Summary
Background & aims
Evidence supports the effectiveness of cognitive behavioral approaches in improving IBS symptoms. Duration, cost, and resistance of many patients towards a psychological therapy have limited their acceptance. We evaluated the effectiveness of a psycho-educational intervention on IBS symptoms.
Methods
69 IBS patients (72% female) were randomized to an intervention or a wait-list control group. The IBS class consisted of education on a biological mind body disease model emphasizing self-efficacy and practical relaxation techniques.
Results
Patients in the intervention showed significant improvement on GI symptom severity, visceral sensitivity, depression, and QoL post intervention and most of these gains were maintained at 3 month follow up (Hedge’s g =−.46 to .77). Moderated mediation analyses indicated change in anxiety, visceral sensitivity, QoL and catastrophizing due to the intervention had moderate mediation effects (Hedge’s g= −.38 to −.60) on improvements in GI symptom severity for patients entering the trial with low to average QoL. Also, change in GI symptom severity due to the intervention had moderate mediation effects on improvements in QoL especially patients with low to average levels of QoL at baseline. Moderated mediation analyses indicated mediation was less effective for patients entering the intervention with high QoL.
Conclusions
A brief psycho-educational group intervention is efficacious in changing cognitions and fears about IBS symptoms, and these changes are associated with clinically meaningful improvement in IBS symptoms and QoL. The intervention seems particularly tailored to patients with low to moderate QoL baseline levels.
Keywords: irritable bowel syndrome, quality of life, psycho-education, group intervention
Introduction
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder (FGID), with prevalence rates up to 15%(1-3). IBS is often characterized by chronic recurrent abdominal pain and discomfort associated with altered bowel habits, as well as increased levels of anxiety and depression, including symptom related anxiety(2-7). Patients usually report extraintestinal symptoms of pain and discomfort, fatigue and poor sleep(2, 4, 7, 8) and a significant portion of patients have comorbid visceral and somatic pain disorders such as fibromyalgia and interstitial cystitis/painful bladder syndrome(2, 9). Studies have documented how these various symptoms and comorbidities contribute to the disproportional impairment of health related quality of life (QoL) among IBS patients(3, 6, 10-12).
Currently pharmacologic therapy of IBS beyond symptomatic treatment for constipation or diarrhea remains unsatisfactory, as few studies have demonstrated an effectiveness of available treatments over placebo effects(13-18). On the other hand, psychological treatments such as hypnotherapy and mindfulness(19-22), patient focused cognitive behavior therapy (CBT)(23), behavior therapy (BT)(24, 25), patient education(26), and internet based CBT(27) have all shown effectiveness in alleviating IBS related symptoms. These interventions target a patient’s appraisal of gastrointestinal (GI) sensations and symptoms (including changes in attention and cognition), reductions in symptom related anxiety, changes in arousal and changes in health behavior(28). Despite the relative effectiveness of these non-pharmacologic interventions, their implementation has been hindered by factors such as added cost, unavailability of trained clinicians, inadequate reimbursement for psychosocial interventions and a general bias towards pharmacotherapy among patients and providers(29).
Education- based interventions have also been used as part of IBS disease management in order to increase knowledge about IBS pathophysiology, clarify misconceptions regarding what IBS is and is not, teach simple self-management strategies in areas of diet and stress management, and decrease symptom related fears and anxiety(26, 30). Research on short-term education programs that include some elements of cognitive therapy and stress management (psycho-education) have yielded mixed outcomes. For instance, a critical comparison of various psychological and educational treatments for IBS revealed evidence from clinical trials suggesting that cognitive, behavioral, psychodynamic, educational, and hypnotherapy based treatments worked in alleviating IBS symptoms, and there was no evidence of the superiority of one treatment over the other(26, 27, 30). However, treatment outcomes appear to be correlated with number of sessions, with a onetime session(31, 32) being less effective as interventions with 8-10 sessions(31, 33). The various underlying mechanisms and processes associated with the success of any therapy have yet to be fully understood. More importantly the specific risk and protective factors associated with any specific therapy remain poorly delineated in the literature(34). The current study was designed in order to address two main questions related to these issues: 1) Can a short course of group psycho-educational treatment consisting of combined CBT and basic relaxation techniques result in sustained, clinically relevant improvement of IBS symptom severity, and health-related quality of life? 2) What are the factors that predict a positive outcome (moderators), and the factors that mediate the positive outcomes of the intervention?
Methods and Materials
Subjects
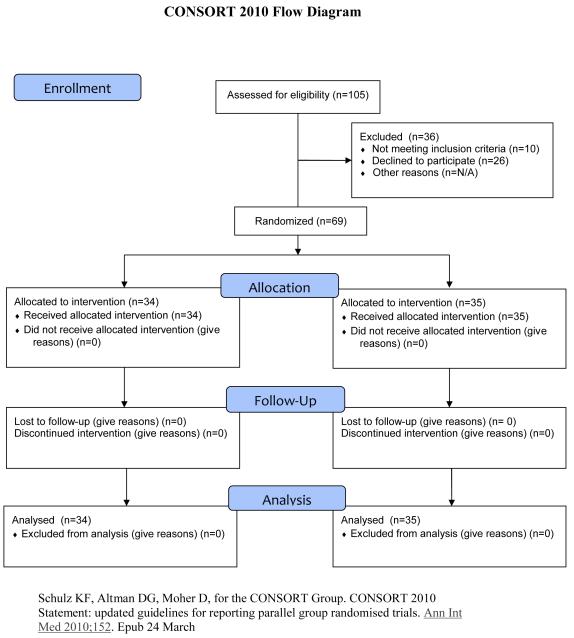
A total of 69 patients (mean age 46.8±12.6 years; 50 females) meeting IBS Rome II criteria(35), seen at a tertiary referral center were included (See Table 1 for detailed demographic data on the sample). Organic disease was excluded with appropriate testing, and a clinical diagnosis of IBS was made by an experienced gastroenterologist. Patients prospectively filled out a daily symptom diary with 6 subscales relating to severity of GI symptoms, and frequency and consistency of stool, for two weeks before entering the study to ensure a minimal symptom severity rating. Subjects were categorized into subgroups based on predominant bowel pattern according to the Rome II criteria(35) yielding 28 diarrhea predominant patients (IBS-D), 24 constipation predominant (IBS-C), and 17 with alternating type IBS (IBS-A). Subjects were randomized to receive either the active intervention (n=34) or assigned to a wait-listed control group (n=35). At the time of enrollment, subjects were instructed to continue the care they were currently receiving for the management of their IBS symptoms. No medical management was provided as part of study participation.
Written and verbal informed consents were obtained from all subjects. The study protocol was approved by the Human Subject Protection Committee at the Veterans Administration Greater Los Angeles Healthcare System.
