Abstract
A 69-year-old woman, who underwent cadaveric liver transplantation for non-B, non-C liver cirrhosis with hepatocellular carcinoma in April 2009, was admitted to our hospital because of graft dysfunction. Enhanced computed tomography revealed stenosis of the left branch of the portal vein, obstruction of the right branch of the portal vein at porta hepatis, and esophagogastric varices. Balloon angioplasty of the left branch of the portal vein under transsuperior mesenteric venous portography was performed by minilaparotomy. After dilatation of the left branch of the portal vein, the narrow segment of the portal vein was dilated, which resulted in reduction of collateral circulation. At 7 days after balloon angioplasty, esophageal varices were improved. The patient made a satisfactory recovery, was discharged 8 days after balloon angioplasty, and remains well.
Keywords: Liver transplantation, Portal stenosis, Balloon angioplasty, Minilaparotomy
Portal stenosis is an uncommon complication after cadaveric liver transplantation, and it is usually diagnosed within the first few months.1–3 In the present study, we report on a successfully treated case of late-onset portal vein stenosis after cadaveric liver transplantation by balloon angioplasty under portography.
Case Report
A 69-year-old woman, who had undergone cadaveric liver transplantation for liver cirrhosis due to nonalcoholic steatohepatitis with hepatocellular carcinoma in April 2009, was admitted to our hospital in January 2012 because of graft dysfunction and portal hypertension. Enhanced computed tomography revealed stenosis of the left branch of the portal vein, obstruction of the right branch of the portal vein at porta hepatis, and esophagogastric varices, but no portal thrombosis, dilatation of intrahepatic bile duct, ascites, or recurrent hepatocellular carcinoma. Blood flow of the hepatic artery and the hepatic vein was normal. Hepatic right lobe received portal blood flow from the collateral and shunt vessels. Liver biopsy revealed no acute cellular rejection, with a rejection activity index of 2. Upper gastrointestinal endoscopy revealed esophageal varices with a positive red color sign (Fig. 1A). On radiologic examination, periportal fibrosis at porta hepatis seemed to have led to portal vein stenosis (Fig. 2). Balloon angioplasty of the left branch of the portal vein under transsuperior mesenteric venous portography was performed by minilaparotomy of pararectal incision for graft dysfunction and esophageal varices. Before balloon angioplasty of the left branch of the portal vein, portography revealed collateral circulation of a coronary vein (Fig. 3A). As for the liver right lobe, adequate portal inflow was supplied by collateral circulation from the mesenterium. The left branch of the portal vein was dilated using a balloon 6 mm in diameter for 3 minutes by 6 atm under trans-superior mesenteric venous portography, and then was dilated using a 7-mm balloon for 3 minutes by 6 atm. After dilatation, the narrow segment of the portal vein was dilated, which resulted in reduction of collateral circulation of the coronary vein (Fig. 3B). At 7 days after balloon angioplasty, esophageal varices were improved and the red color sign became negative (Fig. 1B). The patient made a satisfactory recovery, was discharged on 8 days after balloon angioplasty, and remains well.
Fig. 1.
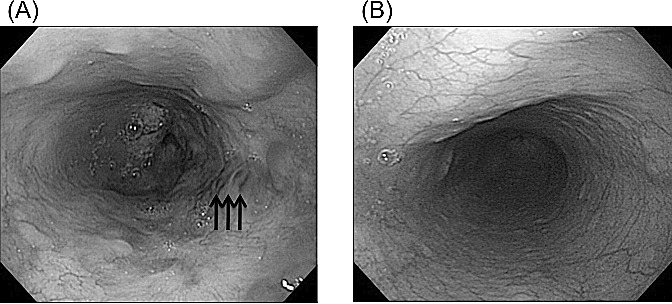
Before balloon angioplasty, upper gastrointestinal endoscopy revealed esophageal varices with a positive red color sign (A; arrows). At 7 days after balloon angioplasty, esophageal varices were improved and the red color signs became negative (B).
Fig. 2.
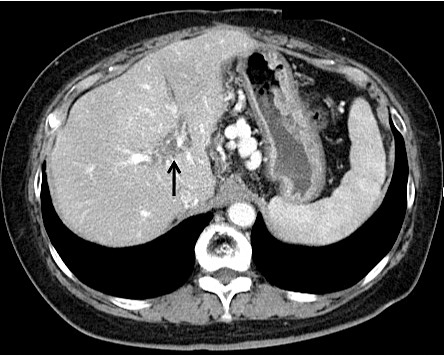
On enhanced computed tomography, periportal fibrosis at porta hepatis (arrow) seemed to have led to portal vein stenosis.
Fig. 3.

Before balloon angioplasty of the left branch of the portal vein, portography revealed collateral circulation of the coronary vein (A; arrow). After dilatation of the left branch of the portal vein under transsuperior mesenteric venous portography, the narrow segment of the portal vein was dilated, which resulted in reduction of collateral circulation of the coronary vein (B; arrowhead).
Discussion
Vascular complications following liver transplantation have been well documented, and portal vein complications are less common than hepatic arterial complications. Portal vein stenosis after liver transplantation may lead to significant morbidity, including graft failure, portopulmonary hypertension, and esophagogastric varices due to portal hypertension.4,5
The cause of late-onset intrahepatic portal vein stenosis is unclear, which could be related to secondary fibrosis or intimal hyperplasia.6 In our patient, on radiologic examination, periportal fibrosis at porta hepatis seemed to have led to portal vein stenosis without anastomotic stenosis.
