Abstract
Objectives. We sought to determine if reported racial discrimination was associated with medication nonadherence among African Americans with hypertension and if distrust of physicians was a contributing factor.
Methods. Data were obtained from the TRUST project conducted in Birmingham, Alabama, 2006 to 2008. All participants were African Americans diagnosed with hypertension and receiving care at an inner city, safety net setting. Three categories of increasing adherence were defined based on the Morisky Medication Adherence Scale. Trust in physicians was measured with the Hall General Trust Scale, and discrimination was measured with the Experiences of Discrimination Scale. Associations were quantified by ordinal logistic regression, adjusting for gender, age, education, and income.
Results. The analytic sample consisted of 227 African American men and 553 African American women, with a mean age of 53.7 ±9.9 years. Mean discrimination scores decreased monotonically across increasing category of medication adherence (4.1, 3.6, 2.9; P = .025), though the opposite was found for trust scores (36.5, 38.5, 40.8; P < .001). Trust mediated 39% (95% confidence interval = 17%, 100%) of the association between discrimination and medication adherence.
Conclusions. Within our sample of inner city African Americans with hypertension, racial discrimination was associated with lower medication adherence, and this association was partially mediated by trust in physicians. Patient, physician and system approaches to increase “earned” trust may enhance existing interventions for promoting medication adherence.
Hypertension is a leading cause of cardiovascular morbidity and mortality for African Americans.1 Compared with other populations, African Americans are more likely to be diagnosed with hypertension, more likely to have untreated hypertension, and more likely to suffer adverse clinical consequences from uncontrolled hypertension, including myocardial infarction, heart failure, and chronic kidney disease.2 Within the United States, the prevalence of hypertension is 45.7% among African American women and 43.0% among African American men, compared with 31.3% among White women and 33.9% among White men.2 According to the National Health and Nutrition Examination Survey (NHANES), approximately 33% of Whites diagnosed with hypertension have controlled hypertension compared with 28% of African Americans.3
Several common factors contribute to poor hypertension control regardless of race or ethnicity. Although lifestyle changes such as sodium reduction, exercise, and weight loss are important in achieving hypertension control, most patients with stage II hypertension (defined as systolic blood pressure > 160 mmHg or diastolic blood pressure > 100 mmHg) require at least 1 medication.2 Approximately half of the 2 billion prescriptions filled each year are taken incorrectly or not taken at all.4 The inability to afford medications accounts for approximately 40% of the nonadherence found in the general population.5–8 Nonetheless, the existing evidence has shown that when patients are provided access to medication at a reduced cost or at no cost at all, many patients continue to be nonadherent.9
Although medication adherence may be particularly low among patients with hypertension, the existing literature suggests that these differences cannot simply be attributed to socioeconomic status (SES).10,11 Low adherence has likewise been documented to be a critical problem regardless of race or ethnicity.12 Nonetheless, lack of adherence holds particular relevance for African Americans with hypertension because of the prevalence of cardiovascular disease and the levels of morbidity and mortality within this population.
Psychological and social factors, such as health literacy, cultural beliefs, and attitudes toward health care and the health care system, may be critically important determinants of hypertension disparities.13,14 Discrimination based on race or ethnicity is also a powerful social force that affects both health and health behaviors. For example, racial discrimination has been linked to low birth-weight, breast cancer, stress or anxiety disorder, and poor health status.15,16 A study of African American college students found that viewing film clips depicting acts of racism increased cardiovascular reactivity.17 In addition to the immediate cardiovascular effects of discrimination, several studies suggest that chronic exposure to discrimination increases the risk of having uncontrolled blood pressure, although findings are mixed.18
The physiological response to discrimination is well documented. Stressful experiences, such as experiencing discrimination, stimulate the release of cortisol and catecholamines through the activation of the autonomic nervous system. Consistent activation of the autonomic nervous system may contribute to chronically elevated blood pressure, thus predisposing to long-term morbidity and mortality.19
Beyond the physiologic responses resulting from discrimination, the psychological impact has been shown to erode positive health behaviors.16,20–22 Empirical evidence supports the intuitive association of racial discrimination with lower trust in health care providers and the medical system in general.23–25 Furthermore, patients possessing lower trust are less likely to seek health care and thus less likely to follow the instructions of health care providers.26 For example, O’Malley found that lower-income African Americans with distrust in their providers were less adherent to recommended preventive services.25
In spite of the mounting indirect and direct evidence suggesting that racial discrimination may be an important barrier to medication adherence for African Americans with hypertension, we lack a full understanding of this phenomenon and the mediating pathways. Therefore, we examined the association between reported experiences of discrimination and medication adherence within a population of African American patients receiving care in an inner city, safety net setting. In addition, we sought to determine the proportion of the observed relationship between medication adherence and discrimination that could be accounted for by trust in physicians.
METHODS
The TRUST study was a project within the Alabama Collaboration for Cardiovascular Equality (ACCE) program project, funded by the National Heart Lung and Blood Institute from 2006 to 2008. The objectives of the TRUST study were to examine factors such as discrimination, trust, self-efficacy, access to care, and medication adherence among African Americans with hypertension living in the inner city. Study participants were recruited from the Cooper Green Health System, a safety net system (a health system which provides a significant level of care to low-income, uninsured, and vulnerable populations) in Birmingham, Alabama. Most patients at Cooper Green are either uninsured or receiving Medicaid.
