Abstract
Objectives. We assessed the impact of the minimum legal drinking age (MLDA) on hospital-based treatment for alcohol-related conditions or events in Ontario, Canada.
Methods. We conducted regression–discontinuity analyses to examine MLDA effects with respect to diagnosed alcohol-related conditions. Data were derived from administrative records detailing inpatient and emergency department events in Ontario from April 2002 to March 2007.
Results. Relative to youths slightly younger than the MLDA, youths just older than the MLDA exhibited increases in inpatient and emergency department events associated with alcohol-use disorders (10.8%; P = .048), assaults (7.9%; P < .001), and suicides related to alcohol (51.8%; P = .01). Among young men who had recently crossed the MLDA threshold, there was a 2.0% increase (P = .01) in hospitalizations for injuries.
Conclusions. Young adults gaining legal access to alcohol incur increases in hospital-based care for a range of serious alcohol-related conditions. Our regression–discontinuity approach can be used in future studies to assess the effects of the MLDA across different settings, and our estimates can be used to inform cost-benefit analyses across MLDA scenarios.
Given that alcohol consumption contributes to a substantial burden of disability and mortality among young people,1 most countries worldwide have implemented minimum legal drinking age (MLDA) legislation that seeks to reduce alcohol-related harm among youths by imposing age restrictions on the purchasing, possession, and consumption of alcohol.2,3 Although a large body of work has attempted to assess the impact of MLDA laws,2,4,5 this literature has focused primarily on assessments of patterns of alcohol consumption or motor vehicle accidents (MVAs) in the United States. As a result, the current literature likely underestimates the full impact of the MLDA on morbidity, especially alcohol-related conditions resulting in health service use in hospital settings. For example, a recent cost-effectiveness study of population-based interventions designed to reduce alcohol-related morbidity in Canada considered the effects of the MLDA only on MVAs.6
Understanding the full role of MLDA legislation in alcohol-related harm is a critical aspect of evidence-based policies, and an earlier Canadian study we conducted showed that the MLDA has a substantial impact on inpatient hospital admissions for a range of serious alcohol-related conditions.7 The study’s findings revealed that, relative to youths slightly younger than the MLDA, those slightly older than the MLDA exhibited significant increases in admissions for alcohol-use disorders (16%-20%; P ≤ .001) and self-inflicted injuries (9.6%; P = .03). Among young men who had recently crossed the MLDA threshold, there was a significant 4.4% increase (P = .001) in hospitalizations for external injuries, including a 9.2% jump (P = .02) in admissions for MVAs. However, this earlier study relied exclusively on inpatient admissions and, thus, probably captured only a small (but extremely costly) proportion of total alcohol-related health service use in hospital settings.
In the present study, we addressed this limitation by examining integrated inpatient and emergency department records from Canada’s most populous province, Ontario, which has an MLDA of 19 years. Use of inpatient and emergency department records from Ontario—a setting with universal access to physician and hospital-based services—allowed us to make comprehensive, population-based estimates of alcohol-related health service use in hospital settings without the potential biases resulting from variations in patients’ medical insurance status.
We used a regression-discontinuity (RD) approach8,9 (a quasi-experimental approach that can provide credible estimates of the causal effect of an intervention on a specified outcome10) in our study. The RD design allowed us to take advantage of the sharp discontinuity in the legality of alcohol purchasing and consumption occurring at the MLDA. We assigned youths who had not reached the MLDA and youths no longer subject to the MLDA to separate groups. The basic, underlying assumption of our RD approach was that, with the exception of the effect of the removal of the MLDA in the latter group, individuals slightly older than the MLDA and those slightly younger than the MLDA would be similar in terms of observed (and unobserved) characteristics. This seemed to be a reasonable assumption given the likelihood that individuals separated by only a single month in age on either side of the MLDA would have similar characteristics related to our outcome variables (other than the impact of the MLDA in the older group).
Our design also assumed that all observed and unobserved variables (which might influence alcohol-related morbidity outcomes) were smoothly distributed across the age cutoff11 and that the effects of the MLDA could be inferred if the regression line showed a discontinuity—a change in intercept—at the MLDA cutoff.12 Another major advantage of our approach is that the results can be clearly represented by simple scatterplots showing changes in rates of the outcome variables before and after the legal drinking age.
We expected significant increases in hospital-based health service use for alcohol-related conditions to appear abruptly just after the MLDA. In light of the ongoing, vigorous debate about lowering the MLDA in the United States,13 as well as evidence-based recommendations for raising the MLDA to 21 years in Australia,14,15 it is critical for well-supported alcohol policies to integrate a full assessment of the impact of the MLDA on alcohol-related morbidity, a neglected area in the current literature.
METHODS
Data on all Ontario inpatient and emergency department events from April 1, 2002, to March 31, 2007, among individuals aged 16 to 22 years were drawn from the Canadian Institute for Health Information’s Hospital Morbidity Database (a national database capturing administrative, clinical, and demographic information on all hospital inpatient events) and the National Ambulatory Care Reporting System (a national database designed to capture information on ambulatory care visits). During the study period, the Hospital Morbidity Database included information from approximately 170 acute care facilities in Ontario,16 and the National Ambulatory Care Reporting System included data from approximately 180 emergency departments across the province.17
At the time of our initial data request (2008), Ontario was the only Canadian province that had comprehensive coverage of linked inpatient–emergency department records available from the Canadian Institute for Health Information. Reabstraction studies have demonstrated the validity of the diagnostic information contained in the Hospital Morbidity Database by showing a high correspondence between information in electronic records and in paper-based medical charts.18,19
Outcomes
Control condition: appendicitis.
We selected appendicitis as the primary diagnostic control condition because it is a relatively frequent reason for presentation to hospital-based settings, it is not associated with socioeconomic status,20 it does not appear on theoretical grounds to be related to alcohol-related conditions, and it has a well-defined clinical course.21
Alcohol-related conditions.
