Abstract
Background
Prehospital 12‐lead electrocardiography (ECG) is critical to timely STEMI care although its use remains inconsistent. Previous studies to identify reasons for failure to obtain a prehospital ECG have generally only focused on individual emergency medical service (EMS) systems in urban areas. Our study objective was to identify patient, geographic, and EMS agency‐related factors associated with failure to perform a prehospital ECG across a statewide geography.
Methods and Results
We analyzed data from the Prehospital Medical Information System (PreMIS) in North Carolina from January 2008 to November 2010 for patients >30 years of age who used EMS and had a prehospital chief complaint of chest pain. Among 3.1 million EMS encounters, 134 350 patients met study criteria. From 2008–2010, 82 311 (61%) persons with chest pain received a prehospital ECG; utilization increased from 55% in 2008 to 65% in 2010 (trend P<0.001). Utilization by health referral region ranged from 22.9% to 74.2% and was lowest in rural areas. Men were more likely than women to have an ECG performed (63.0% vs 61.3%, adjusted RR 1.02, 95% CI 1.01 to 1.04). The certification‐level of the EMS provider (paramedic vsbasic/intermediate) and system‐level ECG equipment availability were the strongest predictors of ECG utilization. Persons in an ambulance with a certified paramedic were significantly more likely to receive a prehospital ECG than nonparamedics (RR 2.15, 95% CI 1.55, 2.99).
Conclusions
Across a large geographic area prehospital ECG use increased significantly, although important quality improvement opportunities remain. Increasing ECG availability and improving EMS certification and training levels are needed to improve overall care and reduce rural‐urban treatment differences.
Keywords: emergency medical services, health policy and outcomes research
Introduction
Emergency medical services (EMS) play a critical role in the early recognition of acute STEMI. Prehospital 12‐lead electrocardiography (ECG) significantly reduces treatment times for STEMI and lowers mortality.1–3 It allows paramedics to diagnose STEMI and thereby provide advanced notification to receiving emergency departments or enable them to bypass a nearby hospital without the capability to perform percutaneous coronary intervention (PCI).4 Therefore, EMS has been the focus of national efforts to improve systems of care for patients with STEMI. For example, the use of prehospital 12‐lead ECG by EMS to diagnose STEMI is recommended by the American Heart Association (AHA), the American College of Cardiology (ACC), the National Association of EMS Physicians, and is part of the ACC/AHA Guidelines for Management of Patients with STEMI.5–8
Despite the clear benefit of prehospital ECGs for patients with STEMI, adherence to the recommendation that EMS personnel obtain an ECG when indicated has been problematic. In a recent study of 12 097 patients with STEMI identified in the National Cardiovascular Data Registry, only 27.4% of patients who were transported to a hospital by EMS received a prehospital ECG, resulting in delays in PCI.1 Barriers to effective adoption of ECG by EMS include the cost and replacement of equipment, paramedic training, and ongoing competency assessment.9 However, previous studies designed to identify reasons for failure to obtain an ECG by EMS have generally focused on individual cities/EMS agencies or utilized only registry data where EMS systems in rural and underserved areas are typically underrepresented.
In 2006, the state of North Carolina began implementing a statewide regionalization program for STEMI care which now includes all 120 hospitals and 500+ EMS agencies.10 The goal of the present study was to utilize a unique statewide EMS database in North Carolina to estimate the proportion of patients with chest pain who received an ECG during EMS transport, to evaluate temporal changes in quality via ECG utilization, and to identify patient‐, geographic‐, and EMS agency‐related factors associated with failure to perform a prehospital ECG.
Methods
Design and Data Sources
This was a retrospective cohort study. The cohort consisted of persons with chest pain who were transported to a hospital by EMS agencies in North Carolina between January 1, 2008 and November 29, 2010. Data for the study were obtained from the Prehospital Medical Information System (PreMIS). PreMIS is a component of the North Carolina EMS Data System and is located within the EMS Performance Improvement Center (EMSPIC) in the Department of Emergency Medicine at the University of North Carolina in Chapel Hill, NC. PreMIS is an electronic system for EMS data capture, analysis, and reporting and serves as the electronic health care record for the documentation of EMS care delivery.11 During the study period PreMIS contained prehospital data that had been submitted by ≈540 licensed EMS agencies for over 3 million transported persons. The data were entered into PreMIS using a web‐based interface or exported by EMS agencies to PreMIS using commercial software that is certified compliant to EMS data standards established by the National EMS Information System (NEMSIS).
The North Carolina Office of Emergency Medical Services (NCOEMS) is responsible for the planning, development, coordination, and regulation of EMS systems. In 2002, North Carolina mandated electronic EMS data collection locally and submission of data into a statewide EMS data system. This legislation also formalized and coordinated EMS at the county level. As of July 2003, all 100 counties in North Carolina were required to develop a written EMS system plan that encompassed every EMS agency in the county. These EMS system plans consolidated the credentialing of EMS agencies, continuing education of EMS professionals, leadership, management, administration, medical direction, clinical protocols, and methods for quality assessment and improvement.
Study Population
The current NC EMS protocols specify that persons over the age of 30 with chest pain should receive an ECG; therefore, we selected the electronic records of persons in this age group who activated emergency (911) medical services and had a chief complaint of chest pain from PreMIS (n=151 324 records). Two datasets of persons were then created from this chest pain cohort (Figure 1). One dataset (geographic) was used to estimate the proportion of patients who received a prehospital ECG and to describe geographic and temporal variation in ECG utilization. A second dataset (risk factor) was used to identify patient‐ and EMS system‐level predictors for failure to receive an ECG.
Figure 1.
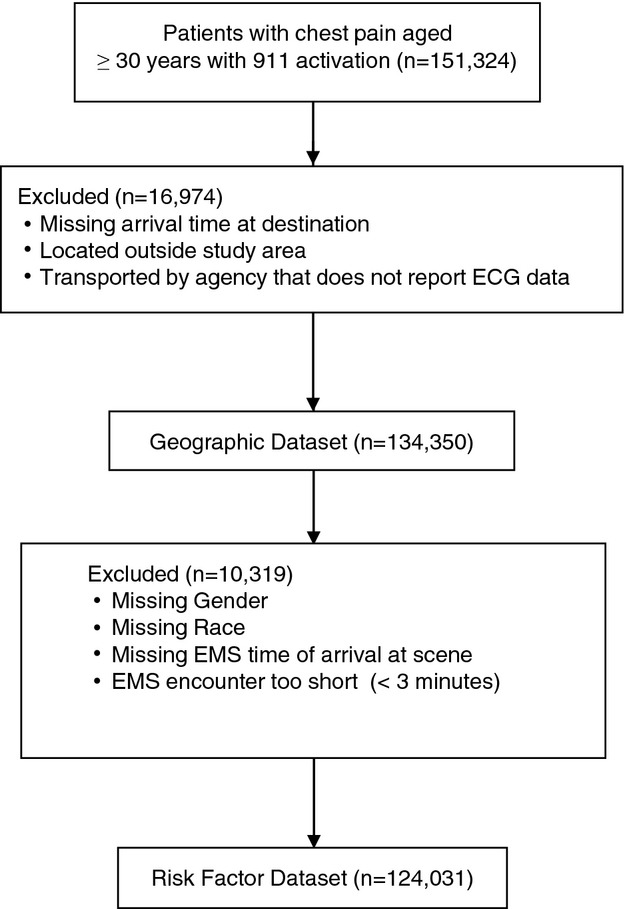
Flowchart of study dataset definition and exclusion criteria. ECG indicates electrocardiography; EMS, emergency medical services.