Assessment Questionnaires
All patients (intervention group and the wait-listed control group) were assessed using self-report measures at baseline, at the end of the five-week intervention course, and then subsequently at three months during a follow-up assessment: Global GI symptom severity over the past week was assessed using a 20-point scale ranging from 0 (no symptoms) to 20 (the most intense symptoms imaginable). The Irritable Bowel Syndrome Quality of Life (IBS-QoL) is a 30 item disease-specific health related quality of life (HRQoL) instrument measuring 9 dimensions of health: emotional functioning, mental health, sleep, energy, physical functioning, diet, social role, physical role, and sexual relations(37, 38). The Hospital Anxiety and Depression Scale(39) is a 14 item scale developed specifically for use among medical outpatients to screen for probable cases of anxiety and depression and provides a measure for severity of mood disorders(40).The Visceral Sensitivity Index (VSI) is a psychometrically well-established 15-item questionnaire designed to measure aspects of fear, anxiety, and hypervigilance that accompany misappraisals of visceral sensations and comfort(36). The Catastrophizing Scale is a brief 6 item self-report subscale from the Coping Strategy Questionnaire (CSQ)(41) assessing the patient’s beliefs regarding severity of discomfort associated with their symptoms. In addition, two questions used in the CSQ to rate overall coping effectiveness were included: 1) amount of control over symptoms, and 2) self-perceived ability to decrease symptoms.
Psycho-educational course
The patients assigned to the intervention group underwent a psycho-educational course. The course was lead by a gastroenterologist (45%) together with a therapist (55%), and consisted of five consecutive weekly two-hour sessions in a group setting with 5-8 participants per group. Participants were also given reading and practical homework assignments related to the topics covered in each session. The gastroenterologist provided interactive lectures on the neurobiology of the stress response, the bio-psychosocial model of IBS, and self-management of diet and medication. The information was disseminated with emphasis given to self-efficacy and empowerment issues, in order for patients to be able to appraise and respond to their symptoms with increased efficiency and accuracy. The therapist taught patients about the role of beliefs and attitudes in IBS and instructed them in two simple relaxation exercises (progressive muscle relaxation and diaphragmatic breathing)(42).
The psycho-education course intervention consisted of four parts: 1. Educational component – Patients were provided with a neurobiological mind/brain/body model linking IBS to the interactions between emotions, stress, and abdominal symptoms with an emphasis on highlighting the nervous system’s ability to self-regulate, so that homeostasis is reestablished and neurochemical imbalances underlying GI symptoms are normalized. 2. Psychological component – Patients were taught about the connection between mood, stress and GI symptoms and ineffective and maladaptive coping styles (e.g. catastrophic thinking), and more effective responses (e.g. conscious rational solutions to stressful situations). 3. Relaxation training – Patients were instructed on diaphragmatic breathing techniques and progressive muscle relaxation. These techniques were practiced under instruction during the group sessions practiced at home with the aid of audio-taped instructions of the procedures. 4. Homework assignments – Patients were assigned homework after each group session: 1) a minimum of 15 min of relaxation exercises twice a day, and 2) monitoring and documentation of symptoms in relationship to mood states, stressors and dietary changes.
Both the gastroenterologist and the therapist led sessions 1, 3, and 5. Sessions 2 and 4 were led solely by the therapist. The estimated cost of the entire 5 week intervention for the entire group was determined from the professional hourly fees of the gastroenterologist ($350) and the therapist ($120) amounting to a total estimated cost for the entire group intervention to be equal to $3,300 (gastroenterologist = 6 total hours; therapist = 10 total hours), or between $ 410 and $ 660 per patient, depending on the group size (5-8 subjects). A brief session-by-session outline of the intervention is provided in Table 1 (Under Supporting Information):
Study design
Patients first attended a screening visit (week 0), which included an examination by one of 4 gastroenterologists and completion of the questionnaires mentioned above. Subjects were also provided with the 2-week symptom diary. Post screening and after completing the 2-week symptom diary (week 2), eligible subjects were randomized to participate in the five-week intervention (intervention group/IBS Class) or assigned to the control condition (wait-list group). In order to fill classes of 8 subjects as quickly as possible, block randomization was used, e.g. consecutive subjects were assigned to the active intervention group until a complete group was obtained, and this was followed by assignment of a consecutive group of patients to the wait list group. Regardless of random assignment to the 2 groups, all subjects received chapters from the publication “IBS and the Mind-Body Brain-Gut connection”(43) and wait-list control subjects were informed that they would be able to attend the psycho-educational class once the study ended. Subjects randomized to receive the intervention started their first session within two weeks post the randomization visit (week 4). Once the questionnaires were completed, a third and fourth visit was scheduled at the end of the intervention evaluation (week 12) and at the follow-up approximately 3 months after enrollment. A study nurse made phone calls to all subjects, including those participants in the wait-listed control group at weeks 4, 8, and 11, as well as before the final follow-up assessment. During the phone calls subjects were asked how they were doing and were also given the opportunity to ask study-related questions.
Statistical analysis
Repeated Measures General Linear Mixed-effects Model
The hypothesized influence of the psycho-educational intervention on primary (IBS symptom severity) and secondary (health-related quality of life (QoL), affect, and coping styles) outcomes were tested using focused linear contrast analyses between groups at the end of the intervention and 3 month follow-up using estimates from a repeated measures general linear mixed effects model (RM GLMM) in SAS v9.3. For each primary and secondary outcome, we specified a model with intervention group, time, and the interaction of intervention group and time as factors. In addition, the outcome measure at baseline was mean centered and included as a covariate to statistically control for any pretreatment differences between the intervention groups that may influence outcome(44). For each model, a first-order autoregressive model yielded the best fit among the commonly used covariance structures as indicated by Akaike’s Information Criteria.
Moderator Analysis
We performed an exploratory analysis to investigate the moderating effects of baseline QoL on the intervention effects on GI symptom severity. This was accomplished by adding the moderator and the moderator*intervention group as factors to RM GLMM model described above for the primary outcome variable. Under this framework, a significant moderator*intervention group interaction indicates a significant moderator effect, i.e. the effect of the intervention depends on the value of the moderator. Given significant moderator effects the results were reported with the intervention effects and the direction of those effects was evaluated at the high (+1 SD from mean), average (mean), and low (− 1 SD from mean) levels (For a more detailed review of the methods see Holroyd, Labus, Carlson, 2009)(44).
Mediation Analysis
Simultaneous regression analysis was applied to test prospective (time-lagged) mediation models to identify potential mechanisms underlying the class intervention effects (45). We examined whether the influence of the class intervention on GI symptom severity measured at 3 month follow-up was mediated by changes in IBS-QoL, Anxiety, Depression, VSI, and Catastrophizing post intervention. We also examined the mediating effects of change in GI symptom severity assessed post intervention on the intervention effects on QoL observed at 3 month follow up.
Figure 1 depicts the moderated mediation model framework where GI symptom severity serves at the mediated outcome (See Figure 1, adapted from Tein et al. 2004)(46). Change in the mediator and outcome variable was represented in the model by including baseline/pre-intervention measurements (Figure 1, paths: d.1, e.1, e.2). Mediation was examined in the context of baseline levels of QoL which was identified as a significant moderator of the effects of the intervention GI symptom severity (Figure 1, paths: f.1, f.2, g.1, g.2(46). Only coefficients for the paths that were critical in evaluating the hypothesized mediation are reported and include the effect of the intervention on the change in the mediator at post intervention (Figures 1, path a), the direct effect of the mediator on the outcome (Figure 1, path b), the direct effect of intervention on the outcome variable (path c’), and the indirect or mediated effect of intervention on the outcome (Figures 1, path a* b). The psycho-education intervention effect was represented by the class versus wait-list (control) contrast coded 1 −1. Analyses were implemented in AMOS 18.0.02 using full information likelihood estimation. Standard errors of direct and indirect effects were determined using bootstrapping with 5000 samples(47, 48). We report parameter estimates and bootstrapped standard errors. To avoid Type II errors we emphasize effect sizes rather than significance testing as has been recommend for program evaluation with small samples. In addition, we calculated 95% confidence intervals for the parameter estimates. To assess the effect of the mediator we calculated effect size Hedges’ g, which is considered a more accurate effect size measure than Cohen’s d because it adjusts for sample sizes(49). Hedges’ g reflects the impact the intervention on the outcome through the mediator, i.e. the mediated effect, in the scale of standard deviation units. As a rule of thumb, an effect size of g=.80 is consider large explaining 14% of the variance, .50 medium (6% variance explained) and .20 small (1% of the variance explained).
