 41 569 | 69 | 55 657 | 71 | 423 699 | 18 |
| 2009 | 14 076 | 80 | 47 070 | 72 | 61 146 | 74 | 418 889 | 19 |
Combined data from DC and AK, AZ, CO, HI, ID, IL, MD, MO, MT, ND, NE, NH, NJ, NV, PA, TX, and WV.
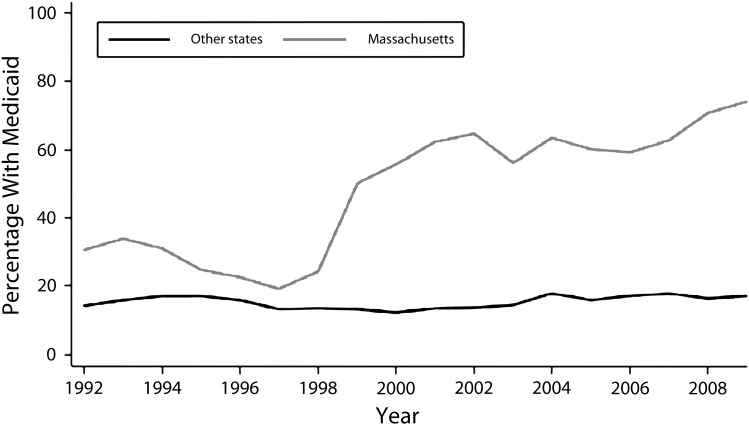
Results of the time-series models are displayed in Table 2. For model 1, which compared trends in Medicaid enrollment among substance use disorder treatment programs in Massachusetts and in the other states combined, the secular trend, before-to-after 1997, and trend after 1997 were all statistically insignificant, suggesting that no significant change developed over time, before or after 1997, when the MassHealth policy was implemented. The state variable was statistically significant (b = 17.19; SE = 5.45; P = .004), demonstrating significant differences between Massachusetts and the other states during the study period. The state * secular trend interaction was not statistically significant, but the state * before-to-after 1997 interaction was significant (b = 25.90; SE = 7.15; P = .001), as was the state * trend after 1997 interaction term (b = 4.33; SE = 1.91; P = .03), suggesting that changes in Medicaid coverage following policy implementation differed between participants in Massachusetts and those in other states (Figure 1).
TABLE 2—
Ordinary Least-Squares Regression Models Comparing Medicaid Enrollment Among Adults Entering Substance Use Disorder Treatment Programs in Massachusetts and in Comparison States Before and After 1997 MassHealth Eligibility Expansion: Treatment Episodes Data Set, 1992–2009
| Independent Variables | b (SE) | P |
| Model 1a | ||
| Constant | 16.55 (3.85) | <.001 |
| Overall secular trend | −0.27 (1.35) | .84 |
| Before-to-after 1997 | −4.69 (5.06) | .36 |
| Trend after 1997 | 1.07 (1.35) | .43 |
| State | 17.19 (5.45) | .004 |
| State * overall secular trend | −2.47 (1.80) | .18 |
| State * before-to-after 1997 | 25.90 (7.15) | .001 |
| State * trend after 1997 | 4.33 (1.91) | .03 |
| Model 2b | ||
| Constant | 35.17 (5.20) | <.001 |
| Overall secular trend | −3.05 (1.72) | .09 |
| Before-to-after 1997 | 20.58 (6.82) | .01 |
| Trend after 1997 | 5.59 (1.82) | .01 |
| Homeless | −8.89 (7.35) | .24 |
| Homeless * overall secular trend | 1.81 (2.43) | .46 |
| Homeless * before-to-after 1997 | 4.00 (9.65) | .68 |
| Homeless * trend after 1997 | −1.45 (2.57) | .58 |
| Model 3c | ||
| Constant | 33.74 (5.35) | <.001 |
| Overall secular trend | −2.73 (1.77) | .14 |
| Before-to-after 1997 | 21.21 (7.02) | .01 |
| Trend after 1997 | 5.40 (1.87) | .01 |
Comparison of change in Medicaid enrollment after 1997 among adults entering substance use disorder treatment programs in Massachusetts and comparison states (combined data from DC and AK, AZ, CO, HI, ID, IL, MD, MO, MT, ND, NE, NH, NJ, NV, PA, TX, and WV).
