SYNOPSIS
Objective
This study seeks to extend the investigation of parenting as an explanatory mechanism for relations between parental depressive symptoms and adolescent adjustment in the context of a four-wave longitudinal study.
Design
Participants were cohabiting parents and their 320 children (156 boys, 164 girls). Parental depressive symptoms were assessed in kindergarten (T1), parental negative responses to children’s emotional distress in first grade (T2), children’s representations of attachment with parents in second grade (T3), and adolescent adjustment in seventh grade (T4).
Results
Multiple pathways were identified in predicting adolescent conduct problems, including links involving (1) mothers’ depressive symptoms, mothers’ negative responses to children’s distress and insecure father-child attachment representations; (2) fathers’ depressive symptoms and insecure father-child attachment representations; and (3) fathers’ depressive symptoms and negative responses to children’s distress. A pathway was also found among mothers’ depressive symptoms, mothers’ negative responses to children’s distress, insecure mother-child attachment representations, and peer problems in adolescence.
Conclusion
The findings support a role of parents’ negative responses to children’s distress and representations of father-child and mother-child attachment in relations between children’s early experience with parental depressive symptoms and socioemotional outcomes in early adolescence.
Keywords: Parental Depression, Conduct Disorder, Attachment, Parenting, Peer Relationships
INTRODUCTION
Children of depressed parents are two to five times more likely to develop disorders than children of non-depressed parents, including multiple forms of psychological dysfunction (Owens & Shaw, 2003; Weissman, Warner, Wickramaratne, Moreau, & Olfson, 1997). Subclinical as well as clinical levels of parental depressive symptoms have been related to problems in family functioning and children’s adjustment (Farmer, McGuffin, & Williams, 2002; Lim, Wood, Miller & Simmens, 2011). Even after accounting for genetic factors, family environments have been related to the impact of both fathers’ and mothers’ depression on child adjustment (Lewis, Rice, Harold, & Thapar, 2011; Silberg, Maes, & Eaves, 2010).
Moreover, substantial evidence documents relations among parental depression, multiple dimensions of parenting, and child adjustment (e.g., Goodman & Gotlib, 1999; Hammen, 2009; Lim et al., 2011). In their review and framework for the familial influences of parental depression on child adjustment, Cummings, Campbell, and Davies (2000) hypothesized that parents’ negative responsiveness to children’s distress and parent-child attachment (e.g., Lyons-Ruth, Lyubchik, Wolfe, & Bronfman, 2002; Martins & Gaffan, 2000) contribute to relations between parental depression and child adjustment. Longitudinal investigation of the associations of these specific dimensions of parenting in associations between parental depressive symptoms and child adjustment problems holds promise to further explicate etiological processes (Dix & Meunier, 2009; Restifo & Bögels, 2009). The present study examines parental responses to children’s distress (Eisenberg, Cumberland, & Spinrad, 1998) and children’s representations of parent-child attachment relationships (Bretherton, 1985) in relations between fathers’ and mothers’ depressive symptoms and children’s conduct and peer problems between kindergarten and early adolescence.
Parent’s Negative Reactions to Children’s Emotions
Parental depressive symptoms have been linked with parents’ negative reactions to children’s emotions (Conger, Patterson & Ge, 1995; Harnish, Dodge, & Valente, 1995; Lovejoy, Graczyk, O’Hare, & Neuman, 2000). Relatedly, there are bases for expecting depressed parents to be less appropriately responsive when interacting with their children, including greater negative responsivity to children’s signals of distress (e.g., Campbell, Cohn, & Meyers, 1995). Moreover, parental psychological insensitivity and negative reactivity have been associated with insecure parent-child attachment (De Wolff & van IJzendoorn, 1997). Accordingly, we expected that parental negative responsiveness to children’s distress associated with parental depressive symptoms would be linked with children’s representations of insecure parent-child attachment as well as risk for adjustment problems.
