Abstract
Background
Little is known about recovery of female sexual function following an acute myocardial infarction (MI). Interventions to improve sexual outcomes in women are limited.
Methods and Results
Semistructured, qualitative telephone interviews were conducted with 17 partnered women (aged 43 to 75 years) purposively selected from the Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status Registry to deepen knowledge of recovery of female sexual function following an acute myocardial infarction (MI) and to improve sexual outcomes in women. Sixteen women had a monogamous relationship with a male spouse; 1 had a long‐term female partner. Most women resumed sexual activity within 4 weeks of their MI. Sexual problems and concerns were prevalent, including patient and/or partner fear of “causing another heart attack.” Few women received counseling about sexual concerns or the safety of returning to sex. Most women who discussed sex with a physician initiated the discussion themselves. Inquiry about strategies to improve sexual outcomes elicited key themes: need for privacy, patient‐centeredness, and information about the timing and safe resumption of sexual activity. In addition, respondents felt that counseling should be initiated by the treating cardiologist, who “knows whether your heart is safe,” and then reinforced by the care team throughout the rehabilitation period.
Conclusions
Partnered women commonly resume sexual activity soon after an MI with fear but without directed counseling from their physicians. Proactive attention to women's concerns related to sexual function and the safety of sexual activity following an MI could improve post‐MI outcomes for women and their partners.
Keywords: aging, myocardial infarction, outcomes, sex, women
Introduction
Interventions to improve myocardial infarction (MI) outcomes have significantly affected the survival of the acute event.1–3 As a result, the vast majority of people with MI (>80% in US and European studies) survive to 1 year.4–7 Longer‐term outcomes are less well documented, especially in the domain of sexual function. Survivors of MIs value sexuality as an important aspect of health and quality of life,8 and satisfaction with sexual life has been associated with a reduced risk of incident coronary heart disease.9
Recent guidelines from the American College of Cardiology and the American Heart Association recommend that physicians counsel patients about resuming sexual activity following an MI.10–11 Similar guidelines for MI management from the European Society of Cardiology provide general recommendations around the timing of resumption of sexual activity.12 Cardiac rehabilitation guidelines include identification and management of sexual dysfunction,13 yet evidence‐based strategies to improve sexual outcomes following an MI, especially in women, are very limited.
The Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status Registry (TRIUMPH) is a multisite, prospective, longitudinal study that followed patient outcomes for 12 months after MI hospitalization. Analysis of TRIUMPH data previously showed that a majority of men (74%) and 44% of women were sexually active in the year before their MIs, and many continued to be sexually active in the year after.14 However, only 47% of men and 35% of women reported receiving counseling about resuming sexual activity after an MI. Those who were not counseled on discharge were significantly less likely to be sexually active 1 year later; the magnitude of this effect was more pronounced in women.
This qualitative substudy of female TRIUMPH participants who were sexually active in the year before MI was conducted to expand on quantitative findings from the larger TRIUMPH Study. Specifically, this study aimed to more fully understand female sexual recovery following an MI and to inform design of an evidence‐based strategy to improve female sexual outcomes after MI.
Methods
Sample and Setting
The TRIUMPH study design has been previously described.14–15 This qualitative substudy enrolled women from the TRIUMPH Registry who reported sexual activity in the year before MI. Purposive random sampling was used to select patients from the TRIUMPH Registry to enroll approximately equal numbers from 3 age groups (55 to 64, 65 to 74, and 75+ years). All participants were interviewed within 18 months of completing the TRIUMPH study (mean, 12 months) or within 30 months of their MIs (mean, 24 months). This study was approved by the Institutional Review Board of Saint Luke's Hospital in Kansas City (TRIUMPH Study Coordinating Center) and the University of Chicago. All participants provided informed consent.
Procedure
A semistructured interview guide (Data S1) was developed to complement data generated through the large‐scale, multisite TRIUMPH Registry, which used closed‐coded surveys (items administered with a finite set of predetermined response options) to generate quantitative observations.14 This substudy was designed to gain contextualized, patient‐driven understanding of communication and counseling about sexuality after an MI and to elicit themes related to the desired features of an effective intervention to address sexual outcomes following an MI.
Domains of inquiry were developed with expertise from an interdisciplinary research team (a nurse with clinical and research expertise in cardiology [C.D.], a psychologist [L.G.], a public health researcher with clinical and research knowledge about female sexuality [E.M.A.], a medical anthropologist [B.G.], and a gynecologist with clinical and survey research expertise in female sexuality in the context of aging and disease [S.T.L.]) and triangulation with quantitative results from the TRIUMPH Registry and a thorough review of the literature (Table 1). The team was supported by the TRIUMPH Study's statistician, who identified the sampling frame (K.G.), and 2 cardiologists and outcomes researchers (H.M.K., J.A.S.), who reviewed the coding and analysis process used by the team and contributed to the rigor of the interpretation, the process for data reduction, and the conclusions drawn. Data obtained from participants’ TRIUMPH baseline interviews were used to characterize sociodemographic and other health characteristics.
Table 1.