Comparison of the impact of MassHealth on Medicaid enrollment among homeless and housed adults entering substance use disorder treatment programs in MA.
Nonsignificant interactions removed.
FIGURE 1—
Trends in Medicaid enrollment among adults entering substance use disorder treatment programs in Massachusetts and in other states: Treatment Episode Data Set, 1992–2009.
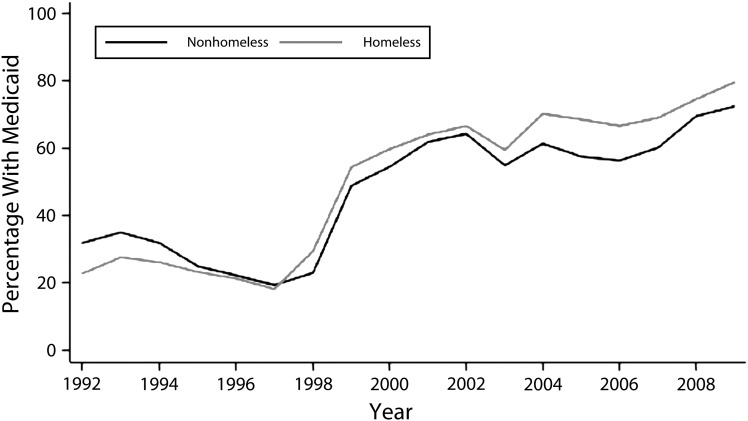
In model 2, which was limited to the state of Massachusetts, none of the interaction terms were statistically significant, indicating that the effect of MassHealth on Medicaid enrollment was similar among the homeless and housed in Massachusetts. Furthermore, we found no differences between the homeless and housed with regard to enrollment. However, the analyses revealed a statistically significant increase in percentage points after policy implementation in both the homeless and housed groups (Figure 2). Because the interaction terms were not statistically significant, we removed them from the final model for estimating the magnitude of change in enrollment after implementation. Results of these analyses demonstrated an average increase of more than 21 percentage points after implementation (b = 21.21; SE = 7.02; P = .01) and an additional average increase of more than 5 percentage points per year (b = 5.40; SE = 1.87; P = .01) following implementation.
FIGURE 2—
Trends in Medicaid enrollment among homeless and housed adults entering substance use disorder treatment programs in Massachusetts before and after implementation of MassHealth program in 1997: Treatment Episode Data Set, 1992–2009.
Medicaid enrollment rates among first admissions in Massachusetts ranged from 13% to 28% prior to the MassHealth policy implementation and reached to as high as 56% during the period after implementation (Appendix A, Table A, available as a supplement to the online version of this article at http://www.ajph.org). When stratified by housing status, enrollment prior to the study ranged from 10% to 21% for homeless admissions and from 13% to 29% for housed admissions. By the end of the study period, 66% of homeless admissions and 55% of housed first admissions were for individuals covered by Medicaid. In other states, enrollment rates ranged from 10% to 15% during the entire study period. Results of the time-series analyses in these first admissions were comparable to the main analysis (Appendix A, Table B, available as a supplement to the online version of this article at http://www.ajph.org). In our comparison of Massachusetts to other states, the state * before-to-after 1997 (b = 16.53; SE = 6.14; P = .01) and state * trend after 1997 (b = 4.69; SE = 1.64; P = .01) terms were both statistically significant (Appendix A, Table B, available as a supplement to the online version of this article at http://www.ajph.org). However, when we compared homeless and housed adults in Massachusetts, we detected no statistically significant interactions. Overall, among first admissions, MassHealth was associated with an increase of more than 13 percentage points in Medicaid enrollment (b = 13.69; SE = 6.07; P = .04) and an additional average increase of more than 5 percentage points for each year after implementation (b = 5.45; SE = 1.62; P = .01), figures that are comparable to the numbers for all participants.