The recruitment process began with a list of all patients treated within the past year for hypertension at Cooper Green Health System. Patients were contacted by phone to ascertain preliminary interest in the study. A follow-up visit was scheduled in the clinic for all those expressing initial interest, at which time informed consent was obtained. Recruitment proceeded according to a closely monitored standard protocol.
Survey data were collected through in-person interviews using computer-assisted protocols. We trained, certified, and monitored interviewers for fidelity according to a standardized protocol. The diagnosis of hypertension was ascertained from physician notes in the medical record. Approximately 5% of the medical records were dually abstracted with greater than 95% reliability and validity agreement (interrater reliability) obtained for key variables.
Inclusion and Exclusion Criteria
Eligible participants, who self-reported race or ethnicity as African American, received primary care from Cooper Green Health System for a diagnosis of hypertension recorded in the medical record, were 19 years of age or older, were able to provide informed consent, and were not pregnant (n = 788). Patients were excluded if they did not respond to questions regarding medication adherence, discrimination, or trust (n = 8).
Medication Adherence
The dependent variable for this study was self-reported medication adherence, measured by an adaptation of the 4-item Morisky Medication Adherence Scale.27 The Morisky Medication Adherence Scale consists of the following questions: (1) “Do you ever forget to take your medicine?” (2) “Are you careless at times about taking your medications?” (3) “When you feel better, do you sometimes stop taking your medicine?” and (4)” Sometimes if you feel worse when you take the medicine do you stop taking it?” Each item of the Morisky scale has a dichotomous (yes or no) response option. A score is calculated by assigning 1 point for each response of “no” and 0 points for each response of “yes” and then taking the sum. The resulting scale ranges from 0 to 4, with higher scores indicating better adherence. (Original participant counts from this study in each original category of increasing adherence were 33, 79, 127, 223, and 318.) For this study, we modified the Morisky scale by combining the 2 lowest adherence categories and the 2 middle adherence categories because of low cell counts. Collapsing the categories produced a 3-level adherence variable. The validity of the Morisky scale has been confirmed in several studies, including in studies with only African American participants.27–29
Reported Racial Discrimination
Discrimination was measured using the Experiences of Discrimination (EOD) Scale.30–32 The EOD Scale has 6 subscales that focus respectively on discrimination based on race or ethnicity or color, weight, SES, sexual preference, gender and religion. Only the questions pertaining to racial/ethnic discrimination were included in this study. The race or ethnicity subscale begins with the question, “Have you ever experienced discrimination, were prevented from doing something, hassled or made to feel inferior in any of the following situations because of your race or color?” For the present study, we repeated this question for 7 settings: (1) at school, (2) getting a job, (3) getting housing, (4) at work, (5) at home, (6) seeking medical care, and (7) in public. Each setting received a score of 0 to 3 based on a response of never, rarely, sometimes, or often (scored respectively). Therefore, the EOD Scale ranged from 0 to 21 with a higher score indicating more reported discrimination.
We associated EOD scores with blood pressure levels in a biracial cohort.30 In addition, the EOD Scale was validated among 98 African Americans and 110 Latinos revealing adequate internal consistency and that responses were correlated with psychological distress, smoking, and scores from the Major and Everyday Discrimination scales, suggesting solid construct validity.32
Mediator
We measured trust using the Hall General Trust Scale.33 The Hall Trust Scale consists of 25 questions related to patient trust in their physicians based on 5 domains: (1) caring about the patient’s best interest, (2) physician competence, (3) honesty, (4) confidentiality, and (5) global trust. The Hall General Trust Scale ranges from 11 to 54 with a higher score indicating greater trust. The Hall General Trust scale was validated using a sample that consisted of 67% women and 18% African American.34 We correlated the final instrument with satisfaction, willingness to recommend physician to friends, desire to remain with physician, and lower likelihood of seeking a second opinion. The assessment indicated the scale had high reliability, acceptable item means, and good construct validity.
Covariates
All covariates, including age and gender, were obtained from self-report. Total annual household income was categorized as less than $5000, $5000 to $11 999, $12 000 to $15 999, or $16 000 or more. Education was divided into 4 categories: less than high school, high school, some college, or college degree. Income and education were collected in predefined categories and collapsed into a smaller number of categories because of small participant numbers.
Statistical Analysis
We began by examining distributions and univariate statistics for all variables. Bivariate comparisons used ANOVA for continuous variables (discrimination, age, and trust) and the χ2 test for categorical variables (gender, education, and income) to examine participant characteristic across the main independent variable (level of increasing medication adherence). We set the threshold for statistical significance at P < .05. Ordinal logistic regression was used to examine multivariable relationships, taking the 3-level adherence variable as the outcome.35,36 Therefore, the outcome for the ordinal logistic regression was present in the best adherence category.
We performed mediation analysis with extended techniques from the tradition of Baron and Kenny.37 For dichotomous and categorical outcomes, parameter estimates had to be standardized before comparing across the mediation equations.38 Therefore, the parameter estimates were standardized by multiplying by the standard deviation of the independent variables and dividing by the standard deviation of the outcome variable in the context of the multivariable model. Using this approach, we developed 2 regression models for the mediation analysis, with both models taking the 3-category adherence measure as the outcome. As such, the total association between medication adherence and discrimination (c) was decomposed into a direct effect (c’) and an indirect effect (c – c’) that was assumed to be transmitted through the mediator. We obtained the total effect (c) from the standardized parameter estimate of discrimination, adjusting for age, gender, income, and education. The direct effect (c’) was obtained from the standardized parameter estimate of discrimination, adjusting for age, gender, income, education, and the mediator (trust). Next, we calculated the “mediated proportion” as (c – c’)/c. The mediated proportion approximately represents the proportion of the total effect of the independent variable that is transmitted through the mediator.39 Confidence intervals were generated for the mediated proportion by 1000 replications of the bias-corrected and accelerated bootstrap.40 Statistical analysis was conducted using STATA version 12 (StataCorp, College Station, TX).