We used the Centers for Disease Control and Prevention’s classification of alcohol-related medical conditions as a general framework to define our outcomes.22 We selected the following conditions as our primary outcomes: alcohol-use disorders, external injuries, suicides by and exposure to alcohol (“suicides related to alcohol”), suicides broadly defined, MVAs, and assault (International Classification of Diseases, 10th Revision [ICD-10] codes for the medical conditions assessed in this study are presented in Table A, available as a supplement to the online version of this article at http://www.ajph.org). Injury classifications also followed Centers for Disease Control and Prevention definitions and included suicides, MVAs, and assaults along with a number of other injury-related conditions. The outcomes represented diagnosed conditions seen in inpatient and emergency department settings; it was not possible to assess whether an individual died as a result of the diagnosed condition or other conditions.
Analytic Plan
We conducted RD analyses to estimate the impact of the MLDA on alcohol-related use of inpatient and emergency department services in Ontario. Patient ages were collapsed into month and year of birth. For each alcohol-related outcome, we summed the number of outcome events for each age group, defined as age in months in relation to the Ontario MLDA. For example, Ontario adolescents aged 18.5 years were placed into the “−6 months from the MLDA” age category, given the Ontario MLDA of 19 years. To account for potential variability in the total number of inpatient and emergency department events across calendar years and ages, we converted outcomes into rates per 1000 hospital events within each age group.
We used the following mathematical formula in our RD analyses:
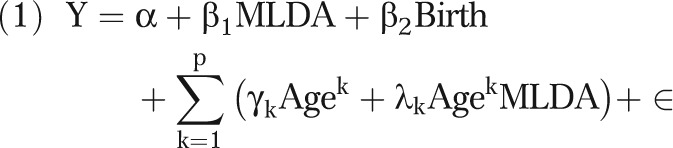 |
The term Y is the number of outcome-related presentations per 1000 hospital episodes; MLDA is the legal drinking age indicator, and its coefficient β1 is the estimate of the MLDA effect (MLDA was coded as 1 if the individual was at least 19 years old, the MLDA in Ontario); birth is the indicator of birthday month (which accommodates “birthday-celebration” effects occurring at the MLDA and all other birthdays in the data span); age (in months) is a running variable centered at the MLDA (with P = 1,2,3 representing the degree of the polynomial equation across ages; this includes the MLDA × Age interaction term, which allows for different regression equations before and after the MLDA cutoff); α is the intercept, which is the estimate of the baseline hospital-event rate (i.e., the rate just before to the legislated MLDA) of each outcome variable; and ɛ is the error term.
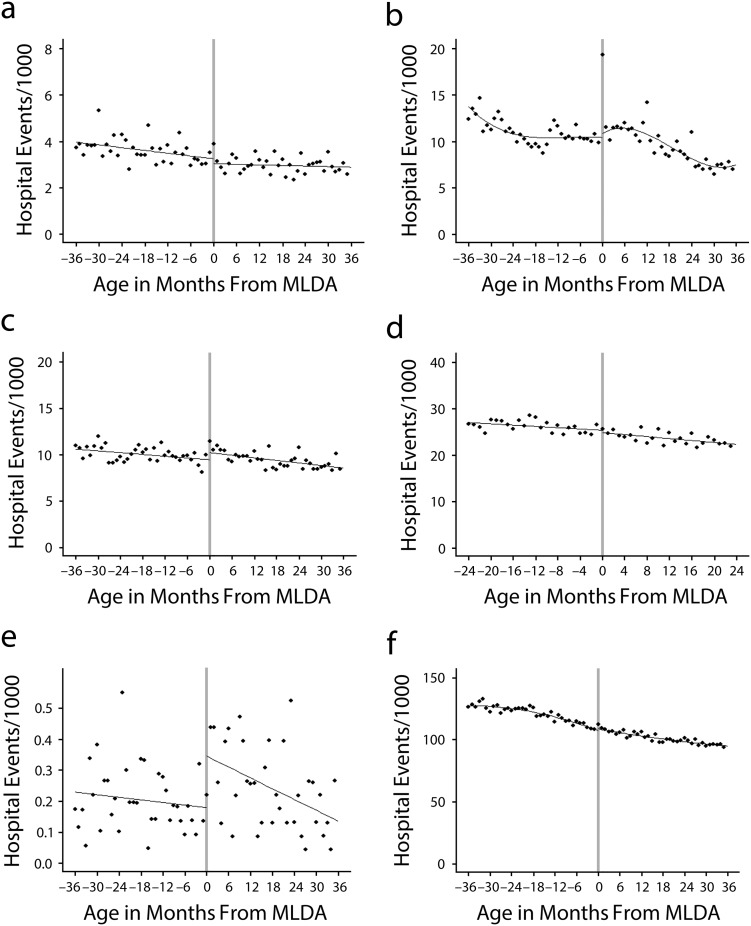
Our approach followed recent best-practices guidelines for RD analyses.12 We undertook parametric regression analyses that included linear, quadratic, and cubic terms for the running variable age. For example, in our tabled results, we refer to models including the quadratic term for age as quadratic, and the models incorporating the cubic term for age are labeled as cubic. Regarding model selection, we chose the cubic model when the cubic term for age in equation 1 was statistically significant, the quadratic model when the quadratic term for age was statistically significant (but not the cubic term), and a linear model when neither the cubic nor the quadratic term was statistically significant. The algorithm used to select the best model followed the standard rationale for model selection in regression analyses.23,24 Regression models were run for the total sample, as well as separately for young men and young women. Figure 1 presents the scatterplots for the selected best regression models for the sample as a whole.
FIGURE 1—
Rates of hospital treatment for (a) appendicitis, (b) alcohol-use disorders, (c) alcohol-related assaults, (d) alcohol-related motor vehicle accidents, (e) alcohol-related suicides, and (f) alcohol-related external injuries Ontario, 2002–2007.
Note. MLDA = minimum legal drinking age.