Geographic dataset
Records were excluded from this dataset if the time of arrival at the destination was not recorded, if the incident zip code was located more than 0.15 decimal degrees (≈10 miles) outside of North Carolina, or if the transport was associated with an agency that did not transmit data to PreMIS about prehospital ECG use. The latter scenario sometimes occurred due to known software incompatibility between certain agencies and PreMIS. Records located in zip codes containing <10 persons with chest pain who were transported per year were also excluded. If the incident zip code was missing or invalid, then the person's home zip code was used as a surrogate for the incident location. If both the incident and home zip code were missing, the zip code of the transferring EMS agency was used as the event location. The incident zip code was missing for ≈7% of all records. After exclusions, the final geographic dataset population contained 134 350 records (88.7% of all eligible records).
Risk factor dataset
Additional exclusions were made for this dataset if data on patient gender or race were missing, if time of EMS arrival at scene was missing, or if the total time of the EMS transport was <3 minutes (ie, there was inadequate opportunity for EMS to perform an ECG). This left a total of 124 031 records (82.0% of all eligible records) for the risk‐factor analysis.
Data Analysis
A summary of the analyses performed using the geographic and risk factor datasets are presented in Table 1. For the geographic dataset, the frequency of overall ECG utilization was calculated by health referral region and by service year. Hospital referral regions were derived from the Dartmouth Atlas using zip codes. These regions represent the health care markets for tertiary medical care that generally require the services of a major referral center.12 Because of data use agreement restrictions, we present the data in map‐form at the health referral region instead of smaller geographic distributions (ie, counties) to prevent identification of individual agencies or counties.
Table 1.
Summary of Analyses of ECG Utilization in Chest Pain Patients Transported in NC During 2008 to 2010
| Analysis Sample | Unit of Analysis | Outcomes |
|---|---|---|
| Geographic dataset | Health Referral Region | 1. Overall ECG utilization by region |
| 2. ECG utilization trends by year and region | ||
| Risk factor dataset | Patient | 1. Demographic, clinical, EMS system, and geographic factors associated with ECG utilization |
| 2. Multiple risk‐factor adjusted associations with ECG utilization |
ECG indicates electrocardiography; EMS, emergency medical services.
For the risk factor dataset, risk factors for failure to obtain an ECG for patients with chest pain were determined. Analyses were completed using patient demographics, clinical‐related factors, transport‐related factors, EMS system factors, and geographic location. Patient demographics included age, gender, and race. Age in years was categorized into the following group: 30 to <50, 50 to <70, 70 to <80, and ≥80. The race groups American Indian or Alaska Native, Asian, and Native Hawaiian or Other Pacific Islander accounted for <5% of the cohort and were merged as “Other”.
Clinical‐related factors were presenting vital signs (pulse and blood pressure). Hypotension (systolic BP <90 bpm) and high pulse rate (>100 bpm) were defined using the first measured set of vital signs. Transport‐related factors included transport time, time of day, day of week (weekday vs weekend), and year of service and highest certification level of the EMS crew. Certification level was defined as paramedic or nonparamedic. The highest EMS certification level for North Carolina is paramedic. Basic and intermediate level certification were combined into a single nonparamedic category. Agency type was classified as private/hospital, public governmental, or community/nonprofit. The public governmental category includes EMS services provided by fire departments. The date/time the ambulance unit was notified by dispatch was defined as the time of day, day, and year that the service was provided. Transport time was the difference between the arrival at destination (ie, hospital) time and the scene arrival time. EMS system‐related factors included agency type (ie, public vs private), rural status (yes vs no) of incident county, and EMS system ECG capability. The latter information was obtained from an internal, unpublished survey of EMS county medical directors in North Carolina. County‐level prehospital ECG capabilities were defined as the proportion of EMS agencies within a county that had prehospital ECG capability/equipment and were grouped as 0%, >0%—<25%, 25%—<50%, 50%—<75%, 75%—<100%, 100%.
The primary outcome of interest was whether a prehospital ECG was performed. In the geographic dataset, crude ECG utilization rates were calculated by dividing the number of ECGs performed by the total number of eligible patients. ECG utilization rates were calculated for each region by year. A Cochran‐Armitage test for linear trend over time of ECG utilization was performed for all regions combined and separately for each region.
In the risk factor dataset, multivariable analyses were performed to estimate the relative risk of ECG utilization in chest pain patients transported by EMS in North Carolina from 2008 through 2010. Generalized estimating equations were used to account for data dependency by county. Variables were grouped into 4 categories (clinical, transport, system, and spatial) and these were included in the respective multivariable models. Statistical analysis was performed using SAS version 9.1 or higher (SAS Institute). This project was approved by the Institutional Review Board at UNC.
Results
Geographic Dataset
During the study period 82 311 (61%) persons with chest pain who met the study criteria received a prehospital ECG (Table 2). Statewide ECG utilization increased from an average of 55% in 2008 to almost 64% in 2009 and 65% in 2010 (P value for trend <0.001). ECG utilization by health referral region (HRR) ranged from 22.9% to 74.2% (Figure 2). The eastern part of North Carolina, which comprises the “stroke belt”, and the far western part of the state comprise the most rural populations. Regions in these areas had the lowest proportion of prehospital ECG utilization. ECG utilization increased significantly in most regions during the study period. Persons transported by EMS systems (ie, counties) that had 100% capability to perform an ECG had the highest proportion of ECG utilization. However, even among regions where EMS agencies reported high levels of ECG capability (ie, 75% or 100% of agencies), there was wide variation in use. For example, among regions who reported 100% ECG capability, ECG utilization range from a low of 62% in Region 5 to a high of 91% in Region 2 (table not shown).
Table 2.
ECG Utilization (%) in the Geographic Dataset that Included 134 350 Patients With Chest Pain Transported by North Carolina EMS Agencies in 2008 to 2010
| Health Referral Region | ECG Utilization | ||||
|---|---|---|---|---|---|
| Overall Events (%) | 2008 Events (%) | 2009 Events (%) | 2010 Events (%) | ||
| Geographic Dataset | 82 311 (61.3%) | 24 083 (55.2%) | 30 044 (63.5%) | 28 184 (64.9%) | |
| Region 01 | Charlotte, NC | 12 106 (70.9%) | 3044 (54.9%) | 3993 (78.4%) | 5069 (78.9%) |
| Region 02 | Winston‐Salem, NC | 11 778 (68.0%) | 4470 (74.1%) | 4653 (68.3%) | 2655 (59.2%) |
| Region 03 | Greenville, NC | 5060 (36.1%) | 1236 (28.6%) | 1886 (36.7%) | 1938 (42.4%) |
| Region 04 | Greensboro, NC | 2809 (27.5%) | 664 (18.5%) | 1063 (30.3%) | 1082 (34.7%) |
| Region 05 | Durham, NC | 8304 (52.5%) | 2189 (42.1%) | 3252 (56.3%) | 2863 (59.2%) |
| Region 06* | Raleigh, NC | 23 225 (74.2%) | 7129 (71.8%) | 8631 (78.7%) | 7465 (71.8%) |
| Region 07 | Hickory, NC | 3512 (64.4%) | 953 (51.7%) | 1016 (55.9%) | 1543 (86.2%) |
| Region 08* | Wilmington, NC | 6180 (69.9%) | 1852 (69.8%) | 2150 (68.0%) | 2178 (72.0%) |
| Region 09 | Asheville, NC | 8132 (68.0%) | 2168 (56.8%) | 2966 (72.6%) | 2998 (74.1%) |
| Region 10* | Norfolk, VA | 1105 (57.3%) | 362 (54.6%) | 412 (58.5%) | 331 (58.8%) |
| Region 11 | Johnson City, TN | 100 (22.9%) | 16 (21.1%) | 22 (10.0%) | 62 (44.3%) |
ECG indicates electrocardiography; EMS, emergency medical services.