We performed 2 sensitivity analyses. First, we repeated the mediation analysis separate for each gender. Second, we reran the main multivariable models adding an interviewer fixed effect.
RESULTS
The analytic sample consisted of 780 African Americans. Of all participants, 553 (71%) were female and the mean (±SD) age was 53 (±9.9) years. Overall, 112 (14%) participants reported low adherence, 350 (45%) reported moderate adherence, and 318 (41%) reported high adherence. Approximately 66% of the participants reported an income of $11 999 or less, yet most (68%) had attended some college. The overall mean (±SD) scores for reported racial discrimination and trust were 3.4 (±4.4) and 39.2 (±8.0), respectively.
Bivariate Analysis
Characteristics of the study participants stratified by medication adherence level are presented in Table 1. Mean discrimination scores decreased monotonically across increasing category of better medication adherence (4.1, 3.6, 2.9; P = .025), although the opposite was found for trust scores (36.5, 38.5, 40.8; P < .001). Women also reported less adherence than did men (P = .018). We found no statistically significant differences in medication adherence for education or income. In addition, we found a significant inverse correlation between trust and discrimination (ρ = –0.33; P < .001).
TABLE 1—
Characteristics of African American Participants With Hypertension by Adherence Level: TRUST Study, Birmingham, AL, 2007–2008
| Adherence Levelsa |
||||
| Variable | Low (n = 112) | Moderate (n = 350) | High (n = 318) | P |
| Discrimination, meanb | 4.05 | 3.58 | 2.88 | .025 |
| Age, mean | 50.79 | 53.58 | 54.83 | < .001 |
| Gender, % | .018 | |||
| Male | 8.81 | 48.02 | 43.17 | |
| Female | 16.64 | 43.58 | 39.78 | |
| Education, % | .315 | |||
| < high school | 14.07 | 46.67 | 39.26 | |
| High school | 21.05 | 42.11 | 36.84 | |
| Some college | 13.82 | 44.74 | 41.45 | |
| College degree | 8.00 | 46.67 | 45.33 | |
| Annual household income, % | .281 | |||
| < $5000 | 16.89 | 48.86 | 34.25 | |
| $5,0000-$11 999 | 14.67 | 43.63 | 41.70 | |
| $12 000-$15 999 | 11.20 | 41.60 | 47.20 | |
| ≥ $16 000 | 11.57 | 47.93 | 40.50 | |
| Trust, meanc | 36.53 | 38.53 | 40.84 | < .001 |
Note. The sample size was 780.
Three-category medication adherence was derived by self-report from the Morisky scale.
The Experiences of Discrimination Scale ranges from 0–21.
The Hall General Trust Scale ranges from 11–54. Higher scores indicate more reported discrimination and greater trust, respectively.
Multivariable and Mediation Analysis
Adjusted associations of reported discrimination and medication adherence are presented in Table 2. Model 1 includes age, gender, education, and income as covariates. Model 2 adds the mediator as an independent variable and includes all covariates from model 1. From model 1, each 1-point increase in reported discrimination reduced the adjusted cumulative odds of being in a better medication adherence category by 6% (odds ratio [OR] = 0.94; 95% confidence interval [CI] = 0.91, 0.97), after accounting for covariates. Greater adherence to medication was associated with increased age (OR = 1.02; 95% CI = 1.01, 1.04), having a college education (OR = 1.86; 95% CI = 1.04, 3.34), and greater income. Women reported lower adherence than did men (OR = 0.64; 95% CI = 0.47, 0.87).
TABLE 2—
Ordinal Logistic Regression Model for the Association Between Reported Discrimination and Medication Adherence Among African American Participants: TRUST Study, Birmingham, AL, 2007–2008
| Model 1 |
Model 2 |
|||
| Variable | Cumulative OR (95% CI) | B | Cumulative OR (95% CI) | B |
| Discriminationa | 0.94 (0.91, 0.97) | −0.145 | 0.96 (0.93, 1.00) | −0.089 |
| Trustb | … | … | 1.04 (1.02, 1.06) | 0.175 |
| Age | 1.02 (1.01, 1.04) | 0.118 | 1.02 (1.01, 1.03) | 0.104 |
| Gender (Ref: male) | 0.64 (0.47, 0.87) | −0.109 | 0.72 (0.52, 0.98) | −0.080 |
| Education (Ref: < high school) | ||||
| High school | 0.79 (0.48, 1.31) | −0.043 | 0.74 (0.45, 1.23) | −0.056 |
| Some college | 1.26 (0.85, 1.85) | 0.060 | 1.26 (0.86, 1.87) | 0.061 |
| College degree | 1.86 (1.04, 3.34) | 0.099 | 2.01 (1.12, 3.63) | 0.110 |
| Annual household income, $ (Ref: < 5000) | ||||
| 5000–11 999 | 1.31 (0.93, 1.85) | 0.070 | 1.31 (0.92, 1.85) | 0.067 |
| 12 000–15 999 | 1.62 (1.05, 2.48) | 0.097 | 1.61 (1.05, 2.48) | 0.095 |
| ≥ 16 000 | 1.23 (0.80, 1.90) | 0.042 | 1.20 (0.78, 1.85) | 0.036 |
Note. CI = confidence interval; OR = odds ratio. The sample size was 724. Three-category medication adherence was derived by self-report from the Morisky scale.
