Abstract
Porcine small intestinal submucosa (SIS [Oasis®]) is an acellular, biological extracellular matrix (ECM) that has been found to significantly improve the healing of difficult-to-heal or chronic wounds in humans. Like dermal ECM, SIS contains collagen, elastin, glycosaminoglycans, proteoglycans, and growth factors that play important roles in healing. Preclinical studies have shown that numerous cell types attach to SIS, proliferate and migrate into the matrix, and differentiate. In addition, SIS can reduce the activity of matrix metalloproteinases (MMPs)—endogenous proteolytic enzymes whose levels and activities are increased in chronic wounds. Compared to the original single-layer SIS, multi-layer SIS has stronger mechanical properties and is more slowly degraded in wounds. Together, these SIS products provide flexibility in the selection of biologically-active ECMs that may be useful for the repair of diverse wound types.
Keywords: Small intestinal submucosa, SIS, extracellular matrix, burn, chronic wounds
Introduction
Chronic wounds affect millions of Americans and cost the country more than $50 billion annually [1,2]. These wounds can dramatically reduce quality of life, causing pain, impairing mobility, interfering with everyday activities, and, in some cases, leading to amputation [3-5]. Although standard of care is effective for some patients, 40-60% of chronic ulcers remain unhealed after 3 or more months of treatment [6,7].
The molecular environment of chronic wounds exhibits numerous changes that impede healing. High levels of inflammatory cytokines are associated with chronic inflammation [8], and high levels of matrix metalloproteinases (MMPs) degrade extracellular matrix (ECM) [9,10]. Degradation of the ECM interferes with the dynamic and reciprocal cell-ECM interactions that are essential in every step of wound healing.
Porcine small intestinal submucosa (SIS)—an acellular, biological ECM (see Figure 1)—has been applied to chronic wounds in an attempt to address the ECM deficits and stimulate the cell-ECM interactions that are necessary for healing to occur. In randomized, controlled trials, SIS has been found to significantly increase the percentage of wounds healed and healing rate compared to standard of care alone [11-13]. These clinical findings are buttressed by a plethora of preclinical research investigating the biochemical and biomechanical features of SIS. In this review, we summarize the preclinical findings related to the basic properties of SIS, comparing the single-layer and triple-layer SIS constructs where data are available.
Figure 1.
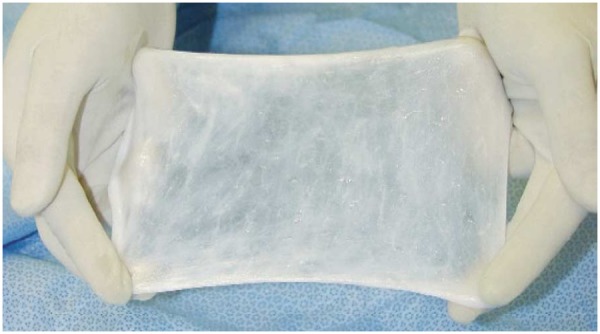
SIS material stretched after being wetted.
Structural and biochemical properties of SIS
The structural properties and biochemical composition of SIS have been well studied, as documented in Table 1. Porcine SIS ranges in thickness from 0.05 to 0.22 mm [14] and has a variable, porous microstructure with pores ranging from 20 to 30 μm [15,16] that enables the oxygen diffusion necessary for maintaining cell proliferation and viability. Androjna et al. determined the oxygen diffusion coefficients of SIS to be 7 × 10-6 - 2 × 10-5 cm2/s [17]. The same analyses showed that the oxygen diffusion coefficients of engineered ECMs, human dermis (Alloderm®) and canine fascia lata were 1.9 - 3.1 x 10-5 cm2/s and 1.6 - 4 x 10-5 cm2/s [17].
Table 1.
