Abstract
We report a very rare case of malignant invasive thymoma with intraluminal growth through the thymic veins into the superior vena cava (SVC), with intracardiac right atrium extension. A 44-year old female with SVC syndrome underwent a radical thymectomy with pericardiectomy and complete removal of the endovascular and endocardiac neoplastic thrombus by a longitudinal incision starting from the atrium and extending along the SVC. The left anonymous vein was sacrificed, and the SVC and atrium were repaired with a continuous 5-0 Prolene suture. The hospital stay was uneventful. Postoperatively, the patient received adjuvant chemoradiotherapy (three cycles of cisplatin, doxorubicin and cyclophosphamide and subsequent mediastinal irradiation with 50 Gy). Nine months after surgery, no recurrences were seen and the patient is still well. This thymoma presentation with intravascular growth without direct vascular wall infiltration, although very rare, is possible and the management may be challenging. In our case, a primary radical operation was considered mandatory due to the clinical symptoms and the risk of neoplastic embolization. The collection of other similar cases could better clarify the role of adjuvant therapy.
Keywords: Thymoma, Superior vena cava syndrome, Neoplastic intravascular thrombus
INTRODUCTION
Invasive thymoma is characterized by infiltration and extension into the neighbouring structures [left anonymous vein, superior vena cava (SVC), pericardium, pleura and lung]. Invasive thymoma may cause SCV syndrome by direct infiltration or extrinsic compression; however, in very rare cases, an intraluminal extension of the tumour with thrombus formation into the SVC system and right atrium with polypoid growth has been described [1–4]. In case of intraluminal permeation by thymoma causing the SVC syndrome, induction therapy is often not possible or high risk, and the surgical removal of the neoplastic tissue with a complete resolution of symptoms and potential radical resection represents the only available option as rescue treatment.
CASE REPORT
A 44-year old female presented at our surgical department with facial and left upper limb oedema. A chest computed tomography (CT) scan showed a complete thrombosis of the left anonymous vein and SVC extending into the right atrium and an anterior mediastinal mass 5 × 2 cm in diameter apparently not infiltrating the vessels (Fig. 1A). [18F]-fluorodeoxyglucose positron emission tomography (PET)/CT scan demonstrated a pathological uptake in the thymic region and in the intraluminal mass, with maximum standardized uptake values (SUVmax) of 4.8 and 12.4, respectively (Fig. 1B). A cardiac ultrasound demonstrated a hyperechogenic lesion extending into the right atrium and a mass anterior to the aorta not determining compression.
Figure 1:
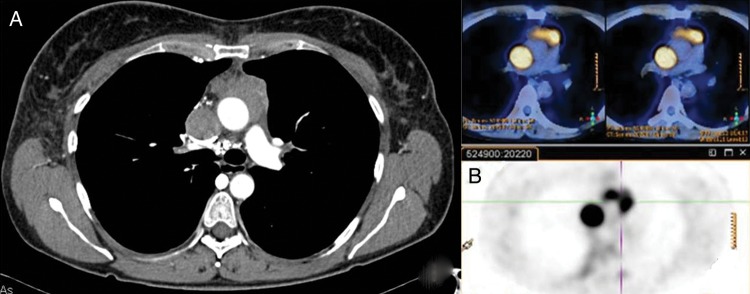
(A) Chest CT scan shows superior vena cava (SVC) thrombosis until the right atrium and a separate anterior mediastinal mass. (B) PET/CT scan shows two different pathological uptake values in the thymic region anteriorly to the ascendant aorta and in the SVC.
A multidisciplinary discussion was made: an induction treatment was considered high risk due to the SVC syndrome and the intracardiac and intravascular tumour that could cause neoplastic embolization: for that reason, the direct surgical approach was considered the only available rescue option. Through a median sternotomy, it was noticed that the thymoma had invaded the pericardium and partially, the left anonymous vein at the junction of the thymic veins. We performed a radical thymectomy with pericardiectomy with 2 cm of safe margins. At that point, a cardiopulmonary bypass on the beating heart, placing cannulas in the inferior vena cava and in the aorta, was established. The neoplastic thrombus had occluded the left anonimuos vein, the SVC and part of the right atrium; a long longitudinal incision of the SVC through the atrium was made, the left anonymous vein was scarified and sutured at the confluence into the SVC and the endovascular thrombus non-infiltrating the SVC and the heart was completely removed (Fig. 2). Both the SVC and atrium were repaired with a continuous 5-0 prolene suture (Ethicon, Inc., Somerville, NJ, USA). Pathological examination revealed a B3 thymoma with infiltration of thymic veins, mediastinal perithymic fat and pericardium with free margins and the neoplastic thrombus.