The Krieger Experiences of Discrimination Scale ranges from 0–21.
bThe Hall General Trust Scale ranges from 11–54. Higher scores indicate more reported discrimination and greater trust, respectively.
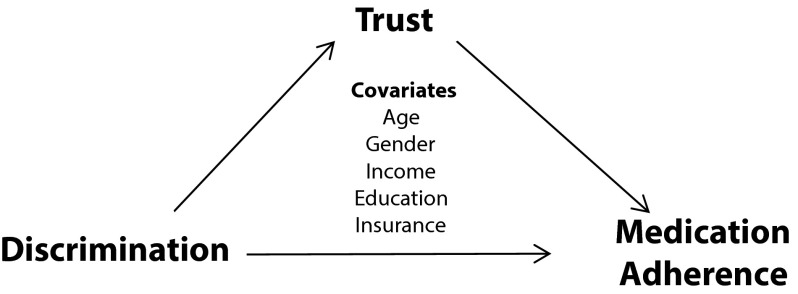
Model 2 revealed that the association between racial discrimination and medication adherence was reduced in magnitude and statistical significance after trust was introduced as the mediator. Each 1-point increase in trust increased the cumulative odds of being in better medication adherence category by 4% (OR = 1.04; 95% CI = 1.02, 1.06), after adjusting for reported discrimination and other covariates. We used standardized parameter estimates from Table 2 to calculate the mediated proportion (Figure 1), indicating that trust explained 39% (95% CI = 17%, 100%) of the association between discrimination and medication adherence.
FIGURE 1—
Mediation triangle depicting the association between discrimination and medication adherence with trust as a mediator.
Note. Total effect: c = –0.145. Direct effect: c’ = –0.089. Mediated proportion: (c- c’)/c = 39%. Effects are from standardized parameter estimates. Bias-corrected and accelerated bootstrap 95% confidence interval for mediated proportion = 17%, 100%.
Sensitivity Analysis
As a sensitivity analysis, we repeated the mediation analysis stratified by gender and found no important differences. More specifically, among women only, approximately 39% of the relationship between discrimination and medication adherence was influenced by trust, compared with 28% for men (P < .05 for both). In a final sensitivity analysis we reran the 2 main multivariable models presented in Table 2 after including the interviewer as a fixed effect, which did not substantively alter any of the findings.
DISCUSSION
In this sample of African American primary care patients with hypertension followed in an inner city, safety net setting, racial discrimination was associated with lower medication adherence. We associated high adherence with increased age, male gender, and greater reported trust in physicians. In general, more education was associated with better adherence, although a gradient was not observed and statistical significance was not present for all levels of education, perhaps because of the limited socioeconomic range found within this sample. Importantly, we found that general trust in physicians explained a substantial portion of the association between reported discrimination and medication adherence.
Our main findings are consistent with several reports in the scientific literature, including a previous report limited to African American men from this same sample.41 In that study greater trust in physicians was associated with better medication adherence. A systematic review by our group examined the association between hypertension and racial discrimination which revealed a preponderance of evidence linking racial discrimination with greater risk of hypertension and less likelihood of attaining control of hypertension once diagnosed.18 Providing insight into a potential mechanism through which discrimination may be translated into worse hypertension control, Van Houtven et al. found that racial discrimination was associated with delays in filling prescriptions among 522 African American, White, and Latino patients living in Durham County, North Carolina.16 A recent meta-analysis concluded that discrimination was associated with worse physical and mental health as well as less participation in healthy behaviors.42
Although there is ample evidence linking racial discrimination with adverse health outcomes such as hypertension, the picture is not completely consistent. For example, in the systematic review by our group, null studies were limited by measurement problems, such as floor or ceiling effects, and small sample sizes.18 For example, Peters reported no association between racism and hypertension among 162 African American adults.43 As a possible explanation for the lack of association, the authors noted that the majority of their study participants, including those that were previously diagnosed with hypertension, were normotensive. Kressin et al. recently conducted a study assessing blood pressure among African American and White patients with hypertension receiving care at an inner city, safety net setting.44 Unexpectedly, the authors found patients endorsing the sentiment that they would receive better care if they were a different race also had better rates of controlled blood pressure. Nonetheless, we believe that the preponderance of evidence suggests that experiencing discrimination may lead to worse hypertension control.