Structural Properties and Biochemical Composition of Porcine SIS
| Property | Description |
|---|---|
| Thickness | 0.05 to 0.22 mm [14] |
| Ultrastructure | Pores varying from 20 to 30 μm [17] |
| Mechanical strength [40] | 1 layer: 20.6 MPa (dry) and 7.2 MPa (wet) |
| 2 layer: 24.7 MPa (dry) and 18.8 MPa (wet) | |
| 3 layer: 31.2 MPa (dry) and 22.0 MPa (wet) | |
| 4 layer: 36.7 MPa (dry) and 22.4 MPa (wet) | |
| Suture Retention [40] | 1 layer: 0.5 N (dry) and 0.7 N (wet) |
| 2 layer: 1.3 N (dry) and 2.6 N (wet) | |
| 3 layer: 2.1 N (dry) and 4.1 N (wet) | |
| 4 layer: 2.8 N (dry) and 5.2 N (wet) | |
| Oxygen diffusion coefficient | 7 x 10-6 - 2 x 10-5 cm2/s [17] |
| Fiber structure | Single, continuous preferred fiber direction, parallel to the long axis of the intestine [41] |
| Biochemical composition | Collagen [18,21] |
| Elastin [18] | |
| Fibronectin [19,20] | |
| Laminin [20] | |
| Glycosaminoglycans and proteoglycans [21,22] | |
| Fibroblast growth factor-2 (FGF-2) [27] | |
| Transforming growth factor-beta1 (TGF-β1) [26] | |
| Vascular endothelial growth factor (VEGF) [27] |
Like dermal extracellular matrix, SIS is primarily composed of type I collagen fibers (see the fibrous construct in Figure 2), but also contains minor amounts of elastin and collagen types III, IV, and VI [18]. Multidomain glycoproteins such as fibronectin [19,20] and laminin [20], which mediate cell adhesion to the extracellular matrix, have been identified in SIS. Additionally, SIS contains glycosaminoglycans and proteoglycans [21,22] that provide cell attachment and growth factor binding sites, sequester matrix-degrading enzymes, and enhance cellular infiltration into injured tissue [23-25]. SIS has also been reported to release growth factors including fibroblast growth factor-2 (FGF-2), transforming growth factor-beta1 (TGF-β1), and vascular endothelial growth factor (VEGF) [21,26,27].
Figure 2.

Microstructure of SIS material (Optical microscopy, 10X, dry).
Mechanisms of SIS effects on cellular growth and differentiation
In vivo, cells and ECM exhibit continuous, bidirectional interactions that have been termed dynamic reciprocity [28]. These interactions occur in response to alterations in the cellular microenvironment and under homeostatic conditions, as well as during tissue repair, angiogenesis, embryogenesis, and malignant transformation [29]. For example, changes in the microenvironment (e.g., due to tissue damage) may induce changes in cellular gene expression which then alter the extracellular matrix leading to further alterations in gene expression and cytoskeletal properties.
Cells interact with endogenous ECM largely through integrin binding. The mechanism by which cells interact with SIS presumably also involves integrin binding. Hodde et al. evaluated the peptide sequences within fibronectin that may be important in adherence of cells to SIS [30]. Results with human microvascular endothelial cells showed that the RCG and REDV played a role in the attachment to SIS, suggesting that the binding of integrins to these sequences in SIS may mediate cell attachment. Badylak et al. found that attachment of human microvascular endothelial cells to SIS depended on both its composition and architecture [31]. In addition, Hurst et al. reported that neutralization of beta 1, beta 4, and alpha 6 integrins altered the adhesion of bladder cancer cells to SIS [32], suggesting the importance of these integrin subunits in cell attachment.
Hodde et al. has conducted several studies to investigate the release of growth factors from SIS and resultant effects on cell differentiation and angiogenesis in vitro [33,34]. A neutralizing antibody against FGF-2 inhibited the differentiation of PC12 cells induced by SIS, [34] raising the possibility that FGF-2 may contribute to the biological response to SIS in vivo. Similarly, neutralizing antibodies against VEGF blocked the ability of SIS to induce tube formation from human microvascular endothelial cells in a fibrin-based angiogenesis assay [33].
Matrix metalloproteinases interacting with SIS
Various studies have reported the presence of high MMP levels and activity in chronic wound fluid [35,36]. Excess levels of MMPs found in chronic wounds are believed to be a key contributor to wound chronicity; thus, reducing elevated levels of MMPs in chronic wounds may promote healing.
Clinical evidence supporting this hypothesis was provided by Trengove and colleagues [35], who reported that levels of proteases decreased as chronic venous ulcers began to heal, and by Ladwig and colleagues [37], who reported that optimal healing of chronic pressure ulcers correlated with low values of the ratio of MMP-9/tissue inhibitor of metalloproteinases-1 (TIMP-1). Thus, control of MMP levels may improve the poor healing conditions found in chronic wounds.