To explore the robustness of the parametric regression results, we also conducted local linear regression analyses with different bandwidths (i.e., smoothing parameters). Local regression can be viewed as a smoothing technique that attempts to estimate a model on each point by smoothing through a set of other points in the neighborhood, giving greater weight to proximal data points. The bandwidth defines how many points in the neighborhood set will be used to estimate the regression model at a given point. The larger the bandwidth, the smoother the regression model will be because more data points are included in the model. For example, in a local regression analysis with a bandwidth of 20, 20 data points are used in each local regression iteration. We used the Stata version 11 (StataCorp LP, College Station, TX) RD macro,25 which calculates optimum bandwidths and local regression models, in fitting our models.26 As recommended, we used 0.5, 1.0, 1.5, and 2.0 multiples of the optimal bandwidth in conducting our sensitivity analyses.25
RESULTS
The overall rate of hospital events among young men and young women of varying ages (centered at the MLDA) was approximately 40 000 per month across the study period (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). No MLDA-specific group differences in event rates were observed for our primary control medical condition (appendicitis).
Key findings from our RD analyses related to appendicitis (control condition), alcohol-use disorder, and assault outcomes are shown in Table 1, and findings with respect to MVAs, suicides related to alcohol, and external injuries can be found in Table 2. Youths who had recently crossed the MLDA threshold (relative to youths who were slightly younger than the MLDA) exhibited significant overall increases in the numbers of inpatient and emergency department events associated with alcohol-use disorders, assaults, and suicides related to alcohol (Figure 1). There was no evidence of a significant increase in the broad category of suicide-related events (Table 1). Events related to alcohol-use disorders showed an approximate rate increase of 10.8% overall among youths just older than the MLDA in comparison with their slightly younger counterparts (who had a rate of 14 alcohol-use disorder events per 1000 episodes; Figure 1). Among young men who had recently crossed the MLDA threshold, there was a significant 15.3% increase in alcohol-use disorder events in relation to the corresponding rate among young men still under MLDA restrictions (Figure B, available as a supplement to the online version of this article at http://www.ajph.org), but the increase among young women was not significant.
TABLE 1—
Regression-Discontinuity Models for Suicides, Alcohol-Use Disorders, and Assaults: Young Women and Men in Ontario, 2002–2007
| Suicide Broadly Defined |
Alcohol-Use Disorders |
Assaults |
|||||||
| Total | Female | Male | Total | Female | Male | Total | Female | Male | |
| Linear, b (95% CI) | −0.07 (−0.37, 0.22)a | −0.13 (−0.56, 0.29)a | 0.02 (−0.38, 0.43)a | 2.50*** (1.51, 3.49) | 2.50*** (1.46, 3.55) | 2.55*** (1.33, 3.78)a | 1.99*** (1.17, 2.81)a | 0.77* (0.09, 1.46)a | 3.64*** (2.12, 5.16)a |
| Quadratic, b (95% CI) | 0.11 (−0.58, 0.36) | −0.38 (−1.04, 0.27) | 0.20 (−0.43, 0.82) | 1.51* (6.08, 10.58)a | 1.02 (−0.52, 2.57) | 2.18* (0.29, 4.08) | 2.08*** (0.81, 3.34) | 1.26* (0.19, 2.33) | 3.59** (1.25, 5.92) |
| Cubic, b (95% CI) | 0.09 (−0.56, 0.74) | 0.09 (−0.82, 1.00) | 0.08 (−0.78, 0.96) | 1.10 (−0.97, 3.16) | 0.46 (−1.66, 2.57)a | 2.03 (−0.64, 4.71) | 2.21* (0.41, 4.01) | 2.01** (0.51, 3.51) | 3.35* (0.02, 6.68) |
| Bandwidth, b (95% CI) | |||||||||
| 3 | 0.68*** (0.42, 0.93) | 0.08* (0.01, 0.14) | 1.37*** (0.73, 2.02) | 8.99*** (4.58, 13.39) | 9.78*** (6.67, 12.90) | 8.07*** (2.25, 13.89) | 4.07*** (1.96, 6.18 | −0.79 (−1.24, 0.06) | 9.51*** (6.24, 12.77) |
| 5 | 0.22 (−0.24, 0.68) | 0.03 (−0.21, 0.15) | 0.51 (−0.47, 1.49) | 7.19* (0.66, 13.72) | 7.01** (1.65, 12.37) | 7.42 (−0.61, 15.44) | 5.09*** (2.74, 7.44) | 1.59 (−0.77, 3.94) | 9.32*** (5.26, 13.38) |
| 10 | 0.28 (−0.11, 0.68) | 0.24 (−0.18, 0.66) | 0.32 (−0.40, 1.04) | 5.60 (−0.26, 11.45) | 4.81 (−0.38, 10.00) | 6.62 (−0.17, 13.40) | 3.65*** (1.55, 5.74) | 2.06** (0.50, 3.63) | 6.03** (2.18, 9.88) |
| 20 | 0.08 (−0.26, 0.42) | −0.11 (−0.49, 0.27) | 0.38 (−0.20, 0.81) | 3.94* (−0.09, 7.79) | 3.28 (−0.17, 6.72) | 4.79* (−0.39, 9.20) | 2.87*** (1.32, 4.41) | 1.70 (0.73, 2.68) | 4.64*** (1.81, 7.46) |
| Intercept | |||||||||
| Linear | 2.64 | 2.78 | 2.44 | 12.93 | 9.72 | 16.65 | 25.31 | 9.50 | 43.76 |
| Quadratic | 2.68 | 3.10 | 2.20 | 13.94 | 10.98 | 17.42 | 24.84 | 9.41 | 42.94 |
| Cubic | 2.40 | 2.71 | 2.04 | 13.42 | 10.43 | 16.89 | 24.54 | 8.85 | 42.77 |
| Effect,b % | |||||||||
| Linear | −2.7a | −4.8a | 0.9a | 19.3 | 25.7 | 15.3a | 7.9a | 8.1a | 8.3a |
| Quadratic, | −4.1 | −12.4 | 8.9 | 10.8a | 9.3 | 12.5 | 8.4 | 13.4 | 8.3 |
| Cubic | −3.7 | 3.3 | 3.9 | 8.2 | 4.4a | 12.0 | 9.0 | 22.7 | 7.8 |
| Optimum bandwidthc | 5.0 | 5.6 | 4.7 | 7.5 | 6.2 | 8.5 | 5.1 | 5.2 | 6.7 |
| Optimum bandwidth result, b (95% CI) | 0.22 (−0.24, 0.68) | 0.01 (−0.18, 0.17) | 0.55 (−0.39, 1.04) | 6.07 (−0.32, 12.43) | 6.15* (0.70, 11.59) | 6.69 (−0.55, 13.92) | 4.99*** (2.84, 7.14) | 1.72 (−0.45, 3.89) | 7.53*** (3.99, 11.08) |
| No. of eventsd | 130 | 68 | 62 | 1008 | 440 | 568 | 1255 | 261 | 994 |
Note. CI = confidence interval. Values are the coefficients of the minimum legal drinking age (MLDA) indicators in the regression model and, therefore, indicate the change in hospital events per 1000 admissions among youths at the MLDA threshold. Bandwidths refer to the bandwidth values used in the local regression models. Bandwidths of 3, 5, 10, and 20 represent the approximate multiples used (approximately 6 across models). The age range was 16 to 22 years of age for all outcomes.