Retransplantation, shunt operation, and excision of fibrous tissue surrounding the portal vein have been reported as treatment for portal vein stenosis.7 These surgical treatment options are invasive and complicated. Transluminal portal vein angioplasty using a percutaneous transhepatic or mesenteric venous approach has a high success rate with minimal invasiveness and low complication rates.8,9 On the long-term results of this procedure, a recent study reported the patency of portal vein after balloon angioplasty for portal stenosis was 71.4% with a mean follow-up of 24.4 months.10 For a residual significant stenosis or a recurrent stenosis within a few months after balloon angioplasty, the metallic stent placement should be considered.11,12 However, there is a retransplantation case report about graft failure caused by portal thrombus after the placement of a portal vein stent for portal stenosis.13 Measuring the long-term outcomes of larger patient pools is necessary for evaluation of portal vein stent for portal stenosis after liver transplantation.12
In conclusion, balloon angioplasty under portography may be a useful therapeutic option for graft failure and esophageal varices due to portal vein stenosis after liver transplantation.
References
- 1.Settmacher U, Nüssler NC, Glanemann M, Haase R, Heise M, Bechstein WO, et al. Venous complications after orthotopic liver transplantation. Clin Transplant. 2000;14(3):235–241. doi: 10.1034/j.1399-0012.2000.140309.x. [DOI] [PubMed] [Google Scholar]
- 2.Schneider N, Scanga A, Stokes L, Perri R. Portal vein stenosis: a rare yet clinically important cause of delayed-onset ascites after adult deceased donor liver transplantation: two case reports. Transplant Proc. 2011;43(10):3829–3834. doi: 10.1016/j.transproceed.2011.09.068. [DOI] [PubMed] [Google Scholar]
- 3.Wang JF, Zhai RY, Wei BJ, Li JJ, Jin WH, Dai DK, et al. Percutaneous intravascular stents for treatment of portal venous stenosis after liver transplantation: midterm results. Transplant Proc. 2006;38(5):1461–1462. doi: 10.1016/j.transproceed.2006.02.113. [DOI] [PubMed] [Google Scholar]
- 4.Millis JM, Seaman DS, Piper JB, Alonso EM, Kelly S, Hackworth CA, et al. Portal vein thrombosis and stenosis in pediatric liver transplantation. Transplantation. 1996;62(6):748–754. doi: 10.1097/00007890-199609270-00008. [DOI] [PubMed] [Google Scholar]
- 5.Ueda M, Egawa H, Ogawa K, Uryuhara K, Fujimoto Y, Kasahara M, et al. Portal vein complications in the long-term course after pediatric living donor liver transplantation. Transplant Proc. 2005;37(2):1138–1140. doi: 10.1016/j.transproceed.2005.01.044. [DOI] [PubMed] [Google Scholar]
- 6.Wei BJ, Zhai RY, Wang JF, Dai DK, Yu P. Percutaneous portal venoplasty and stenting for anastomotic stenosis after liver transplantation. World J Gastroenterol. 2009;15(15):1880–1885. doi: 10.3748/wjg.15.1880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sood D, Kumaran V, Kakodkar R, Punamia SJ, Saigal S, Nundy S, et al. Portal vein stenosis following living donor liver transplant: manifestations and management. Transpl Int. 2009;22(4):496–499. doi: 10.1111/j.1432-2277.2008.00797.x. [DOI] [PubMed] [Google Scholar]
- 8.Duffy JP, Hong JC, Farmer DG, Ghobrial RM, Yersiz H, Hiatt JR, et al. Vascular complications of orthotopic liver transplantation: experience in more than 4,200 patients. J Am Coll Surg. 2009;208(5):896–903. doi: 10.1016/j.jamcollsurg.2008.12.032. [DOI] [PubMed] [Google Scholar]
- 9.Park KB, Choo SW, Do YS, Shin SW, Cho SG, Choo IW. Percutaneous angioplasty of portal vein stenosis that complicates liver transplantation: the mid-term therapeutic results. Korean J Radiol. 2005;6(3):161–166. doi: 10.3348/kjr.2005.6.3.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shibata T, Itoh K, Kubo T, Maetani Y, Shibata T, Togashi K, et al. Percutaneous transhepatic balloon dilation of portal venous stenosis in patients with living donor liver transplantation. Radiology. 2005;235(3):1078–1083. doi: 10.1148/radiol.2353040489. [DOI] [PubMed] [Google Scholar]
- 11.Funaki B, Rosenblum JD, Leef JA, Zaleski GX, Farrell T, Lorenz J, et al. Percutaneous treatment of portal venous stenosis in children and adolescents with segmental hepatic transplants: long-term results. Radiology. 2000;215(1):147–151. doi: 10.1148/radiology.215.1.r00ap38147. [DOI] [PubMed] [Google Scholar]
- 12.Woo DH, Laberge JM, Gordon RL, Wilson MW, Kerlan RK., Jr Management of portal venous complications after liver transplantation. Tech Vasc Interv Radiol. 2007;10(3):233–239. doi: 10.1053/j.tvir.2007.09.017. [DOI] [PubMed] [Google Scholar]
- 13.Zajko AB, Sheng R, Bron K, Reyes J, Nour B, Tzakis A. Percutaneous transluminal angioplasty of venous anastomotic stenoses complicating liver transplantation: intermediate-term results. J Vasc Interv Radiol. 1994;5(1):121–126. doi: 10.1016/s1051-0443(94)71467-6. [DOI] [PubMed] [Google Scholar]