Understanding the psychological mechanisms through which racial discrimination manifests may suggest new intervention approaches. Several related studies have addressed the importance of a trusting relationship between the provider and the patient. For example, Piette et al. found that among a population of lower-income veterans, those with lower trust in physicians were more likely to underuse medications in response to cost pressures.45 There are also physiological effects of experiencing discrimination, and numerous studies have indicated a significant association between discrimination and cardiovascular reactivity and elevated blood pressure.46–49
Historical mistreatment of African Americans seeking care has contributed to mistrust seen among African Americans.50 Boulware et al. found that African American participants reported less trust in their physicians compared with Whites and attributed this difference to underlying fears of experiencing bigotry.51 Supporting this hypothesis, Schulman et al. found that physicians were less likely to refer African American actors for cardiac evaluation for chest pain.52 Other studies provide evidence of provider bias53–56 and have reviewed the importance of physician bias in the delivery of health care.57,58 The patient may recognize the unintentional bias of a provider and thus have reduced trust in that provider. A physician may feel that minorities are less likely to adhere to treatment and may take a fatalistic approach toward their patients. This may be perceived by the patient as a lack of concern or interest in their well-being, thus creating a self-fulfilling prophecy.23,59 Together with our findings, these reports provide a firm foundation for the assertion that trust is a potent mediator though which racial discrimination may lead to adverse health outcomes.
It is also worth noting that the African American women reported lower medication adherence than their male counterparts. Selective enrollment of men who had higher adherence rates could provide a potential explanation for this finding. Another potential explanation for this finding is that the female participants may have placed more priority on the health care needs of the rest of the family rather than attending to their own condition.60 In a community-based survey, Wiltshire et al. reported that African American women reported fewer unmet medical needs although they had significantly lower global health status,61 likewise suggesting that African American women may prioritize the needs of their family at the expense of their own health.
However, findings about gender and medications adherence in the literature are not consistent. For example, a study by Holt et al. found no significant difference in adherence to antihypertensive medications by gender.62 Braverman and Dedier examined the relationship between antihypertensive medication adherence with sociodemographic constructs in a sample of 70 African Americans with hypertension and found that men were more likely to have low adherence.60 Hyre found that African American men with hypertension were less likely to be adherent to antihypertensive medications compared with African American women, White women, or White men.63 In spite of these complexities present in the literature on gender and medication adherence, we found that trust mediated a similar proportion of the association between discrimination and medication adherence for both genders.
Limitations
Although we relied on self-report to ascertain the main outcome of medication adherence, we used an instrument that has been well validated for African Americans with hypertension.27,64 Nonetheless, we cannot account for patients who underreport or overreport medication adherence or the possibility that patients who are more adherent to medication may be more likely to participate in the study. In addition, other factors that may potentially influence medication adherence were not examined. Such factors include the number of years from initial diagnoses with hypertension, stress, depression, social support, and racial concordance between the patient and physician.65–68
The mean discrimination score in our sample was relatively low, suggesting possible underreporting of discrimination. However, our findings are similar to other reports in the literature.69–72 Our measure of discrimination was not specific to the health care setting, did not consider institutional and structural racism, did not capture racial “microaggressions” experienced by patients from physicians, and did not account for underreporting because of the perception that interviewers were affiliated with the medical system.
Entry criteria for the study included a single entry of hypertension in the medical record, but this diagnosis was not further verified. Furthermore, a recent study found the positive predictive value of a hypertension diagnosis recorded in an electronic health record to be approximately 84%.73 We cannot determine with certainty that our sample was representative of the full population. Post-hoc analysis of administrative data found that of all patients seeking treatment from 2009 to 2011, approximately 60% were female, compared with our sample of which 71% were female. Because men are underrepresented in our sample, it is reasonable to question if men with lower adherence were less likely to participate, thereby accounting for the higher adherence rates found among men compared with women.
Furthermore, our study sample was recruited in Birmingham, Alabama, and thus our results may not be generalizable to African Americans in other regions of the United States. This study is cross sectional and we cannot draw cause-and-effect inference. For example, it is possible that rather than the experience of discrimination causing nonadherence, both the experience of discrimination and nonadherence could be related to a common, underlying personality phenotype.
Implications
Promoting medication adherence remains a formidable task for clinicians, those interested in improving population health, and those interested in reducing health disparities. A recent systematic review commissioned by the Agency for Healthcare Research and Quality found that several interventions to improve medication adherence are supported by credible evidence.74 However, the panel noted that because most effect sizes were only modest, additional innovative work was needed to enhance the effectiveness of these known approaches to improving medication adherence. Furthermore, the panel noted that there was a paucity of studies that addressed medication adherence interventions for patients who are vulnerable because of race/ethnicity or SES.
Our findings suggest that interventions to improve medication could be enhanced by incorporating trust-building components. Such a focus on trust fits well within a recent synthesis of conceptual models for behavior change that centers on ability, opportunity, and motivation.75
For example, focusing on the patient–physician relationship in a culturally competent manner might enhance adherence among African Americans.76 In addition, strategies to promote “earned trust” in the medical system77 may offer powerful adjuncts to medication adherence interventions. Although we found lower adherence rates among women, trust was equally potent among both genders as a mediator of the association between reported discrimination and low adherence. Therefore, it is reasonable to anticipate that such strategies to promote “earned trust” would be effective among both men and women.
Conclusions
We found that racial discrimination was associated with decreased medication adherence within our sample of low-income African Americans. Furthermore, a substantial fraction of this association was tempered by trust in physicians. We hope that our findings will encourage researchers to more deeply explore the psychosocial determinants of medication adherence and to develop novel enhancements to more traditional interventions that address this important cause of health disparities.
Acknowledgments
This research was funded by a Dissertation Grant from Agency for Healthcare Research and Quality (R36 HS020755-01), and the TRUST study was funded by a grant from the National Heart, Lung, and Blood Institute (U01 HL079171-01). Support was also provided by the Center for Health Equality and Intervention Research (CHEIR) at the University of Massachusetts Medical School, funded by the National Institute on Minority Health and Health Disparities (1P60MD006912).