Results from the best parametric regression model.
Percentage change in hospital events among youths at the MLDA threshold (the coefficient of the MLDA indicator divided by the intercept of the model).
A parameter indicating the best set of points to be used in the local linear regression to minimize error variance.
Unadjusted count of outcome events appearing in the age category immediately following the minimum legal drinking age. For example, in the first column, there are 130 suicide events in the age category including ages from the MLDA up to 1 month after the MLDA.
*P ≤ .05; **P ≤ .01; ***P ≤ .001.
TABLE 2—
Regression-Discontinuity Models for Motor Vehicle Accidents, Suicides Related to Alcohol, and External Injuries: Young Women and Men in Ontario, 2002–2007
| Motor Vehicle Accidents |
Suicides Related to Alcohol |
External Injuries |
|||||||
| Total | Female | Male | Total | Female | Male | Total | Female | Male | |
| Linear, b (95% CI) | −0.62 (−1.59, 0.35)a | −0.54 (−1.86, 0.79)a | −0.64 (−2.04, 0.75)a | 0.10** (0.03, 0.18)a | 0.17** (0.06, 0.28)a | 0.02 (−0.07, 0.12)a | 0.19 (−2.00, 2.38) | −3.00* (−5.34, −0.66) | 4.33* (1.01, 7.64)a |
| Quadratic, b (95% CI) | −0.26 (−1.79, 1.28) | 0.31 (−1.78, 2.40) | −0.80 (−3.06, 1.45) | 0.10 (−0.02, 2.13) | 0.24** (0.07, 0.41) | −0.07 (−0.21, 0.07) | 2.26 (−0.95, 5.48)a | 1.39 (−1.90, 4.68)a | 5.13 (−0.04, 1.03) |
| Cubic, b (95% CI) | −0.76 (−3.03, 1.51) | −0.21 (−3.26, 2.84) | −1.32 (−4.59, 1.94) | 0.05 (−0.12, 0.21) | 0.21 (−0.04, 0.45) | −0.15 (−0.35, 0.05) | 2.74 (−1.84, 7.32) | 2.26 (−2.42, 6.95) | 6.16 (−1.21, 1.35) |
| Bandwidth, b (95% CI) | |||||||||
| 3 | −2.87*** (−2.89, −2.85) | −3.35*** (−4.25, −2.46) | −2.30*** (−3.37, −1.23) | 0.13*** (0.08, 0.17) | 0.29*** (0.18, 0.40) | −0.06 (−0.29, 0.17) | 9.46*** (8.34, 10.58) | 4.32*** (3.04, 5.61) | 15.52*** (14.58, 16.45) |
| 5 | −1.24 (−2.75, 0.28) | −1.31 (−3.20, 0.59) | −1.14 (−2.49, 0.22) | 0.02 (−0.10, 0.13) | 0.12 (−0.19, 0.42) | −0.10 (−0.34, 0.142) | 8.00*** (5.03, 10.98) | 5.24*** (2.94, 7.84) | 11.75*** (5.25, 18.25) |
| 10 | −0.10 (−1.84, 1.63) | −0.19 (−2.12, 1.73) | 0.06 (−1.74, 1.87) | 0.03 (−0.06, 0.13) | 0.14 (−0.08, 0.35) | 0.89 (−0.32, 0.14) | 5.51*** (2.39, 8.62) | 3.35** (1.17, 5.54) | 9.75*** (5.71, 13.80) |
| 20 | −0.28 (−1.40, 0.85) | 0.17 (−1.14, 1.48) | −0.74 (−2.18, 0.70) | 0.09* (0.03, 0.32) | 0.18* (0.03, 0.32) | −0.01 (−0.15, 0.13) | 3.63** (0.15, 5.98) | 1.60 (−0.56, 3.75) | 6.06** (1.51, 10.62) |
| Intercept | |||||||||
| Linear | 27.39 | 25.4 | 29.7 | 0.19 | 0.18 | 0.207 | 161.49 | 111.2 | 220.44 |
| Quadratic | 26.81 | 24.52 | 29.47 | 0.14 | 0.12 | 0.173 | 158.83 | 107.66 | 218.79 |
| Cubic | 27.02 | 25.36 | 28.93 | 0.19 | 0.18 | 0.189 | 158.4 | 107.2 | 218 |
| Effect,b % | |||||||||
| Linear | −2.3a | −2.1a | −2.2a | 51.8a | 91.8a | 11.6a | 0.1 | −2.7 | 2.0a |
| Quadratic, | −1.0 | 1.3 | −2.7 | 68.5 | 204.7 | −39.9 | 1.4a | 1.3a | 2.3 |
| Cubic | −2.8 | −0.8 | −4.6 | 25.3 | 112.0 | −77.2 | 1.7 | 2.1 | 2.8 |
| Optimum bandwidthc | 6.7 | 6.7 | 6.9 | 2.5 | 2.8 | 3.8 | 8.1 | 8.9 | 7.3 |
| Optimum bandwidth result, b (95% CI) | −0.08 (−2.40, 2.24) | −0.33 (−2.71, 2.05) | 0.36 (−2.12, 2.85) | 0.13*** (0.10, 0.16) | 0.29*** (0.19, 0.39) | −0.11 (−0.33, 0.12) | 6.49*** (3.50, 9.49) | 3.71*** (1.43, 5.99) | 11.42*** (8.05, 14.80) |
| No. of eventsd | 1154 | 585 | 569 | 11 | 5 | 6 | 7033 | 2568 | 4465 |
Note. CI = confidence interval. Values are the coefficients of the minimum legal drinking age (MLDA) indicators in the regression model and, therefore, indicate the change in hospital events per 1000 admissions among youths at the MLDA threshold. Bandwidths refer to the bandwidth values used in the local regression models. Bandwidths of 3, 5, 10, and 20 represent the approximate multiples used (approximately 6 across models). The age range was 16 to 22 years for all outcomes, except for motor vehicle accidents for which the age range was 17 to 21 years.
