Abstract
Background
Prevalence of electrophysiological abnormalities in patients with lumbosacral radiculopathy was evaluated.
Methods
A cross-sectional study was performed on 97 consecutive patients with the clinical diagnosis of lumbosacral radiculopathy. Complete neurological examinations and standard electrophysiological evaluation was performed on the patients.
Results
Patients under study had the mean age of 46.4 ± 13.1 years (mean ± standard deviation). There were positive MRI findings in 64% of the patients. In 43% L5 root and in 40% S1 root was involved. Abnormal electrophysiological findings were recorded in 82% of the patients. In patients with pretibial muscle weakness, there were significant abnormalities recorded in compound motor action potential (CMAP) amplitude of the common peroneal nerve. There was significantly increased frequency of electrophysiological abnormalities in the presence of chronic clinical symptoms (P = 0.001).
Conclusion
The 82% positive findings in electrophysiological studies in the diagnosis of lumbosacral radiculopathy make it an efficacious tool in the evaluation of the patients suffering from lumbosacral radiculopathy.
Keywords: Lumbosacral Radiculopathy, Electrodiagnostic Evaluation
Introduction
Low back pain is a common complaint involving the adults and occurs in 40-80% of population at least once in the lifetime.1 There are many etiologies declared to be responsible. Discopathies and lumbosacral disc herniation is shown to be responsible in a wide range of 2-40% of the cases of lumbosacral radiculopathy in different studies. Inflammatory and degenerative bone diseases would be the other causes.2 Lumbosacral radiculopathy affects 4 to 6% of the population at some point in their lives.1 L5-S1 and L4-5 are by far the most common levels affected in lumbosacral radiculopathy.2 To establish the definitive diagnosis, there are a variety of diagnostic tools such as magnetic resonance imaging (MRI), computed tomography (CT) myelography, discography and electrophysiological studies.3, 4 Despite rapid improvements, imaging techniques are neither adequately sensitive nor specific to be used as the only means of the definitive diagnosis.
Electrophysiological studies are efficacious methods in the diagnosis and predicting the prognosis of radiculopathies. An electrical abnormality represents the involved root in the form of fibrillation potentials and neurogenic MUAPs (motor unit action potentials) in a segment or a myotome. These studies are proper for differentiating diagnosis of the lumbosacral radiculopathy from mimics such as plexopathies, polyneuropathies and so on.3 High accuracy of electrodiagnostic studies, high prevalence of lumbosacral radiculopathy and its considerable economic burden were the purpose to study the association between clinical findings and electrophysiological changes to see whether these studies are sensitive enough in the evaluation of the patients with signs and symptoms of lumbosacral radiculopathy for definitive diagnosis.
Materials and Methods
In a cross-sectional study, 97 consecutive patients with the clinical diagnosis of lumbosacral radiculopathy referred to the Electrodiagnostic Laboratory affiliated to Tehran University of Medical Sciences were recruited in 2007. Patients with any other diagnosed neurological diseases or other signs/symptoms and those with other systemic illnesses which could affect electrodiagnostic (EDX) results were excluded to avoid possible confounding factors. After the describing the study, written informed consent was obtained from all patients. Patients underwent neurological examination and standard EDX study.5, 6 All the EDX studies were performed with Toennies Neuroscreen machine.
Nerve Conduction Study (NCS) was performed on common peroneal, tibialis and sural nerves and H reflexes were obtained from soleus muscles bilaterally. Electromyographic study was performed by recording active and resting potentials in 5 muscle groups consisted of iliopsoas, quadriceps femoris, gastrocnemious, anterior tibialis and extensor hallucis longus muscles. Additionally, lumbar paraspinal muscles were evaluated in all patients. Other muscles were also tested if clinically or electrophysiologically indicated.
Results
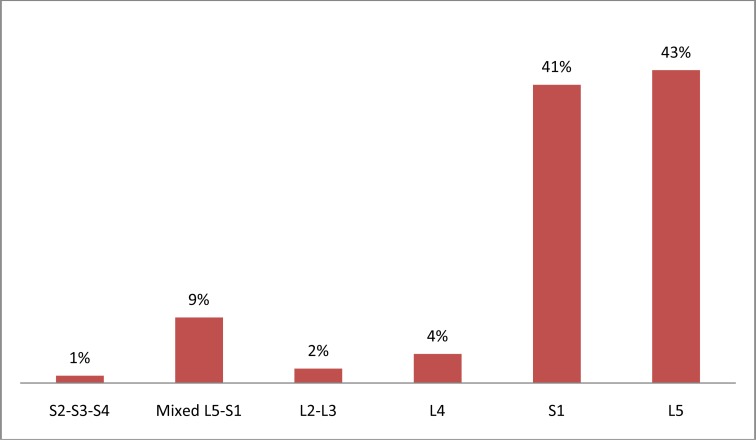
The mean age of the patients (n = 97) was 46.4 ± 13.1 years (mean ± standard deviation) and 48.5% were male. There was isolated left and right lower limb involvement in 38% and 30% of the patients, respectively, and 32% had bilateral involvement (Figure 1). Hypoesthesia was seen mostly in L5 root distribution (21%); 22.8% of patients had paresthesia in L5, and 14% in S1 dermatome. In the population under study, 27% had reduced or absent Achilles reflex, and 20% and 14% had L5 and S1 myotomal weakness, respectively; 48% had positive straight leg raising test.