Human Participant Protection
The TRUST study was approved by institutional review boards at the University of Alabama at Birmingham and Cooper Green. The present study was also approved by the institutional review board at the University of Massachusetts Medical School.
References
- 1.Flack JM, Ferdinand KC, Nasser SA. Epidemiology of hypertension and cardiovascular disease in African Americans. J Clin Hypertens (Greenwich) 2003;5(1, suppl 1):5–11. doi: 10.1111/j.1524-6175.2003.02152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 3.Roger VL, Go AS, Lloyd-Jones DM et al. Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation. 2011;125(1):e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dunbar-Jacob J, Erlen JA, Schlenk EA, Ryan CM, Sereika SM, Doswell WM. Adherence in chronic disease. Annu Rev Nurs Res. 2000;18:48–90. [PubMed] [Google Scholar]
- 5.Kressin NR, Wang F, Long J et al. Hypertensive patients’ race, health beliefs, process of care, and medication adherence. J Gen Intern Med. 2007;22(6):768–774. doi: 10.1007/s11606-007-0165-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogedegbe G, Harrison M, Robbins L, Mancuso CA, Allegrante JP. Barriers and facilitators of medication adherence in hypertensive African Americans: a qualitative study. Ethn Dis. 2004;14(1):3–12. [PubMed] [Google Scholar]
- 7.Turner BJ, Hollenbeak C, Weiner MG, Ten Have T, Roberts C. Barriers to adherence and hypertension control in a racially diverse representative sample of elderly primary care patients. Pharmacoepidemiol Drug Saf. 2009;18(8):672–681. doi: 10.1002/pds.1766. [DOI] [PubMed] [Google Scholar]
- 8.Chan M. Reducing cost-related medication nonadherence in patients with diabetes. 2010. Available at: http://dbt.consultantlive.com/diabetes-management/content/article/1145628/1554670. Accessed September 5, 2013.
- 9.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA. 2003;290(2):199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 10.Odedosu T, Schoenthaler A, Vieira DL, Agyemang C, Ogedegbe G. Overcoming barriers to hypertension control in African Americans. Cleve Clin J Med. 2012;79(1):46–56. doi: 10.3949/ccjm.79a.11068. [DOI] [PubMed] [Google Scholar]
- 11.Rose LE, Kim MT, Dennison CR, Hill MN. The contexts of adherence for African Americans with high blood pressure. J Adv Nurs. 2000;32(3):587–594. doi: 10.1046/j.1365-2648.2000.01538.x. [DOI] [PubMed] [Google Scholar]
- 12.Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA. 2006;296(21):2563–2571. doi: 10.1001/jama.296.21.joc60162. [DOI] [PubMed] [Google Scholar]
- 13.Bosworth HB, Oddone EZ. A model of psychosocial and cultural antecedents of blood pressure control. J Natl Med Assoc. 2002;94(4):236–248. [PMC free article] [PubMed] [Google Scholar]
- 14.Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19(4):357–362. doi: 10.1097/01.hco.0000126978.03828.9e. [DOI] [PubMed] [Google Scholar]
- 15.Mustillo S, Krieger N, Gunderson EP, Sidney S, McCreath H, Kiefe CI. Self-reported experiences of racial discrimination and Black-White differences in preterm and low-birthweight deliveries: the CARDIA Study. Am J Public Health. 2004;94(12):2125–2131. doi: 10.2105/ajph.94.12.2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Houtven CH, Voils CI, Oddone EZ et al. Perceived discrimination and reported delay of pharmacy prescriptions and medical test. J Gen Intern Med. 2005;20:578–583. doi: 10.1111/j.1525-1497.2005.0123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Armstead CA, Lawler KA, Gorden G, Cross J, Gibbons J. Relationship of racial stressors to blood pressure responses and anger expression in black college students. Health Psychol. 1989;8(5):541–556. doi: 10.1037//0278-6133.8.5.541. [DOI] [PubMed] [Google Scholar]
- 18.Cuffee YL, Hargraves JL, Allison J. Exploring the association between reported discrimination and hypertension among African Americans: a systematic review. Ethn Dis. 2012;22(4):422–431. [PubMed] [Google Scholar]
- 19.Charkoudian N, Rabbitts JA. Sympathetic neural mechanisms in human cardiovascular health and disease. Mayo Clin Proc. 2009;84(9):822–830. doi: 10.4065/84.9.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burgess DJ. The association between perceived discrimination and underutilization of needed medical and mental health care in a multi-ethnic community sample. J Health Care Poor Underserved. 2008;19:894–911. doi: 10.1353/hpu.0.0063. [DOI] [PubMed] [Google Scholar]
- 21.Collins JW, Jr, David RJ, Handler A, Wall S, Andes S. Very low birthweight in African American infants: the role of maternal exposure to interpersonal racial discrimination. Am J Public Health. 2004;94(12):2132–2138. doi: 10.2105/ajph.94.12.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hausmann LR, Jeong K, Bost JE, Ibrahim SA. Perceived discrimination in health care and use of preventive health services. J Gen Intern Med. 2008;23(10):1679–1684. doi: 10.1007/s11606-008-0730-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greer TM. Perceived racial discrimination in clinical encounters among African American hypertensive patients. J Health Care Poor Underserved. 2010;21(1):251–263. doi: 10.1353/hpu.0.0265. [DOI] [PubMed] [Google Scholar]