Results from the best parametric regression model.
Percentage change in hospital events among youths at the MLDA threshold (the coefficient of the MLDA indicator divided by the intercept of the model).
A parameter indicating the best set of points to be used in the local linear regression to minimize error variance.
Unadjusted count of outcome events appearing in the age category immediately following the minimum legal drinking age. For example, in the first column, there are 1154 motor vehicle accidents in the age category including ages from the MLDA up to 1 month after the MLDA.
*P ≤ .05; **P ≤ .01; ***P ≤ .001.
The overall rate of assault events among youths slightly older than the MLDA rose by approximately 7.9% relative to youths slightly younger than the MLDA (Figure 1). Assault events increased significantly for both genders: 8.3% among young men (Figure B) and 8.1% among young women (Figure C, available as a supplement to the online version of this article at http://www.ajph.org).
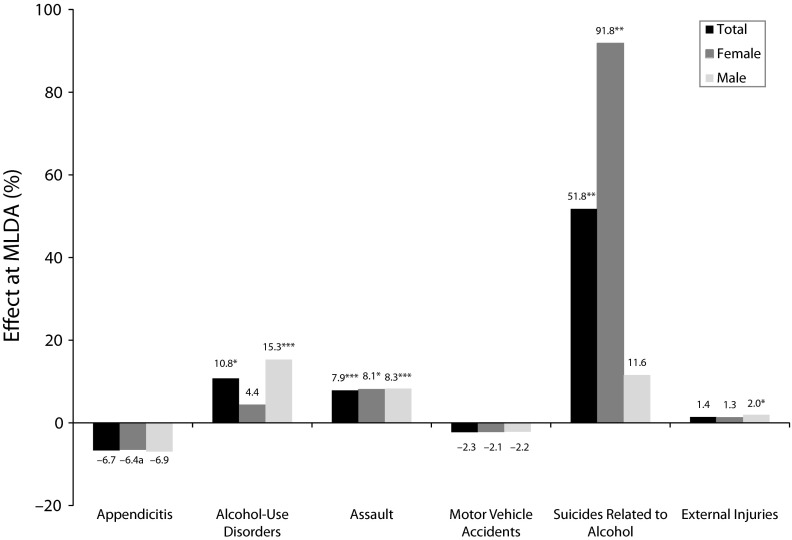
In comparison with youths still under MLDA restrictions, youths who had crossed the MLDA threshold showed a 51.8% increase in events classified as suicides related to alcohol (the pre-MLDA baseline rate was 0.2 events per 1000 episodes; Figure 1). It is important to note that young women who had just crossed the threshold of the MLDA showed a statistically significant increase of 91.8% in suicides related to alcohol (relative to the pre-MLDA baseline of 0.17 events per 1000 episodes; Figure A); in contrast, no significant change was found for young men (Figure B). Surprisingly, no relationship was found between MVA events and the MLDA transition (Figure 1). Also, young men just older than the MLDA exhibited a significant increase of 2.0% in events included in the broad ICD-10 category of external injuries (the baseline pre-MLDA rate was 220 events per 1000 episodes; Figure B), whereas no change was observed among young women. Figure 2 summarizes the MLDA effects across outcomes.
FIGURE 2—
Rate changes in alcohol-related hospital events at the minimum legal drinking age (MLDA): Ontario, 2002–2007.
Note. The rate change was calculated as follows: [(post-MLDA regression Y intercept value − pre-MLDA regression Y intercept value)/pre-MLDA regression Y intercept value]. For example, the overall rate change for alcohol-use disorders was 10.8% [(15.44 − 13.94)/13.94]—immediately following the MLDA.
*P ≤ .05; **P ≤ .01; ***P ≤ .001.
As noted, we also conducted local linear regression analyses with varying bandwidths to evaluate the reliability of our findings. The results showed that the optimal bandwidth across our nonlinear models was approximately 5, and, as a result, we constructed local linear models with bandwidths of 3, 5, 10, and 20 to assess the reliability of our parametric models. In general, the nonparametric models supported our primary linear regression results.
In addition, we reiterated our primary parametric models with mock MLDA age cutoffs for the aggregated data across provinces. For example, we selected mock MLDAs of 18 and 20 years (the Ontario MLDA is 19 years) and reiterated our primary RD analyses. As expected, we did not find any significant increases at the specified MLDA in any of the outcomes (data not shown).