Qualitative Interview Guide Domains and Example Items
| Domains | Example Primary and Secondary Items |
|---|---|
| Health | |
| Self‐reported health | Over the last 4 weeks, would you say your health is excellent, very good, good, fair, or poor? |
| Comorbidities | How was your health before the heart attack? |
| Time since MI | About how long ago was your heart attack? |
| Pre‐MI sexuality | |
| Quality of sex life | How would you describe your sex life before your heart attack? |
| Sexual problems (patient and partner) | Thinking back to the 12 months before your heart attack, has there ever been a period of several months or more when you were not interested in sex or were having difficulties with sex? ● How bothered were you by these problems? ● Had your partner (spouse) been having any difficulties with sex in the 12 months prior to your heart attack? |
| Post‐MI sexuality | |
| Resumption and quality of relationship | Thinking about the time after your heart attack, how would you describe your sex life? ● When did you begin to have sexual activity again? ● Have you noticed any differences in your sexual relationship since your heart attack? ● Why haven't you been sexually active since your heart attack? |
| Sexual problems (patient and partner) | Thinking back to the time since your heart attack, has there ever been a period of several months or more when you were not interested in sex or were having difficulties with sex? ● How bothered were you by these problems? ● Was your partner (spouse) having any difficulties with sex at that time? ● How bothered were you by his/her problems? |
| Motivation | People have sex for different reasons; what are the reasons that you have sex? |
| Satisfaction | How satisfied are you with how things are going with your sex life now? ● How do you think your partner (spouse) feels? ● What could be better about your sex life? |
| Impact of MI on sexual life | Have you noticed any differences in your sexual relationship since your heart attack? ● Do you sense any reluctance or hesitation? ● Have you noticed any differences in the kinds of sexual activities, in the frequency or the intensity of the activities you do? ● Do you have any worries about having sex since your heart attack? |
| Communication | |
| Physician–patient discussion | Has your doctor ever talked to you about sex after having a heart attack? ● If yes, tell me about that discussion. ● If no, why do you think that is? ● What kind of information would you have liked to have about this topic? |
| Intervention | |
| Initiation | Who would you prefer to talk with about resuming sexual activity? |
| Context | Where would be an optimal setting for physicians to deliver this information? |
| Timing | When do you think it would be the most appropriate time to talk to women? |
| Content | What kind of information do you think women would want to know regarding their sex life after a heart attack? |
MI indicates myocardial infarction.
A recruitment letter was mailed to eligible participants that asked for participation and included instructions on how to decline participation. Two experienced qualitative researchers (B.G., L.G.; 1 male, 1 female) conducted the interviews using the same script and interview guidelines. Interviews were serially completed to reach theme saturation (n=17); this occurred when information gained from participants became redundant and additional interviews provided no new insights.16
Audio‐recorded telephone interviews, averaging 25 minutes, were transcribed verbatim and coded, allowing the researchers to assess the added value of each interview until theme saturation occurred. Individual respondents’ quotes are noted by a randomly generated number “x,” noted as Rx; age “y” is notated in years Ay. Further deidentification was accomplished by assigning variation to respondents’ age by randomly adjusting by an integer between −2 and 2.
Data Analysis
Transcripts were coded by an interdisciplinary team; this was important for establishing the construct validity17 of the coding scheme. An initial taxonomy was created to establish consistency in coding across interviews and by coders to achieve consensus; this taxonomy is reflected in the domains of the interview guide. All transcripts were individually coded by 6 members of the research team (E.M.A., C.D., B.G., L.G., K.G., and S.T.L.) and exchanged for final reconciliation. Grounded theory, a common theoretical framework used in qualitative data analysis, was employed to systematically analyze the data and, using inductive reasoning, to develop concepts central to informing the design of an intervention.18 Content analysis, a qualitative research methodology used to analyze and interpret both apparent and latent content, was used to search for patterns and themes that occurred frequently in a single interview or across interviews (units of analyses) and resulted in categorical codes.19 Text was organized by domain and coded with a theme and keyword identifiers. Themes emerged in response to primary and secondary items and prompts within relevant domains (see Table 1). Themes were iterated until consensus was reached among the coders. In addition to the transcribed interviews, data sources included team meeting notes, e‐mails, and field/phone notes, which were collected, reviewed, and integrated throughout the content analysis period. This documented the taxonomy evolution and construction of the coding schema. The audit trail was periodically reviewed as the team moved to consensus of the final domains and themes. Any conclusions drawn from the qualitative data were reviewed in the context of the entire data set with the goal of finding discrepant information. Conclusions were modified if discrepancies were found. The cardiologists provided additional review of the content analysis and conclusions for face validity and to reduce the possibility of researcher bias or faulty clinical logic. Transcripts and codes were entered into an electronic data analysis program (ATLAS.ti GmbH, Berlin, Germany).
Results
Specific themes emerged that detailed respondent characteristics, sexuality and recovery, issues related to resumption of sexual activity, patient–physician communication about sexual activity, and the initiation, context, timing, and content of an intervention to improve sexual outcomes following an MI.
Cooperation, Demographic, and Health Characteristics
Cooperation and refusal rates are summarized in Figure 1. Of 30 eligible female TRIUMPH patients who could be contacted, 17 were interviewed. Two interviews were discontinued by the interviewer because the respondent was too ill. Only 1 of 11 respondents who declined participation had refused the sexuality items in the larger TRIUMPH Study 12‐month interview. Refusal rates among women who were contacted by the male interviewer were slightly higher than those for the female interviewer (8 and 3, respectively); however, no woman explicitly stated that participation or refusal was based on interviewer gender.