Tests for trend are statistically significant (P<0.0001) at α=0.05 except in regions 6 (P=0.74), 8 (P=0.05), and 10 (P=0.12).
Figure 2.
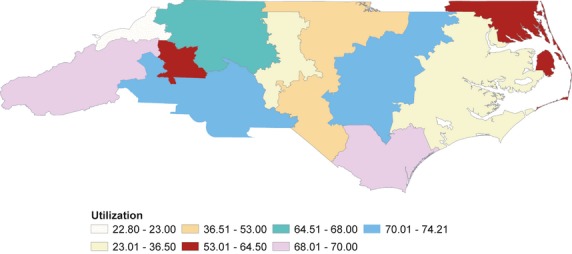
ECG utilization (%) by region for 134 350 individuals with chest pain transported by North Carolina EMS agencies in 2008 to 2010. ECG indicates electrocardiography; EMS, emergency medical services.
Risk‐Factor Dataset
A higher percentage of this cohort was white (65.7%), female (52.9%), normotensive (89.9%), and had an initial pulse rate ≤100 beats per minute (70.9%). (Table 3) Most patients were transported between 8 am and midnight (79.8%) and during the week (74.0%). A majority of patients were transported by public governmental agencies (78.1%) and agencies where the highest crew certification was a paramedic (92.2%). The relative risk (95% CI) of ECG utilization was determined from multivariable analysis models (Table 4). Hypotension, high pulse rate, transport time, year, level of crew certification, and system ECG capability were all significant predictors (P<0.05) of ECG utilization in multivariable models; however, hypotension and high pulse rate were only borderline significant since rounded values for the 95% confidence interval included 1 at the lower bound. In the multivariable models, men were statistically more likely than women with chest pain to have an ECG performed, although the absolute clinical difference was small.
Table 3.
Characteristics for Individuals With Chest Pain who were Transported by North Carolina EMS Agencies in 2008 to 2010 by Analysis Sample and Region
| Characteristics | Geographic Sample | Risk Factor Sample | Region 01 (Charlotte, NC) | Region 02 (Winston‐Salem, NC) | Region 03 (Greenville, NC) | Region 04 (Greensboro, NC) | Region 05 (Durham, NC) | Region 06 (Raleigh, NC) | Region 07 (Hickory, NC) | Region 08 (Wilmington, NC) | Region 09 (Asheville, NC) | Region 10 (Norfolk, VA) | Region 11 (Johnson City, TN) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Subjects (% geographic sample) | 134 350 | 124 031 (92.3%) | 17 065 (12.7%) | 17 329 (12.9%) | 14 027 (10.4%) | 10 209 (7.6%) | 15 813 (11.8%) | 31 298 (23.3%) | 5450 (4.1%) | 8839 (6.6%) | 11 953 (8.9%) | 1930 (1.4%) | 437 (0.3%) |
| Subjects (% risk factor sample) | — | — | 14 175 (11.4%) | 16 295 (13.1%) | 13 219 (10.7%) | 9451 (7.6%) | 14 947 (12.1%) | 30 373 (24.5%) | 5329 (4.3%) | 8440 (6.8%) | 9638 (7.8%) | 1889 (1.5%) | 275 (0.2%) |
| Age, y | |||||||||||||
| N (%) | 134 350 (100%) | 124 031 (100%) | 17 065 (100%) | 17 329 (100%) | 14 027 (100%) | 10 209 (100%) | 15 813 (100%) | 31 298 (100%) | 5450 (100%) | 8839 (100%) | 11 953 (100%) | 1930 (100%) | 437 (100%) |
| Mean (Std) | 60.1 (15.86) | 60.0 (15.84) | 60.5 (16.16) | 60.4 (15.95) | 60.1 (15.74) | 60.4 (16.03) | 59.1 (15.55) | 59.0 (15.66) | 59.6 (15.99) | 60.4 (15.38) | 62.4 (16.22) | 61.1 (15.68) | 63.7 (15.29) |
| Min, Max | 30.0, 109.0 | 30.0, 109.0 | 30.0, 108.0 | 30.0, 106.0 | 30.0, 108.0 | 30.0, 105.0 | 30.0, 107.0 | 30.0, 105.0 | 30.0, 109.0 | 30.0, 104.0 | 30.0, 103.0 | 30.0, 101.0 | 30.0, 95.0 |
| Median | 59 | 58 | 59.0 | 59.0 | 59.0 | 59.0 | 57.0 | 57.0 | 58.0 | 59.0 | 62.0 | 59.0 | 63.0 |
| Q1, Q3 | 48.0, 73.0 | 48.0, 72.0 | 48.0, 73.0 | 48.0, 73.0 | 48.0, 72.0 | 48.0, 73.0 | 47.0, 71.0 | 47.0, 71.0 | 47.0, 73.0 | 49.0, 72.0 | 49.0, 76.0 | 49.0, 74.0 | 52.0, 76.0 |
| Age Groups, y | |||||||||||||
| 30 to 50 | 39 212 (29.2%) | 36 279 (29.2%) | 4951 (29.0%) | 5027 (29.0%) | 3975 (28.3%) | 2923 (28.6%) | 4814 (30.4%) | 9779 (31.2%) | 1687 (31.0%) | 2418 (27.4%) | 3046 (25.5%) | 507 (26.3%) | 85 (19.5%) |
| 50 to 70 | 55 043 (41.0%) | 50 952 (41.1%) | 6802 (39.9%) | 6969 (40.2%) | 5843 (41.7%) | 4178 (40.9%) | 6771 (42.8%) | 12 899 (41.2%) | 2167 (39.8%) | 3740 (42.3%) | 4664 (39.0%) | 812 (42.1%) | 198 (45.3%) |
| 70 to 80 | 20 446 (15.2%) | 18 850 (15.2%) | 2530 (14.8%) | 2721 (15.7%) | 2212 (15.8%) | 1477 (14.5%) | 2190 (13.8%) | 4638 (14.8%) | 846 (15.5%) | 1472 (16.7%) | 1976 (16.5%) | 313 (16.2%) | 71 (16.2%) |
| ≥80 | 19 649 (14.6%) | 17 950 (14.5%) | 2782 (16.3%) | 2612 (15.1%) | 1997 (14.2%) | 1631 (16.0%) | 2038 (12.9%) | 3982 (12.7%) | 750 (13.8%) | 1209 (13.7%) | 2267 (19.0%) | 298 (15.4%) | 83 (19.0%) |
| Gender | |||||||||||||
| Female | 70 647 (52.6%) | 65 594 (52.9%) | 8973 (52.6%) | 9245 (53.3%) | 7159 (51.0%) | 5482 (53.7%) | 8334 (52.7%) | 16 683 (53.3%) | 2802 (51.4%) | 4531 (51.3%) | 6271 (52.5%) | 958 (49.6%) | 209 (47.8%) |