Figure 1. General moderated mediation model framework (Adapted from Tein et al., 2004)46.
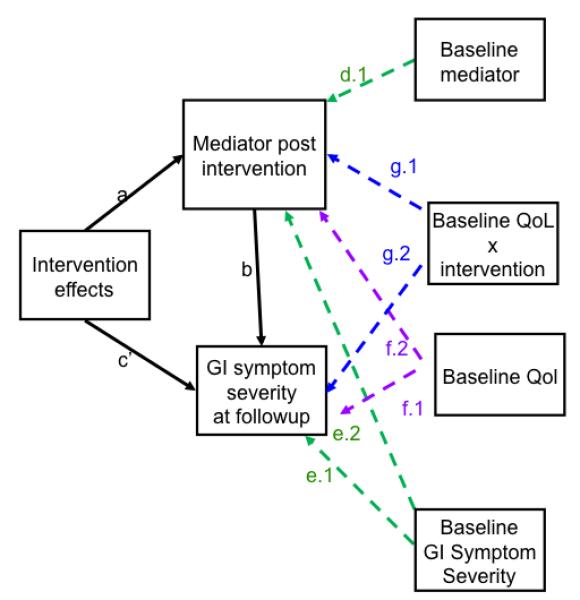
a = effect of intervention on mediator variable assessed at the end of intervention; b = effect of mediator assessed at the end of intervention on outcome at 3 month follow up; c’ = direct effect of intervention on outcome at 3 month follow up; All path estimates adjusted for baseline measures (d.1, e.1, e.2) and the moderator effects (g1, g2, f1, f2).
A priori power analysis based on a two sided independent t-test for the linear contrasts applied to test the main hypotheses indicated that at an alpha =.05, 34 cases per group were required to detect a moderate effect size (Cohen’s d = .70) with adequate power (1-Beta = .80). Demographic characteristics and baseline measures were compared between the intervention and the control groups using independent t-tests for continuous variables and chi-square tests for categorical data.
Results
Demographic and baseline measurements
Tables 2 and 3 show the demographic and psychological characteristics of both groups. There were no significant differences between the intervention (psycho-education intervention, N=34) and the wait-list (control, N=35) group in the distribution of sex (77% vs. 69% females) or age (46.3 ± 13.0 vs. 47.3 ± 12.3 years). There were no significant group differences regarding predominant bowel habits and ethnicity, but marital status differed between groups (p = 0.04), and the psycho-education group tended to have somewhat higher educational levels (p = 0.08).
The majority of the study sample reported overall symptoms as being moderate to severe (mild 10.3%, moderate 26.5%, severe 54.4%, very severe 8.8%) without any significant differences between the intervention group (mild 14.7%, moderate 35.3%, severe 44.1%, very severe 5.9%) and the control group (mild 5.9%, moderate17.6%, severe 64.7%, very severe 11.8%). However, the mean symptom severity score at baseline was somewhat lower in the patients that received the intervention compared to the control group (10.1 ± 4.2 vs. 12.7 ± 3.8; p =0.01) (Table 2).
As measured by the HAD, both the active treatment and the control groups displayed clinical levels of anxiety, but not depression based on the HAD cutoffs (39). Compared to the control group, the intervention group had a higher mean score for anxiety (9.8 ± 3.5 vs. 7.5 ± 4.8; p =.04). However, there were no significant differences between the intervention group and the control group regarding the proportion of patients with depression symptoms (4.7 ± 3.5 vs. 5.4 ± 4.3; p = 0.39). No significant group differences were observed at baseline for the QoL measures, VSI, or Coping Scale.
Intervention Effects
Results of the linear contrasts performed to test for the hypothesized group differences in the primary and secondary outcomes are presented in Table 4. Although our main hypotheses were tested using focused linear contrast, we also report on the omnibus tests from the model. No significant intervention group*time effects were observed in the repeated measures general linear mixed effects model (RM GLMM).
Primary Outcomes
After controlling for baseline levels of overall symptom severity (p < 0.0001), the effect of the intervention on symptom severity was significant (p =.0003). The main effect for time in the model was not significant. Hypotheses testing with linear contrasts indicated that patients receiving the psycho-education intervention demonstrated lower overall severity ratings compared to the control group at the end of the intervention (7.8 vs. 10.9, p = 0.002, Hedge’s g=−.78), and this difference was maintained at the 3-month follow-up (6.8 vs. 10.2, p = 0.001, g=−.85).
Secondary Outcomes
The main effect of the intervention on total IBS-QoL was significant (p = 0.002) after controlling for baseline QoL levels (p < 0.0001). The main effect for time was significant (p=.04). Patients receiving the intervention demonstrated significantly higher QoL scores than controls at the end of the intervention (75.6 vs. 66.4, p=.002, g=.77) and at the 3-month follow-up (77.6 vs. 70.2, p=.012, g=.62).
After adjusting for baseline levels of affect (p’s <.0001), the intervention reduced depression (p = 0.006) but not anxiety (p = 0.13). Patients receiving the intervention demonstrated lower depression scores at the end of the intervention compared to the controls (4.6 vs. 6.5, p = 0.005, g=−.68) and this difference was maintained at follow-up (4.2 vs. 5.5, p = 0.04, g=−.50). The main effect for time was only significant in the depression model (p=.04).
After controlling for baseline visceral sensitivity (p < 0.0001), the main effect of the psycho-education intervention on visceral sensitivity (VSI) levels was significant (p = 0.003) as was the main effect of time (p=.01). Patients receiving the intervention demonstrated significantly less visceral sensitivity than controls at end of the class (34.0 vs. 42.3, p = 0.001, g=−.84). Even though patients receiving the intervention maintained decreased visceral sensitivity at the 3-month follow-up assessment, group differences were not maintained (37.4 vs. 32.7, p = 0.06, g=−.42) due to a significant reduction in visceral sensitivity in the control group.
After controlling for baseline levels, the main effects of intervention were significantly reduced for coping skills: catastrophizing (p < 0.0001), improved ability to control symptoms (p =0.009), and improved ability to change/decrease symptoms (p = 0.008). Compared to controls, patients receiving the intervention showed improvements in catastrophizing by the end of the psycho-education intervention (7.4 vs. 11.6, p = 0.001, g=−.87), and this difference was maintained at follow-up (5.9 vs. 8.9, p = 0.012, g=−.62). Compared to controls, patients receiving the intervention tended to demonstrate improved coping skills to control symptoms at the end of the intervention (3.2 vs. 2.6, p = 0.03, g=.52) and this improvement was maintained at 3-month follow-up (3.2 vs. 2.5, p = 0.02, g=.56). Patients receiving the intervention also demonstrated improvements in their coping skills related to their ability to change/decrease symptoms at the end of the intervention compared to those in the control group (3.0 vs. 2.1, p = 0.002, g=.77) but this difference was no longer significant at the 3-month follow-up assessment (2.6 vs. 2.3, p = 0.14, g=.36).
