Abstract
This paper evaluates a new technique that can lead to excision of pilonidal sinus with less healing time and low recurrence rate. A prospective randomized double-blind controlled study on 142 patients with pilonidal sinus conducted during the period from September 2008 to March 2012. The patients were prospectively randomized to be operated with one of four surgical techniques, excision and primary closure, or excision after using hydrogen peroxide (H202) and primary closure, or excision without closure, or excision after injection of H202 without closure. The main outcome measures were the healing time and the recurrence rate. Out of 142 patients, 118 patients were males (83%), and 24 were females (17%). The mean age was 24.5 years. The recurrence rate in patients treated with excision after injection of H202 without closure was the lowest (1.8%) with P-value < 0.005, and the mean duration of healing was 30.7 days with P-value < 0.005. We recommend using excision after injection of H202 without closure in management of PNS. Injection of H202 into the pilonidal tracts can give a precise delineation of the affected tracts, which can be excised with minimal amount of surrounding normal tissues and hence lead to a quicker recovery and low recurrence rate.
Keywords: Pilonidal sinus, Hydrogen peroxide, Excision, Closure
Pilonidal sinus (PNS) is not an uncommon disease in Saudi Arabia among the young and middle age population. It is more common in males than females. This is because of the abundance of back hair and sitting on hard surfaces as well as driving for extended hours. The standard treatment of this problem is usually surgical after failure of conservative management. The main pitfalls of surgery are the recurrence rate and the long duration of healing. In our study, we tried to minimize the healing time and recurrence rate by the precise excision of the only affected tissues using H202 3% prior to injection of methylene blue into the sinus tracts.
Materials and Methods
Our study was held at King Abdulaziz University Hospital (KAUH), Jeddah, Saudi Arabia, which is the only university hospital in the western region of Saudi Arabia with a capacity of 850 beds. During the period from May 2004 to September 2006, 142 patients who were randomly double-blind categorized into four groups. Thirty-one patients were in group (A) and were treated by excision and primary closure of the wound (closed method) only while 12 patients in group (B) were treated by excision and primary closure (standard old method) after using H202 pre-operatively. In group (C) we adopted the (open method), i.e., excision followed by dressing of the opened wound in 24 patients, while in the last group (D), 72 patients were treated by the standard open technique with the use of H202 pre-operatively. Inclusion criteria was any patient with PNS between the ages of 12 and 60 years without any medical comorbidity that could affect wound healing. Any patient with diabetes mellitus or morbid obesity with body mass index of greater than 40, or on corticosteroid medication was excluded from the study. The follow-up of the patients in the four groups was estimated with a mean period of 53.2 days, and the results regarding healing time and rate of recurrences were established. Data was described as means, proportions or medians as appropriate. Analysis was done using the Mann-Whitney test to relate median and Fisher's exact test to compare proportions taken in consideration of the sample size to eliminate any error. A P value of <0.05 was considered to be significant. An ethical approval to conduct the study was obtained from the local Ethical Committee of KAUH.
Results
One hundred forty-two cases with PNS were divided into four groups (A, B, C, and D), where the standard techniques of open and closed methods with and without the use of hydrogen peroxide 3% (H202) were adopted.
The age of the patients ranged between 16 and 55 years with a mean of 24.5 years. One hundred eighteen patients were males (83%), and 24 were females (17%).
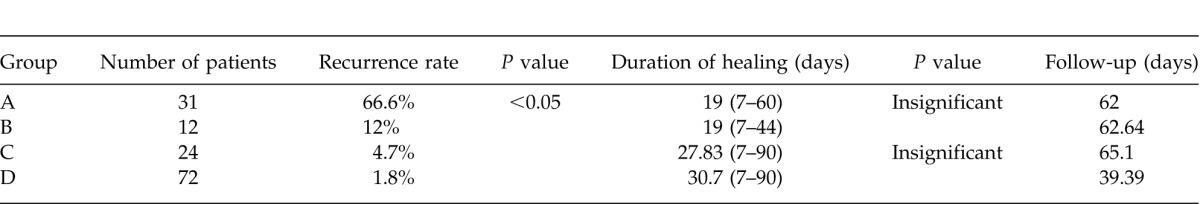
The mean duration for follow-up was 53.2 days, while that of healing was 25.8 days. Most of the patients' complaints were pain and discharge (68%) while the rest were asymptomatic. The overall recurrence rate after the surgery was 6.3%. The recurrence rate, duration of healing and the follow-up time of each group are shown as follows in Table 1.