Results of further analyses comparing Massachusetts with 3 comparable states were also consistent with results reported for all states (Appendix B, available as a supplement to the online version of this article at http://www.ajph.org). Prior to implementation of MassHealth, the rates of Medicaid enrollment were 18% to 30% in Illinois, 12% to 23% in Maryland, and 18% to 21% in New Jersey. Following implementation of MassHealth, rates of enrollment were 17% to 29% in Illinois, 11% to 24% in Maryland, and 14% to 23% in New Jersey (Appendix B, Table A, available as a supplement to the online version of this article at http://www.ajph.org). We observed statistically significant state * before-to-after 1997 interactions in comparisons of Massachusetts with Illinois (b = 26.05; SE = 7.34; P = .001), Maryland (b = 20.12; SE = 7.43; P = .01), and New Jersey (b = 24.58; SE = 7.21; P = .002). In addition, we observed a significant state * trend after 1997 interaction in a comparison with New Jersey (b = 4.36; SE = 1.92; P = .03) (Appendix B, Table B, available as an online supplement).
DISCUSSION
We sought to determine whether implementation of the MassHealth program affected homeless adults entering substance use disorder treatment programs in Massachusetts to the same degree as it affected the housed population. Results demonstrated an increase in Medicaid enrollment among the homeless as well as the housed. Overall, the increase in individuals entering substance abuse treatment programs who were Medicare enrollees was more than 21% following implementation, with an additional average increase of more than 5% per year during each of the 12 years after implementation. Our comparison of rates of Medicaid coverage among individuals entering substance abuse treatments in Massachusetts and in other states suggested that the increase in coverage was specific to Massachusetts, providing evidence that the MassHealth policy was the cause of this change.
Homeless and housed adults were equally affected by this policy, a surprising, although encouraging, finding, in light of previous research documenting difficulties enrolling marginalized populations, including homeless adults.16,20–24 However, previous reports that examined Medicaid enrollment in marginalized populations relied on descriptive reports or studies from states other than Massachusetts; no previous large-scale quantitative evaluation of this issue was conducted in Massachusetts. Therefore, our study provides an important contribution to the limited research available.
It is possible that the increased Medicaid enrollment of homeless substance-abusing adults was a result of the outreach initiatives developed to increase ease of enrollment in MassHealth. The state formed collaborations with both community organizations and primary care providers, so that they could inform eligible clients about the program and assist in enrolling them. Similarly, media campaigns specifically targeted newly eligible Massachusetts residents who may have been less likely to know about this policy change. Finally, the state created a toll-free phone number to answer individuals' questions.16 Our findings provide justification for the use of similar outreach initiatives in states that choose to expand their Medicaid programs in 2014.
One of the major strengths of our study was that it included a large sample of homeless adults, a group that is especially difficult to reach but particularly important to study because of the many public health challenges homeless people face.27–30,44 The overall sample from which the data were drawn comprised nearly 960 000 admissions in Massachusetts and more than 6.5 million admissions from other states, increasing the generalizability of our results. Another strength was the interrupted time-series design, which is believed to be among the strongest quasi-experimental methods to estimate effects when randomization is not possible. This method minimizes threats to internal validity, such as maturation and history, and helps to control for preexisting trends in the outcome variable, Medicaid coverage. Although in interrupted time-series studies it is often difficult to separate out the effects of secular trends, we addressed this problem by comparing trends in Massachusetts to those in other states and the District of Columbia combined and in 3 states most similar to Massachusetts in size and other characteristics.39,40
Limitations
The TEDS data set records only individuals entering substance abuse treatment, so our findings may not be generalizable to the general population of Massachusetts or even to substance-abusing adults who are not in treatment. In studies of hard-to-reach populations, those least likely to be surveyed often have more severe problems, which contributes to the difficulties in reaching them.45,46 It is reasonable to assume that individuals entering treatment, particularly those who are homeless, possess a certain level of stability distinguishing them from those who do not enter treatment. Future studies need to examine community samples of homeless substance abusers to assess whether this trend is comparable to our observations in the treatment sample. TEDS is also limited to treatment admissions from facilities that receive federal funding. Many patients may receive substance abuse treatment in other settings, such as general medical or mental health facilities, emergency departments, or private practices. It is possible that our findings will not generalize to recipients of treatment in these other types of facilities. However, with the exception of emergency departments,4 homeless individuals are unlikely to be treated in such facilities. Therefore, this limitation probably did not significantly affect our results.