Children’s Representations of Parent-Child Attachment Security
Parental depressive symptoms have also been associated with representations of parent-child attachment insecurity over time (Cummings, Schermerhorn, Keller, & Davies, 2008). Attachment security is identified as a mechanism relating to children’s adjustment over time (DeKlyen & Greenberg, 2008). The present study examines children’s representations of the parent as a secure base, which is articulated by Bowlby (1969) in terms of the construct of internal working models. Representations of the security of parent-child attachment, that is internal working models, have long been hypothesized to be a significant mechanism associated with attachment security (Bretherton, 1985). Children are posited to develop differentiated internal working models of relationships with mothers and fathers (Bretherton & Munholland, 2008). Despite the interest in this conceptualization, however, representations of attachment relationships have rarely been measured or evaluated systematically. A unique contribution of the present study is to examine children’s representations of attachment in the context of parental depressive symptoms and parenting (Cummings, Schermerhorn, Keller, & Davies, 2008).
Representations of parent-child attachment reflect children’s beliefs about other individuals’ likely behavior, based on prior experiences (Bretherton, 1985). Representations are more proximal to children’s psychological development than external events, thereby providing a window into processes that may underlie continuity in development (Grych, Wachsmuth-Schlaefer, & Klockow, 2002; Shamir, DuRocher Schudlich, & Cummings, 2001). The cognitive and emotional contents of internal working models of the self and others associated with insecure attachment (Oppenheim, Emde, & Warren, 1997; Oppenheim, Nir, Warren, & Emde, 1997) bear some similarities in some respects to the emotional and cognitive patterns characteristic of internalizing problems, such as depression. For example, a sense of loss and rejection, and negative self-concepts, are linked with both insecure parent-child attachment and depression (Cummings & Cicchetti, 1990). Insecure representations may lead to chronic stress and pervasive worries about the responsivity and reliability of family relationships, and motivate maladaptive behavioral responses for dealing with stress that generalize to multiple social settings (e.g., conduct problems, peer relationships; Cassidy, Kirsh, Scolton, & Parke, 1996).
Notably, the quality of the attachment relationship is hypothesized to indicate more than the quality of current parent-child interactions, but a lasting emotional bond between children and parents (Colin, 1996). The security of attachment relationships reflects a level of analysis of the parent-child relationship beyond simply the current quality or warmth of that relationship, and therefore might be expected to relate to adjustment outcomes above and beyond relations with parental warmth (Cummings et al., 2000). Given established close associations between parental warmth and attachment, it is important to account for parental warmth in analyses to better test whether attachment security per se relates to child outcomes. Warmth was assessed in this study to allow us to sharpen conclusions about the role of representations of parent-child attachment security in relation to adjustment outcomes. That is, by including warmth in model testing, findings can be interpreted to reflect the influence of security of parent-child attachment rather than simply representations of positive behaviors (i.e., warmth).
Father’s and Mother’s Depressive Symptoms
Although recent work supports the impact of fathers’ depressive symptoms on child adjustment (Ramchandani et al., 2008; Shelton & Harold, 2008), linkages between fathers’ depressive symptoms and child psychopathology continue to receive less study than associations between mothers’ depression and child psychopathology (Brennan, Hammen, Katz, & Brocque, 2002). Meta-analyses underscore that the familial effects of fathers’ depression may include negative effects on parenting and father-child relationships (Kane & Garber, 2004), with effect sizes for relations between fathers’ depressive symptoms and fathers’ parenting comparable to those for mothers (Wilson & Durbin, 2010). Research examining the depressive symptoms of both mothers and fathers in the same model tests offers the possibility for more comprehensive explanatory models for understanding the influence of parental depressive symptoms on child adjustment.
Children’s relationships with mothers and fathers may be associated with different pathways of child adjustment (Liu, 2008). For example, Lim et al. (2011) reported that fathers’ and mothers’ depressive symptoms related to child adjustment by different pathways of intervening mechanisms. That is, mothers’ depressive symptoms contributed to negative parenting and thereby internalizing symptoms and child asthma difficulties, whereas fathers’ depressive symptoms were related to child outcomes through a more complex pattern of family factors, including interparental conflict. Moreover, Paquette (2004) posited differences in associations between attachment and adjustment, with mother-child attachment influencing children’s functioning in peer relationships and father-child attachment likely affecting obedience and competence.
