Abstract
We present a case of a 13-year old girl experiencing recurring angina pectoris due to an occlusion of the left main coronary artery after arterial switch operation in infancy. To avoid a repeat sternotomy and the use of cardiopulmonary bypass, the patient underwent uncomplicated operative myocardial revascularization in the minimally invasive direct coronary artery bypass (MIDCAB) technique.
Keywords: Minimally invasive direct coronary artery bypass, Left main coronary artery stenosis, Arterial switch operation
INTRODUCTION
Arterial switch operation (ASO) is widely accepted as the treatment of choice for infants with transposition of the great arteries (TGA). Nevertheless, coronary lesions following ASO are not uncommon and can influence outcome. Therapeutic options include medical management, percutaneous coronary intervention (PCI) and surgical revascularization [1, 2].
Minimally invasive direct coronary artery bypass (MIDCAB)—grafting the left internal mammary artery (IMA) with the left anterior descending (LAD) artery through an anterolateral minithoracotomy under beating heart conditions—is an established alternative for revascularization of isolated LAD stenosis, and in combination with PCI for multivessel revascularization as part of a hybrid concept. But it is also more and more often used in high-risk patients, for whom cardiopulmonary bypass (CPB) with cardiac arrest seems too risky. By avoidance of sternotomy and additional CPB, a reduction of perioperative complications is possible [3, 4].
We describe our first use of the MIDCAB technique in a 13-year old patient with an occlusion of the left main coronary artery (LCA) after ASO, to reduce the negative effects associated with repeat sternotomy and CPB.
CASE REPORT
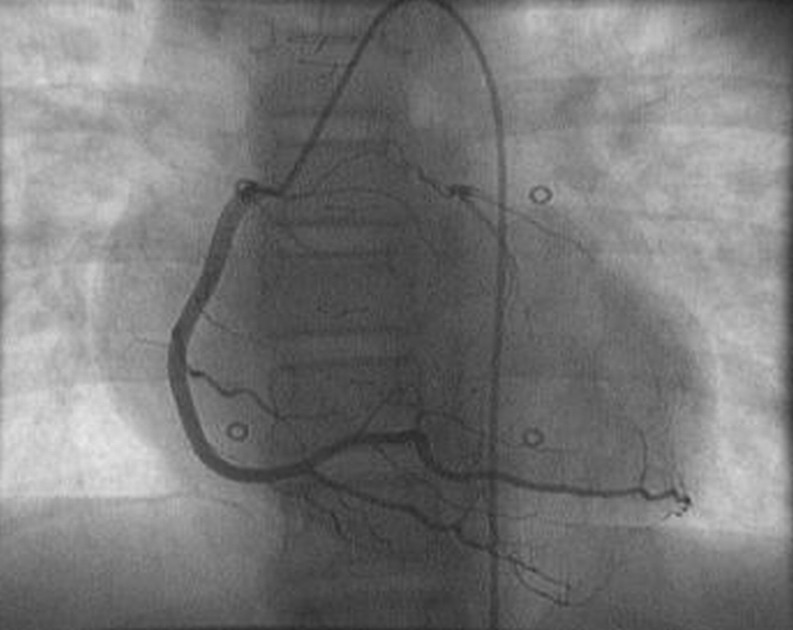
The patient was born with a transposition of TGA. She had an operative correction shortly after birth with ASO. At the 5-year follow-up, an occlusion of the LCA was diagnosed. At that time, the patient did not have any symptoms. In the 10-year follow-up, she reported deterioration of physical condition and that she increasingly developed angina pectoris symptoms during sport activities. In a diagnostic cardiac catheterization, the obstruction of the LCA was re-evaluated. Reduced perfusion was maintained via collaterals out of the right coronary artery (Fig. 1). In a stress-perfusion magnetic resonance imaging (MRI), an excessive anteroseptal ischaemia was demonstrated. The lateral wall showed no pathological findings. Several alternatives were discussed and after re-evaluation of the diagnostic findings, the MIDCAB approach appeared to be the most attractive option to reduce the negative effects associated with repeat sternotomy and CPB. The patient was then 13 years old.
Figure 1:
The cardiac catheterization shows an obstruction of the left main coronary artery with reduced perfusion via collaterals out of the right coronary artery.