| Male | 63 219 (47.1%) | 58 437 (47.1%) | 8020 (47.0%) | 8045 (46.4%) | 6829 (48.7%) | 4708 (46.1%) | 7425 (47.0%) | 14 493 (46.3%) | 2632 (48.3%) | 4233 (47.9%) | 5635 (47.1%) | 971 (50.3%) | 228 (52.2%) |
| Unknown | 484 (0.4%) | 0 | 72 (0.4%) | 39 (0.2%) | 39 (0.3%) | 19 (0.2%) | 54 (0.3%) | 122 (0.4%) | 16 (0.3%) | 75 (0.8%) | 47 (0.4%) | 1 (0.1%) | 0 |
| Race | |||||||||||||
| Black or African American | 33 445 (24.9%) | 33 221 (26.8%) | 2828 (16.6%) | 3167 (18.3%) | 4775 (34.0%) | 2474 (24.2%) | 5508 (34.8%) | 11 245 (35.9%) | 400 (7.3%) | 2102 (23.8%) | 483 (4.0%) | 460 (23.8%) | 3 (0.7%) |
| Other race | 9366 (7.0%) | 9313 (7.5%) | 162 (0.9%) | 253 (1.5%) | 192 (1.4%) | 96 (0.9%) | 1652 (10.4%) | 6271 (20.0%) | 47 (0.9%) | 119 (1.3%) | 377 (3.2%) | 194 (10.1%) | 3 (0.7%) |
| Unknown | 9408 (7.0%) | 0 | 2759 (16.2%) | 975 (5.6%) | 723 (5.2%) | 722 (7.1%) | 706 (4.5%) | 716 (2.3%) | 100 (1.8%) | 272 (3.1%) | 2243 (18.8%) | 30 (1.6%) | 162 (37.1%) |
| White | 82 131 (61.1%) | 81 497 (65.7%) | 11 316 (66.3%) | 12 934 (74.6%) | 8337 (59.4%) | 6917 (67.8%) | 7947 (50.3%) | 13 066 (41.7%) | 4903 (90.0%) | 6346 (71.8%) | 8850 (74.0%) | 1246 (64.6%) | 269 (61.6%) |
| Hypotension, SBP <90 mm Hg | |||||||||||||
| No | 120 710 (89.8%) | 111 502 (89.9%) | 15 012 (88.0%) | 15 388 (88.8%) | 13 417 (95.7%) | 5613 (55.0%) | 14 742 (93.2%) | 29 334 (93.7%) | 5259 (96.5%) | 8267 (93.5%) | 11 417 (95.5%) | 1845 (95.6%) | 416 (95.2%) |
| Yes | 2434 (1.8%) | 2241 (1.8%) | 407 (2.4%) | 300 (1.7%) | 260 (1.9%) | 85 (0.8%) | 291 (1.8%) | 473 (1.5%) | 114 (2.1%) | 183 (2.1%) | 286 (2.4%) | 23 (1.2%) | 12 (2.7%) |
| Missing | 11 206 (8.3%) | 10 288 (8.3%) | 1646 (9.6%) | 1641 (9.5%) | 350 (2.5%) | 4511 (44.2%) | 780 (4.9%) | 1491 (4.8%) | 77 (1.4%) | 389 (4.4%) | 250 (2.1%) | 62 (3.2%) | 9 (2.1%) |
| High Pulse Rate, >100 bpm | |||||||||||||
| No | 95 255 (70.9%) | 87 981 (70.9%) | 11 599 (68.0%) | 12 338 (71.2%) | 10 737 (76.5%) | 4513 (44.2%) | 11 630 (73.5%) | 22 967 (73.4%) | 4151 (76.2%) | 6390 (72.3%) | 9167 (76.7%) | 1443 (74.8%) | 320 (73.2%) |
| Yes | 26 645 (19.8%) | 24 635 (19.9%) | 3663 (21.5%) | 3241 (18.7%) | 2829 (20.2%) | 1111 (10.9%) | 3223 (20.4%) | 6523 (20.8%) | 1112 (20.4%) | 1968 (22.3%) | 2480 (20.7%) | 406 (21.0%) | 89 (20.4%) |
| Missing | 12 450 (9.3%) | 11 415 (9.2%) | 1803 (10.6%) | 1750 (10.1%) | 461 (3.3%) | 4585 (44.9%) | 960 (6.1%) | 1808 (5.8%) | 187 (3.4%) | 481 (5.4%) | 306 (2.6%) | 81 (4.2%) | 28 (6.4%) |
| Transport Time, min | |||||||||||||
| N (%) | 133 816 (99.6%) | 124 031 (100%) | 16 992 (99.6%) | 17 304 (99.9%) | 13 976 (99.6%) | 10 189 (99.8%) | 15 693 (99.2%) | 31 192 (99.7%) | 5443 (99.9%) | 8771 (99.2%) | 11 899 (99.5%) | 1920 (99.5%) | 437 (100%) |
| Mean (Std) | 33.7 (15.32) | 33.4 (14.66) | 31.7 (11.61) | 32.6 (14.42) | 36.7 (21.01) | 32.4 (12.90) | 35.7 (16.34) | 33.8 (14.20) | 33.7 (11.10) | 33.6 (16.53) | 32.4 (14.53) | 37.7 (21.56) | 37.3 (29.25) |
| Min, Max | 3.0, 281.4 | 3.0, 281.4 | 3.0, 270.0 | 3.0, 281.4 | 3.0, 279.0 | 3.0, 254.0 | 3.0, 276.7 | 3.0, 235.2 | 5.0, 157.0 | 3.0, 222.0 | 3.0, 266.0 | 6.0, 184.0 | 5.0, 155.0 |
| Median | 31 | 31 | 30.0 | 30.0 | 32.0 | 30.5 | 33.0 | 32.0 | 32.0 | 31.0 | 29.7 | 33.1 | 30.0 |
| Q1, Q3 | 24.0, 40.0 | 24.0, 40.0 | 24.0, 38.0 | 23.4, 38.0 | 23.0, 44.0 | 24.0, 38.3 | 26.0, 42.0 | 25.0, 40.0 | 26.0, 40.0 | 24.0, 40.0 | 23.3, 38.0 | 24.0, 44.0 | 21.0, 39.0 |
| Transport Time, min | |||||||||||||
| 03 to 13 | 3569 (2.7%) | 3356 (2.7%) | 391 (2.3%) | 460 (2.7%) | 676 (4.8%) | 291 (2.9%) | 254 (1.6%) | 779 (2.5%) | 64 (1.2%) | 228 (2.6%) | 334 (2.8%) | 68 (3.5%) | 24 (5.5%) |
| 13 to 18 | 8904 (6.6%) | 8399 (6.8%) | 1209 (7.1%) | 1258 (7.3%) | 1174 (8.4%) | 677 (6.6%) | 754 (4.8%) | 1927 (6.2%) | 228 (4.2%) | 697 (7.9%) | 805 (6.7%) | 128 (6.6%) | 47 (10.8%) |
| 18 to 23 | 17 293 (12.9%) | 16 234 (13.1%) | 2497 (14.6%) | 2434 (14.0%) | 1747 (12.5%) | 1306 (12.8%) | 1787 (11.3%) | 3587 (11.5%) | 629 (11.5%) | 1234 (14.0%) | 1755 (14.7%) | 249 (12.9%) | 68 (15.6%) |
| 23 to 28 | 23 070 (17.2%) | 21 520 (17.4%) | 3121 (18.3%) | 3271 (18.9%) | 1888 (13.5%) | 1914 (18.7%) | 2461 (15.6%) | 5217 (16.7%) | 944 (17.3%) | 1536 (17.4%) | 2395 (20.0%) | 261 (13.5%) | 62 (14.2%) |
| 28 to 33 | 23 245 (17.3%) | 21 640 (17.4%) | 3154 (18.5%) | 3127 (18.0%) | 1876 (13.4%) | 1878 (18.4%) | 2656 (16.8%) | 5551 (17.7%) | 1054 (19.3%) | 1412 (16.0%) | 2215 (18.5%) | 253 (13.1%) | 69 (15.8%) |
| >33 | 57 735 (43.0%) | 52 882 (42.6%) | 6620 (38.8%) | 6754 (39.0%) | 6615 (47.2%) | 4123 (40.4%) | 7781 (49.2%) | 14 131 (45.1%) | 2524 (46.3%) | 3664 (41.5%) | 4395 (36.8%) | 961 (49.8%) | 167 (38.2%) |