Expansion of Medicaid was only one of a series of policy initiatives in the State of Massachusetts over the past 2 decades, a notable one being a universal coverage mandate in the middle of the first decade of this century. Although we focused on the 1997 Medicaid expansion, these other policies might well have affected the response to the MassHealth Medicaid expansion and the post-1997 gradual increase in Medicaid enrollment. Unfortunately, the TEDS data did not allow us to examine these potential effects. Furthermore, because of these other initiatives, not all of the observed changes in Medicaid enrollment in Massachusetts can be attributed to the MassHealth Medicaid expansion. Similar Medicaid expansion legislation in other states may not have the same effect as in Massachusetts.
Analyses comparing trends in Massachusetts and trends in other states were limited by the availability of information on health insurance coverage in each state. Consequently, we had data from only 17 other states and the District of Columbia in our analyses, potentially limiting the generalizability of these findings. Finally, the impact of MassHealth and other similar Medicaid expansion programs on Medicaid enrollment of homeless adults was very likely not limited to individuals entering substance abuse treatment. Future research needs to examine the impact of expansion programs on Medicaid enrollment among individuals entering other health services, such as mental health and physical health treatment.
Research Directions
Our study provides the foundation for several future directions for researchers. As more states begin to expand their Medicaid programs, it is important to assess variations across states in enrollment trends. Because Massachusetts has notable differences from many other states that will likely participate in the expansion, homeless adults may not respond to the policy change as successfully as they did in Massachusetts. For example, the National Alliance to End Homelessness estimated that 15 482 individuals experienced homelessness in Massachusetts in 2009, or approximately 23 per 10 000 persons. Prevalence estimates in other states ranged from 7 to 45 per 10 000 persons.47
Furthermore, Massachusetts engaged in aggressive and targeted outreach efforts to enroll marginalized populations, and it is possible that other states will not have the resources or infrastructure necessary to do that. Therefore, studies are necessary to assess the extent to which other states need interventions that increase enrollment and to determine which interventions are most effective for hard-to-reach populations such as homeless adults. For example, it is possible that being able to call a toll-free phone number to receive information may be less helpful for homeless individuals, so greater efforts should be put into other initiatives, such as partnering with community organizations to disseminate information. Therefore, studies are needed to elucidate these differences so that states’ limited resources are used most efficiently. Finally, because enrollment in Medicaid does not guarantee that individuals will enter treatment, research on the relationship between Medicaid coverage and treatment entry among homeless adults is warranted.
Conclusions
Our findings have important public health implications. The expansion of Medicaid in 2014 has been a controversial part of the Affordable Care Act, with opponents suggesting that requiring states to expand their programs violates states’ rights. Twenty-six states filed petitions arguing that this mandate was unconstitutional, and on June 28, 2012, the Supreme Court ruled that states could not be penalized for not expanding their Medicaid programs.37 Consequently, many states will likely decline to participate in the expansion, decreasing the number of substance-abusing homeless adults who will have access to Medicaid coverage and, ultimately, substance abuse treatment and other health services.
Our study provides evidence in favor of state participation in the expansion. Homelessness is a costly problem, partly as a result of the associated increased health care costs, particularly among those with substance use disorders.48–50 Our findings suggest that, if eligible for Medicaid coverage, homeless adults are just as likely as the housed to enroll, which will likely increase their odds of entering treatment, ultimately improving their health status and reducing costs to society.