The surgical technique has already been previously described in detail [3]. An anterolateral skin incision was performed. It was ensured that enough distance to the breast glandular tissue was kept in order not to impair further breast development [5]. The fifth intercostal space was opened. Pleural adhesions were minimal, whereas the left lung was tightly sticking to the mediastinum. After successful preparation of the left IMA, a good diameter and a good flow were to be seen. As parts of the former pericardium had been used for the first operation, the heart was not protected and a thorough preparation of the cardiac surface had to be done. The LAD was partially fragile and its diameter was estimated between 1 and 1.5 mm. After administration of heparin, the IMA was distally dissected to reveal a pulsatile good free flow. Sutures with tourniquets were placed proximally and distally from the planned incision site of the LAD and a time of 2 min of ischaemia and reperfusion each was chosen for preconditioning. After incision, the anastomosis was performed with a 8/0 running suture. Prepericardial fat was mobilized and served as a cover for the anastomosis to guarantee an effective protection of the distal IMA. Closing of the thoracotomy including two transcostal sutures has to be performed with meticulous care to avoid contact of the graft with the chest wall or herniation of mediastinal structures.
After extubation in the operation theatre, the patient was transferred to our intensive care unit. She was at any time cardiopulmonary stable. After 7 days, the patient was completely mobile and could be discharged to rehabilitation.
In the 1-year follow-up, the patient reports an improved physical condition. The cardiac MRI showed a good left ventricular function with excellent flow in the IMA bypass. Vitality test with adenosine stress was very good: none of the former perfusion deficits was visible anymore and no regional wall movement deficits could be located. Therefore, the patient had a very good postoperative result.
COMMENT
Coronary lesions including stenosis, compression, kinking or occlusion after ASO for TGA are not rare. The best treatment of coronary lesions is in debate. Balloon angioplasty, operative reconstruction and coronary artery bypass surgery are also proposed. Conservative treatment can be considered as well. The best treatment will also be dependent on the specific lesion at stake and must be customized [1, 2].
MIDCAB is associated with high graft patency rates in the mid-term and long-term course in experienced centres. A reduction of perioperative complications (wound infections, reoperation for management of bleeding, arrhythmias, stroke etc.) is possible by avoidance of sternotomy and CPB possible [3, 4].
The revascularization using the MIDCAB technique in children after neonatal ASO is a novel concept. The basic idea is to reduce the side-effects associated with CPB and repeat sternotomy. The concept also saves additional vascular cannulation and full systemic heparinization.
In our case, MRI showed that the LAD was the target vessel for revascularization and therefore, the MIDCAB technique was the best option. The other possibility would have been surgical reconstruction of the LCA via angioplasty. This approach restores a more physical antegrade perfusion of the coronary artery. Nevertheless, in this case an operation with CPB support and cardiac arrest would have been needed with no obvious benefit for the patient. For this reason and to spare the young patient the risk of a larger operation with cardiopulmonary arrest, we decided to perform the MIDCAB operation. In our case, the revascularization and the perioperative management were rather simple. The first assessment with MRI showed a good left ventricular function with excellent flow in the left IMA bypass.
In conclusion, our experience suggests that revascularization using the MIDCAB technique in children after neonatal ASO is a possible option in experienced centres. This novel approach should be useful in selected patients, especially, patients who would benefit from the avoidance of resternotomy and the adverse sequels associated with CPB.
Conflict of interest: none declared.
REFERENCES
- 1.Fricke TA, d'Udekem Y, Richardson M, Thuys C, Dronavalli M, Ramsay JM, et al. Outcomes of the arterial switch operation for transposition of the great arteries: 25 years of experience. Ann Thorac Surg. 2012;94:139–45. doi: 10.1016/j.athoracsur.2012.03.019. [DOI] [PubMed] [Google Scholar]
- 2.Raisky O, Bergoend E, Agnoletti G, Ou P, Bonnet D, Sidi D, et al. Late coronary artery lesions after neonatal arterial switch operation: results of surgical coronary revascularization. Eur J Cardiothorac Surg. 2007;31:894–8. doi: 10.1016/j.ejcts.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 3.Cremer J, Schoettler J, Thiem A, Grothusen C, Hoffmann G. The MIDCAB approach in its various dimensions. HSR Proc Intensive Care Cardiovasc Anesth. 2011;3:249–53. [PMC free article] [PubMed] [Google Scholar]
- 4.Holzhey DM, Cornely JP, Rastan AJ, Davierwala P, Mohr FW. Review of a 13-year single-center experience with minimally invasive direct coronary artery bypass as the primary surgical treatment of coronary artery disease. Heart Surg Forum. 2012;15:E61–8. doi: 10.1532/HSF98.20111141. [DOI] [PubMed] [Google Scholar]
- 5.Schreiber C, Bleiziffer S, Lange R. Midaxillary lateral thoracotomy for closure of atrial septal defects in prepubescent female children: reappraisal of an ‘old technique. Cardiol Young. 2003;13:565–7. [PubMed] [Google Scholar]