Shi et al. conducted several studies to investigate the interaction between SIS and MMPs [38]. MMP-1, MMP-2, and MMP-9 displayed different binding affinities, indicated by a loss of activity in solution upon incubation with SIS of 53.8%, 85.9%, and 36.9%, respectively, over 24 hours. A human keratinocyte cell migration study was conducted to evaluate the effects of MMPs and SIS-treated MMP solutions on cell migration. These data indicated that MMPs inhibit keratinocyte migration in vitro, and that the inhibition can be significantly reduced by pre-incubating the MMP solution with SIS. Similar activity was seen in vivo using a diabetic mouse wound healing model. Biopsy samples were collected on days 3 and 7 following wounding for analysis of MMP levels by gelatin zymography. MMP activity was found to be maximally attenuated by SIS treatment on Day 3. On Day 7 the attenuation became less significant, indicating that the MMP binding ability of SIS had become saturated [38]. Overall, results with these models indicate that SIS reduces MMP activity immediately after application and reduces the inhibitory effects of MMP-1, MMP-2, and MMP-9 on keratinocyte migration.
Enzymatic degradation study of SIS with different thicknesses
To enhance the utility of SIS in different clinical situations, the SIS constructs have been designed with different thicknesses. These constructs consist of 1, 2, 3, or 4 layers of SIS matrix (see Figure 3). An in vitro study was designed to determine the relative degradability of the four SIS thicknesses in a proteolytic solution containing collagenases, neutral protease, and other proteases designed to mimic a wound environment [14]. After incubation for two hours at 37 °C, the residue dry weight of SIS was used for calculating the level of degradation.
Figure 3.

Section pictures showing thickness comparison for one, two, three, and four layer SIS constructs (dry).
Results demonstrated that degradation of the product was inversely proportional to the number of layers [14]. The 1-layer matrix was about 82% digested under the test conditions. The 2-layer matrix lost 75% of its weight, slightly less than the one layer matrix when tested under the same conditions. Significantly less degradation was found for the 3-layer (49%) and 4-layer (47%) matrices, indicating that the higher number of layers will likely increase the material’s durability and reduces its susceptibility to enzymatic degradation. However, the thickness effect became less significant as seen between 3 and 4 layer materials, indicating that at certain levels of thickness, the degradation will saturate.
Durability of SIS in pig wounds and diabetic mouse wounds
SIS materials become incorporated into the wound bed over time, with some wounds requiring repeated applications to achieve closure. Based on the results obtained in proteolytic solutions, multiple-layer SIS would be expected to persist longer in the wound bed than single layer SIS.
The incorporation of different-thickness SIS materials in vivo was evaluated in porcine and mouse wound pilot studies [39]. In the pig model, 1-layer SIS and 3-layer SIS were applied to burn wounds after debridement. Four days after application, the 1-layer SIS was visibly incorporated while substantial unincorporated 3-layer SIS matrix remained. All wounds formed a soft eschar surface layer over the course of the study making accurate visual evaluation of incorporation impossible later in the study.
Biopsy samples were taken from two wounds for each treatment, 10 and 17 days after SIS application. Histology demonstrated that 1-layer SIS had incorporated at the wound surface by day 10, while 3-layer SIS samples still exhibited distinct layers not yet incorporated into the wound bed. At day 17, all four SIS-treated samples displayed some degree of reepithelialization, while one of two control samples exhibited no reepithelialization [39].
In the diabetic mouse model, 1-layer SIS and 3-layer SIS were applied to full-thickness wounds on the day of wounding and 3 days later. Inspection of the wounds over time demonstrated that the 1-layer SIS largely or fully incorporated into treated wounds, while the 3-layer SIS had significant unincorporated layers [39]. These studies suggest that one benefit of increasing SIS matrix thickness may be the need for less frequent application.
Comparison of mechanical properties between SIS with different matrix layers
Mechanical properties of the 1-, 2-, 3-, and 4-layer SIS constructs were also compared [40]. The thickness of one layer is approximately 50 μm. The ultimate tensile strength, elastic modulus, elongation, and suture retention strength were determined in both wet and dry conditions. When tested in dry conditions, peak strength increased with the number of layers (Table 1). However, as the number of layers increased, the more the material elongated. The elastic modulus differed little between the SIS materials, suggesting that they all have similar material stress-strain characteristics.
Compared to the dry test, the wet peak stress was lower for all materials, with the 1-layer SIS sample being significantly lower than the multi-layer samples [40]. However, no statistically significant difference was found between the multi-layer samples. Under wet conditions, elongation was inversely related to number of layers and peak stress. The 1-layer SIS elongated the most (~130%), while all multi-layer SIS elongated 30-40%.
Elastic modulus under wet conditions also differed from the dry results. A higher modulus was measured for each increasing layer. For the suture retention test, the wet conditions provided higher retention strength. Both wet and dry samples displayed the same trend that more layers in the material resulted in greater suture retention strength (Table 1).