Acknowledgments
This study was supported by the National Institute on Drug Abuse (grant T32DA007292). The data in the Treatment Episode Data Set (TEDS) system is funded by the US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality.
Human Participant Protection
Institutional review board approval was not necessary because the study was an analysis of secondary data.
References
- 1.US Dept of Health and Human Services. 2013 Poverty guidelines. Available at: http://aspe.hhs.gov/poverty/13poverty.cfm. Accessed May 3, 2013.
- 2.Smith-Campbell B. Emergency department and community health center visits and costs in an uninsured population. J Nurs Scholarsh. 2005;37(1):80–86. doi: 10.1111/j.1547-5069.2005.00011.x. [DOI] [PubMed] [Google Scholar]
- 3.Lowe RA, McConnell KJ, Vogt ME, Smith JA. Impact of Medicaid cutbacks on emergency department use: the Oregon experience. Ann Emerg Med. 2008;52(6):626–634. doi: 10.1016/j.annemergmed.2008.01.335. [DOI] [PubMed] [Google Scholar]
- 4.Ku BS, Scott KC, Kertesz SG, Pitts SR. Factors associated with use of urban emergency departments by the US homeless population. Public Health Rep. 2010;125(3):398–405. doi: 10.1177/003335491012500308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Larson MJ, Saitz R, Horton NJ, Lloyd-Travaglini C, Samet JH. Emergency department and hospital utilization among alcohol and drug-dependent detoxification patients without primary medical care. Am J Drug Alcohol Abuse. 2006;32(3):435–452. doi: 10.1080/00952990600753958. [DOI] [PubMed] [Google Scholar]
- 6.Mann C, Artiga S. The Impact of Recent Changes in Health Care Coverage for Low-Income People: A First Look at the Research Following Changes in Oregon’s Medicaid Program. Washington, DC: Kaiser Family Foundation; 2004. [Google Scholar]
- 7.Moss N, Carver K. The effect of WIC and Medicaid on infant mortality in the United States. Am J Public Health. 1998;88(9):1354–1361. doi: 10.2105/ajph.88.9.1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hanson KW, Neuman P, Dutwin D, Kasper JD. Uncovering the health challenges facing people with disabilities: the role of health insurance. Health Aff (Millwood) 2003 doi: 10.1377/hlthaff.w3.552. (suppl Web exclusives):W3–552–565. [DOI] [PubMed] [Google Scholar]
- 9.Dubay L, Kenney GM. Health care access and use among low-income children: who fares best? Health Aff (Millwood) 2001;20(1):112–121. doi: 10.1377/hlthaff.20.1.112. [DOI] [PubMed] [Google Scholar]
- 10.Goldman DP, Bhattacharya J, McCaffrey DF et al. Effect of insurance on mortality in an HIV-positive population in care. J Am Stat Assoc. 2001;96(455):883–894. [Google Scholar]
- 11.Medicaid Managed Care Cost Savings—A Synthesis of 24 Studies. Falls Church, VA: Lewin Group; 2009. [Google Scholar]
- 12.Dubay L, Holahan J, Cook A. The uninsured and the affordability of health insurance coverage. Health Aff (Millwood) 2007;26(1):w22–w30. doi: 10.1377/hlthaff.26.1.w22. [DOI] [PubMed] [Google Scholar]
- 13.Sommers BD, Tomasi MR, Swartz K, Epstein AM. Reasons for the wide variation in Medicaid participation rates among states hold lessons for coverage expansion in 2014. Health Aff (Millwood) 2012;31(5):909–919. doi: 10.1377/hlthaff.2011.0977. [DOI] [PubMed] [Google Scholar]
- 14.Broaddus M. Childless Adults Who Become Eligible for Medicaid in 2014 Should Receive Standard Benefits Package. Washington, DC: Center on Budget and Policy Priorities; 2010. [Google Scholar]