- 24.Jacobs EA, Rolle I, Ferrans CE, Whitaker EE, Warnecke RB. Understanding African Americans’ views of the trustworthiness of physicians. J Gen Intern Med. 2006;21(6):642–647. doi: 10.1111/j.1525-1497.2006.00485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.O’Malley AS. The role of trust in use of preventive services among low-income African-American women. Prev Med. 2004;38:777–785. doi: 10.1016/j.ypmed.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 26.Halbert CH, Armstrong K, Gandy OH, Jr, Shaker L. Racial differences in trust in health care providers. Arch Intern Med. 2006;166(8):896–901. doi: 10.1001/archinte.166.8.896. [DOI] [PubMed] [Google Scholar]
- 27.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Erickson SR, Coombs JH, Kirking DM, Azimi AR. Compliance from self-reported versus pharmacy claims data with metered-dose inhalers. Ann Pharmacother. 2001;35(9):997–1003. doi: 10.1345/aph.10379. [DOI] [PubMed] [Google Scholar]
- 29.Ogedegbe G, Schoenthaler A, Richardson T et al. An RCT of the effect of motivational interviewing on medication adherence in hypertensive African Americans: rationale and design. Contemp Clin Trials. 2007;28(2):169–181. doi: 10.1016/j.cct.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 30.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA Study of young Black and White adults. Am J Public Health. 1996;86(10):1370–1378. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krieger N, Sidney S, Coakley E. Racial discrimination and skin color in the CARDIA study: implications for public health research. Coronary Artery Risk Development in Young Adults. Am J Public Health. 1998;88(9):1308–1313. doi: 10.2105/ajph.88.9.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61(7):1576–1596. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 33.Hall MA, Zheng B, Dugan E et al. Measuring patients’ trust in their primary care providers. [erratum appears in Med Care Res Rev. 2003;60(1):118.] Med Care Res Rev. 2002;59(3):293–318. doi: 10.1177/1077558702059003004. [DOI] [PubMed] [Google Scholar]
- 34.Hall MA, Camacho F, Dugan E, Balkrishnan R. Trust in the medical profession: conceptual and measurement issues. Health Serv Res. 2002;37(5):1419–1439. doi: 10.1111/1475-6773.01070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cole SR, Ananth CV. Regression models for unconstrained, partially or fully constrained continuation odds ratios. Int J Epidemiol. 2001;30(6):1379–1382. doi: 10.1093/ije/30.6.1379. [DOI] [PubMed] [Google Scholar]
- 36.Williams R. Generalized ordered logit/partial proportional odds models for ordinal dependent variables. Stata J. 2006;6(1):58–82. [Google Scholar]
- 37.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 38.MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev. 1993;17:144–158. [Google Scholar]
- 39.Hafeman DM. “Proportion explained”: a causal interpretation for standard measures of indirect effect? Am J Epidemiol. 2009;170(11):1443–1448. doi: 10.1093/aje/kwp283. [DOI] [PubMed] [Google Scholar]
- 40.Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. 2002;7(4):422–445. [PubMed] [Google Scholar]
- 41.Elder K, Ramamonjiarivelo Z, Wiltshire J et al. Trust, medication adherence, and hypertension control in southern African American men. Am J Public Health. 2012;102(12):2242–5. doi: 10.2105/AJPH.2012.300777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Peters RM. Racism and hypertension among African Americans. West J Nurs Res. 2004;26(6):612–631. doi: 10.1177/0193945904265816. [DOI] [PubMed] [Google Scholar]
- 44.Kressin NR, Orner MB, Manze M, Glickman ME, Berlowitz D. Understanding contributors to racial disparities in blood pressure control. Circ Cardiovasc Qual Outcomes. 2010;3(2):173–180. doi: 10.1161/CIRCOUTCOMES.109.860841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Piette JD, Heisler M, Krein S, Kerr EA. The role of patient-physician trust in moderating medication nonadherence due to cost pressures. Arch Intern Med. 2005;165(15):1749–1755. doi: 10.1001/archinte.165.15.1749. [DOI] [PubMed] [Google Scholar]
- 46.Guyll M, Matthews KA, Bromberger JT. Discrimination and unfair treatment: relationship to cardiovascular reactivity among African American and European American women. Health Psychol. 2001;20(5):315–325. doi: 10.1037//0278-6133.20.5.315. [DOI] [PubMed] [Google Scholar]
- 47.Harrell JP, Hall S, Taliaferro J. Physiological responses to racism and discrimination: an assessment of the evidence. Am J Public Health. 2003;93(2):243–248. doi: 10.2105/ajph.93.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fang CY, Myers HF. The effects of racial stressors and hostility on cardiovascular reactivity in African American and Caucasian men. Health Psychol. 2001;20(1):64–70. doi: 10.1037//0278-6133.20.1.64. [DOI] [PubMed] [Google Scholar]
- 49.Merritt MM, Bennett GG, Jr, Williams RB, Edwards CL, Sollers JJ., 3rd Perceived racism and cardiovascular reactivity and recovery to personally relevant stress. Health Psychol. 2006;25(3):364–369. doi: 10.1037/0278-6133.25.3.364. [DOI] [PubMed] [Google Scholar]