Conclusions
SIS is a well-studied biomaterial that significantly improves the healing of chronic wounds [11]. As a naturally-occurring ECM, SIS supports the adherence, proliferation, migration, and differentiation of numerous cell types. The bioactivity of SIS includes releasing growth factors, minimizing the destructive activity of MMPs, and inducing angiogenesis to support new blood vessel in growth. SIS is biodegradable and can be well incorporated into tissue. Recently, studies have demonstrated that the new multi-layer SIS has stronger mechanical properties and is more slowly degraded in wounds than single-layer SIS. Thus, the multi-layer SIS combines the known beneficial properties of SIS with increased durability to meet the needs for repair of diverse tissues and wounds.
Acknowledgements
The authors acknowledge the assistance of Dr. Mary Ann Chapman and Mrs. Renée Carstens in the editing of this manuscript.
Disclosure of conflict of interest
None.
Trademark statement
OASIS® and OASIS® Ultra are registered trademarks of Cook Biotech, Inc.
References
- 1.Fife CE, Carter MJ, Walker D, Thomson B. Wound care outcomes and associated cost among patients treated in US outpatient wound centers: data from the US Wound Registry. Wounds. 2012;24:10–17. [PubMed] [Google Scholar]
- 2.Brem H, Kirsner RS, Falanga V. Protocol for the successful treatment of venous ulcers. Am J Surg. 2004;188:1–8. doi: 10.1016/S0002-9610(03)00284-8. [DOI] [PubMed] [Google Scholar]
- 3.Nabuurs-Franssen MH, Huijberts MS, Nieuwenhuijzen Kruseman AC, Willems J, Schaper NC. Health-related quality of life of diabetic foot ulcer patients and their caregivers. Diabetologia. 2005;48:1906–10. doi: 10.1007/s00125-005-1856-6. [DOI] [PubMed] [Google Scholar]
- 4.Persoon A, Heinen MM, van der Vleuten CJ, de Rooij MJ, van de Kerkhof PC, van Achterberg T. Leg ulcers: a review of their impact on daily life. J Clin Nurs. 2004;13:341–354. doi: 10.1046/j.1365-2702.2003.00859.x. [DOI] [PubMed] [Google Scholar]
- 5.Ramsey SD, Newton K, Blough D, McCulloch DK, Sandhu N, Reiber GE, Wagner EH. Incidence, outcomes, and cost of foot ulcers in patients with diabetes. Diabetes Care. 1999;22:382–7. doi: 10.2337/diacare.22.3.382. [DOI] [PubMed] [Google Scholar]
- 6.Veves A, Falanga V, Armstrong DG, Sabolinski ML. Graftskin, a human skin equivalent, is effective in the management of noninfected neuropathic diabetic foot ulcers: a prospective randomized multicenter clinical trial. Diabetes Care. 2001;24:290–295. doi: 10.2337/diacare.24.2.290. [DOI] [PubMed] [Google Scholar]
- 7.Marston WA, Hanft J, Norwood P, Pollak R. The efficacy and safety of Dermagraft in improving the healing of chronic diabetic foot ulcers: results of a prospective randomized trial. Diabetes Care. 2003;26:1701–1705. doi: 10.2337/diacare.26.6.1701. [DOI] [PubMed] [Google Scholar]
- 8.Pradhan L, Cai X, Wu S, Andersen ND, Martin M, Malek J, Guthrie P, Veves A, Logerfo FW. Gene expression of pro-inflammatory cytokines and neuropeptides in diabetic wound healing. J Surg Res. 2011;167:336–342. doi: 10.1016/j.jss.2009.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nwomeh BC, Liang HX, Cohen IK, Yager DR. MMP-8 is the predominant collagenase in healing wounds and nonhealing ulcers. J Surg Res. 1999;81:189–195. doi: 10.1006/jsre.1998.5495. [DOI] [PubMed] [Google Scholar]
- 10.Grinnell F, Ho CH, Wysocki A. Degradation of fibronectin and vitronectin in chronic wound fluid: analysis by cell blotting, immunoblotting, and cell adhesion assays. J Invest Dermatol. 1992;98:410–416. doi: 10.1111/1523-1747.ep12499839. [DOI] [PubMed] [Google Scholar]