Figure 1.
Distribution of root involvement in lumbosacral radiculopathy
There were positive MRI findings in 64% of the patients. Abnormal lumbosacral MRI findings were seen more frequently in females than males (78% vs. 49%, P = 0.049). There was no significant association in patients’ age, gender, the type of pain, and clinical sensory findings with EDX results.
Abnormal electrophysiological findings were recorded in 82% of the patients. 73% had abnormal electromyographic (EMG) findings in the lower extremity muscles. Paravertebral muscles were evaluated in all the patients, 23% of whom had normal findings, 68% had spontaneous activity and 9% had neurogenic MUAPs. There were 28% abnormal nerve conduction studies. CMAP amplitude of common peroneal nerve recorded from extensor digitorum brevis (EDB) was abnormal in 24% of the patients, and 11% of the patients had reduced CMAP amplitude of tibialis nerve.
A notably important finding was the significant relationship between electrophysiological findings and the duration of the clinical symptoms; patients with chronic course of disease defined as clinical lumbosacral radiculopathy for more than 6 months, had more abnormalities in the EDX studies (Table 1).
Table 1.
Chronicity of the lumbosacral radiculopathy in the study population
| Course of the disease | Patients |
|---|---|
| Chronic (> 6 months) | 66% |
| Subacute (1 to 6 months) | 20.6% |
| Acute (< 1 months) | 13.4% |
In the group of patients with chronic involvement, abnormal electrical findings in paravertebral muscles were recorded in 90.6% of the patients, compared to 50% and 46.1% in the subacute and acute course of the problem, respectively (P = 0.001). In the muscles of the lower extremity, EMG abnormalities were seen in 84.3% of the chronic group compared to 40 and 46.1% in the subacute and acute involvement, respectively (P = 0.001).
Association of clinical findings with abnormal H-reflex supposed as interside difference of more than 1.5 msec, unilateral absence and absolute values above normal range adjusted for height was investigated. From 30 patients with hypoesthesia in one of the studied dermatomes, normal H-reflex was detected in 19 patients and at least one of the various definition of abnormal H-reflex was seen in 11 patients (P = 0.001). In the 37 patients with paresthesia in dermatomal pattern, normal H- reflex was detected in 22 patients (P = 0.014). In 9 patients with abnormal patellar reflex all had normal H-reflex (P = 0.001). In 17 patients with abnormal Achilles reflex all had abnormal H-reflexes (P = 0.001).
In patients with pretibial muscle weakness, CMAP amplitude abnormality of the common peroneal nerve was significant. In 19 patients with pretibial muscle weakness, 13 and 6 patients had localizing signs of L5-S1 and L4-L5 radiculopathy, respectively. In 12 of these 13 patients (92.3%), CMAP was low amplitude or absent (P = 0.001). The relationship of S1 dermatomal involvement with CMAP amplitude abnormality in tibialis nerve was not statistically significant (P = 0.055).
In both patients with L5 dermatome muscle atrophy, motor NCV of the peroneal nerve was absent (P = 0.001). In 47 patients with positive straight leg rising (SLR), 13 patients had decreased CMAP amplitude (27.6%) compared to 2 of the 50 patients with negative SLR (P = 0.049).
Discussion
Abnormal electrophysiological findings seen in 82% of the patients make these studies sensitive tools in the diagnosis of lumbosacral radiculopathy. Comparatively, previous studies had estimated lower sensitivities.7–9 The higher positive results in our study can be due to the fact that patients with radicular symptoms/signs were only included, and patients with pain restricted to lumbar area without any other symptoms were excluded. In clinical practice, dermatomal radiation, more pain on coughing, sneezing or straining, positive straight leg raising test may be used to predict nerve root compression on MRI.10
In 1994, Czyrny and Lawrence mentioned that electromyography of the paraspinal muscle should be performed in all the patients with suspected lumbosacral radiculopathy.8 In our study, 73% and 77% of the patients had abnormal lower extremity and lumbar paraspinal muscles EMG, respectively.
There was significant relationship between the electrophysiological findings and the duration of the symptoms in our study. The frequency of abnormal EMG findings in the chronicly involved patients was significantly higher than subacutely and acutely involved ones. Some of the previous studies have inferred that patients with the duration of symptoms more than 1 month have more EDX abnormalities compared to patients with clinical involvement less than 1 month.11 There are studies that found no significant association between the duration of symptoms and electrophysiological findings.12, 13
Similar to previous studies,13, 14 there was no significant relationship between age, clinical manifestations and electrophysiological characteristics. Abnormal MRI findings were present in 64% of the patients that is similar to other studies;4 also there was a high percentage of false positive MRI results (low specificity), and one should not base the diagnosis only on MRI changes. Frequency of abnormal findings in MRI was higher in females compared to males, possibly because of more prevalence of skeletal degeneration and early anatomical changes seen in female vertebral column.
