Abstract
We describe a 40-year-old woman presenting with headache, nausea, episodic amnesia and blurred optic disc. Brain MRI disclosed diffuse leptomeningeal enhancement. CSF analysis showed aseptic meningitis with elevated ACE level. Neurosarcoidosis was diagnosed based on granulomatosis changes on tissue biopsy.
Keywords: Sarcoidosis, Meningitis, Central Nervous System
Introduction
Sarcoidosis is a chronic granulomatous systemic disease of unknown etiology, with many different clinical presentations [1, 2]. Non-caseating granuloma is the hallmark pathologic finding. Pulmonary, lymph node, ocular, and skin lesions are the most common manifestations of Sarcoidosis [3]. Nervous system can also be involved. The reported prevalence of neurological involvement varies due to case selection and diagnostic criteria, and can be as high as 5% [1, 4].
Cranial neuropathies from chronic basal meningitis constitute the most common neurological manifestation of Sarcoidosis; most often the facial nerve is involved, sometimes bilaterally. Encephalopathy, seizures, mass lesions, obstructive hydrocephalus, basilar granulomatous meningitis, aseptic meningitis, myelopathy, and pituitary-hypothalamic lesions are the other manifestations of Cranial Nervous System (CNS) involvement [1, 5].
In 62 to 74% of neurosarcoidosis patients, neurological symptoms are the primary manifestation of the disease [6, 7]; therefore, many patients with neurosarcoidosis develop systemic symptoms only after presenting with neurological signs of the disease [2].
In this article, we describe a case of neurosarcoidosis who presented with nervous system complaints.
Case Report
A 40 year old woman was presented to Shariati hospital (TUMS), with headache, nausea, and episodic amnesia. The episodes lasted less than five minutes, and resolved after vomiting.
The patient complained of no fever, focal weakness, or sensory symptoms; but she mentioned episodic dyspnea for more than 5 years, leading to cardiac and respiratory evaluations, which failed to show any specific etiology.
She had a history of admission to other hospital, about 9 months earlier, due to headache, blurring of vision and diplopia. At that time she was diagnosed as cerebral venous sinus thrombosis and had been treated with anticoagulants.
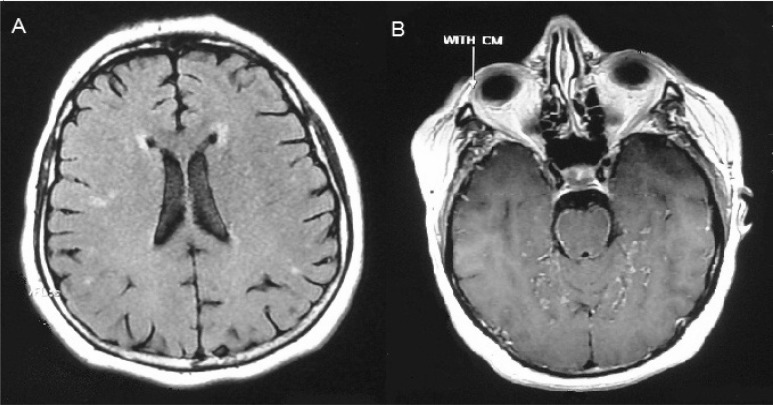
Examination disclosed blurred optic disc margins and slight neck rigidity. Brain MRI showed diffuse leptomeningeal enhancement, with scattered white matter changes (Figure 1).
Figure 1.
(A) FLAIR image shows scattered white matter changes, (B) postcontrast T1 weighted image shows meningeal enhancement.
Cerebrospinal Fluid (CSF) examination showed lymphocytosis (WBC:37,70% lymphocyte), elevated protein (277mg/dl) and low glucose (13mg/dl); but cytological examination, stains for bacteria, mycobacteria, and fungi, VDRL, Wright, and PCR for TB, all were negative in the CSF.
CSF exam was repeated three more times, each time with complete laboratory evaluation (including cytological examination), with similar results.
Routine hematology and biochemistry tests, liver function tests, thyroid function tests, PPD (purified protein derivative), HIV antibody, C-ANCA, P-ANCA, C3, C4, CH50, anticardiolipin and antiphospholipid antibodies, were normal/negative, as well as tumor markers in search of malignancy. Chest roentgenography, HRCT of thorax, and the result of bronchoscopy with BAL (BronchoAlveolar Lavage) were unrevealing.Serum ACE level was normal, but CSF ACE was raised (24; NL < 5).