- 11.Mostow EN, Haraway GD, Dalsing M, Hodde JP, King D. Effectiveness of an extracellular matrix graft (OASIS Wound Matrix) in the treatment of chronic leg ulcers: a randomized clinical trial. J Vasc Surg. 2005;41:837–843. doi: 10.1016/j.jvs.2005.01.042. [DOI] [PubMed] [Google Scholar]
- 12.Romanelli M, Dini V, Bertone M, Barbanera S, Brilli C. OASIS wound matrix versus Hyaloskin in the treatment of difficult-to-heal wounds of mixed arterial/venous aetiology. Int Wound J. 2007;4:3–7. doi: 10.1111/j.1742-481X.2007.00300.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Romanelli M, Dini V, Bertone MS. Randomized comparison of OASIS wound matrix versus moist wound dressing in the treatment of difficult-to-heal wounds of mixed arterial/venous etiology. Adv Skin Wound Care. 2010;23:34–38. doi: 10.1097/01.ASW.0000363485.17224.26. [DOI] [PubMed] [Google Scholar]
- 14.Mewaldt R, Shi L, Carson D. Enzymatic degradation study of single layer and multi-layer small intestinal submucosa (SIS) matrices; Poster presented as part of the Wound Healing Society Annual Meeting; 2011 Apr. 14-17; Dallas, TX. [Google Scholar]
- 15.Badylak SF, Lantz GC, Coffey A, Geddes LA. Small intestinal submucosa as a large diameter vascular graft in the dog. J Surg Res. 1989;47:74–80. doi: 10.1016/0022-4804(89)90050-4. [DOI] [PubMed] [Google Scholar]
- 16.Nihsen ES, Johnson CE, Hiles MC. Bioactivity of small intestinal submucosa and oxidized regenerated cellulose/collagen. Adv Skin Wound Care. 2008;21:479–86. doi: 10.1097/01.ASW.0000323561.14144.19. [DOI] [PubMed] [Google Scholar]
- 17.Androjna C, Gatica JE, Belovich JM, Derwin KA. Oxygen diffusion through natural extracellular matrices: implications for estimating “critical thickness” values in tendon tissue engineering. Tissue Eng Part A. 2008;14:559–69. doi: 10.1089/tea.2006.0361. [DOI] [PubMed] [Google Scholar]
- 18.US Pharmacopoeia, Inc. USP Monographs: Small Intestinal Submucosa Wound Matrix. Available at: http://www.pharmacopoeia.com.cn/v29240/usp29nf24s0_m541.html. Accessed July 15, 2011.
- 19.McPherson TB, Badylak SF. Characterization of fibronectin derived from porcine small intestinal submucosa. Tissue Eng Part A. 1998;4:75–83. [Google Scholar]
- 20.Lindberg K, Badylak SF. Porcine small intestinal submucosa (SIS): a bioscaffold supporting in vitro primary human epidermal cell differentiation and synthesis of basement membrane proteins. Burns. 2001;27:254–266. doi: 10.1016/s0305-4179(00)00113-3. [DOI] [PubMed] [Google Scholar]
- 21.Hurst RE, Bonner RB. Mapping of the distribution of significant proteins and proteoglycans in small intestinal submucosa by fluorescence microscopy. J Biomater Sci Polym Ed. 2001;12:1267–1279. doi: 10.1163/156856201753395798. [DOI] [PubMed] [Google Scholar]
- 22.Hodde JP, Badylak SF, Brightman AO, Voytik-Harbin SL. Glycosaminoglycan content of small intestinal submucosa: a bioscaffold for tissue replacement. Tissue Eng. 1996;2:209–217. doi: 10.1089/ten.1996.2.209. [DOI] [PubMed] [Google Scholar]
- 23.Mulloy B, Rider CC. Cytokines and proteoglycans: an introductory overview. Biochem Soc Trans. 2006;34:409–413. doi: 10.1042/BST0340409. [DOI] [PubMed] [Google Scholar]
- 24.Baum CL, Arpey CJ. Normal cutaneous wound healing: clinical correlation with cellular and molecular events. Dermatol Surg. 2005;31:674–86. doi: 10.1111/j.1524-4725.2005.31612. discussion 686. [DOI] [PubMed] [Google Scholar]
- 25.Gallo RL. Proteoglycans and cutaneous vascular defense and repair. J Investig Dermatol Symp Proc. 2000;5:55–60. doi: 10.1046/j.1087-0024.2000.00008.x. [DOI] [PubMed] [Google Scholar]
- 26.McDevitt CA, Wildey GM, Cutrone RM. Transforming growth factor-beta1 in a sterilized tissue derived from the pig small intestine submucosa. J Biomed Mater Res A. 2003;67:637–640. doi: 10.1002/jbm.a.10144. [DOI] [PubMed] [Google Scholar]