Figure 1.
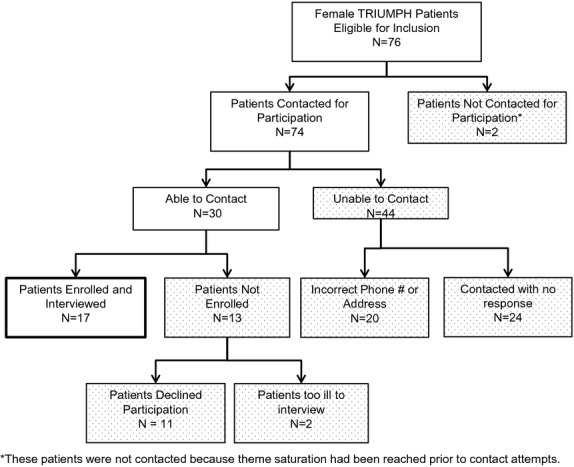
TRIUMPH qualitative interview enrollment flow chart. TRIUMPH indicates Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status.
Respondent characteristics are summarized in Table 2. Median age of participants was 60 years (range, 43 to 75 years), consistent with the age distribution in the TRIUMPH Registry. Sixteen women were married, and 1 reported a long‐term same‐sex relationship. Most respondents had a current romantic partner. Self‐reported health at the time of the interview was generally rated as good to very good. Common comorbidities included diabetes (n=4) and “stress” (n=4). Four women said their partners had heart disease or a history of MI.
Table 2.
Characteristics of TRIUMPH Qualitative Interview Respondents (n=17)*
| Demographics | |
| Age, (y), median (range) | 58 (43 to 75) |
| 40 to 49 | 5/17 |
| 50 to 59 | 4/17 |
| 60+ | 8/17 |
| Married | 16/17 |
| Race/ethnicity* | |
| White | 15/17 |
| Black or African American | 2/17 |
| Health characteristics | |
| Post‐MI self‐reported health | |
| Excellent/very good/good | 12/16 |
| Fair/poor | 4/16 |
| Length of time since MI* | |
| 20 to 24 months | 10/17 |
| 25 to 29 months | 7/17 |
| Menopausal** | 13/17 |
| Depression** | 9/17 |
| GRACE risk score ≥89** | 9/17 |
| Sexuality | |
| Current romantic partner | 10/10 |
| Resumed sex following MI | 16/17 |
| Length of time to resume sex following MI | |
| Never | 1/14 |
| Within 1 month | 8/14 |
| More than 1 month | 4/14 |
TRIUMPH indicates Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status; MI, myocardial infarction.
Displayed as n/# of respondents of whom the question was asked.
Taken from respondents’ TRIUMPH baseline interview.
Menopausal status determined dichotomously (Y/N).
Depression assessed using the Patient Health Questionnaire (PHQ‐9).20
Elements of the Global Registry of Acute Coronary Events (GRACE) risk score were prospectively collected at baseline and used to describe the severity of patients’ MIs based on their predicted 6‐month mortality.21
Pre‐ and Post‐MI Sexuality: Perceived Importance, Quality, and Recovery
Women were asked to reflect on their sexual life before their MIs. Themes emerged detailing the quality and frequency of sexual activity. Most women used positive or neutral terms to describe their prior sexual life, such as “active,” “very good,” “routine,” or “normal.” In contrast with the period before their MIs, a prevalent theme of “indifference” about sex was common post‐MI: “I can take it or leave it. It's not a big thing anymore (R1A68)”; “When we do have sex it's acceptable … It's okay (R10A69).” Most women discussed the quality of their sexual lives post‐MI in terms of decreased frequency but improved satisfaction:
“It's certainly not as often as either of us would like. But you know, sometimes life gets in the way when you let it… I think we're both kind of on the same page that we'd like to get to it more often. But when we do it's very good.” (R15A43)
“I just think that now … things are better than they ever have been because we've committed ourselves to not allowing that part of our relationship to become routine, but to become better all the time. So I'd say it's great.” (R6A50)
Participants reported sexual problems both before and following their MIs, including low desire and vaginal dryness (Figure 2A). Themes of attribution to older age, medical problems, fatigue, menopause, and medication side effects were common. Following MI, several women reported new sexual concerns attributed to the MI or related procedures: “My concern was … some positions you get in, you're flat on your bed … different positions put pressure on your chest. So that was my main concern, that [staples from open‐heart surgery] might come open (R5A54).” One woman who did not resume sexual activity felt her loss of libido was due to antidepressant therapy for depression since her MI (R9A69). Sexual problems experienced by respondents’ partners both before and following their MIs included erectile dysfunction and low desire and sexual issues related to health problems such as diabetes, heart disease, and fatigue (Figure 2B).
Figure 2.