Discussion
Pilonidal disease is a well-known problem especially among young and middle-aged male population. It is an acquired disease, resulting from the mechanical forces that lead to the insertion of the hair shaft falling from the back of the patient and inserted into the skin of usually the upper part of the natal cleft. Pilonidal disease is a chronic inflammatory condition that mostly affects the post anal region. It can be asymptomatic, but usually presents as a cyst, an abscess or a sinus. The hair may sometimes be seen projecting from the sinus orifice.1 It is dead hair. The disease was first discovered during the World War II among soldiers and described as “Jeep disease.” It usually affects males more than females in their third decade of life by three- to fourfold, and rarely encountered after age 45. The sinus may be single or multiple, and usually gives rise to a bloody or pus-based discharge. Some clinicians advocate conservative management by removal of the hair and strict hygiene since no operative procedure showed a proven superiority on the other in regards to healing time, return to work or rate of recurrence.2 The ideal operation of PNS should be simple with low recurrence rate and the pain should be also minimal with minimum days of wound care and return to work and normal activities.3 It had been traditional to inject methylene blue into the external orifice of the sinus to stain the diseased area to be excised.4 This method led to the excision of more normal surrounding tissues than should be. Hydrogen peroxide (H202) is a known antiseptic solution in clinical practice. Several studies showed no positive or negative effects of H202 on wound healing.5–8 We started our study of the efficacy of H202 3% in the management of PNS on two groups of our patients (B, D) and found that injection of H202 3% into the sinus tract two minutes before the injection of the methylene blue gave better results regarding the recurrence rate and healing time in the closed as well as in the open methods. This is because H202 causes an opening and, at the same time, lining of the tracts leading to precise delineation and prevents extra ordinary diffusion of methylene blue into normal tissue greatly minimizing the removal of unnecessary surrounding normal tissues and enhancing rapid healing and less rate of recurrence.
We had a recurrence rate of 12% (2 cases) for the closed technique with H202 group and 1.8% (1 case) for the open technique with H202 group. This lies within the range reported in literature for closed technique (3.7%–20%).9–11 and compares favourably with the rates reported for the open technique (3%-12%).9–11
Conclusion
In our study, we showed that injection of H202 3% into the PNS tracts 2 minutes before the injection of methylene blue can give a precise delineation of the affected tracts, which can be excised with minimal amount of surrounding normal tissues and hence lead to a quicker recovery and low recurrence rate.
Acknowledgments
The authors have no conflict of interest, and are not supported/funded by any drug company.
Table 1.
References
- 1.Hull TL, Wu J. Pilonidal disease. Surg Clin N Am. 2002;82(6):1169–1185. doi: 10.1016/s0039-6109(02)00062-2. [DOI] [PubMed] [Google Scholar]
- 2.Humphries AE, Duncan JE. Evaluation and management of pilonidal disease. Surg Clin N Am. 2010;90(1):113–124. doi: 10.1016/j.suc.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 3.JD McCallum LJ, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ. 2008;336(7649):868–871. doi: 10.1136/bmj.39517.808160.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doll D, Novotny A, Rothe R, Kristianse JE, Wietelmann K, Boulesteix AL, et al. Methylene blue halves the long-term recurrence rate in acute pilonidal sinus disease. Int J Colorectal Dis. 2008;23(4):181–187. doi: 10.1007/s00384-007-0393-9. [DOI] [PubMed] [Google Scholar]
- 5.Lineaweaver W, Howard R, Soucy D, McMorris S, Freeman J, Crain C, et al. Topical antimicrobial toxicity. Arch Surg. 1985;120(3):267–270. doi: 10.1001/archsurg.1985.01390270007001. [DOI] [PubMed] [Google Scholar]
- 6.Gruber RP, Vistnes L, Pardoe R. The effect of commonly used antiseptics on wound healing. Plast Reconstr Surg. 1975;55(4):472–476. [PubMed] [Google Scholar]
- 7.Tur E, Bolton L, Constantine BE. Topical hydrogen peroxide treatment of ischemic ulcers in the guinea pig: blood recruitment in multiple skin sites. JAAD. 1995;33(2:1):217–221. doi: 10.1016/0190-9622(95)90238-4. [DOI] [PubMed] [Google Scholar]
- 8.Lau WY, Wong SH. Randomized prospective trial of topical hydrogen peroxide in appendectomy wound infection. Am J Surg. 1981;142(3):393–397. doi: 10.1016/0002-9610(81)90358-5. [DOI] [PubMed] [Google Scholar]
- 9.Al-Salamah SM, Hussain MI, Mirza SM. Excision with or without primary closure for pilonidal sinus disease. J Pak Med Assoc. 2007;57(8):388–391. [PubMed] [Google Scholar]
- 10.Søndenaa K, Nesvik I, Andersen E, Søreide JA. Recurrent pilonidal sinus after excision with closed or open treatment: final result of a randomised trial. Eur J Surg. 1996;162(3):237–240. [PubMed] [Google Scholar]
- 11.Al-Hassan HK, Francis IM, Neglén P. Primary closure or secondary granulation after excision of pilonidal sinus. Acta Chir Scand. 1990;156(10):695–699. [PubMed] [Google Scholar]