- 50.Gamble VN. Under the shadow of Tuskegee: African Americans and health care. Am J Public Health. 1997;87(11):1773–1778. doi: 10.2105/ajph.87.11.1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Rep. 2003;118(4):358–365. doi: 10.1016/S0033-3549(04)50262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schulman KA, Berlin JA, Harless W et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340(8):618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 53.Green AR, Carney DR, Pallin DJ et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22(9):1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Penner LA, Dovidio JF, West TV et al. Aversive Racism and Medical Interactions with Black Patients: A Field Study. J Exp Soc Psychol. 2010;46(2):436–440. doi: 10.1016/j.jesp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sabin J, Nosek BA, Greenwald A, Rivara FP. Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. J Health Care Poor Underserved. 2009;20(3):896–913. doi: 10.1353/hpu.0.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.White-Means S, Zhiyong D, Hufstader M, Brown LT. Cultural competency, race, and skin tone bias among pharmacy, nursing, and medical students: implications for addressing health disparities. Med Care Res Rev. 2009;66(4):436–455. doi: 10.1177/1077558709333995. [DOI] [PubMed] [Google Scholar]
- 57.Fincher C, Williams JE, MacLean V, Allison JJ, Kiefe CI, Canto J. Racial disparities in coronary heart disease: a sociological view of the medical literature on physician bias. Ethn Dis. 2004;14(3):360–371. [PubMed] [Google Scholar]
- 58.Santry HP, Wren SM. The role of unconscious bias in surgical safety and outcomes. Surg Clin North Am. 2012;92(1):137–151. doi: 10.1016/j.suc.2011.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Soc Sci Med. 2000;50(6):813–828. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- 60.Braverman J, Dedier J. Predictors of medication adherence for African American patients diagnosed with hypertension. Ethn Dis. 2009;19(4):396–400. [PubMed] [Google Scholar]
- 61.Wiltshire JC, Person SD, Kiefe CI, Allison JJ. Disentangling the influence of socioeconomic status on differences between African American and White women in unmet medical needs. Am J Public Health. 2009;99(9):1659–1665. doi: 10.2105/AJPH.2008.154088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Holt E, Joyce C, Dornelles A et al. Sex differences in barriers to antihypertensive medication adherence: findings from the cohort study of medication adherence among older adults. J Am Geriatr Soc. 2013;61(4):558–564. doi: 10.1111/jgs.12171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hyre AD, Krousel-Wood MA, Muntner P, Kawasaki L, DeSalvo KB. Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting. J Clin Hypertens. 2007;9(3):179–186. doi: 10.1111/j.1524-6175.2007.06372.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008;10(5):348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 65.Schoenthaler A, Allegrante JP, Chaplin W, Ogedegbe G. The effect of patient-provider communication on medication adherence in hypertensive Black patients: does race concordance matter? Ann Behav Med. 2012;43(3):372–382. doi: 10.1007/s12160-011-9342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter? J Gen Intern Med. 2010;25(11):1172–1177. doi: 10.1007/s11606-010-1424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schoenthaler A, Chaplin WF, Allegrante JP et al. Provider communication effects medication adherence in hypertensive African Americans. Patient Educ Couns. 2009;75(2):185–191. doi: 10.1016/j.pec.2008.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Konrad TR, Howard DL, Edwards LJ, Ivanova A, Carey TS. Physician-patient racial concordance, continuity of care, and patterns of care for hypertension. Am J Public Health. 2005;95(12):2186–2190. doi: 10.2105/AJPH.2004.046177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Halanych JH, Safford MM, Shikany JM et al. The association between income, education, and experiences of discrimination in older African American and European American patients. Ethn Dis. 2011;21(2):223–229. [PMC free article] [PubMed] [Google Scholar]
- 70.Taylor TR, Williams CD, Makambi KH et al. Racial discrimination and breast cancer incidence in US Black women: the Black Women’s Health Study. Am J Epidemiol. 2007;166(1):46–54. doi: 10.1093/aje/kwm056. [DOI] [PubMed] [Google Scholar]
- 71.Gee GC, Ryan A, Laflamme DJ, Holt J. Self-reported discrimination and mental health status among African descendants, Mexican Americans, and other Latinos in the New Hampshire REACH 2010 Initiative: the added dimension of immigration. Am J Public Health. 2006;96(10):1821–1828. doi: 10.2105/AJPH.2005.080085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Noh S, Kaspar V. Perceived discrimination and depression: moderating effects of coping, acculturation, and ethnic support. Am J Public Health. 2003;93(2):232–238. doi: 10.2105/ajph.93.2.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.de Burgos-Lunar C, Salinero-Fort MA, Cardenas-Valladolid J et al. Validation of diabetes mellitus and hypertension diagnosis in computerized medical records in primary health care. BMC Med Res Methodol. 2011;11:146–157. doi: 10.1186/1471-2288-11-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Medication Adherence Interventions: Comparative Effectiveness. Closing the Quality Gap: Revisiting the State of the Science: Evidence Report No. 208 (AHRQ Publication No. 12-E010-1) Rockville, MD: Agency for Healthcare Quality and Research; 2012. [PMC free article] [PubMed] [Google Scholar]
- 75.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42–53. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.van Ryn M, Saha S. Exploring unconscious bias in disparities research and medical education. JAMA. 2011;306(9):995–996. doi: 10.1001/jama.2011.1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.US Department of Health and Human Services, National Committee on Vital and Health Statistics; 2011. The Community as a Learning System: Using Local Data to Improve Local Health. [Google Scholar]