QoL moderates the effect on pyschoeducational intervention on GI symptom Severity
Baseline QOL moderated the effects of the intervention on symptom severity as evidenced by a significant interaction between the intervention and baseline levels of IBS-QoL (p = 0.04). Interestingly, the psycho-education intervention had no effects on symptom severity among patients with high baseline levels of IBS-QoL. For average levels of QoL, severity scores are higher in the control group compared to the intervention group at the end of the intervention (p=.0006) and at follow up p<.0001). This was also observed for low levels of QOL (p=.0005, p=.0002).
Mediators of Intervention effects on GI Symptom Severity at 3 Month Follow-up
Table 5 presents the mediator analyses of the intervention effects on GI symptom severity, in the context of baseline levels of QoL. Only coefficients for the paths that are critical for evaluating the hypothesis of mediation are presented
IBS QoL
The test for mediation analyses indicated that under conditions of moderate to low baseline IBS-QoL scores, the effects of the psycho-education intervention on GI symptom severity at 3 month follow up was mediated by change in QoL levels by the end of the intervention. Mediation was greatest at low (g= −.60) compared to moderate (g= −.49) baseline levels of total IBS-QoL scores.
Anxiety
Changes in anxiety at the end of intervention appeared to mediate the effects of the intervention on GI symptom severity at 3 month follow up especially for individuals with low baseline levels of QoL (g=−.54)
Depression
Changes in depression by end of the intervention showed weak to moderate evidence for mediating the effects of the intervention on GI symptom severity at 3 month follow up for low, moderate and high baseline scores of QoL (g=−.25 to −.29).
VSI
Changes in VSI by end of the intervention showed small moderate effects for mediating the effects of the intervention on GI symptom severity at 3 month follow up with the larger effects observed for low baseline QoL scores (g=−.39).
Catastrophizing
Changes in catastrophizing post intervention demonstrated a trend for mediating the effects of the intervention on GI symptom severity at 3 month follow up. As baseline IBS-QoL decreased from high to low, the mediating effects of changing catastrophic cognitions at 3 month follow up increased (g=−.27 to −.48).
Changes in GI Symptom Severity as a Mediator of The intervention effects on QoL
Changes in GI symptom severity post intervention mediated the effects of the psycho-education intervention on IBS-QoL at the 3-month follow up assessment for low (g=.65) to moderate (g=.59) baseline levels of QoL (Table 6).
Discussion
In this study we evaluated the feasibility and effectiveness of a brief, group psycho-educational intervention for moderate to severe IBS patients seen at a tertiary referral center. The results demonstrate that a brief 5-week psycho-educational group therapy intervention can improve IBS symptoms in this patient population. Compared to a wait-list control, patients undergoing the treatment reported overall significant reduction in IBS symptom severity and significant improvement in health related quality of life (QoL), and many of the improvements were maintained at 3 months follow up. These results are similar to those seen in other studies that focused on patient education(26, 30). The effect size differences between groups on IBS-QOL (hedge’s g=−.78 at post intervention, −.87 at three month follow up) are larger than the small (Cohen’s d=.20) to moderate (Cohen’s d=.57) effect sizes reported in other cognitive behavioral and mindfulness approaches, (27, 29, 51) and suggest that the observed findings are clinically meaningful. In addition, the intervention helped patients to reduce symptoms of depression (g= −.50) and visceral anxiety (g=−.84). The intervention also gave patients tools to control their symptoms (g=.52)and improve catastrophizing (g=−.87) both of which were maintained at the 3-month follow up assessment.
The results from our study are similar to landmark studies published in the field, on utilizing cognitive behavior therapy (CBT) to improve IBS symptoms and improve quality of life(33, 46, 48). For example, Lackner et al (2010)(33) sought to identify the circumstances under which a short 4 week CBT intervention was effective in reducing IBS related symptoms post intervention and at follow-up. Similar to the Lackner et al (2010)(33) study we were also able to demonstrate reduced IBS symptoms and improved coping using a short 5 week group based CBT and relaxation psycho-education intervention, despite the fact that patients had limited number of direct contact hours with a physician. Similar to both Morris et al. (2010)(48) and Jarrett et al. (2009)(46) CBT based interventions, we were also able to demonstrate improved self-management skills among IBS patients.
Despite the reported effectiveness of CBT interventions in decreasing IBS symptoms and improving QoL, primary limitations exist related to traditional CBT interventions, including cost, shortage of adequately trained therapists, long wait-lists to get into treatment, time requirements involved in purely psychologically based therapies, and the resistance of a significant number of patients to engage in only psychologically based treatments(28, 33). As a result of these limitations, several modifications to the traditional CBT format have been evaluated (e.g. patient administered, group based and Internet focused), and these studies have shown that CBT based interventions can be delivered in different, more cost effective formats(33, 46, 48).
Moderators and mediators of intervention outcomes
Baseline quality of life (QoL-BL) served as a predictor to the success of the intervention in decreasing IBS symptoms and in improving QoL. In other words, baseline QoL functioned as a moderator of the intervention outcome. Patients with low or moderate baseline OoL scores demonstrated the greatest improvement in symptom severity and QoL post intervention. Similarly, improvements in IBS-QoL by the end of the intervention mediated improvements in overall GI symptom severity at 3 month follow up in individuals with low to moderate baseline values of IBS QoL, suggesting that an alternative intervention may be more helpful for individuals with higher QoL baseline levels.
Limitations
Due to the nature of organizing a group therapy class, block randomization was used to assign participants to the intervention and control groups in this study, resulting in some baseline differences in symptom severity and anxiety However, there were no significant demographic differences between the groups, and all analyses were performed controlling for baseline differences in clinical variables. Although, we can expect that there were some limitations to the study in terms of expectations of the waitlist control strategy. While not ideal, the use of a wait-list control condition in this study as in other initial studies of IBS interventions, does demonstrate the positive effects for the class are not due to simply variability in IBS symptoms over time or repeated measurements (29). Further studies with more active control or comparator conditions will of course be necessary to determine if specific class components or expectations are driving the intervention effects. As the results were obtained in a relatively small sample of patients, our findings need replication in a larger randomized controlled trial before a final conclusion can be made regarding the efficacy of this form of intervention. A larger sample would also make it possible to identify possible differences in treatment effectiveness in subgroups of patients based on predominant bowel habit or pain predominance.