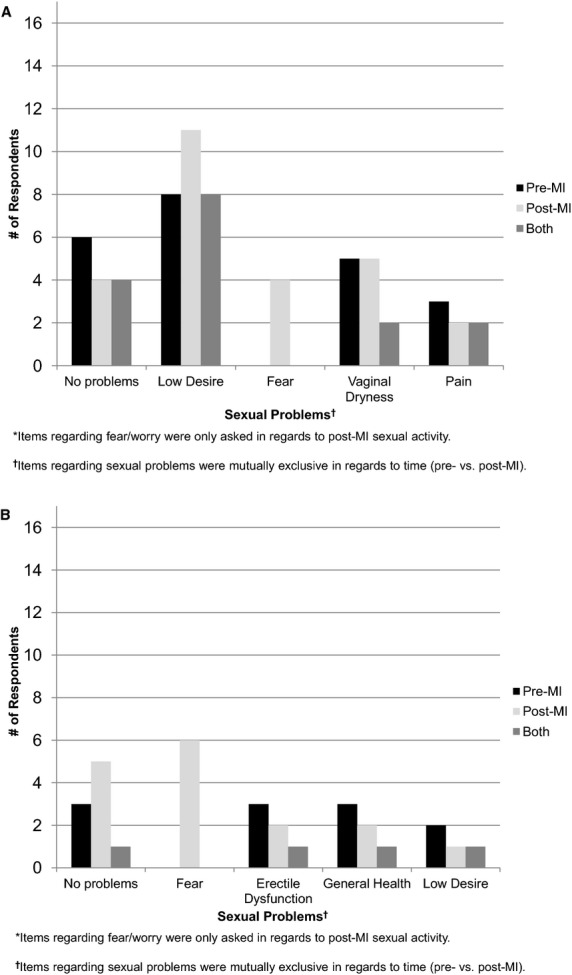
A, Patients’ sexual problems reported by TRIUMPH interview respondents.* B, Partners’ sexual problems reported by TRIUMPH interview respondents.* TRIUMPH indicates Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status; MI, myocardial infarction.
Resumption of Sexual Activity: Motivation and Fear
For many women, sexual activity was less frequent but nonsexual physical intimacy increased and satisfaction was higher after the MI. “I want to hold his hand more and snuggle more and have more hugs and stuff like that (R4A47).” Others talked about sex after an MI as life affirming and important for regaining a sense of normalcy.
“I think the first couple of times you get to it after the heart attack, and it's with a lot of things and not just sex … you want to do it just to prove that you can and to feel normal again. You don't always want to be the lady that had the heart attack.” (R15A43)
“I just didn't want to be stigmatized as a heart patient at that point. So, of course, I was concerned about that and also just wanting to return to a normal life.” (R6A50)
Motivation
Despite prevalent themes of fear, the majority of women expressed motivation to resume sexual activity. Most had resumed sex within 4 weeks of their MIs; all but 1 had resumed within 6 months. Many women were motivated to have sex for closeness with their spouse or partner: “I think, after you have a heart attack, you want somebody close to you (R17A63).” Others were mainly seeking physical pleasure (“For orgasm, basically … that's the primary goal. That's still the same [R11A43]”) or to please their partner (“I enjoy him having his and that's all I need (R1A68]”).
Fear
Fear of engaging in sexual activity after MI emerged as a prevalent theme. Respondents were fearful, and many had partners who were scared that sex could be harmful. For example:
“Well, I did not know that I would even have a problem with it until after I had experienced sex after having my heart attack and my heart wanted to pant too fast for me; it was my own fear. So, I thought that was me.” (R8A65)
“At first he was afraid because he thought I would have another heart attack … and I told him I'd rather die with a smile on my face… I had to convince my husband that I wasn't going to die in bed.” (R17A63)
In many cases, fear was identified as the driving factor behind women's loss of sexuality following MI:
“It's certainly psychological… Fear is not conducive to a healthy romp.” (R15A43)
“I was trying so hard I had a real heart palpitation… And my heart beat real fast and it scared me. And so I didn't want to get to that point, so … apparently I was cutting [sex] off.” (R8A65)
Patient–Physician Communication About Sexual Concerns After MI
The vast majority of women interviewed did not recall receiving instructions from their physicians regarding the resumption of sex post‐MI. Of the few women who did (n=5), most initiated the discussion themselves at the time of hospital discharge. Women who received instructions were particularly concerned about the safety of returning to sex, specifically in terms of levels of exertion and timing of resumption. Respondents recounted details of instructions received at the time of discharge; many described feeling overwhelmed and dissatisfied.
“There is so much being thrown at you on what to do and what to take and this, that, and the other that it's hard to remember everything.” (R2A60)
“You're totally overwhelmed with what has happened to you anyway; definitely overload.” (R13A54)
Discussions about resuming sexual activity were described as vague:
“The day before I left the hospital I said, ‘You didn't tell me when I could have relations.’ So then he says, ‘Well, that's going to be up to you, how you feel.’ But that's not giving me an answer.” (R17A63)
“[The physician] was walking out the door, and I said, ‘How long do I have to wait to have sex?’ And then he said, ‘Oh, just whenever, it's fine.’ And that was about it.” (R11A43)
Or they were confusing:
“When I came home … I asked the doctor point‐blank when could I have sex again, because … we were really sexually active. And he said when you can climb two flights of stairs without getting out of breath. Well, I couldn't hardly climb two flights of stairs before I had a heart attack.” (R5A54)
Respondents also identified factors that could facilitate or act as a barrier to patient–physician communication about sexual activity following an MI (Table 3). Physician‐initiated communication and a positive patient–physician relationship were seen as facilitators. Perceived barriers to communication about sexual activity following an MI included male sex of physician and perceived physician uncertainty about patients’ receptivity to discussing sexual matters.