Figure 2:
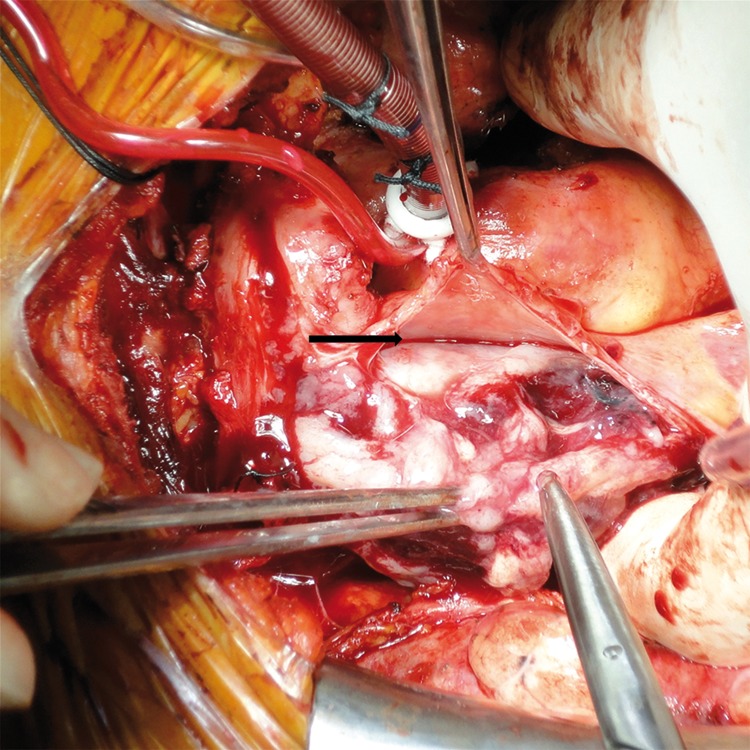
Intraoperative view of an opened superior vena cava with the neoplastic thrombus inside. The black arrow shows the border between the thrombus and the healthy endothelium.
The hospital stay was uneventful, and the patient was discharged on the seventh postoperative day without symptoms. Adjuvant chemoradiotherapy was administered 1 month after surgery (three cycles of cisplatin, doxorubicin and cyclophosphamide followed by mediastinal irradiation with 50 Gy). At 9 months of postoperative follow-up, the patient is well with no signs of local or distant relapse.
DISCUSSION
We described the case of a thymoma infiltrating the thymic veins with a neoplastic intracaval and intracardiac thrombus.
The patient underwent the surgical procedure without any preoperative histological diagnosis or induction treatment because of the risk of neoplastic detachment from the vascular wall of the SVC or right atrium and subsequent pulmonary embolism; in addition, the symptomatic SVC syndrome required a rapid intervention. The preoperative PET/CT scan was useful for two reasons, demonstrating the absence of distant metastases and the presence of two different uptake values [5]. We believe that a higher SUVmax in the neoplastic thrombus could be related to a higher concentration of epithelial tumour cells in endovascular metastasis than in the thymus where different cellular components were present. Nevertheless, this is the first case reported with a PET/CT scan study, and more reports are necessary to achieve conclusions. Moreover, this case indicates that, in the rare event of intravascular thymoma growth, a conservative radical operation in the main vessels and heart is possible and achieves good outcome. In our case, a radical excision was possible without the removal of the SVC also, as shown by other authors [2, 4], and avoiding the use of vascular reconstruction with a graft [1, 3]. Cardiopulmonary bypass with beating heart was useful to allow the opening of the SCV and atrium, the removal of the intravascular neoplastic tissue and then to obtain a radical resection.
The root of intravascular invasion of the neoplasm in our case was recognized in thymic veins. We agree with Terada et al. [2], who suggest that the examination of thymic veins is mandatory in routine thymectomy to obtain the highest grade of success of radical surgery.
After a multidisciplinary team discussion, we considered the patient to be affected by an advanced invasive thymoma, and we planned adjuvant chemoradiotherapy. However, the role of adjuvant therapy is still controversial and needs to be supported by the collection of other similar cases. In conclusion, this rare type of vessel invasion with intracaval growth into the right atrium may be considered potentially surgically resectable with a conservative and radical surgery that can achieve a good prognosis if managed in a multidisciplinary group.
Conflict of interest: none declared.
ACKNOWLEDGEMENTS
We are grateful to the interdisciplinary team of Thoracic Oncology of Humanitas Gavazzeni Hospital.
REFERENCES
- 1.Yamazaki K, Takeo S, Takeshita M, Sugimachi K. Thymic carcinoma presenting as an intraluminal growth into the great vessels and the cardiac cavity. Ann Thorac Cardiovasc Surg. 2002;8:163–6. [PubMed] [Google Scholar]
- 2.Terada Y, Ono N, Noguchi T, Kamakari K, Kitano M. A case of thymoma protruding into the superior vena cava through the thymic vein. Ann Thorac Surg. 2004;77:1088–90. doi: 10.1016/S0003-4975(03)01172-X. [DOI] [PubMed] [Google Scholar]
- 3.Ichimura H, Usui S, Okazaki H, Konishi T, Osaka M, Jikuya T, et al. Excision after chemoradiotherapy of invasive thymoma extending into the right atrium: report of a case. Surg Today. 2006;36:534–7. doi: 10.1007/s00595-006-3188-7. [DOI] [PubMed] [Google Scholar]
- 4.Li W, Chen X, Lv X, Guo X, Yang Y, Ni Y, et al. Resection of an invasive thymoma extending into the superior vena cava and right atrium. J Card Surg. 2010;25:515–7. doi: 10.1111/j.1540-8191.2010.01036.x. [DOI] [PubMed] [Google Scholar]
- 5.Terzi A, Bertolaccini L, Rizzardi G, Luzzi L, Bianchi A, Campione A, et al. Usefulness of 18-F FDG PET/CT in the pre-treatment evaluation of thymic epithelial neoplasms. Lung Cancer. 2011;74:239–43. doi: 10.1016/j.lungcan.2011.02.018. [DOI] [PubMed] [Google Scholar]