Summary and clinical implications
This study demonstrates the feasibility of a cost-effective brief group psycho-educational therapy intervention that equaled the cost of one-hour consultation with a gastroenterologist. Patients attending the psycho-education classes improved on all key measures by the end of the intervention, and demonstrated lower overall symptom severity ratings than those in the control group. The present study suggests that a brief CBT group psycho-educational model is an efficient, efficacious, and clinically useful treatment that can provide symptom reduction, and improvement in quality of life of patients. Like other recently proposed novel delivery methods of cognitive behavioral approaches, the psycho-educational group intervention would be beneficial to patients and clinicians, by reducing the cost of treatment, the amount of unnecessary follow up visits to clinicians, and enhance the patients ability to self-manage and cope with the symptoms of their condition. In addition, when combined with specific pharmacologic therapies, it may reduce side effects, increase effectiveness of the drug and increase compliance. It is also important to note that although group psycho-educational interventions appear to be a helpful adjunct to standard medical care they are not commonly available for IBS patients. This is likely a result of several factors including lack of availability of appropriately trained clinicians, added cost and inadequate reimbursement for psychosocial interventions, and a general bias towards pharmacotherapy among patients and providers. It is hoped that evidence like that provided in this study and others will produce changes in health care delivery that can lead to expansion of availability of appropriate psychosocial treatments.
Supplementary Material
Acknowledgements
Guarantor of the article: Dr Emeran A Mayer will be acting as the submission’s guarantor.
Financial Support This study was supported in part by GlaxoSmithKline, and grants from the National Institutes of Health P50 DK64539 and R24 AT002681.
Appendix
Table 2.
Sample Demographics
| INTERVENTION (PSYCHO- EDUCATION CLASS) (N=34) |
CONTROL (N=35) |
P-VALUE | |
|---|---|---|---|
| Gender (%) | |||
| – Female | 76.5% | 68.6% | 0.47 |
| – Male | 23.5% | 31.4% | |
| Age (mean±SD) | 46.3±13.0 | 47.3±12.3 | 0.30 |
| Ethnicity (%) | |||
| – Asian | 3.1% | 0.0% | 0.67 |
| – African American | 6.3% | 11.8% | |
| – White | 84.4% | 82.4% | |
| – Hispanic | 3.1% | 2.9% | |
| – Other | 3.1% | 2.9% | |
| Marital status (%) | |||
| – Never married | 47.1% | 52.9% | 0.04* |
| – Married | 47.0% | 20.7% | |
| – Divorced | 5.9% | 23.5% | |
| – Widowed | 0.0% | 2.9% | |
| Education (%) | |||
| – High school graduate | 0.0% | 3.0% | 0.08 |
| – Some college | 17.6% | 42.4% | |
| – College graduate | 29.4% | 24.2% | |
| – Any post-graduate work | 52.9% | 30.4% | |
| Bowel habit (%) | |||
| – Constipation (IBS-C) | 23.5% | 45.7% | 0.14 |
| – Diarrhea (IBS-D) | 50.0% | 31.4% | |
| – Alternating (IBS-A) | 26.5% | 22.9% | |
NOTE. Demographic characteristics of the group with active intervention (psycho-education) and the group with inactive treatment (control/wait-listed).
Table 3.
Psychological Characteristics of Study Sample
| ACTIVE INTERVENTION |
CONTROL | P-VALUE | |
|---|---|---|---|
| GI symptom severity | 10.1±4.2 | 12.6±3.7 | 0.01* |
| IBS-QoL | 67.4±16.2 | 63.8±18.4 | 0.21 |
| HAD | |||
| – Anxiety | 9.8±3.5 | 7.6±4.6 | 0.04* |
| – Depression | 4.7±3.9 | 5.4±4.3 | 0.39 |
| VSI | 42.2±16.9 | 38.2±18.4 | 0.34 |
| Coping skills | |||
| - Catastrophizing | 12.0±7.8 | 9.5±7.3 | 0.67 |
| - Control | 2.5±1.3 | 2.3±1.2 | 0.18 |
| - Symptom Change | 2.3±1.4 | 2.0±1.2 | 0.16 |
NOTE. Assessment measures at baseline in the intervention (psycho-education) and control (waitlisted) groups, displayed as mean ± SD.
Table 4.
Within and between group parameter estimates for the primary and secondary outcomes at post intervention and 3 month follow-up
| POST INTERVENTION | 3 MONTH FOLLOW-UP | |||||
|---|---|---|---|---|---|---|
| Measures | Estimate(SE) | 95% CI | p | Estimate(SE) | 95% CI | p |
| 1. GI Symptom Severity | ||||||
| Control | 10.90 (.67) | 9.58, 12.23 | 10.20 (.67) | 8.87, 11.52 | ||
| Class | 7.82 (.67) | 6.50, 9.15 | 6.83 (.68) | 5.49, 8.17 | ||
| Difference | 3.08 (.96) | 1.17, 4.99 | .002 | 3.37 (.97) | 1.44, 5.29 | .001 |
| 2. QoL | ||||||
| Control | 66.42 (2.05) | 62.34, 70.50 | 70.22 (2.08) | 66.09, 74.35 | ||
| Class | 75.62 (2.03) | 71.59, 79.65 | 77.64 (2.00) | 73.65, 81.62 | ||
| Difference | −9.20 (2.89) | −14.95, −3.45 | .002 | −7.42 (2.30) | −13.17, −1.66 | .012 |
| 3. Depression | ||||||
| Control | 6.49 (.48) | 5.55, 7.43 | 5.54 (.46) | 4.62, 6.46 | ||
| Class | 4.61 (.46) | 3.70, 5.52 | 4.19 (.46) | 3.28, 5.11 | ||
| Difference | 1.88 (.66) | .57, 3.19 | .005 | 1.34 (.66) | .04, 2.64 | .043 |
| 4. Anxiety | ||||||
| Control | 9.24 (.55) | 8.16, 10.33 | 8.63 (.54) | 7.57, 9.69 | ||
| Class | 8.00 (.52) | 6.96, 9.05 | 7.82 (.53) | 6.76, 8.87 | ||
| Difference | 1.24 (.77) | −.28, 2.77 | .109 | .81 (.76) | −.70, 2.32 | .290 |
| 5. VSI | ||||||
| Control | 42.31 (1.71) | 38.91, 45.70 | 37.43 (1.69) | 34.08, 40.78 | ||
| Class | 34.04 (1.66) | 30.74, 37.34 | 32.71 (1.77) | 29.19, 36.22 | ||
| Difference | 8.26 (2.39) | 3.52, 13.01 | .001 | 4.72 (2.46) | −.15, 9.59 | .058 |
| 6. Coping Skills: Catastrophizing | ||||||
| Control | 11.63 (.82) | 10.00, 13.27 | 8.89 (.82) | 7.25, 10.52 | ||
| Class | 7.40 (.84) | 5.75, 9.06 | 5.88 (.84) | 4.22, 7.53 | ||
| Difference | 4.23 (1.18) | 1.89, 6.56 | .001 | 3.01 (1.18) | .68, 5.35 | .012 |
| 7. Coping Skills: Control | ||||||
| Control | 2.57 (.21) | 2.16, 2.97 | 2.54 (.21) | 2.13, 2.94 | ||
| Class | 3.20 (.20) | 2.80, 3.60 | 3.23 (.21) | 2.83, 3.64 | ||
| Difference | −.64 (.29) | −1.21, −.07 | .029 | −.70 (.29) | −1.27, −.012 | .019 |
| 8. Coping Skills: Symptom Change | ||||||
| Control | 2.06 (.20) | 1.67, 2.46 | 2.21 (.20) | 1.81, 2.61 | ||
| Class | 2.96 (0.20) | 2.56, 3.35 | 2.63 (.20) | 2.23, 3.03 | ||
| Difference | −.89 (.28) | −1.45, −.33 | .002 | −.42 (.29) | −.99, .15 | .143 |
Bootstrapped estimates and standard errors
CI: Confidence Intervals
Measures: 1. GI symptom severity; 2. IBS-QoL: IBS Quality of Life Measure(37, 38); 3. Depression using the HAD: Hospital Anxiety and Depression(39,40); 4. Depression using the HAD: Hospital Anxiety and Depression(39,40); 5. VSI: Visceral Sensitivity Index(36); 6. Coping Skills Catastrophizing(41); 7. Coping Skills Control(41); 8. Coping Skills Symptom Change)(41)
Table 5.