- 15.Quigley K, Shelto A, Turnbull N. MassHealth: Dispelling Myths and Preserving Progress. Waltham, MA: Massachusetts Health Policy Forum; 2002. [PubMed] [Google Scholar]
- 16.Bovbjerg R, Ullman F. Recent Changes in Health Policy for Low-Income People in Massachusetts. Washington, DC: Urban Institute; 2002. [Google Scholar]
- 17.Zuckerman S, Kenney GM, Dubay L, Haley J, Holahan J. Shifting health insurance coverage, 1997–1999. Health Aff (Millwood) 2001;20(1):169–177. doi: 10.1377/hlthaff.20.1.169. [DOI] [PubMed] [Google Scholar]
- 18.Long SK, Zuckerman S. MassHealth succeeds in expanding coverage for adults. Inquiry. 2004;41(3):268–279. [PubMed] [Google Scholar]
- 19.Long SK, Zuckerman S, Graves JA. Are adults benefiting from state coverage expansions? Health Aff (Millwood) 2006;25(2):w1–w14. doi: 10.1377/hlthaff.25.w1. [DOI] [PubMed] [Google Scholar]
- 20.Ruwe M, Capitman J, Bengiamin M, Soto T. A systematic review and meta-analysis of racial disparities in prenatal care in California: How much? Does insurance matter? Soc Work Public Health. 2010;25(6):550–571. doi: 10.1080/19371910903344217. [DOI] [PubMed] [Google Scholar]
- 21.Feld P, Matlock C, Sandman D. Insuring the Children of New York City’s Low-Income Families: Focus Group Findings on Barriers to Enrollment in Medicaid and Child Health Plus. New York, NY: Commonwealth Fund; 1998. [Google Scholar]
- 22.Stuber J, Kronebusch K. Stigma and other determinants of participation in TANF and Medicaid. J Policy Anal Manage. 2004;23(3):509–530. doi: 10.1002/pam.20024. [DOI] [PubMed] [Google Scholar]
- 23.Post P. Casualties of Complexity: Why Eligible Homeless People Are Not Enrolled in Medicaid. Nashville, TN: National Health Care for the Homeless Council; 2001. [Google Scholar]
- 24.Wood D, Valdez RB. Barriers to medical care for homeless families compared with housed poor families. Am J Dis Child. 1991;145(10):1109–1115. doi: 10.1001/archpedi.1991.02160100041021. [DOI] [PubMed] [Google Scholar]
- 25.Burt M, Aron L, Douglas T, Valente J, Lee E, Iwen B. Homelessness: Programs and the People They Serve. Washington, DC: US Department of Housing and Urban Development; 1999. [Google Scholar]
- 26.Dietz TL. Predictors of reported current and lifetime substance abuse problems among a national sample of US homeless. Subst Use Misuse. 2007;42(11):1745–1766. doi: 10.1080/10826080701212360. [DOI] [PubMed] [Google Scholar]
- 27.Raoult D, Foucault C, Brouqui P. Infections in the homeless. Lancet Infect Dis. 2001;1(2):77–84. doi: 10.1016/S1473-3099(01)00062-7. [DOI] [PubMed] [Google Scholar]
- 28.Badiaga S, Richet H, Azas P et al. Contribution of a shelter-based survey for screening respiratory diseases in the homeless. Eur J Public Health. 2009;19(2):157–160. doi: 10.1093/eurpub/ckn142. [DOI] [PubMed] [Google Scholar]
- 29.Finnie A, Nicolson P. Injecting drug use: implications for skin and wound management. Br J Nurs. 2002;11(6, suppl):S17–S28. doi: 10.12968/bjon.2002.11.Sup1.12246. [DOI] [PubMed] [Google Scholar]
- 30.Austin J, McKellar JD, Moos R. The influence of co-occurring axis I disorders on treatment utilization and outcome in homeless patients with substance use disorders. Addict Behav. 2011;36(9):941–944. doi: 10.1016/j.addbeh.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Hibbs JR, Benner L, Klugman L et al. Mortality in a cohort of homeless adults in Philadelphia. N Engl J Med. 1994;331(5):304–309. doi: 10.1056/NEJM199408043310506. [DOI] [PubMed] [Google Scholar]