Table 3.
Access and Barriers to Patient–Physician Communication About Sexual Activity
| Theme | n | Example |
|---|---|---|
| Access | ||
| Physician assertiveness | 4 | “Just bring it up and open the door… Maybe once they've been asked about it … they feel more comfortable saying or asking something (R11A43).” |
| Patient–physician relationship | 5 | “I have a good relationship with her… I would have been comfortable discussing it had she made it a routine part of our checkups (R6A50).” |
| Patient assertiveness | 5 | “My doctor … would never have brought this up, but I asked because I knew how active I was before I came in, and that was before I had the heart attack. So I thought I better ask (R5A54).” |
| Barriers | ||
| Male sex of physician | 5 | “I think they're probably afraid to say anything to women, though. For the guys, they might say something. But for the women, they just don't know… It might be taken the wrong way (R11A43).” |
| Perceived sex or age discrepancies in receptivity of discussions about sexual activity | 7 | “They think women are more passive [during sex] than men, so they would be more likely to tell a man who had a heart attack (R13A54).” “I was very young… So maybe because they're used to seeing women that are that much older … nobody really thinks to bring it up (R15A43).” |
Elements of an Effective Intervention: Initiation, Context, Timing and Content
Almost all women (n=16) felt that physicians should address resumption of sexual activity following an MI. Participants’ views on the elements of an effective intervention to improve sexual outcomes following an MI were summarized by the following themes.
Initiation of Discussion
Most women felt the cardiologist was the most appropriate member of the medical team to counsel patients regarding sexual activity following an MI. The cardiologist was described as “the one that would really know whether your heart is safe or not (R12A54).” Some women felt that their primary care doctor or gynecologist could also be helpful in addressing sexual issues later in the continuum of care.
“Well, your cardiologist is the one who should tell you. He's the one that takes care of you while you're in the hospital, and before you leave there, he should tell you, along with his other guidelines, what his guideline is for that.” (R7A73)
“I think [the cardiologist] knows your health situation better than anybody, so I think he is definitely the one that should talk to you.” (R2A60)
“I really do think my [cardiologist] would be effective… Had she initiated discussions about it, I probably would have responded to her questions… But I think I have a good relationship with her, that I would have been comfortable discussing it had she made it a routine part of our checkups.” (R6A50)
Context for Discussion
Most women preferred a private conversation with their physician, rather than a group discussion. The minority who were receptive to group counseling felt this should complement physician counseling and suggested an all‐female discussion session in the context of cardiac rehabilitation.
“I know that my doctor initially tried to get me to join a women's group … like that would be an avenue where I could meet other women who had had similar experiences… But I still don't think suggesting going to a support group … is a good replacement for the doctor discussing it [sex] with you as a patient.” (R6A50)
“One thing that I was real pleased about with my particular care were all the different support classes that they had on nutrition and exercise… But there was nothing offered in the sexuality area. That would be one area that they might want to look into.” (R9A69)
Timing of Discussion
Key subthemes included immediate versus delayed implementation of an intervention and expressions of feeling overwhelmed by information at hospital discharge. Most women felt the discussion around resumption of sexual activity should be initiated on hospital discharge and then more fully explored during the aftercare continuum. Introducing the subject early in a patient's care conveyed to the patient that the physician was open to this discussion should problems arise:
“I think for a doctor to develop a comfort level with a patient, that they should be asking about it every time. Especially on the 1‐month visit, because it sets a precedent. And it could take some women more visits before they would want to open up about it. Just knowing that it's an open topic would go a long way in encouraging women to discuss it more openly.” (R6A50)
Content of Counseling
Women expressed the importance of identifying “risk factors” for complications from sexual activity and “how to know when it's safe to resume activity (R16A49),” specifically in terms of exertion levels.
“I think what they're expecting is for their doctor to give them a timeline, like, don't do this for 4 weeks, don't do this for 6 weeks… You might have some kind of guideline for exertion, but I think that's something the doctors would have to come up with.” (R7A73)
“[I]t should be something that the doctors do talk to women about … when they've had a heart attack… [S]ex is strenuous and it's a lot on your heart muscles… They tell you when you have a heart attack not to run the vacuum cleaner, not to do this or that for so many months after… Why not say, as far as your sexual activity, hold off for 4 weeks until you come back?” (R12A54)
Key subthemes around delivery of the counseling included patient‐centeredness and counseling that addresses the patient holistically: “He dismisses [my questions] as not being what's important to him. What's important is the heart. And it's like, I'm a whole person here (R13A54).”
Discussion
Guidelines recommend that physicians counsel patients regarding resumption of sexual activity following an MI.10–11 In this study, most women had resumed sexual activity within 4 weeks of their MIs, despite fear of reinfarction or death, without directed communication from their physicians regarding safety. Of those who did discuss sexual matters with their physicians, most initiated the conversation themselves, and most were dissatisfied with the quality of instructions they received.