Mediators of the Intervention Effects on GI Symptom Severity at 3 Month Follow-Up
| Mediator | IBS-QoL (Baseline) |
a | 95% CI (a) |
b | 95% CI (b) |
c’ | 95% CI (c’) |
a*b | 95% CI (a*b) |
Hedge’s g |
|---|---|---|---|---|---|---|---|---|---|---|
| IBS-QoL | ||||||||||
| High | 0.23 (1.39) |
−2.49 2.95 |
−0.10* (.04) |
−0.18 −0.02 |
− 1.31* (.45) |
−2.19 −0.43 |
−0.02 | −0.30 0.25 |
−.04 | |
| Moderate | 4.02* (1.39) |
1.30 6.74 |
−0.10* (.04) |
−0.18 −0.02 |
− 1.64* (.49) |
−2.60 −0.68 |
−0.38 | −0.82 0.01 |
−.49 | |
| Low | 7.82* (1.39) |
5.10 10.54 |
−0.10* (.04) |
−0.18 −0.02 |
− 1.98* (.56) |
−3.08 −0.88 |
− 0.78 * |
−1.45 −0.11 |
−.60 | |
| Anxiety | ||||||||||
| High | − 0.24* (.35) |
−0.92 0.44 |
0.26* (.11) |
0.04 0.48 |
− 2.01* (.44) |
−2.89 −1.15 |
−.06 | −0.25 0.12 |
−.18 | |
| Moderate | − 0.77* (.35) |
−1.45 −0.09 |
0.26* (.11) |
0.04 0.48 |
− 2.38* (.45) |
−3.26 −1.50 |
−.20 | −0.45 0.04 |
−.44 | |
| Low | − 1.30* (.35) |
−1.98 −0.62 |
0.26* (.11) |
0.04 0.48 |
− 2.75* (.46) |
−3.66 −1.84 |
−.34* | −0.67 −0.01 |
−.54 | |
| Depression | ||||||||||
| High | −0.51 (0.30) |
−1.09 0.07 |
.146 (0.13) |
−0.11 (0.40) |
−1.69 (.44) |
−2.56 −0.82 |
−0.07 | −0.23 0.08 |
−0.25 | |
| Moderate | − .935* (0.30) |
−1.52 −0.35 |
.146 (0.13) |
−0.11 0.40 |
− 2.17* (.46) |
−3.06 −1.28 |
−0.14 | −0.39 0.12 |
−0.28 | |
| Low | − 1.37* (0.30) |
−1.95 −0.79 |
.146 (0.13) |
−0.11 0.40 |
− 2.65* (.47) |
−3.58 −1.72 |
−0.20 | −0.56 0.16 |
−0.29 | |
| VSI | ||||||||||
| High | − 2.61* (1.15) |
−4.86 −0.36 |
0.05 (.033) |
−0.01 0.11 |
− 1.37* (.485) |
−2.32 −0.42 |
−.13 | −0.33 0.07 |
−.33 | |
| Moderate | − 4.12* (1.15) |
−6.37 −1.87 |
0.05 (.033) |
−0.01 0.11 |
− 2.02* (.497) |
−2.99 −1.05 |
−.21 | −0.47 0.06 |
−.38 | |
| Low | − 5.64* (1.15) |
−7.89 −3.39 |
0.05 (.033) |
−0.01 0.11 |
− 2.68* (.512) |
−3.68 −1.68 |
−.28 | −0.63 0.07 |
−.39 | |
| Catastrophizing | ||||||||||
| High | − 0.79* (.656) |
−2.08 0.50 |
0.14* (.069) |
0.00 0.28 |
− 1.34* (.452) |
−2.26 −0.45 |
−.11 | −0.32 0.10 |
−.27 | |
| Moderate | − 1.79* (.656) |
−3.08 −0.50 |
0.14* (.069) |
0.00 0.28 |
− 2.04* (.465) |
−2.95 −1.13 |
−.26 | −0.55 0.05 |
−.43 | |
| Low | − 2.79* (.656) |
−4.08 −1.50 |
0.14* (.069) |
0.00 0.28 |
− 2.74* (.488) |
−3.70 −1.78 |
−.39 | −0.81 0.03 |
−.48 | |
CI: 95% bootstrapped confidence intervals
a = change in the mediator at posttest,
b = the direct effect of the mediator on the outcome,
c’= the direct effect of intervention on the outcome variable,
a*b = the indirect effect of intervention on the outcome
= parameter estimates where 95% CI do not contain zero.
The psychoeducation intervention effect was represented by the class (intervention) versus wait-list (control) contrast coded 1 −1.
Table 6.
GI Symptom Severity Mediates Intervention Effects on QoL at 3 Month Follow-Up
| IBS-QoL (Baseline) |
PATH a |
95% CI a |
PATH b |
95% CI b |
PATH c’ |
95% CI c’ |
PATH ab |
95% CI ab |
HEDGE’S (INDIRECT EFFECT) g |
|---|---|---|---|---|---|---|---|---|---|
| High | −0.93* (.46) |
−1.83 −0.03 |
−0.88* (.321) |
−1.51 −0.25 |
−0.12 (1.31) |
−2.69 2.45 |
0.82 | −0.17 1.80 |
.43 |
| Moderate | −1.74* (.46) |
−2.64 −0.84 |
−0.88* (.321) |
−1.51 −0.25 |
1.75* (1.39) |
−0.97 4.47 |
1.53* | 0.18 2.88 |
.59 |
| Low | −2.55* (.46) |
−3.45 −1.65 |
−0.88* (.321) |
−1.51 −0.25 |
3.61* (1.51) |
0.65 6.57 |
2.24* | 0.46 4.03 |
.65 |
CI: 95% bootstrapped confidence intervals
A = change in the mediator at posttest,
b = the direct effect of the mediator on the outcome,
c’= the direct effect of intervention on the outcome variable,
a*b = the indirect effect of intervention on the outcome
= parameter estimates where 95% CI do not contain zero.
The psychoeducation intervention effect was represented by the class (intervention) versus wait-list (control) contrast coded 1 −1.
Footnotes
Randomized Clinical Trials This study was not registered with the clinical trials registry as the study was conducted between 2002 and 2004, before the registry requirements. Full trial protocol can be assessed by contacting PI on the study (Dr. Emeran Mayer) at emayer@ucla.edu
Disclosure An abstract of some of the preliminary results were presented prior to this manuscript: Mayer EA, Naliboff BD, Raeen H, Mayer M, Liu C, Bolus R. Psycho-educational intervention in IBS patients improves symptoms, symptom-related anxieties, coping and health-related quality of life. Gastroenterology 128: A-67, 2005.