- 32.Barrow SM, Herman DB, Córdova P, Struening EL. Mortality among homeless shelter residents in New York City. Am J Public Health. 1999;89(4):529–534. doi: 10.2105/ajph.89.4.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Orwin RG, Scott CK, Arieira C. Transitions through homelessness and factors that predict them: three-year treatment outcomes. J Subst Abuse Treat. 2005;28(suppl 1):S23–S39. doi: 10.1016/j.jsat.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 34.O’Connell MJ, Kasprow W, Rosenheck RA. Rates and risk factors for homelessness after successful housing in a sample of formerly homeless veterans. Psychiatr Serv. 2008;59(3):268–275. doi: 10.1176/ps.2008.59.3.268. [DOI] [PubMed] [Google Scholar]
- 35.Goldfinger SM, Schutt RK, Tolomiczenko GS et al. Housing placement and subsequent days homeless among formerly homeless adults with mental illness. Psychiatr Serv. 1999;50(5):674–679. doi: 10.1176/ps.50.5.674. [DOI] [PubMed] [Google Scholar]
- 36.Bebout RR, Drake RE, Xie H, McHugo GJ, Harris M. Housing status among formerly homeless dually diagnosed adults. Psychiatr Serv. 1997;48(7):936–941. doi: 10.1176/ps.48.7.936. [DOI] [PubMed] [Google Scholar]
- 37. National Federation of Independent Business v Sebelius, 567 U.S. 11–393 (2012)
- 38. Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Treatment episode data set—admissions (TEDS-A) concatenated, 1992 to 2009. Available at: http://www.icpsr.umich.edu/icpsrweb/SAMHDA/series/56. Accessed May 6, 2013.
- 39.Lagarde M. How to do (or not to do)… Assessing the impact of a policy change with routine longitudinal data. Health Policy Plan. 2012;27(1):76–83. doi: 10.1093/heapol/czr004. [DOI] [PubMed] [Google Scholar]
- 40.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 41.Newey WK, West KD. Automatic lag selection in covariance matrix estimation. Rev Econ Stud. 1994;61(4):631–653. [Google Scholar]
- 42.State Health Facts. Washington, DC: Henry J. Kaiser Family Foundation; 2011. [Google Scholar]
- 43.Stata Statistical Software: Release 10.0 [computer program] College Station, TX: Stata Corp LP; 2007. [Google Scholar]
- 44.Faugier J, Sargeant M. Sampling hard to reach populations. J Adv Nurs. 1997;26(4):790–797. doi: 10.1046/j.1365-2648.1997.00371.x. [DOI] [PubMed] [Google Scholar]
- 45.Shield KD, Rehm J. Difficulties with telephone-based surveys on alcohol consumption in high-income countries: the Canadian example. Int J Methods Psychiatr Res. 2012;21(1):17–28. doi: 10.1002/mpr.1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Humphreys K, Harris AHS, Weingardt KR. Subject eligibility criteria can substantially influence the results of alcohol-treatment outcome research. J Stud Alcohol Drugs. 2008;69(5):757–764. doi: 10.15288/jsad.2008.69.757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.State of Homelessness in American 2011. Washington DC: National Alliance to End Homelessness; 2011. [Google Scholar]
- 48.Larimer ME, Malone DK, Garner MD et al. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301(13):1349–1357. doi: 10.1001/jama.2009.414. [DOI] [PubMed] [Google Scholar]
- 49.Poulin SR, Maguire M, Metraux S, Culhane DP. Service use and costs for persons experiencing chronic homelessness in Philadelphia: a population-based study. Psychiatr Serv. 2010;61(11):1093–1098. doi: 10.1176/ps.2010.61.11.1093. [DOI] [PubMed] [Google Scholar]
- 50.Buchholz JR, Malte CA, Calsyn DA et al. Associations of housing status with substance abuse treatment and service use outcomes among veterans. Psychiatr Serv. 2010;61(7):698–706. doi: 10.1176/ps.2010.61.7.698. [DOI] [PubMed] [Google Scholar]