Hypotheses about Pathways
The current study uniquely examines several hypotheses regarding pathways among parental depressive symptoms, parenting processes, and adolescent externalizing problem behaviors. Specifically, parental depressive symptoms in kindergarten (T1) are expected to be prospectively related to each parent’s negative responses to child distress (T2) and children’s representations of insecure mother- and father-child attachment (T3). Second, parent’s negative responsiveness (T2) is hypothesized to be related to insecure representations of attachments (T3) and directly linked with adolescent adjustment problems (T4), even when accounting for each parent’s warmth as a possible mechanism (T3). Third, children’s insecure representations of mother- and father-child attachment relationships (T3) are predicted to be associated with adolescent conduct problems and problems with peers (T4), even when allowing for each parent’s warmth as a possible separate mechanism (T3). Given the relative lack of prospective tests, the comparison of mothers and fathers is exploratory. To better specify the role of intervening mechanisms, we further tested the primary SEM mediational model by comparing results with alternative models, including (1) tests of direct effects only of parental depression, negative parental responsiveness, and attachment representations, that is without mediation/indirect effects, and (2) tests of direct effects and parent-specific pathways only, that is without cross-parent mediation pathways (e.g., mothers’ effects on father processes and vice versa). The primary mediational model specified above is expected to fit the data significantly better than the alternative models.
METHOD
Participants
Participants included 321 families taking part in a larger, dual-site longitudinal study consisting of two cohorts of families. Families participated when children were in kindergarten (M age = 6.00, SD = .45), first (M age = 6.97, SD = .50), second (M age = 8.00, SD = .53), and seventh (M age = 13.10, SD = .54) grades. The first cohort of families (n = 235; 106 boys, 129 girls; T1 M age = 6.00, SD = .48) were eligible to participate if they had a child in kindergarten, all three family members had been cohabitating for a minimum of 3 years, and all members were English proficient. A second cohort of families (n = 85; 50 boys, 35 girls; T4 M age = 12.77, SD = .53) was recruited during a second phase of the longitudinal study when the first cohort of children was in seventh grade with eligibility criteria to match the original sample. Eligibility criteria for the second cohort of families required that all three family members were cohabitating for a minimum of 1 year, had a child in the seventh grade, and were English proficient. Families from both cohorts were recruited from communities in the Midwest and Northeast U. S. through flyers distributed to local schools, churches, community events, and neighborhoods. Families participated in two visits during each time point to reduce the length of time spent in each session; each session lasted approximately 2.5 hr. Informed consent or assent was obtained for all participants at the beginning of each session.
Data for the present study were from the kindergarten, first, second, and seventh grade time points. Data for all recruited families were included in the present analyses, that is data from any and all family members were retained for any time points that families participated. Structural equation modeling analyses were conducted using Analysis of Moment Structures (AMOS, v. 16.0.1; Arbuckle, 2007). AMOS utilizes a full information maximum likelihood (FIML) approach to estimating missing data, which computes the likelihood function for each case incorporating all of the available data (Bollen & Curran, 2006), which is an effective approach for dealing with missing data in structural equation models (Enders & Bandalos, 2001).
The second cohort of families did not differ from families recruited during kindergarten on most key demographics including ethnicity, relationship to the child, family income, and marital status at T4. However, fathers and mothers in the second cohort (M age = 42.21, SD = 7.97; M age = 40.46, SD = 6.30, respectively) were younger compared to parents of the first cohort of families (M age = 44.34, SD = 5.93, F(1,252) = 5.73, p < .05; M age = 42.73, SD = 5.99, F(1,276) = 5.64, p < .05, respectively). Children in the second cohort (M age = 12.77, SD = .53) were older than the longitudinal children (M age = 12.55, SD = .56), F(1,257) = 8.97, p < .01. The second cohort of families did not differ from the first cohort of families on the adolescent adjustment variables included in the current study.
Of the families recruited during kindergarten, 81.5% were retained during adolescence (T4). Retained families did not differ from families lost to attrition on parental depressive symptoms, child internalizing and externalizing problems, children’s representations of parent-child attachment or parental warmth, family income, marital status, relationship to child, and most parental responsiveness variables at the start of the study. Families lost to attrition at T4 had mothers with higher levels of punitive (M = 2.45, SD = .97) and minimizing responses (M = 2.82, SD = 1.00) to children’s distress compared to families retained at T4 (M = 2.18, SD = .64, F(1,229) = 6.02, p < .05; M = 2.51, SD = .79, F(1,229) = 4.43, p < .05, respectively). Additionally, fathers of non-retained families had higher levels of minimizing responses (M = 3.45, SD = 1.19) compared to retained families (M = 2.99, SD = .87), F(1,222) = 7.69, p < .01. However, comparisons of the families not retained at T2, when parenting variables in the current analyses are utilized, showed no differences in these variables among retained and non-retained families.