Specific author contributions: Labus: data analysis and manuscript writing
Gupta: data analysis & manuscript writing
Gil: data collection & manuscript writing
Posserud: data collection, study intervention
Mayer, Minou: study intervention, study coordination
Raeen: data collection, study intervention
Bolus: data collection, study intervention
Simren: study conceptualization
Naliboff: study design, study conceptualization, manuscript writing
Mayer, Emeran: study design, study conceptualization, study intervention, and manuscript writing
All authors approved the final version of the manuscript.
Supporting Documents Table 1: Session-by-Session Outline of the Intervention Details regarding the session-by-session breakdown of % effort contributed by either the gastroenterologist and therapist and focus of each session over the entire intervention.
References
- 1.Torri A, Toda G. Management of irritable bowel syndrome. Internal Med. 2004;43(5):353–9. doi: 10.2169/internalmedicine.43.353. [DOI] [PubMed] [Google Scholar]
- 2.Mayer EA. Irritable Bowel Syndrom. New England Journal of Medicine. 2008;358(16):1692–9. doi: 10.1056/NEJMcp0801447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hutchings HA, Wareham K, Baxter JN, Atherton P, Kingham JG, Duane P, et al. A Randomised, Cross-Over, Placebo-Controlled Study of Aloe vera in Patients with Irritable Bowel Syndrome: Effects on Patient Quality of Life. ISRN gastroenterology. 2011;2011:206103. doi: 10.5402/2011/206103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.null, Brandt LJ, Chey WD, Foxx-Orenstein AE, Schiller LR, Schoenfeld PS, et al. An evidence-based position statement on the management of irritable bowel syndrome. The American journal of gastroenterology. 2009;104(Suppl 1):S1–35. doi: 10.1038/ajg.2008.122. [DOI] [PubMed] [Google Scholar]
- 5.Tillisch K, Labus J, Nam B, Bueller J, Smith S, Suyenobu B, et al. Neurokinin-1-receptor antagonism decreases anxiety and emotional arousal circuit response to noxious visceral distension in women with irritable bowel syndrome: a pilot study. Alimentary pharmacology & therapeutics. 2012;35(3):360–7. doi: 10.1111/j.1365-2036.2011.04958.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koloski N, Boyce P, Jones M, Talley N. What level of IBS symptoms drives impairment in health-related quality of life in community subjects with irritable bowel syndrome? Quality of Life Research. 2012;21(5):829–36. doi: 10.1007/s11136-011-9985-5. [DOI] [PubMed] [Google Scholar]
- 7.Tillisch K, Mayer EA, Labus J, Stains J, Chang L, Naliboff BD. Sex specific alterations in autonomic function among patients with irritable bowel syndrome. Gut. 2005;54(10):1396–401. doi: 10.1136/gut.2004.058685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fass R, Fullerton S, Tung S, Mayer EA. Sleep disturbances in clinic patients with functional bowel disorders. The American journal of gastroenterology. 2000;95(5):1195–2000. doi: 10.1111/j.1572-0241.2000.02009.x. [DOI] [PubMed] [Google Scholar]
- 9.Mayer EA, Tillisch K. The brain-gut axis in abdominal pain syndromes. Annu Rev Med. 2011;62:381–96. doi: 10.1146/annurev-med-012309-103958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wiklund IK, Fullerton S, Hawkey CJ, Jones RH, Longstreth GF, Mayer EA, et al. An irritable bowel syndrome-specific symptom questionnaire: development and validation. Scandinavian journal of gastroenterology. 2003;38(9):947–54. doi: 10.1080/00365520310004209. [DOI] [PubMed] [Google Scholar]
- 11.Spiegel BM, Gralnek IM, Bolus R, Chang L, Dulai GS, Mayer EA, et al. Clinical determinants of health-related quality of life in patients with irritable bowel syndrome. Archives of internal medicine. 2004;164(16):1773–80. doi: 10.1001/archinte.164.16.1773. [DOI] [PubMed] [Google Scholar]
- 12.Gralnek IM, Hays RD, Kilbourne A, Naliboff B, Mayer EA. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology. 2000;119(3):654–60. doi: 10.1053/gast.2000.16484. [DOI] [PubMed] [Google Scholar]
- 13.Clave P. Treatment of IBS-D with 5-HT3 receptor antagonists vs spasmolytic agents: similar therapeutical effects from heterogeneous pharmacological targets. Neurogastroenterol Motil. 2011;23(12):1051–5. doi: 10.1111/j.1365-2982.2011.01808.x. [DOI] [PubMed] [Google Scholar]
- 14.Sands BE. The Placebo Response Rate in Irritable Bowel Syndrome and Inflammatory Bowel Disease. Digest Dis. 2009;27:68–75. doi: 10.1159/000268123. [DOI] [PubMed] [Google Scholar]
- 15.Saad RJ, Chey WD. Recent developments in the therapy of irritable bowel syndrome. Expert opinion on investigational drugs. 2008;17(2):117–30. doi: 10.1517/13543784.17.2.117. [DOI] [PubMed] [Google Scholar]
- 16.Chey WD, Maneerattaporn M, Saad R. Pharmacologic and complementary and alternative medicine therapies for irritable bowel syndrome. Gut and liver. 2011;5(3):253–66. doi: 10.5009/gnl.2011.5.3.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McFarland LV. Meta-analysis of probiotics for the prevention of antibiotic associated diarrhea and the treatment of Clostridium difficile disease. The American journal of gastroenterology. 2006;101(4):812–22. doi: 10.1111/j.1572-0241.2006.00465.x. [DOI] [PubMed] [Google Scholar]
- 18.Spiller R. Review article: probiotics and prebiotics in irritable bowel syndrome. Alimentary pharmacology & therapeutics. 2008;28(4):385–96. doi: 10.1111/j.1365-2036.2008.03750.x. [DOI] [PubMed] [Google Scholar]
- 19.Shen YH, Nahas R. Complementary and alternative medicine for treatment of irritable bowel syndrome. Canadian family physician Medecin de famille canadien. 2009;55(2):143–8. [PMC free article] [PubMed] [Google Scholar]
- 20.Hefner J, Rilk A, Herbert BM, Zipfel S, Enck P, Martens U. [Hypnotherapy for irritable bowel syndrome--a systematic review] Z Gastroenterol. 2009;47(11):1153–9. doi: 10.1055/s-0028-1109697. [DOI] [PubMed] [Google Scholar]
- 21.Gaylord SA, Whitehead WE, Coble RS, Faurot KR, Palsson OS, Garland EL, et al. Mindfulness for irritable bowel syndrome: protocol development for a controlled clinical trial. BMC complementary and alternative medicine. 2009;9:24. doi: 10.1186/1472-6882-9-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Webb AN, Kukuruzovic RH, Catto-Smith AG, Sawyer SM. Hypnotherapy for treatment of irritable bowel syndrome. Cochrane Database Syst Rev. 2007;(4) doi: 10.1002/14651858.CD005110.pub2. CD005110. [DOI] [PubMed] [Google Scholar]
- 23.Golden WL. Cognitive-behavioral hypnotherapy in the treatment of irritable-bowel-syndrome-induced agoraphobia. Int J Clin Exp Hypn. 2007;55(2):131–46. doi: 10.1080/00207140601177889. [DOI] [PubMed] [Google Scholar]
- 24.Whorwell PJ. Behavioral therapy for IBS. Nat Clin Pract Gastroenterol Hepatol. 2009;6(3):148–9. doi: 10.1038/ncpgasthep1361. [DOI] [PubMed] [Google Scholar]