| Missing | 534 (0.4%) | 0 | 73 (0.4%) | 25 (0.1%) | 51 (0.4%) | 20 (0.2%) | 120 (0.8%) | 106 (0.3%) | 7 (0.1%) | 68 (0.8%) | 54 (0.5%) | 10 (0.5%) | 0 |
| Time of Day | |||||||||||||
| Daytime | 59 145 (44.0%) | 54 689 (44.1%) | 7145 (41.9%) | 7817 (45.1%) | 6219 (44.3%) | 4418 (43.3%) | 7222 (45.7%) | 13 561 (43.3%) | 2329 (42.7%) | 4060 (45.9%) | 5323 (44.5%) | 860 (44.6%) | 191 (43.7%) |
| Evening | 48 146 (35.8%) | 44 269 (35.7%) | 6504 (38.1%) | 6085 (35.1%) | 4882 (34.8%) | 3523 (34.5%) | 5598 (35.4%) | 11 161 (35.7%) | 1974 (36.2%) | 3205 (36.3%) | 4369 (36.6%) | 679 (35.2%) | 166 (38.0%) |
| Overnight | 27 059 (20.1%) | 25 073 (20.2%) | 3416 (20.0%) | 3427 (19.8%) | 2926 (20.9%) | 2268 (22.2%) | 2993 (18.9%) | 6576 (21.0%) | 1147 (21.0%) | 1574 (17.8%) | 2261 (18.9%) | 391 (20.3%) | 80 (18.3%) |
| Weekend | |||||||||||||
| Weekday | 99 457 (74.0%) | 91 839 (74.0%) | 12 395 (72.6%) | 13 034 (75.2%) | 10 488 (74.8%) | 7630 (74.7%) | 11 739 (74.2%) | 23 027 (73.6%) | 4032 74.0%) | 6578 (74.4%) | 8807 (73.7%) | 1412 (73.2%) | 315 (72.1%) |
| Weekend | 34 893 (26.0%) | 32 192 (26.0%) | 4670 (27.4%) | 4295 (24.8%) | 3539 (25.2%) | 2579 (25.3%) | 4074 (25.8%) | 8271 (26.4%) | 1418 (26.0%) | 2261 (25.6%) | 3146 (26.3%) | 518 (26.8%) | 122 (27.9%) |
| Service Year | |||||||||||||
| 2008 | 43 656 (32.5%) | 39 462 (31.8%) | 5548 (32.5%) | 6034 (34.8%) | 4316 (30.8%) | 3581 (35.1%) | 5195 (32.9%) | 9929 (31.7%) | 1843 (33.8%) | 2652 (30.0%) | 3819 (32.0%) | 663 (34.4%) | 76 (17.4%) |
| 2009 | 47 295 (35.2%) | 43 776 (35.3%) | 5092 (29.8%) | 6810 (39.3%) | 5145 (36.7%) | 3510 (34.4%) | 5781 (36.6%) | 10 967 (35.0%) | 1817 (33.3%) | 3162 (35.8%) | 4086 (34.2%) | 704 (36.5%) | 221 (50.6%) |
| 2010 | 43 399 (32.3%) | 40 793 (32.9%) | 6425 (37.7%) | 4485 (25.9%) | 4566 (32.6%) | 3118 (30.5%) | 4837 (30.6%) | 10 402 (33.2%) | 1790 (32.8%) | 3025 (34.2%) | 4048 (33.9%) | 563 (29.2%) | 140 (32.0%) |
| Highest Crew Certification | |||||||||||||
| Nonparamedic | 10 650 (7.9%) | 9658 (7.8%) | 879 (5.2%) | 408 (2.4%) | 4199 (29.9%) | 345 (3.4%) | 873 (5.5%) | 1863 (6.0%) | 34 (0.6%) | 1223 (13.8%) | 464 (3.9%) | 359 (18.6%) | 3 (0.7%) |
| Paramedic | 123 700 (92.1%) | 114 373 (92.2%) | 16 186 (94.8%) | 16 921 (97.6%) | 9828 (70.1%) | 9864 (96.6%) | 14 940 (94.5%) | 29 435 (94.0%) | 5416 (99.4%) | 7616 (86.2%) | 11 489 (96.1%) | 1571 (81.4%) | 434 (99.3%) |
| Agency Type | |||||||||||||
| Community, nonprofit | 12 493 (9.3%) | 11 502 (9.3%) | 1246 (7.3%) | 199 (1.1%) | 3785 (27.0%) | 283 (2.8%) | 558 (3.5%) | 3643 (11.6%) | 0 | 2309 (26.1%) | 117 (1.0%) | 353 (18.3%) | 0 |
| Private/hospital | 17 757 (13.2%) | 15 683 (12.6%) | 808 (4.7%) | 362 (2.1%) | 1927 (13.7%) | 582 (5.7%) | 2878 (18.2%) | 6110 (19.5%) | 1 (0.0%) | 3344 (37.8%) | 1393 (11.7%) | 31 (1.6%) | 321 (73.5%) |
| Public/government | 104 100 (77.5%) | 96 846 (78.1%) | 15 011 (88.0%) | 16 768 (96.8%) | 8315 (59.3%) | 9344 (91.5%) | 12 377 (78.3%) | 21 545 (68.8%) | 5449 (100%) | 3186 (36.0%) | 10 443 (87.4%) | 1546 (80.1%) | 116 (26.5%) |
| System Capability | |||||||||||||
| 0% | 1505 (1.1%) | 1039 (0.8%) | 0 | 0 | 704 (5.0%) | 0 | 0 | 1 (0.0%) | 0 | 0 | 440 (3.7%) | 360 (18.7%) | 0 |
| <25% | 1860 (1.4%) | 1818 (1.5%) | 0 | 1 (0.0%) | 1837 (13.1%) | 0 | 0 | 19 (0.1%) | 0 | 0 | 1 (0.0%) | 2 (0.1%) | 0 |
| 25% to <50% | 2961 (2.2%) | 2587 (2.1%) | 0 | 1125 (6.5%) | 359 (2.6%) | 0 | 0 | 480 (1.5%) | 0 | 989 (11.2%) | 0 | 0 | 8 (1.8%) |
| 50% to <75% | 14 607 (10.9%) | 13 916 (11.2%) | 1858 (10.9%) | 1517 (8.8%) | 2877 (20.5%) | 1901 (18.6%) | 3430 (21.7%) | 1945 (6.2%) | 868 (15.9%) | 0 | 211 (1.8%) | 0 | 0 |
| 75% to <100% | 51 684 (38.5%) | 48 617 (39.2%) | 6394 (37.5%) | 7904 (45.6%) | 4354 (31.0%) | 7726 (75.7%) | 3902 (24.7%) | 8049 (25.7%) | 4106 (75.3%) | 1165 (13.2%) | 6422 (53.7%) | 1349 (69.9%) | 313 (71.6%) |
| 100% | 61 733 (45.9%) | 56 054 (45.2%) | 8813 (51.6%) | 6782 (39.1%) | 3896 (27.8%) | 582 (5.7%) | 8481 (53.6%) | 20 804 (66.5%) | 476 (8.7%) | 6685 (75.6%) | 4879 (40.8%) | 219 (11.3%) | 116 (26.5%) |
| Rural | |||||||||||||
| No | 93 375 (69.5%) | 86 084 (69.4%) | 13 303 (78.0%) | 11 096 (64.0%) | 5595 (39.9%) | 9559 (93.6%) | 9385 (59.3%) | 26 800 (85.6%) | 4732 (86.8%) | 5691 (64.4%) | 7184 (60.1%) | 30 (1.6%) | 0 |
| Yes | 40 975 (30.5%) | 37 947 (30.6%) | 3762 (22.0%) | 6233 (36.0%) | 8432 (60.1%) | 650 (6.4%) | 6428 (40.7%) | 4498 (14.4%) | 718 (13.2%) | 3148 (35.6%) | 4769 (39.9%) | 1900 (98.4%) | 437 (100%) |
EMS indicates emergency medical services; SBP, systolic blood pressure.