Given the relatively small number of suicides related to alcohol and the possibility that our RD models were unduly influenced by outliers in this outcome, we identified outliers using a widely accepted strategy.27 We selected quartile points in the distribution (Q1, Q2, and Q3); calculated an interquartile range, defined as Q1 to Q3; and then defined outliers as those points extending beyond values at Q1 or Q3 farther than 150% of the interquartile range. We removed these outliers from the sensitivity analyses. Removal of outliers did not affect the evidence of statistically significant jumps immediately following the MLDA; therefore, our final models included all available points.
We also included a secondary control condition, asthma, as an outcome. We found that it was smoothly distributed across the MLDA transition for both young men and young women, as expected; however, in the combined sample there was some evidence of a very modest but statistically significant increase appearing directly after the MLDA threshold (data not shown).
Given the unexpected null results regarding our MVA outcomes, we conducted sensitivity RD analyses on MVA data found in the 2002 through 2007 Ontario inpatient-only records. The results demonstrated no evidence of a significant jump in MVAs immediately following the MLDA.
DISCUSSION
We found that young adults making the transition across the MLDA had significant increases in serious alcohol-related inpatient and emergency department events for alcohol-use disorders, suicides related to alcohol, and assaults. In addition, young men had significant jumps in hospital-based episodes for a broad class of injury conditions. Given that the major assumptions of our RD approach were met, this analytic approach can provide reasonable estimates of the causal impact of the MLDA on serious alcohol-related morbidity in Ontario hospital settings.
Our findings demonstrated a significant 11% increase in inpatient and emergency department admissions for alcohol-use disorders among youths who had just crossed the MLDA threshold. A large body of research has consistently shown that removing the strictures of MLDA legislation is associated with elevated patterns of alcohol consumption, especially heavy episodic drinking,2,28–31 as well as sharp increases in inpatient hospital events related to alcohol-use disorders or poisoning.7 Previous RD analyses involving statewide inpatient or emergency department data from 5 US states (Arizona, New York, Texas, New Jersey, and Wisconsin) revealed significant and comparatively larger increases in alcohol intoxication events (as defined in the ICD-9) just after the threshold of the MLDA; emergency department visits related to these events rose by approximately 50%, and inpatient hospitalizations increased by 26%.32
Given the evidence from previous research that excessive alcohol consumption can influence suicidal behavior among young people through a number of causal mechanisms, increases in alcohol consumption among young adults may lead to increases in suicide-related events at the population level.33–35 Previous US-based work comparing states with different MLDAs showed that lower MLDAs were associated with increases in completed suicides of approximately 8% to 10%,36,37 and an RD study in which national US death certificate data were used revealed a 16% rise in suicide deaths at the age of 21 years, the legislated MLDA in the United States.29
However, research examining the impact of the MLDA on nonfatal suicide events has produced mixed results. Whereas our previous Canadian RD study involving national inpatient data revealed a 9.2% increase in suicide-related hospital events among youths who had just crossed the MLDA threshold,7 the present Ontario-based study showed no evidence of a significant jump in suicide outcomes (defined broadly) just after the MLDA. However, we did find evidence of significant increases in those relatively infrequent suicide outcomes coded as directly resulting from hazardous alcohol consumption, although the relatively low numbers of these outcomes may underpin the large effects shown in Figure 2.
In a similar way, Carpenter and Dobkin, examining inpatient and emergency department data from 5 US states, found no evidence of statistically significant increases in nonfatal suicide events at the transition across the MLDA.32 Although the data are limited, it is possible to speculate that the MLDA has an impact on patterns of completed suicides but more limited or variable effects on nonfatal suicide-related events treated in hospital settings.
We found that the transition across the MLDA was associated with a significant 8% increase in assault-related hospital events among both young men and young women. Many epidemiological studies have supported strong theoretical and empirical links between alcohol-use and assault-related injuries among young people.38–43 In particular, a US-based RD study showed that, in comparison with youths just younger than the MLDA, those who were just older exhibited an 11% increase in assault-related visits to statewide emergency department settings.32 Our findings are in agreement with recent research demonstrating that alcohol increases aggression across both genders, but much more so among men.44 The current literature has not, to our knowledge, addressed how alcohol-related legislation might affect assault victimization, and thus our study contributes important initial estimates of the impact of MLDA policies on population-level assault rates.
Previous work has provided evidence supporting the causal link between alcohol consumption and injuries,45,46 including those resulting from MVAs.2,4,5 Although we found significantly increased rates of a broad class of injuries occurring immediately after the MLDA among young men, we were surprised that our results did not show evidence of significant upward discontinuities in injuries due to MVAs. The present findings are inconsistent with our previous work (based on comprehensive 1996–2006 Canadian inpatient data) demonstrating that young men exhibited a 9.2% increase in national MVA inpatient hospital events immediately after the MLDA,7 as well as the conclusions of reviews in this area.2,5
One possible explanation for our null results is the relatively low incidence of driving after drinking among college-aged young people in Ontario, where the prevalence of this risk behavior is the lowest in Canada (students from Ontario are at half the risk of alcohol-impaired driving relative to students from other regions of Canada) and also much lower than that reported among college students in the United States. For example, in 2004, 4.4% of Ontario university students reported “driving after drinking too much” in the preceding year,39 whereas a much larger percentage (20% to 34%) of their US college counterparts indicated “drinking and driving under the influence of alcohol” or driving “while drunk or intoxicated” in the preceding year.38,47
Limitations
Our study involved a number of limitations. For example, our approach captured only those alcohol-related events that resulted in hospital-based care. In addition, even though our study took place in a setting with universal health care, it is possible that underage youths avoided hospital-based medical attention because of a fear of legal consequences. However, in Ontario, inpatient and emergency department services are not closely aligned with enforcement services, and it seems unlikely that such avoidance would be prominent enough to affect our results.
In our RD design, we assumed that all observed and unobserved variables that might influence the outcomes were smoothly distributed across the age cutoff. Given the very limited nature of the variables contained in the medical records, we were not able to assess this assumption in a meaningful way. As a result, it is important to acknowledge that variables unaccounted for in our analyses could have influenced our results, especially variables differentially influencing individuals on either side of the MLDA threshold.