- 25.Wald A, Rakel D. Behavioral and complementary approaches for the treatment of irritable bowel syndrome. Nutr Clin Pract. 2008;23(3):284–92. doi: 10.1177/0884533608318677. [DOI] [PubMed] [Google Scholar]
- 26.Ringström G, Störsrud S, Lundqvist S, Westman B, Simrén M. Development of an educational intervention for patients with Irritable Bowel Syndrome (IBS): a pilot study. BMC gastroenterology. 2009;9:10. doi: 10.1186/1471-230X-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ljotsson B, Hedman E, Andersson E, Hesser H, Lindfors P, Hursti T, et al. Internet-Delivered Exposure-Based Treatment vs. Stress Management for Irritable Bowel Syndrome: A Randomized Trial. Am J Gastroenterol. 2011;106(8):1481–91. doi: 10.1038/ajg.2011.139. [DOI] [PubMed] [Google Scholar]
- 28.Lackner JM, McCracken LM. Functional Pain Syndromes: Presentation and Pathophysiology. IASP Press; Seattle, WA: 2009. Cognitive-Behavioral Treatment of Functional Pain Disorders; pp. 491–509. [Google Scholar]
- 29.Lackner JM, Jaccard J, Krasner SS, Katz LA, Gudleski GD, Holroyd K. Self-administered cognitive behavior therapy for moderate to severe irritable bowel syndrome: clinical efficacy, tolerability, feasibility. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2008;6(8):899–906. doi: 10.1016/j.cgh.2008.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ringström G, Störsrud S, Posserud I, Lundqvist S, Westman B, Simrén M. Structured patient education is superior to written information in the management of patients with irritable bowel syndrome: a randomized controlled study. European journal of gastroenterology & hepatology. 2010;22(4):420–8. doi: 10.1097/MEG.0b013e3283333b61. [DOI] [PubMed] [Google Scholar]
- 31.Heitkemper MM, Jarrett ME, Levy RL, Cain KC, Burr RL, Feld A, et al. Self-management for women with irritable bowel syndrome. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2004;2(7):585–96. doi: 10.1016/s1542-3565(04)00242-3. [DOI] [PubMed] [Google Scholar]
- 32.Saito YA, Prather CM, Van Dyke CT, Fett S, Zinsmeister AR, Locke GR. Effects of multidisciplinary education on outcomes in patients with irritable bowel syndrome. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2004;2(7):576–84. doi: 10.1016/s1542-3565(04)00241-1. [DOI] [PubMed] [Google Scholar]
- 33.Heymann-Monnikes I, Arnold R, Florin I, Herda C, Melfsen S, Monnikes H. The combination of medical treatment plus multicomponent behavioral therapy is superior to medical treatment alone in the therapy of irritable bowel syndrome. Am J Gastroenterol. 2000;95(4):981–94. doi: 10.1111/j.1572-0241.2000.01937.x. [DOI] [PubMed] [Google Scholar]
- 34.Lackner JM, Gudleski GD, Keefer L, Krasner SS, Powell C, Katz LA. Rapid response to cognitive behavior therapy predicts treatment outcome in patients with irritable bowel syndrome. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2010;8(5):426–32. doi: 10.1016/j.cgh.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Müller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999;45(Suppl 2):II43–7. doi: 10.1136/gut.45.2008.ii43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Labus JS, Bolus R, Chang L, Wiklund I, Naesdal J, Mayer EA, et al. The Visceral Sensitivity Index: development and validation of a gastrointestinal symptom-specific anxiety scale. Alimentary pharmacology & therapeutics. 2004;20(1):89–97. doi: 10.1111/j.1365-2036.2004.02007.x. [DOI] [PubMed] [Google Scholar]
- 37.Hahn BA, Kirchdoerfer LJ, Fullerton S, Mayer E. Evaluation of a new quality of life questionnaire for patients with irritable bowel syndrome. Alimentary pharmacology & therapeutics. 1997;11(3):547–52. doi: 10.1046/j.1365-2036.1997.00168.x. [DOI] [PubMed] [Google Scholar]
- 38.Bijkerk CJ, de Wit NJ, Muris JW, Jones RH, Knottnerus JA, Hoes AW. Outcome measures in irritable bowel syndrome: comparison of psychometric and methodological characteristics. The American journal of gastroenterology. 2003;98(1):122–7. doi: 10.1111/j.1572-0241.2003.07158.x. [DOI] [PubMed] [Google Scholar]
- 39.Adams RB, Franklin RG, Rule NO, Freeman JB, Kveraga K, Hadjikhani N, et al. Culture, gaze and the neural processing of fear expressions. Social cognitive and affective neuroscience. 2010;5(2-3):340–8. doi: 10.1093/scan/nsp047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta psychiatrica Scandinavica. 1983;67(6):361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 41.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17(1):33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- 42.Kohl F. [Progressive muscle relaxation according to E. Jacobson. A modern relaxation technique] Med Monatsschr Pharm. 2002;25(3):77–87. [PubMed] [Google Scholar]
- 43.Salt WB. IBS and the Mind-Body Brain-Gut Connection. Parkview Publishing; Columbus: 1997. [Google Scholar]
- 44.Holroyd KA, Labus JS, Carlson B. Moderation and mediation in the psychological and drug treatment of chronic tension-type headache: the role of disorder severity and psychiatric comorbidity. Pain. 2009;143(3):213–22. doi: 10.1016/j.pain.2009.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76(4):408–20. [Google Scholar]
- 46.Tein JY, Sandler IN, MacKinnon DP, Wolchik SA. How did it work? Who did it work for? Mediation in the context of a moderated prevention effect for children of divorce. Journal of Consulting and Clinical Psychology. 2004;72(4):617–24. doi: 10.1037/0022-006X.72.4.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Preacher KJ, Rucker DD, Hayes AF. Addressing Moderated Mediation Hypotheses: Theory, Methods, and Prescriptions. Multivariate Behavioral Research. 2007;42(1):185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- 48.Jarrett ME, Cain KC, Burr RL, Hertig VL, Rosen SN, Heitkemper MM. Comprehensive self-management for irritable bowel syndrome: randomized trial of in-person vs. combined in-person and telephone sessions. The American journal of gastroenterology. 2009;104(12):3004–14. doi: 10.1038/ajg.2009.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hansen WB, McNeal RB., Jr The law of maximum expected potential effect: Constraints placed on program effectiveness by mediator relationships. Health Education Research. 1996;11(4):501–7. [Google Scholar]
- 50.Moss-Morris R, McAlpine L, Didsbury LP, Spence MJ. A randomized controlled trial of a cognitive behavioural therapy-based self-management intervention for irritable bowel syndrome in primary care. Psychological medicine. 2010;40(1):85–94. doi: 10.1017/S0033291709990195. [DOI] [PubMed] [Google Scholar]
- 51.Craske MG, Wolitzky-Taylor KB, Labus J, Wu S, Frese M, Mayer EM, Naliboff BD. A cognitive-behavioral treatmnet for irritable bowel syndrome using interoceptive exposure to visceral sensations. Behavioral Research Therapy. 2011;49(6-7):413–421. doi: 10.1016/j.brat.2011.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.