The patient was treated with IV methyl prednisolone and continued on prednisolone with the impression of probable neurosarcoidosis.
Two weeks later, she developed another episode of dyspnea. She was re-evaluated by pulmonary specialist, and because of an abnormality in the base of her lung, an open biopsy was performed. The pathology report was consistent with Sarcoidosis. Dyspnea was ascribed to pulmonary hypertension.
Patient's neurological symptoms and signs improved after 2 months and after 7 months follow up, she was still free of symptoms.
Discussion
We describe clinical and laboratory data of a case of neurosarcoidosis. In accordance with Zajieck's diagnostic criteria, diagnosis of probable Sarcoidosis was made at first; and after open lung biopsy, definite Sarcoidosis was diagnosed [6].
In most reported series, the incidence of clinically evident neurosarcoidosis is about 5%. Neurosarcoidosis is often suspected in patients with known Sarcoidosis [8]. Stern et al reported that 73% of patients with neurosarcoidosis developed their symptoms and signs within the first two years of their systemic Sarcoidosis [8]. In our patient, systemic (pulmonary) Sarcoidosis was diagnosed after diagnosis of neurosarcoidosis in the form of chronic meningitis, which presented with headache, nausea, vomiting, and episodic amnesia. Brain MRI showed diffuse meningeal enhancement, without any parenchymal involvement. Meningeal inflammation with concomitant CSF abnormalities is one of the most common manifestations of neurosarcoidosis [4]. CSF analysis in our patient showed abnormalities compatible with previous studies in the literature [5]. Although ACE level in the CSF is not a reliable marker for CNS Sarcoidosis; with both false negative and false positive results [6], significant elevation of CSF ACE in our patient, along with exclusion of infections and malignancies, can be in favor of neurosarcoidosis. Diagnosis and management of neurosarcoidosis are both challenging; Stern et al recommended biopsy proof of granulomatous inflammation from any involved (including nervous system) tissue specimens before initiation oftreatment [1, 5]. We started treatment by a probable diagnosis of neurosarcoidosis, and definite diagnosis was made two weeks later by open lung biopsy.
Patient's neurological symptoms and signs improved after 2 months and now, after 7 months of follow up, she is still free of neurological symptoms.
References
- 1.Aminoff M.J. Neurological complication of systemic disease in adult. In: Bradly W.G, Daroff R.B, Jankovic J, editors. Neurology in clinical practice. Ed. 5. Elsevier Philadelphia; 2008. pp. 1074–1075. [Google Scholar]
- 2.Marangoni S, Argentiero V, Tavolato B. Neurosarcoidosis. Clinical description of 7 cases with aproposal for a new diagnostic strategy. J Neurol. 2006;253:488–95. doi: 10.1007/s00415-005-0043-5. [DOI] [PubMed] [Google Scholar]
- 3.Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med. 2007;357:2153–65. doi: 10.1056/NEJMra071714. [DOI] [PubMed] [Google Scholar]
- 4.Stern BJ, Krumholz A, Johns C, et al. Sarcoidosis and its neurological manifestations. Arch Neurol. 1985;42:909–17. doi: 10.1001/archneur.1985.04060080095022. [DOI] [PubMed] [Google Scholar]
- 5.Stern BJ, Aksamit A, Clifford D, et al. Neurologic presentations of Sarcoidosis. Neurology Clinics. 2010;28:185–198. doi: 10.1016/j.ncl.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 6.Zajicek JP, Scolding NJ, Foster O, et al. Central nervous system sarcoidosis-diagnosis and management. QJM. 1999;92:103–117. doi: 10.1093/qjmed/92.2.103. [DOI] [PubMed] [Google Scholar]
- 7.Ferriby D, de Seze J, Stojkovic T, et al. Long-term follow-up of neurosarcoidosis. Neurology. 2001;57:927–9. doi: 10.1212/wnl.57.5.927. [DOI] [PubMed] [Google Scholar]
- 8.Veres L, Utz JP, Houser OW. Sarcoidosis presenting as a central nervous system mass lesion. CHEST. 1997;111:518–521. doi: 10.1378/chest.111.2.518. [DOI] [PubMed] [Google Scholar]