Conclusions
MLDA legislation stands as a central component in youth alcohol control policies not only in Canada but worldwide. As a result, it is critical to understand the impact of this legislation on the full spectrum of alcohol-related morbidity and mortality. Our study demonstrates that significant and abrupt increases in alcohol-use disorders, assault victimization, and suicides (entirely attributable to alcohol) occur immediately after the MLDA. In addition, young men making the transition across the MLDA exhibit significant increases in hospital-based episodes for a broad class of injuries.
Given the ongoing international debates about the MLDA, our study makes an important contribution by providing comprehensive, population-based estimates of the impact of the MLDA on serious and costly alcohol-related health service use in hospital settings. Future studies can draw on our RD approach to assess the effects of the MLDA across various settings and can use our estimates to inform cost-benefit analyses across different MLDA scenarios.
Acknowledgments
This research was supported by an institutional grant from the Ontario Ministry of Health and Long-Term Care to the Centre for Addiction and Mental Health.
We thank Stephen Kish for his careful reading of the article.
Human Participant Protection
This study was approved by the institutional review board of the Centre for Addiction and Mental Health. No protocol approval was needed because deidentified data were used.
References
- 1.Gore FM, Bloem PJ, Patton GC et al. Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet. 2011;377(9783):2093–2102. doi: 10.1016/S0140-6736(11)60512-6. [DOI] [PubMed] [Google Scholar]
- 2.Wagenaar AC, Toomey TL. Effects of minimum drinking age laws: review and analyses of the literature from 1960 to 2000. J Stud Alcohol Suppl. 2002;14:206–225. doi: 10.15288/jsas.2002.s14.206. [DOI] [PubMed] [Google Scholar]
- 3.International Center for Alcohol Policies. Minimum age limits worldwide. Available at: http://www.icap.org/Table/MinimumAgeLimitsWorldwide. Accessed May 22, 2013.
- 4.McCartt AT, Hellinga LA, Kirley BB. The effects of minimum legal drinking age 21 laws on alcohol-related driving in the United States. J Safety Res. 2010;41(2):173–181. doi: 10.1016/j.jsr.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 5.Shults RA, Elder RW, Sleet DA et al. Reviews of evidence regarding interventions to reduce alcohol-impaired driving. Am J Prev Med. 2001;21(suppl 4):66–88. doi: 10.1016/s0749-3797(01)00381-6. [DOI] [PubMed] [Google Scholar]
- 6.Rehm J, Patra J, Gnam WH, Sarnocinska-Hart A, Popova S. Avoidable cost of alcohol abuse in Canada. Eur Addict Res. 2011;17(2):72–79. doi: 10.1159/000321463. [DOI] [PubMed] [Google Scholar]
- 7.Callaghan RC, Sanches M, Gatley JM. Impacts of the minimum legal drinking age legislation on alcohol-related inpatient morbidity in Canada, 1997–2007: a regression-discontinuity approach. Addiction. 2013 doi: 10.1111/add.12201. Epub ahead of print May 17, 2013. [DOI] [PubMed] [Google Scholar]
- 8.Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston, MA: Houghton Mifflin; 2002. [Google Scholar]
- 9.Thistlethwaite DL, Campbell DT. Regression-discontinuity analysis: an alternative to the ex post facto experiment. J Educ Psychol. 1960;51(6):309–317. [Google Scholar]
- 10.Lee DS, Lemieux T. Regression discontinuity designs in economics. J Econ Lit. 2010;48(2):281–355. [Google Scholar]
- 11.Hahn J, Todd P, Van der Klaauw W. Identification and estimation of treatment effects with a regression-discontinuity design. Econometrica. 2001;69(1):201–209. [Google Scholar]
- 12.Imbens GW, Lemieux T. Regression discontinuity designs: a guide to practice. J Econ. 2007;142(2):615–635. [Google Scholar]
- 13.Wechsler H, Nelson TF. Will increasing alcohol availability by lowering the minimum legal drinking age decrease drinking and related consequences among youths? Am J Public Health. 2010;100(6):986–992. doi: 10.2105/AJPH.2009.178004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cobiac L, Vos T, Doran C, Wallace A. Cost-effectiveness of interventions to prevent alcohol-related disease and injury in Australia. Addiction. 2009;104(10):1646–1655. doi: 10.1111/j.1360-0443.2009.02708.x. [DOI] [PubMed] [Google Scholar]
- 15.Doran CM, Hall WD, Shakeshaft AP, Vos T, Cobiac LJ. Alcohol policy reform in Australia: what can we learn from the evidence? Med J Aust. 2010;192(8):468–470. doi: 10.5694/j.1326-5377.2010.tb03589.x. [DOI] [PubMed] [Google Scholar]
- 16.Executive Summary: Data Quality Documentation, Hospital Morbidity Database (HMDB) 2004–2005. Ottawa, Ontario: Canadian Institute for Health Information; 2006. [Google Scholar]
- 17.Database Background Documentation: National Ambulatory Care Reporting System (NACRS) FY 2003–2004. Ottawa, Ontario: Canadian Institute for Health Information; 2004. [Google Scholar]
- 18.Reabstraction Study of the Ontario Case Costing Facilities: For Fiscal Years 2002/2003 and 2003/2004. Ottawa, Ontario: Canadian Health Information Management Association and Canadian Institute for Health Information; 2005. [Google Scholar]
- 19.Data Quality of the Discharge Abstract Database Following the First-Year Implementation of ICD-10-CA/CCI: Final Report. Ottawa, Ontario: Canadian Institute for Health Information; 2004. [Google Scholar]
- 20.Hale DA, Molloy M, Pearl RH, Schutt DC, Jaques DP. Appendectomy: a contemporary appraisal. Ann Surg. 1997;225(3):252–261. doi: 10.1097/00000658-199703000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sauerland S, Lefering R, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2004;4:CD001546. doi: 10.1002/14651858.CD001546.pub2. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Alcohol and public health: alcohol-related disease impact. Available at: http://apps.nccd.cdc.gov/DACH_ARDI/Info/ICDCodes.aspx. Accessed May 22, 2013.