Lack of patient–physician communication, rather than lack of information about safety, presents a major barrier to improving sexual outcomes for women after MI. Studies have repeatedly shown that sexual activity after MI is relatively safe.22 Studies consistently show that middle‐aged and older women and men value their sexual life and regard sex as relevant for health and appropriate for discussion with a physician,23–25 yet major gaps in communication—especially for women—persist.26 Recommendations for how the topic of sex should be handled after MI varies across studies. Some recommend that the topic be handled primarily in the rehabilitation setting by cardiac rehabilitation nurses.26–27 Other studies recommend a self‐help strategy, using educational literature or video.28–29 Group education or couples' counseling sessions have also been recommended.13 One prior study suggested that, like the women we interviewed, communication about sexual matters after MI be initiated before hospital discharge and continued through aftercare.30 Themes from the women we interviewed pointed to some additional features of an intervention that would be effective in improving sexual outcomes for women after MI: (1) initiation of discussion by the treating cardiologist before hospital discharge, with a focus on safety to mitigate patient and partner fear, timing of resumption, and problems women might encounter; (2) attention to sexual function through the continuum of recovery; and (3) delivery in a one‐on‐one rather than a group setting. Patient and partner fear of sexual activity following MI has been demonstrated in previous studies and appears to be a major barrier that should be addressed by an intervention to improve sexual outcomes after MI.31–32
Very few interventions exist that are specifically designed to improve sexual outcomes for women following an MI. One important randomized, controlled trial (n=115, 20% female) evaluated a home‐based, self‐administered videotape to increase knowledge around resuming sexual activity, decrease related anxiety, improve sexual satisfaction, and decrease time to resumption.29 Compared with controls who received usual care (verbal and/or written instructions on resumption of sexual activity that varied based on cardiac rehabilitation nurses’ time constraints), those in the experimental group showed increased short‐term knowledge regarding sex after MI, yet had higher rates of anxiety at 1 month. No differences between groups were seen in sexual satisfaction or time to resumption of sexual activity. Based on our findings, most MI patients with sexual concerns do not initiate discussion of these with their physicians.14 An effective intervention to improve sexual outcomes without raising anxiety may need to be embedded in a 2‐way, physician‐initiated discussion.
Cardiac rehabilitation (CR) is effective at increasing survival, decreasing subsequent cardiac events, and improving quality of life through multifaceted programming.33–34 However, women are less likely than men to be referred to and enrolled in CR programs.35–36 Identification of sexual dysfunction is recommended as a component of psychosocial management in CR programs, but treatment strategies are not provided.13 Based on our findings, an effective intervention to improve sexual outcomes for women after MI likely begins at discharge with discussion of parameters about resuming sexual activity and referral to CR. Women can only benefit from CR if they participate. Future research is needed to know whether cardiologists might promote women's participation in CR and overall recovery by initiating predischarge discussions that include issues that are salient to a woman's “whole person” recovery—like sexuality. A strategy for “whole person” training and materials for CR providers that includes but is not limited to sexual recovery after MI should also support cardiologists, primary care physicians, and gynecologists involved in long‐term care of women with a history of MI.
Limitations of the Study
These findings should be interpreted in the context of potential limitations. This study was based in the United States, so it may have limited relevance in countries with different or more comprehensive models of aftercare for MI. The findings presented are based on those who agreed to participate in this research study and therefore may reflect attribution bias. Social response bias is always possible in survey research, although we did find consistency between patient responses in open‐ended interviews and the structured survey responses in the TRIUMPH Registry database. In addition, the mode of interview did not allow for collection or interpretation of nonverbal expressions. Despite broad inclusion criteria, participants in this sample were more likely than sexually active participants in the larger TRIUMPH Registry to be white and married. Also, interviews relied on recall, potentially introducing bias. However, recall bias was assessed in prior analysis, indicating no significant discrepancy between the medical record and patient recall about communication with a physician about sexual matters prior to hospital discharge.14
Conclusions and Next Steps
Partnered women were sexually active soon after an MI, even with concerns of safety and issues related to sexual function. Evidence‐based strategies to improve sexual outcomes in women following an MI are needed. MI is a life‐threatening event that some patients experience as traumatic. Social cognitive theory finds self‐efficacy to be an important indicator of differences in coping after a traumatic event37 that may extend to how patients and couples cope with sexual life after MI. Patient self‐efficacy may also influence the patient–physician relationship.38 Development of an effective intervention might include brief assessment of patient self‐efficacy and coping style early in the course of MI care and use this information to personalize care for improvement of sexual and other outcomes. An effective intervention to improve sexual outcomes in women after an MI should be informed by additional research to gain cardiologists’ input, leverage advances in health information technology that can be used for real‐time, personalized decision making and counseling support, fit efficiently into healthcare work flows, extend to other primary care providers, and be easily updated to accommodate expected advances in knowledge about treatment for female sexual dysfunction.
Sources of Funding
This work was supported by the National Heart, Lung, and Blood Institute (Center for Cardiovascular Outcomes Research at Yale University grant number U01 HL105270‐02, to H.M.K.; Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients [VIRGO] grant number R01 HL081153‐05, to Dr Krumholz; and CV Outcomes, Inc., Kansas City, MO, grant number P50 HL077113, to Dr Spertus) and the National Institute on Aging (grant numbers K23AG032870, to Dr Lindau, and the Chicago Core on Biomeasures in Population‐Based Health and Aging Research, at the NORC – University of Chicago Center on Demography and Economics of Aging (PI, L. Waite 5P30 AG 012857). Contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health or the National Institute on Aging.
