Abstract
Sternal cleft is a rare congenital malformation affecting the anterior part of the chest wall. Surgical closure is recommended. It should be done early during the neonatal period because of the chest's flexibility. Associated abnormalities may have been previously excluded. Different surgical repairs have been described, but none has been proved to be superior to the others. We present the description of 2 cases managed with an original surgical technique. After dissecting the two sternal bars, they were approximated with several intercostal sutures under close cardiac and respiratory monitoring. A double perichondrium flap technique was then used and resulted in a double perichondrium layer. This technique is suitable for most cases and offers satisfying anatomical restoring and cosmetic results.
Keywords: Sternal cleft, Primary repair, Congenital anomaly
INTRODUCTION
Sternal cleft (SC) is a rare congenital malformation of the superior celosomy cleft type that affects the anterior part of the chest wall. It can be either complete or partial. This latter category can be divided into superior or inferior. SC is usually asymptomatic and frequently associated with other visceral defects.
Its surgical treatment, consisting in closing the cleft, should be done early during the neonatal period because of the high flexibility of the chest. Taking advantage of the healing and adaptation potential of this age favours better results. Different techniques include primary closure [1], bone graft interposition, prosthetic closure and muscle flap interposition [2, 3]. Recommending one single technique as the best is not easy. The important points are the simplicity of the surgical repair technique, along with good aesthetical and functional results. We present 2 cases observed in our department and propose a description of an original and effective surgical technique to manage SC.
CASE REPORT
Two SC cases were recently managed in our department. Both were treated by a primary SC surgical repair consisting in a double perichondrium flap technique.
The first patient was an 8-day old full-term female who was diagnosed in the prenatal period with an anterior thoracic defect. At birth, a complete SC was confirmed. There was no circulatory or respiratory deficiency. Thoracic computed tomography (CT)-scan confirmed the complete isolated SC. Cardiac, medullar and abdominal sonographies were normal and showed no associated abnormalities. A surgical repair of this isolated SC was performed at 8 days of age. Immediate postoperative follow-up was uneventful. The patient started feeding at Day 4 postoperatively and was discharged 8 days after repair.
The second patient was a 38-day old full-term female. She presented at birth a large superior SC with an inferior cartilaginous costal bridge at birth and was completely asymptomatic and stable. No prenatal diagnosis of this malformation was made. The echocardiography showed an atrial septal defect with a left–right shunt without systemic consequences. The thoracic CT-scan confirmed the large superior SC and excluded other mediastinal defects. Lungs and heart tissues were normal. Abdominal and medullar sonographies detected no associated malformations. The patient was operated on at 38 days of age and discharged at Day 5 postoperatively. Clinical control was made for both patients at 2 and 4 months. It showed a well-united sternum with complete wound healing and a satisfying cosmetic result (Fig. 1). No recurrence was observed and no patient developed a chest wall deformity. Both remain asymptomatic without evidence of cardiorespiratory failure after 4 years and 8 months of follow-up.
Figure 1:
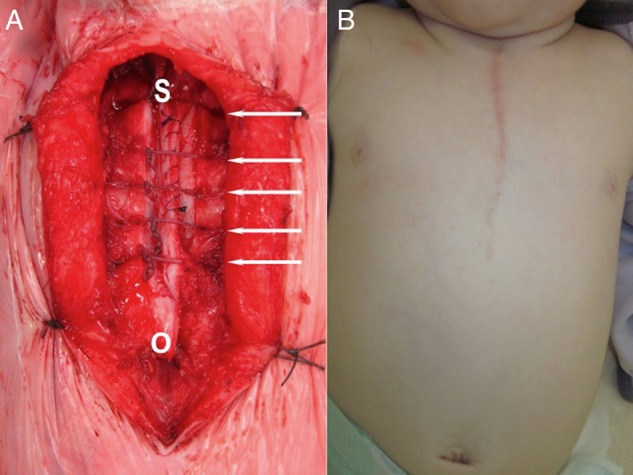
(A) Operative view after sternal reconstruction. O: place of the osteotomy. Arrows: intercostal braided non-absorbable interrupted sutures. S: superficial perichondrium suture. (B) Photograph showing the cosmetic result. The follow-up at 4 months after primary closure of sternal cleft.
SURGICAL TECHNIQUE
Surgery was done through a vertical midline incision. The skin overlying the sternal defect was excised in the middle line. It was found to be in direct contact with the pericardium. Cutaneous tissue was detached and sternal bars were carefully dissected and separated from the pericardium in order to preserve the diaphragmatic nerves. The sternal tables were freed laterally to the intercostal border. An osteotomy was performed to remove the inferior sternal bridge in the midline. An incision was made on the anterior border of the left sternal bar and on the posterior border of the right sternal bar. The underlying cartilage was exposed and two perichondrium flaps were obtained.