There was a significant relationship between pretibial muscle weakness and L5 radiculopathy, and CMAP amplitude of common peroneal nerve in our study. Only 36.8% of the patients with pretibial muscle weakness had normal CMAP amplitude of the common peroneal nerve and in the rest, amplitude was either decreased or absent. In a study performed on 66 patients with the L5-S1 radiculopathy, there was a significant relationship between the muscle weakness in L5 and S1 myotomes and CMAP amplitude decrement in tibialis nerve in S1 involvement and peroneal nerve in L5 involvement, when there was at least 3 months period of involvement.15
In a study in 1990, the H-reflex was recorded from the vastus medialis, and soleus muscles in patients with radiculopathy at L4 and S1 roots. Reflex parameters were compared to normal standards and were found to be correlated with other electromyography and clinical evaluations, as well as magnetic resonance imaging scan reports. The H-reflex had significantly smaller peak-to-peak amplitude and longer latency. A strong correlation was recorded between the pathologic changes in reflex parameters and clinical findings of different segmental lesions,16 that were also seen in our study.
References
- 1.Frymoyer JW. Lumbar disk disease: epidemiology. Instr Course Lect. 1992;41:217–23. [PubMed] [Google Scholar]
- 2.Tsao B. The electrodiagnosis of cervical and lumbosacral radiculopathy. Neurol Clin. 2007;25(2):473–94. doi: 10.1016/j.ncl.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Ropper AH, Brown RJ. Adams and Victors Principles of Neurology. 8th ed. New York, NY: McGraw Hill Professional; 2005. [Google Scholar]
- 4.Robinson LR. Electromyography, magnetic resonance imaging, and radiculopathy: it's time to focus on specificity. Muscle Nerve. 1999;22(2):149–50. doi: 10.1002/(sici)1097-4598(199902)22:2<149::aid-mus1>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 5.Preston DC, Shapiro BE. Electromyography and Neuromuscular Disorders: Clinical-Electrophysiologic Correlations. 2nd ed. Philadelphia, PA: Elsevier Health Sciences; 2005. [Google Scholar]
- 6.Farina D, Merletti R, Enoka RM. The extraction of neural strategies from the surface EMG. J Appl Physiol. 2004;96(4):1486–95. doi: 10.1152/japplphysiol.01070.2003. [DOI] [PubMed] [Google Scholar]
- 7.Mazzocchio R, Scarfo GB, Mariottini A, et al. Recruitment curve of the soleus H-reflex in chronic back pain and lumbosacral radiculopathy. BMC Musculoskelet Disord. 2001;2:4. doi: 10.1186/1471-2474-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Czyrny JJ, Lawrence J. The importance of paraspinal muscle EMG in cervical and lumbosacral radiculopathy: review of 100 cases. Electromyogr Clin Neurophysiol. 1996;36(8):503–8. [PubMed] [Google Scholar]
- 9.Dillingham TR, Lauder TD, Andary M, et al. Identification of cervical radiculopathies: optimizing the electromyographic screen. Am J Phys Med Rehabil. 2001;80(2):84–91. doi: 10.1097/00002060-200102000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Coster S, de Bruijn SF, Tavy DL. Diagnostic value of history, physical examination and needle electromyography in diagnosing lumbosacral radiculopathy. J Neurol. 2010;257(3):332–7. doi: 10.1007/s00415-009-5316-y. [DOI] [PubMed] [Google Scholar]
- 11.Tomasella M, Crielaard JM, Wang FC. How I explore... lumbar paraspinal muscle electromyography in the assessment of radiculopathy. Rev Med Liege. 2001;56(10):716–22. [In French] [PubMed] [Google Scholar]
- 12.Haig AJ, Talley C, Grobler LJ, et al. Paraspinal mapping: quantified needle electromyography in lumbar radiculopathy. Muscle Nerve. 1993;16(5):477–84. doi: 10.1002/mus.880160508. [DOI] [PubMed] [Google Scholar]
- 13.Scelsa SN, Berger AR, Herskovitz S. Electrophysiologic correlates of weakness in L5/S1 radiculopathy. Electromyogr Clin Neurophysiol. 2001;41(3):145–51. [PubMed] [Google Scholar]
- 14.Levin KH. Distribution of fibrillation potentials in radiculopathies. Muscle Nerve. 1999;22(2):287–8. doi: 10.1002/(sici)1097-4598(199902)22:2<287::aid-mus23>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 15.Wee AS. Surface compound action potentials recorded from different locations on the anterior tibial muscle. Electromyogr Clin Neurophysiol. 2002;42(2):119–23. [PubMed] [Google Scholar]
- 16.Tsao BE, Levin KH, Bodner RA. Comparison of surgical and electrodiagnostic findings in single root lumbosacral radiculopathies. Muscle Nerve. 2003;27(1):60–4. doi: 10.1002/mus.10291. [DOI] [PubMed] [Google Scholar]