Disclosures
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare no support from any organization for the submitted work other than grant support listed above (Drs Abramsohn, Lindau, Decker, B. Garavalia, L. Garavalia, and Gosch). Dr Krumholz discloses that he is the recipient of a research grant from Medtronic, Inc, through Yale University and is chair of a cardiac scientific advisory board for UnitedHealth. Dr Spertus discloses that he has partial salary support from grant number 1UL1RR033179.
References
- 1.Silber S. Evidence‐based management of ST‐segment elevation myocardial infarction (STEMI). Latest guidelines of the European Society of Cardiology (ESC) 2010. Herz. 2010; 35:558-564 [DOI] [PubMed] [Google Scholar]
- 2.Tunstall‐Pedoe H, Vanuzzo D, Hobbs M, Mahonen M, Cepaitis Z, Kuulasmaa K, Keil U. Estimation of contribution of changes in coronary care to improving survival, event rates, and coronary heart disease mortality across the WHO MONICA Project populations. Lancet. 2000; 355:688-700 [DOI] [PubMed] [Google Scholar]
- 3.Fitchett D, Theroux P, Brophy J, Cantor W, Cox J, Gupta M, Kertland H, Mehta S, Welsh R, Goodman S. Assessment and management of acute coronary syndromes (ACS): a Canadian perspective on current guideline‐recommended treatment—Part 2: ST‐segment elevation myocardial infarction. Can J Cardiol. 2011; 27:S402-S412 [DOI] [PubMed] [Google Scholar]
- 4.Fox K, Steg P, Eagle K, Goodman S, Anderson F, Granger C, Flather M, Budaj A, Quill A, Gore J. Decline in rates of death and heart failure in acute coronary syndromes, 1999–2006. JAMA. 2007; 297:1892-1900 [DOI] [PubMed] [Google Scholar]
- 5.Jernberg T, Johanson P, Held C, Svennblad B, Lindback J, Wallentin LSWEDEHEART/RIKS‐HIA Association between adoption of evidence‐based treatment and survival for patients with ST‐elevation myocardial infarction. JAMA. 2011; 305:1677-1684 [DOI] [PubMed] [Google Scholar]
- 6.Roger VL, Go AS, Lloyd‐Jones DM, Adams RJ, Berry JD, Brown TM, Camethon MR, Dai S, de Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpem SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie‐Rosett J. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011; 123:E18-E209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Setoguchi S, Glynn R, Avorn J, Mittleman M, Levin R, Winkelmayer W. Improvements in long‐term mortality after myocardial infarction and increased use of cardiovascular drugs after discharge. J Am Coll Cardiol. 2008; 51:1247-1254 [DOI] [PubMed] [Google Scholar]
- 8.Drory Y, Kravetz S, Weingarten M. Comparison of sexual activity of women and men after a first acute myocardial infarction. Am J Cardiol. 2000; 85:1283-1287 [DOI] [PubMed] [Google Scholar]
- 9.Boehm JK, Peterson C, Kivimaki M, Kubzansky LD. Heart health when life is satisfying: evidence from the Whitehall II cohort study. Eur Heart J. 2011; 32:2672-2677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anderson J, Adams C, Antman E, Bridges C, Califf R, Casey DJ, Chavey WE, Fesmire F, Hochman J, Levin T, Lincoff A, Peterson E, Theroux P, Wenger N, Wright R. ACCF/AHA focused update incorporated into the ACC/AHA 2007 guidelines for the management of patients with unstable angina/non–ST‐elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2011; 57:e215-e367 [DOI] [PubMed] [Google Scholar]
- 11.Levine G, Steinke E, Bakaeen F, Bozkurt B, Cheitlin M, Conti J, Foster E, Jaarsma T, Kloner R, Lange R, Lindau S, Maron B, Moser D, Ohman E, Seftel A, Stewart W. Sexual activity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2012; 125:1058-1072 [DOI] [PubMed] [Google Scholar]
- 12.Steg G, James SK, Atar D, Badano LP, Blomstrom‐Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez‐Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, van't Hof A, Widimsky P, Zahger DAuthors Task Force M ESC guidelines for the management of acute myocardial infarction in patients presenting with ST‐segment elevation. Eur Heart J. 2012; 33:2569-2619 [DOI] [PubMed] [Google Scholar]
- 13.Balady G, Williams M, Ades P, Bittner V, Comoss P, Foody J, Franklin B, Sanderson B, Southard D. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007; 115:2675-2682 [DOI] [PubMed] [Google Scholar]
- 14.Lindau S, Abramsohn E, Gosch K, Wroblewski K, Spatz E, Chan P, Spertus J, Krumholz H. Patterns and loss of sexual activity in the year following hospitalization for myocardial infarction: a U.S. national, multi‐site observational study. Am J Cardiol. 2012; 109:1439-1444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arnold S, Chan P, Jones P, Decker C, Buchanan D, Krumholz H, Ho P, Spertus J. Translational Research Investigating Underlying disparities in acute Myocardial infarction Patients’ Health status (TRIUMPH): design and rationale of the prospective multicenter registry. Circulation. 2011; 4:467-476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marshall M. Sampling for qualitative research. Fam Pract. 1996; 13:522-525 [DOI] [PubMed] [Google Scholar]