The two sternal bars were then approximated by several intercostal braided non-absorbable interrupted sutures. Close monitoring of the cardiac (heart rate, systolic blood pressure and central venous pressure) and respiratory (tidal volume and plateau pressure) functions was then performed for several minutes to exclude thoracic compartment syndrome before the sutures were tied. Each perichondrium flap was then sutured with the perichondrium ledge on the opposite sternal bar with absorbable sutures resulting in a double perichondrium layer (Figs 1 and 2). The skin layer was finally closed.
Figure 2:
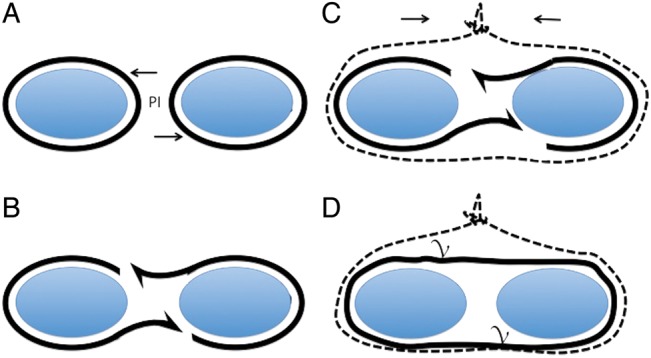
Coronal view of the sternal halves. (A) Asymmetric perichondrium incision (PI), (B) the two elevated flaps are gently elevated, (C) braided non-absorbable interrupted sutures (dotted line) approximate the sternal bars and (D) Each perichondrium flap is sutured to the opposite one (v).
DISCUSSION
In 1740, the first SC case report was published. Lannelong described, in 1888, the first SC surgical correction. Two successful cases were reported by Burton in 1847. No specific cause of SC has been found. It is probably a multifactorial pathology. Recent studies link SC to a genetic defect concerning the Hoxb gene [2]. Most series are small and most cases are sporadic.
This congenital chest wall abnormality is rare, and prenatal diagnoses can miss it. SC can be associated with other malformations, cardiac defects being the most frequent [2]. They must be ruled out before concluding on an isolated SC. Prognosis is favourable in case of isolated SC but can be poor when associated with syndromes like in Cantrell's pentalogy [2] (Omphalocele, Anterior diaphragmatic hernia, Ectopia cordis, Intracardiac defects and SC).
SC causes paradoxical respiratory movements and surgical correction is therefore recommended. It should be done early in the neonatal period. The thoracic wall has a higher compliance at this age, making primary closure easier. We believe that surgical treatment should be done at 1 month of age when other associated defects have been ruled out by physical examination, cardiological evaluation and radiological imaging (thoracic CT-scan).
Many techniques have been described. All have given satisfying results. We think that midline sternal osteotomy is necessary to minimize the tension when approximating the two sternal bars and prevents the need for sliding osteochondroplasty [4]. No comparative study has been made and no treatment was proven to be superior. Direct closure is the easiest technique. Nevertheless, it can be impossible when the SC is too wide or associated with other thoracic conditions like pectus excavatum. In the long-term, it can lead to a mild degree of pectus excavatum too [5]. The use of prosthesis or bone graft is a good alternative to this technique for difficult cases. The surgeon has to find the most suitable repair for each case.
In conclusion, we propose a simple surgical SC repair technique suitable for most cases. In comparison with previous techniques [1], it offers the theoretical advantage of restoring the anatomy with the two perichondrium layers. When performed in the neonatal period, it permits direct closure with satisfactory cosmetic results.
Conflict of interest: none declared.
REFERENCES
- 1.Salley RK, Stewart S. Superior sternal cleft: repair in the newborn. Ann Thorac Surg. 1985;39:582–3. doi: 10.1016/s0003-4975(10)62007-3. [DOI] [PubMed] [Google Scholar]
- 2.Torre M, Rapuzzi G, Carlucci M, Pio L, Jasonni V. Phenotypic spectrum and management of sternal cleft: literature review and presentation of a new series. Eur J Cardiothorac Surg. 2012;41:4–9. doi: 10.1016/j.ejcts.2011.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yavuzer S, Kara M. Primary repair of a sternal cleft in an infant with autogenous tissues. Interact CardioVasc Thorac Surg. 2003;2:541–3. doi: 10.1016/S1569-9293(03)00127-0. [DOI] [PubMed] [Google Scholar]
- 4.Muthialu N. Primary repair of sternal cleft in infancy using combined periosteal flap and sliding osteochondroplasty. Interact CardioVasc Thorac Surg. 2013;20:1–3. doi: 10.1093/icvts/ivt060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Acastello E, Majluf R, Garrido P, Barbosa LM, Peredo A. Sternal cleft: a surgical opportunity. J Pediatr Surg. 2003;38:178–83. doi: 10.1053/jpsu.2003.50038. [DOI] [PubMed] [Google Scholar]