- 23.Seber GA, Lee AJ. Linear Regression Analysis. 2nd ed. New York, NY: John Wiley & Sons Inc; 2003. [Google Scholar]
- 24.Freund RJ, Wilson WJ, Sa P. Regression Analysis: Statistical Modeling of a Response Variable. 2nd ed. New York, NY: Academic Press; 2006. [Google Scholar]
- 25.Nichols A. Causal inference with observational data. Stata J. 2007;7(4):507–541. [Google Scholar]
- 26.Imbens G, Kalyanaraman K. Optimal bandwidth choice for the regression discontinuity estimator. Rev Econ Stud. 2012;79(3):933–959. [Google Scholar]
- 27.Hoaglin DC, Mosteller F, Tukey JW. Understanding Robust and Exploratory Data Analysis. New York, NY: John Wiley & Sons Inc; 1983. [Google Scholar]
- 28.Carpenter CS, Kloska DD, O’Malley P, Johnston L. Alcohol control policies and youth alcohol consumption: evidence from 28 years of monitoring the future. BE J Econ Anal Policy. 2007;7(1):1–21. [Google Scholar]
- 29.Carpenter C, Dobkin C. The effect of alcohol consumption on mortality: regression discontinuity evidence from the minimum drinking age. Am Econ J Appl Econ. 2009;1(1):164–182. doi: 10.1257/app.1.1.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yoruk BK, Yoruk CE. The impact of minimum legal drinking age laws on alcohol consumption, smoking, and marijuana use: evidence from a regression discontinuity design using exact date of birth. J Health Econ. 2011;30(4):740–752. doi: 10.1016/j.jhealeco.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 31.Crost B, Guerrero S. The effect of alcohol availability on marijuana use: evidence from the minimum legal drinking age. J Health Econ. 2012;31(1):112–121. doi: 10.1016/j.jhealeco.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 32.Carpenter C, Dobkin C. The effects of minimum legal drinking age on morbidity. Available at: http://www.maxwell.syr.edu/uploadedFiles/econ/seminars/Carpenter_Dobkin_morbidity_mlda_10_19_2011.pdf. Accessed May 22, 2013.
- 33.Hufford MR. Alcohol and suicidal behavior. Clin Psychol Rev. 2001;21(5):797–811. doi: 10.1016/s0272-7358(00)00070-2. [DOI] [PubMed] [Google Scholar]
- 34.Esposito-Smythers C, Spirito A. Adolescent substance use and suicidal behavior: a review with implications for treatment research. Alcohol Clin Exp Res. 2004;28(suppl 5):77S–88S. doi: 10.1097/01.alc.0000127417.99752.87. [DOI] [PubMed] [Google Scholar]
- 35.Bagge CL, Sher KJ. Adolescent alcohol involvement and suicide attempts: toward the development of a conceptual framework. Clin Psychol Rev. 2008;28(8):1283–1296. doi: 10.1016/j.cpr.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Birckmayer J, Hemenway D. Minimum-age drinking laws and youth suicide, 1970–1990. Am J Public Health. 1999;89(9):1365–1368. doi: 10.2105/ajph.89.9.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jones NE, Pieper CF, Robertson LS. The effect of legal drinking age on fatal injuries of adolescents and young adults. Am J Public Health. 1992;82(1):112–115. doi: 10.2105/ajph.82.1.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hingson RW, Zha W, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18–24, 1998–2005. J Stud Alcohol Drugs Suppl. 2009;16:12–20. doi: 10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Adlaf EM, Demers A, Gliksman L. Canadian Campus Survey 2004. Toronto, Ontario: Centre for Addiction and Mental Health; 2005. [Google Scholar]
- 40.Wechsler H, Moeykens B, Davenport A, Castillo S, Hansen J. The adverse impact of heavy episodic drinkers on other college students. J Stud Alcohol. 1995;56(6):628–634. doi: 10.15288/jsa.1995.56.628. [DOI] [PubMed] [Google Scholar]
- 41.Engs RC, Hanson DJ. Boozing and brawling on campus: a national study of violent problems associated with drinking over the past decade. J Crim Justice. 1994;22(2):171–180. [Google Scholar]
- 42.Wells SL, Thompson JM. Alcohol-related victimization among young adult Canadian drinkers: the explanatory roles of hazardous drinking and illicit drug use. Can J Public Health. 2009;100(1):55–59. doi: 10.1007/BF03405494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ray JG, Moineddin R, Bell CM et al. Alcohol sales and risk of serious assault. PLoS Med. 2008;5(5):e104. doi: 10.1371/journal.pmed.0050104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Giancola PR, Levinson CA, Corman MD et al. Men and women, alcohol and aggression. Exp Clin Psychopharmacol. 2009;17(3):154–164. doi: 10.1037/a0016385. [DOI] [PubMed] [Google Scholar]
- 45.Cherpitel CJ. Alcohol and injuries: a review of international emergency room studies since 1995. Drug Alcohol Rev. 2007;26(2):201–214. doi: 10.1080/09595230601146686. [DOI] [PubMed] [Google Scholar]
- 46.Sindelar HA, Barnett NP, Spirito A. Adolescent alcohol use and injury: a summary and critical review of the literature. Minerva Pediatr. 2004;56(3):291–309. [PubMed] [Google Scholar]
- 47.Beck KH, Arria AM, Caldeira KM, Vincent KB, O’Grady KE, Wish ED. Social context of drinking and alcohol problems among college students. Am J Health Behav. 2008;32(4):420–430. doi: 10.5555/ajhb.2008.32.4.420. [DOI] [PMC free article] [PubMed] [Google Scholar]