Table 4.
ECG Utilization (%) in the Risk Factor Dataset that Included ≈124000 Individuals With Chest Pain Transported by North Carolina EMS Agencies in 2008 to 2010 Summarized by Characteristics Included in 4 Multivariable Models
| No ECG Performed | ECG Performed | Single Variable P Value | RR (95% CI) | Multi‐variable P Value | |
|---|---|---|---|---|---|
| Clinical Characteristics | |||||
| Age Groups, y | 0.34 | 0.20 | |||
| 30 to 50 | 13 960 (38.5%) | 22 319 (61.5%) | [Reference] | ||
| 50 to 70 | 19 250 (37.8%) | 31 702 (62.2%) | 1.01 (1.00, 1.03) | ||
| 70 to 80 | 6949 (36.9%) | 11 901 (63.1%) | 1.01 (0.98, 1.04) | ||
| ≥80 | 6853 (38.2%) | 11 097 (61.8%) | 0.99 (0.97, 1.00) | ||
| Gender | <0.01 | <0.05 | |||
| Female | 25 372 (38.7%) | 40 222 (61.3%) | [Reference] | ||
| Male | 21 640 (37.0%) | 36 797 (63.0%) | 1.02 (1.01, 1.04) | ||
| Race | <0.01 | <0.05 | |||
| Black or African American | 14 235 (42.8%) | 18 986 (57.2%) | 0.95 (0.84, 1.07) | ||
| Other race | 1626 (17.5%) | 7687 (82.5%) | 1.27 (1.02, 1.56) | ||
| White | 31 151 (38.2%) | 50 346 (61.8%) | [Reference] | ||
| Hypotension, SBP <90 | 0.05 | <0.05 | |||
| No | 37 228 (33.4%) | 74 274 (66.6%) | [Reference] | ||
| Yes | 665 (29.7%) | 1576 (70.3%) | 1.05 (1.00, 1.09) | ||
| High Pulse Rate, >100 | 0.06 | <0.05 | |||
| No | 29 698 (33.8%) | 58 283 (66.2%) | [Reference] | ||
| Yes | 7804 (31.7%) | 16 831 (68.3%) | 1.03 (1.00, 1.06) | ||
| Ride Characteristics | |||||
| Age Groups, y | 0.34 | 0.18 | |||
| 30 to 50 | 13 960 (38.5%) | 22 319 (61.5%) | [Reference] | ||
| 50 to 70 | 19 250 (37.8%) | 31 702 (62.2%) | 1.01 (1.00, 1.02) | ||
| 70 to 80 | 6949 (36.9%) | 11 901 (63.1%) | 1.01 (0.98, 1.03) | ||
| ≥80 | 6853 (38.2%) | 11 097 (61.8%) | 0.99 (0.98, 1.01) | ||
| Gender | <0.01 | <0.05 | |||
| Female | 25 372 (38.7%) | 40 222 (61.3%) | [Reference] | ||
| Male | 21 640 (37.0%) | 36 797 (63.0%) | 1.03 (1.01, 1.04) | ||
| Race | <0.01 | 0.12 | |||
| Black or African American | 14 235 (42.8%) | 18 986 (57.2%) | 0.98 (0.89, 1.09) | ||
| Other race | 1626 (17.5%) | 7687 (82.5%) | 1.21 (1.01, 1.46) | ||
| White | 31 151 (38.2%) | 50 346 (61.8%) | [Reference] | ||
| Transport Time, min | <0.01 | <0.05 | |||
| 03 to 13 | 2278 (67.9%) | 1078 (32.1%) | 0.53 (0.46, 0.62) | ||
| 13 to 18 | 3974 (47.3%) | 4425 (52.7%) | 0.84 (0.77, 0.91) | ||
| 18 to 23 | 6512 (40.1%) | 9722 (59.9%) | 0.94 (0.88, 1.00) | ||
| 23 to 28 | 7920 (36.8%) | 13 600 (63.2%) | 0.99 (0.95, 1.04) | ||
| 28 to 33 | 7745 (35.8%) | 13 895 (64.2%) | 1.01 (0.97, 1.05) | ||
| >33 | 18 583 (35.1%) | 34 299 (64.9%) | [Reference] | ||
| Time of Day | 0.38 | 0.40 | |||
| Daytime | 20 895 (38.2%) | 33 794 (61.8%) | [Reference] | ||
| Evening | 16 508 (37.3%) | 27 761 (62.7%) | 1.01 (0.99, 1.02) | ||
| Overnight | 9609 (38.3%) | 15 464 (61.7%) | 0.99 (0.97, 1.02) | ||
| Weekend | 0.12 | 0.08 | |||
| Weekday | 35 001 (38.1%) | 56 838 (61.9%) | [Reference] | ||
| Weekend | 12 011 (37.3%) | 20 181 (62.7%) | 1.01 (1.00, 1.02) | ||
| Service Year | 0.02 | <0.05 | |||
| 2008 | 17 086 (43.3%) | 22 376 (56.7%) | [Reference] | ||
| 2009 | 15 750 (36.0%) | 28 026 (64.0%) | 1.13 (1.02, 1.25) | ||
| 2010 | 14 176 (34.8%) | 26 617 (65.2%) | 1.14 (0.99, 1.30) | ||
| Highest Crew Certification | <0.01 | <0.05 | |||
| Nonparamedic | 6697 (69.3%) | 2961 (30.7%) | [Reference] | ||
| Paramedic | 40 315 (35.2%) | 74 058 (64.8%) | 2.15 (1.55, 2.99) | ||
| System Characteristics | |||||
| Age Groups | 0.34 | <0.05 | |||
| 30 to 50 | 13 960 (38.5%) | 22 319 (61.5%) | [Reference] | ||
| 50 to 70 | 19 250 (37.8%) | 31 702 (62.2%) | 1.01 (1.00, 1.02) | ||
| 70 to 80 | 6949 (36.9%) | 11 901 (63.1%) | 1.01 (0.99, 1.02) | ||
| ≥80 | 6853 (38.2%) | 11 097 (61.8%) | 0.99 (0.97, 1.00) | ||
| Gender | <0.01 | <0.05 | |||
| Female | 25 372 (38.7%) | 40 222 (61.3%) | [Reference] | ||
| Male | 21 640 (37.0%) | 36 797 (63.0%) | 1.02 (1.01, 1.03) | ||
| Race | <0.01 | <0.05 | |||
| Black or African American | 14 235 (42.8%) | 18 986 (57.2%) | 0.96 (0.89, 1.03) | ||
| Other race | 1626 (17.5%) | 7687 (82.5%) | 1.13 (1.04, 1.24) | ||
| White | 31 151 (38.2%) | 50 346 (61.8%) | [Reference] | ||
| Agency Type | 0.19 | 0.10 | |||
| Community, nonprofit | 6377 (55.4%) | 5125 (44.6%) | 0.79 (0.59, 1.07) | ||
| Private/hospital | 6443 (41.1%) | 9240 (58.9%) | 0.90 (0.78, 1.05) | ||
| Public governmental | 34 192 (35.3%) | 62 654 (64.7%) | [Reference] | ||
| System Capability | <0.01 | <0.05 | |||
| 0% | 1030 (99.1%) | 9 (0.9%) | 0.01 (0.00, 0.06) | ||
| >0% to <25% | 1718 (94.5%) | 100 (5.5%) | 0.08 (0.03, 0.24) | ||
| 25% to <50% | 1437 (55.5%) | 1150 (44.5%) | 0.67 (0.37, 1.24) | ||
| 50% to <75% | 5811 (41.8%) | 8105 (58.2%) | 0.76 (0.61, 0.94) | ||
| 75% to <100% | 24 821 (51.1%) | 23 796 (48.9%) | 0.70 (0.58, 0.85) | ||
| 100% | 12 195 (21.8%) | 43 859 (78.2%) | [Reference] | ||
| Rural | 0.79 | 0.77 | |||
| No | 32 052 (37.2%) | 54 032 (62.8%) | 0.99 (0.89, 1.10) | ||
| Yes | 14 960 (39.4%) | 22 987 (60.6%) | [Reference] | ||
| Spatial Characteristics | |||||
| Age Groups | 0.34 | <0.05 | |||
| 30 to 50 | 13 960 (38.5%) | 22 319 (61.5%) | [Reference] | ||
| 50 to 70 | 19 250 (37.8%) | 31 702 (62.2%) | 1.01 (1.00, 1.02) | ||
| 70 to 80 | 6949 (36.9%) | 11 901 (63.1%) | 1.01 (0.98, 1.03) | ||
| ≥80 | 6853 (38.2%) | 11 097 (61.8%) | 0.98 (0.96, 1.00) | ||
| Gender | <0.01 | <0.05 | |||
| Female | 25 372 (38.7%) | 40 222 (61.3%) | [Reference] | ||
| Male | 21 640 (37.0%) | 36 797 (63.0%) | 1.03 (1.01, 1.04) | ||
| Race | <0.01 | 0.12 | |||
| Black or African American | 14 235 (42.8%) | 18 986 (57.2%) | 0.99 (0.91, 1.07) | ||