- 27.Voytik-Harbin SL, Brightman AO, Kraine MR, Waisner B, Badylak SF. Identification of extractable growth factors from small intestinal submucosa. J Cell Biochem. 1997;67:478–491. [PubMed] [Google Scholar]
- 28.Bissell MJ, Aggeler J. Dynamic reciprocity: how do extracellular matrix and hormones direct gene expression? Prog Clin Biol Res. 1987;249:251–62. [PubMed] [Google Scholar]
- 29.Nelson CM, Bissell MJ. Of extracellular matrix, scaffolds, and signaling: tissue architecture regulates development, homeostasis, and cancer. Annu Rev Cell Dev Biol. 2006;22:287–309. doi: 10.1146/annurev.cellbio.22.010305.104315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hodde J, Record R, Tullius R, Badylak S. Fibronectin peptides mediate HMEC adhesion to porcine-derived extracellular matrix. Biomaterials. 2002;23:1841–8. doi: 10.1016/s0142-9612(01)00310-6. [DOI] [PubMed] [Google Scholar]
- 31.Badylak S, Liang A, Record R, Tullius R, Hodde J. Endothelial cell adherence to small intestinal submucosa: an acellular bioscaffold. Biomaterials. 1999;20:2257–2263. doi: 10.1016/s0142-9612(99)00156-8. [DOI] [PubMed] [Google Scholar]
- 32.Hurst RE, Kyker KD, Bonner RB, Bowditch RD, Hemstreet GP 3rd. Matrix-dependent plasticity of the malignant phenotype of bladder cancer cells. Anticancer Res. 2003;23:3119–28. [PMC free article] [PubMed] [Google Scholar]
- 33.Hodde JP, Record RD, Liang HA, Badylak SF. Vascular endothelial growth factor in porcine-derived extracellular matrix. Endothelium. 2001;8:11–24. doi: 10.3109/10623320109063154. [DOI] [PubMed] [Google Scholar]
- 34.Hodde JP, Hiles MC. Bioactive FGF-2 in sterilized extracellular matrix. Wounds. 2001;13:195–201. [Google Scholar]
- 35.Trengove NJ, Stacey MC, MacAuley S, Bennett N, Gibson J, Burslem F, Murphy G, Schultz G. Analysis of the acute and chronic wound environments: the role of proteases and their inhibitors. Wound Repair Regen. 1999;7:442–452. doi: 10.1046/j.1524-475x.1999.00442.x. [DOI] [PubMed] [Google Scholar]
- 36.Wysocki AB. Wound fluids and the pathogenesis of chronic wounds. J Wound Ostomy Continence Nurs. 1996;23:283–290. doi: 10.1016/s1071-5754(96)90047-9. [DOI] [PubMed] [Google Scholar]
- 37.Ladwig GP, Robson MC, Liu R, Kuhn MA, Muir DF, Schultz GS. Ratios of activated matrix metalloproteinase-9 to tissue inhibitor of matrix metalloproteinase-1 in wound fluids are inversely correlated with healing of pressure ulcers. Wound Repair Regen. 2002;10:26–37. doi: 10.1046/j.1524-475x.2002.10903.x. [DOI] [PubMed] [Google Scholar]
- 38.Shi L, Ramsay S, Ermis R, Carson D. In vitro and in vivo studies on matrix metalloproteinases interacting with small intestine submucosa wound matrix. Int Wound J. 2012;9:44–53. doi: 10.1111/j.1742-481X.2011.00843.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tetens S, Ramsay S, Roche E, Carson D. Greater persistence of a novel small intestinal submucosa matrix in wounds; Poster presented as part of the Wound Healing Society Annual Meeting; 2011 April 14-17; Dallas, TX. [Google Scholar]
- 40.Ermis R, Shi L, Carson D. Comparison of mechanical properties between small intestinal submucosa (SIS) with varying layers; Poster presented as part of the Wound Healing Society Annual Meeting; 2011 April 14-17; Dallas, TX. [Google Scholar]
- 41.Hodde J, Janis A, Ernst D, Zopf D, Sherman D, Johnson C. Effects of sterilization on an extracellular matrix scaffold: part I. Composition and matrix architecture. J Mater Sci Mater Med. 2007 Apr;18:537–43. doi: 10.1007/s10856-007-2300-x. [DOI] [PubMed] [Google Scholar]