- 17.Campbell D, Fiske D. Convergent and discriminant validation by the multitrait‐multimethod matrix. Psychol Bull. 1959; 56:81-105 [PubMed] [Google Scholar]
- 18.Glaser B, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. 1967Chicago, IL: Aldine [Google Scholar]
- 19.Graneheim U, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurs Educ Today. 2004; 24:105-112 [DOI] [PubMed] [Google Scholar]
- 20.Spitzer R, Kroenke K, Williams J. Validation and utility of a self‐report version of PRIME‐MD: the PHQ primary care study. JAMA. 1999; 282:1737-1744 [DOI] [PubMed] [Google Scholar]
- 21.Eagle K, Lim M, Dabbous O, Pieper K, Goldberg R, Van de Werf F, Goodman S, Granger C, Steg PG, Gore J, Budaj A, Avezum A, Flather M, Fox K. A validated prediction model for all forms of acute coronary syndrome: estimating the risk of 6‐month postdischarge death in an international registry. JAMA. 2004; 291:2727-2733 [DOI] [PubMed] [Google Scholar]
- 22.Dahabreh I, Paulus J. Association of episodic physical and sexual activity with triggering of acute cardiac events. JAMA. 2011; 305:1225-1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davison S, Bell R, LaChina M, Holden S, Davis S. The relationship between self‐reported sexual satisfaction and general well‐being in women. J Sex Med. 2009; 6:2690-2697 [DOI] [PubMed] [Google Scholar]
- 24.Laumann E, Paik A, Glasser D, Kang J, Wang T, Levinson B, Moreira E, Nicolosi A, Gingell C. A cross‐national study of subjective sexual well‐being among older women and men: findings from the Global Study of Sexual Attitudes and Behaviors. Arch Sex Behav. 2006; 35:145-161 [DOI] [PubMed] [Google Scholar]
- 25.Lindau S, Schumm L, Laumann E, Levinson W, O'Muircheartaigh C, Waite L. A study of sexuality and health among older adults in the United States. N Engl J Med. 2007; 357:762-774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steinke E, Mosack V, Barnason S, Wright D. Progress in sexual counseling by cardiac nurses, 1994 to 2009. Heart Lung. 2011; 40:e15-e24 [DOI] [PubMed] [Google Scholar]
- 27.Barnason S, Steinke E, Mosack V, Wright D. Comparison of cardiac rehabilitation and acute care nurses perceptions of providing sexual counseling for cardiac patients. J Cardiopulm Rehabil. 2011; 31:157-163 [DOI] [PubMed] [Google Scholar]
- 28.Steinke E. A videotape intervention for sexual counseling after myocardial infarction. Heart Lung. 2002; 31:348-354 [DOI] [PubMed] [Google Scholar]
- 29.Steinke E, Swan J. Effectiveness of a videotape for sexual counseling after myocardial infarction. Res Nurs Health. 2004; 27:269-280 [DOI] [PubMed] [Google Scholar]
- 30.Steinke E, Patterson‐Midgley P. Importance and timing of sexual counseling after myocardial infarction. J Cardiopulm Rehabil. 1998; 18:401-407 [DOI] [PubMed] [Google Scholar]
- 31.Kazemi‐Saleh D, Pishgou B, Assari S, Tavallaii S. Fear of sexual intercourse in patients with coronary artery disease: a pilot study of associated morbidity. J Sex Med. 2007; 4:1619-1625 [DOI] [PubMed] [Google Scholar]
- 32.Steinke E, Wright D. The role of sexual satisfaction, age, and cardiac risk factors in the reduction of post‐MI anxiety. Eur J Cardiovasc Nurs. 2006; 5:190-196 [DOI] [PubMed] [Google Scholar]
- 33.Savage P, Sanderson B, Brown T, Berra K, Ades P. Clinical research in cardiac rehabilitation and secondary prevention. J Cardiopulm Rehabil. 2011; 31:333-341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shepherd C, While A. Cardiac rehabilitation and quality of life: a systematic review. Int J Nurs Stud. 2012; 49:755-771 [DOI] [PubMed] [Google Scholar]
- 35.Aragam K, Moscucci M, Smith D, Riba A, Zainea M, Chambers J, Share D, Gurm H. Trends and disparities in referral to cardiac rehabilitation after percutaneous coronary intervention. Am Heart J. 2011; 161:544.e2-551.e2 [DOI] [PubMed] [Google Scholar]
- 36.Leon A, Franklin B, Costa F, Balady G, Berra K, Stewart K, Thompson P, Williams M, Lauer M. Cardiac rehabilitation and secondary prevention of coronary heart disease: an American Heart Association Scientific Statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity), in collaboration with the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2005; 111:369-376 [DOI] [PubMed] [Google Scholar]
- 37.Benight C, Bandura A. Social cognitive theory of posttraumatic recovery: the role of perceived self‐efficacy. Behav Res Ther. 2004; 42:1129-1148 [DOI] [PubMed] [Google Scholar]
- 38.Raymond M, Iliffe S, Harari D, Swift C, Gillmann G, Stuck A. Health risk appraisal for older people 5: self efficacy in patient‐doctor interactions. Prim Health Care Res Dev. 2011; 12:348-356 [DOI] [PubMed] [Google Scholar]