| Other race | 1626 (17.5%) | 7687 (82.5%) | 1.22 (1.10, 1.36) | ||
| White | 31 151 (38.2%) | 50 346 (61.8%) | [Reference] | ||
| Area | 0.03 | <0.05 | |||
| Region 01 | 4272 (30.1%) | 9903 (69.9%) | 1.04 (0.88, 1.23) | ||
| Region 02 | 4897 (30.1%) | 11 398 (69.9%) | 1.03 (0.78, 1.36) | ||
| Region 03 | 8592 (65.0%) | 4627 (35.0%) | 0.49 (0.32, 0.73) | ||
| Region 04 | 6660 (70.5%) | 2791 (29.5%) | 0.71 (0.43, 1.17) | ||
| Region 05 | 6878 (46.0%) | 8069 (54.0%) | 0.74 (0.58, 0.94) | ||
| Region 06 | 7786 (25.6%) | 22 587 (74.4%) | [Reference] | ||
| Region 07 | 1890 (35.5%) | 3439 (64.5%) | 0.87 (0.58, 1.30) | ||
| Region 08 | 2539 (30.1%) | 5901 (69.9%) | 0.96 (0.73, 1.27) | ||
| Region 09 | 2514 (26.1%) | 7124 (73.9%) | 1.00 (0.85, 1.17) | ||
| Region 10 | 803 (42.5%) | 1086 (57.5%) | 0.77 (0.50, 1.19) | ||
| Region 11 | 181 (65.8%) | 94 (34.2%) | 0.49 (0.37, 0.64) | ||
Age, Gender, and Race were included in all 4 models. ECG indicates electrocardiography; RR, relative risk; EMS, emergency medical services; CI, confidence interval; SBP, systolic blood pressure.
The EMS certification‐level of the provider and EMS system prehospital ECG capability (ie, equipment availability) were the strongest predictors of ECG utilization. Persons in an ambulance with a certified paramedic were significantly more likely to receive a prehospital ECG than if a paramedic was not available (RR 2.15, 95% CI 1.55, 2.99). Persons who had shorter transport times were also significantly less likely to receive an ECG than those with longer transport times, presumably a reflection of the time required to perform a 12‐lead ECG.
Discussion
Among 151 324 patients who activated 911 and had a chief complaint of chest pain from 2008–2010 across North Carolina, ECG utilization by EMS was 61%. To our knowledge this is the largest population‐based study to date of prehospital ECG use by EMS. Prehospital ECG use increased significantly over the study period, from 56.7% in 2008 to 65.2% of eligible patients in 2010. The most important patient‐ and system‐level barriers to ECG use in the prehospital setting were the availability of prehospital ECG equipment and EMS crew certification levels. In general, these barriers to ECG use by EMS agencies disproportionately affected health care delivery in rural and underserved areas including the “stroke belt” where cardiovascular morbidity and mortality rates are among the highest in the country.13
The observed prehospital ECG utilization rate of 61% is more than twice the 27% rate observed using data from the National Cardiovascular Data Registry (NCDR) Acute Coronary Treatment and Intervention Outcomes Network (ACTION) registry for patients with STEMI who were transported by EMS from January 1, 2007 to December 31, 2007.1 In 2006, North Carolina began implementing a statewide regionalization program for STEMI care which has now expanded to include virtually all hospitals and EMS systems throughout the state.10 A key feature of this program has been to increase use of prehospital ECGs and improve coordination between EMS and receiving hospital emergency departments. During the program prehospital ECG use among patients transported to PCI centers by EMS improved from 67% to 88%. However, despite these efforts, only 32% of STEMI patients presenting to non‐PCI centers had a prehospital ECG performed.10 The present study highlights critical patient‐, provider‐, and system‐level factors that may be contributing to these ongoing gaps in care.
The availability and operability of prehospital ECG equipment is essential for EMS management of patients with chest pain. Prehospital ECG equipment availability in North Carolina was found to be lowest in the rural areas of the state and, not surprisingly, these areas had the lowest rates of ECG use. In Region 3, which comprises mostly rural areas in eastern North Carolina, a majority (59%) of agencies were operating in counties that were <75% capable of performing an ECG and the overall ECG rates were 36.1%. Although ECG utilization was higher in more urbanized areas with greater prehospital ECG capabilities, there is still significant room for improvement (ie, 58% overall rate in areas with 75% to 100% capability). Since these areas are more urbanized and thus treat significantly more patients with chest pain than rural areas, small improvements in overall prehospital utilization would potentially affect a large number of patients. Therefore, improving ECG utilization in all areas, including urban areas that already have ECG capability, should remain an important quality improvement goal.
Traditionally, the cost of integrated devices ($9000 to $25 000 each for a prehospital 12‐lead electrocardiograph with monitor‐defibrillator) made them cost‐prohibitive for poorly resourced agencies.9 While the price has decreased significantly over time, cost still remains a limiting factor for many EMS agencies. Access to proper equipment must be a priority for programs designed to improve ECG utilization for patients with chest pain. In 2010, the North Carolina Department of Health and Human Services was awarded a grant by the Duke Endowment to upgrade medical devices, including purchase and placement of ECG machines in ambulances. Future research should assess the impact of these types of investments on ECG utilization nationwide, patient treatment times, and outcomes, especially in low‐performing areas. This will require greater collection of data from rural EMS agencies and hospitals which are currently underrepresented in national cardiovascular disease registries.
The availability of prehospital ECG equipment alone is not enough to ensure adequate use. Even among agencies with ECG equipment, treatment by a nonparamedic EMT was associated with significantly lower prehospital ECG use compared with EMT's with paramedic certification. A survey of EMS practices in 9 states showed that only personnel with paramedic credentials were authorized to perform an ECG in 88% of agencies while only 23% and 37% of agencies authorized ECG performance at the EMT basic and intermediate level of licensure, respectively.14 Although fewer than 10% of chest pain patients in our study were transported without at least 1 member of their team having paramedic certification, gaps in certification were greatest in rural areas. The 2009 EMS protocol in North Carolina authorized individuals who hold an EMT‐basic certification or above to perform an ECG. However, only those with paramedic certification may be able to interpret the results.15 Others with lower certification may either transmit the results or call in an interpretation of the ECG provided by the device. Additional training in prehospital care STEMI care for EMTs is needed regarding the appropriate patient care chest pain patients, especially in rural areas which have the highest probability of having an all nonparamedic crew.
Limitations
An important limitation of this statewide study of patients with chest pain is that the EMS data were not linked to hospital records or registry data in NC. Therefore, we could not determine which patients with chest pain were ultimately diagnosed with STEMI or whether a prehospital ECG performed by EMS affected PCI treatment times and affected patient outcomes. In addition, this study was observational in nature and thus unmeasured confounders such as comorbidities could not be considered in the risk factor analyses. Finally, it is possible that some ECGs were performed during EMS transport, but these were not recorded in PreMIS. However, PreMIS has an ongoing data quality oversight process to detect such omissions and reduce them to a minimum.
Conclusion
Across a large geographic area prehospital ECG use increased significantly, there remain important opportunities to improve the quality of prehospital care. Increasing ECG availability in rural areas and improving EMS certification and training levels are important to address for reducing rural‐urban differences in NC EMS health care. Additionally, improving overall ECG utilization rates in more urbanized areas should also be a priority. This study highlights the value of having statewide systems in place for comprehensive EMS data collection, data analyses, and information sharing such as PreMIS in NC. This is critical for designing and implementing regional, patient‐centered health care practices for acute time‐sensitive health conditions such as STEMI and stroke. The value of such systems would be further enhanced by linking them with disease‐specific registries in order to better evaluate the impact of prehospital interventions on patient outcomes.
Sources of Funding
Dr. Glickman was supported by a Physician Faculty Scholar Award from the Robert Wood Johnson Foundation. The project described was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant KL2TR000084.
Disclosures
None.
References
- 1.Diercks DB, Kontos MC, Chen Y, Pollack CV, Jr, Wiviott SD, Rumsfeld JS, Magid DJ, Gibler WB, Cannon CP, Peterson ED, Roe MTNCDR ACTION Registry Participants Utilization and impact of pre‐hospital electrocardiograms for patients with acute ST‐segment elevation myocardial infarction: data from the NCDR (National Cardiovascular Data Registry) ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry. J Am Coll Cardiol. 2009; 53:161-166 [DOI] [PubMed] [Google Scholar]
- 2.Amit G, Cafri C, Gilutz H, Ilia R, Zahger D. Benefit of direct ambulance to coronary care unit admission of acute myocardial infarction patients undergoing primary percutaneous intervention. Int J Cardiol. 2007; 119:355-358 [DOI] [PubMed] [Google Scholar]
- 3.Rokos IC, French WJ, Koenig WJ, Stratton SJ, Nighswonger B, Strunk B, Jewell J, Mahmud E, Dunford JV, Hokanson J, Smith SW, Baran KW, Swor R, Berman A, Wilson BH, Aluko AO, Gross BW, Rostykus PS, Salvucci A, Dev V, McNally B, Manoukian SV, King SB., III Integration of pre‐hospital electrocardiograms and ST‐elevation myocardial infarction receiving center (SRC) networks: impact on Door‐to‐Balloon times across 10 independent regions. JACC Cardiovasc Interv. 2009; 2:339-346 [DOI] [PubMed] [Google Scholar]
- 4.Fosbol EL, Granger CB, Jollis JG, Monk L, Lin L, Lytle B, Xian Y, Garvey JL, Mears G, Corbett CC, Peterson ED, Glickman SW. The impact of a statewide pre‐hospital STEMI strategy to bypass hospitals without percutaneous coronary intervention capability on treatment times. Circulation. 2013; 127:604-612 [DOI] [PubMed] [Google Scholar]
- 5. The American Heart Association in collaboration with the International Liaison Committee on Science Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care. An international consensus on science. Part 7: the era of reperfusion: section 1: acute coronary syndromes (acute myocardial infarction). Circulation. 2000; 102:I172-I203 [PubMed] [Google Scholar]
- 6.Hutter AM, Weaver WED. 31st Bethesda conference. Emergency cardiac care. Task force 2: acute coronary syndromes: section 2A—prehospital issues. J Am Coll Cardiol. 2000; 35:846-853 [PubMed] [Google Scholar]
- 7.Crocco TJ, Sayre MR, Aufderheide TP. Position paper prehospital triage of chest pain patients. Prehosp Emerg Care. 2002; 6:224-228 [DOI] [PubMed] [Google Scholar]
- 8.Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK, Ornato JP. ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction). J Am Coll Cardiol. 2004; 44:E1-E211 [DOI] [PubMed] [Google Scholar]
- 9.Garvey JL, MacLeod BA, Sopko G, Hand MMNational Heart Attack Alert Program (NHAAP) Coordinating Committee Pre‐hospital 12‐lead electrocardiography programs: a call for implementation by emergency medical services systems providing advanced life support—National Heart Attack Alert Program (NHAAP) Coordinating Committee; National Heart, Lung, and Blood Institute (NHLBI); National Institutes of Health. J Am Coll Cardiol. 2006; 47:485-491 [DOI] [PubMed] [Google Scholar]
- 10.Jollis JG, Al‐Khalidi HR, Monk L, Roettig ML, Garvey JL, Aluko AO, Wilson BH, Applegate RJ, Mears G, Corbett CC, Granger CBRegional Approach to Cardiovascular Emergencies (RACE) Investigators Expansion of a regional ST‐segment‐elevation myocardial infarction system to an entire state. Circulation. 2012; 126:189-195 [DOI] [PubMed] [Google Scholar]
- 11.Mears GD, Pratt D, Glickman SW, Brice JH, Glickman LT, Cabanas JG. The North Carolina EMS data system: a comprehensive integrated emergency medical services quality improvement program. Prehosp Emerg Care. 2010; 14:85-94 [DOI] [PubMed] [Google Scholar]
- 12.Cooper MM. (ed.). In: Cooper MM. (ed.). Part one: the geography of health care in the United States. The Dartmouth Atlas of Health Care. 1996Chicago, Illinois: American Hospital Publishing, Inc; 11-36 [Google Scholar]
- 13.Howard G, Howard VJ, Katholi C, Oli MK, Huston S. Decline in US stroke mortality: an analysis of temporal patterns by sex, race, and geographic region. Stroke. 2001; 32:2213-2220 [DOI] [PubMed] [Google Scholar]
- 14.Williams I, Valderrama AL, Bolton P, Greek A, Greer S, Patterson DG, Zhang Z. Factors associated with emergency medical services scope of practice for acute cardiovascular events. Prehosp Emerg Care. 2012; 16:189-197 [DOI] [PubMed] [Google Scholar]
- 15.Paramedic national standard curriculum. Available at http://www.ems.gov/EducationStandards.htm. Accessed April 24, 2013.