Families were representative of the demographics of the communities in which they were drawn. Of participants, 72.8% were European American, 17.3% were African American, 4.0% were Latin American, and 5.8% reported other racial and ethnic backgrounds. Most couples were married at recruitment (88.2%) and were the biological parent of the participating child (93.1% mothers, 83.5% fathers). During the adolescent assessment, 84.9% of couples were married. At T1, mothers’ reported median family annual income ranged between $40,000–54,999 (n = 63) and at T4 ranged between $55,000–74,999 (n = 60).
Measures
Parental depressive symptoms
Mothers and fathers completed the Center for Epidemiological Studies Depression scale at T1 of the study (CES-D; Radloff, 1977). The CES-D is a 20-item measure assessing depressive symptomotology in the past week. The CES-D has good discriminant validity and moderate test-retest reliability (Radloff, 1977). Good internal reliability was found for the current sample for mothers (α = .87) and fathers (α = .86). Scores of 16 or higher met criteria for clinical levels of depression; 16.7% of mothers and 13.7% of fathers scored in this range at T1. Of the families with depressive symptoms meeting clinical criteria at T1, 48.7% (n = 19) of mothers and 43.8% (n = 14) of fathers met these criteria again at subsequent time points. Across the longitudinal study, 30.9% of mothers and 32.7% of fathers reported scores meeting clinical criteria on at least one occasion. However, fewer than 5% of parents reported levels of depression that met criteria for clinical depression across all time points of the study. The average correlation between consecutive time points of depressive symptoms was .41 for mothers and .52 for fathers, ps < .01. Thus, although depressive symptomatology was relatively stable across waves of the study and criteria for clinical depression were met at least once among a substantial minority of parents over the course of the study, chronic levels of clinical depression that spanned the entire study were uncommon.
Parental negative responsiveness to child distress
At T2 mothers and fathers each completed the Coping with Children’s Negative Emotions Scale (CCNES; Fabes, Eisenberg, & Bernzweig, 1990). Parents were presented with 12 vignettes in which children expressed negative emotion. They were asked to respond to 6 items for each vignette, reflecting qualitatively distinct responses to children’s emotion. Three of these responses represented negative, that is non-supportive, ways of responding: (1) reacted punitively toward the child, (2) minimized the seriousness of the child’s distress or devalued the child’s problem, or (3) experienced their own distress. Scores were averaged across the vignettes. The CCNES has strong internal reliability, test-retest reliability, and construct validity (Fabes, Poulin, Eisenberg, & Madden-Derdich, 2002). For this sample: punitive reactions: mother α = .71, father α = .82; distressing reactions: mother α = .64, father α = .70; minimizing reactions: mother α = .79, father α = .86. Latent variables were created for mothers’ and fathers’ negative parenting, respectively, each with the three manifest indicators (i.e., punitive, minimizing, distressed reactions).
Children’s attachment representations of parent-child relationships
At T3 children’s internal representations of parent-child relationships (i.e., mother-child and father-child) were assessed by a revised version of the MacArthur Story Stem Battery (MSSB-R; Cummings et al., 2008), a narrative story-telling procedure. Consistent with the original procedures (MSSB; Bretherton et al., 1990), the experimenter presented story stems describing various situations designed to elicit stress and threaten the target relationship. Two stories were used to assess children’s attachment representations, one for each parent. Using toy props and action figures of family members, children were prompted to complete the story. Action figures were chosen to correspond to the child’s ethnicity and gender.
The assessments were videotaped and later coded by four trained research assistants using a manualized coding system (Davies & Winter, 2003). Stories were presented to assess children’s representations of mother-child attachment and father-child attachment, including separation and reunion themes. Coding included assessment of the relationship quality, caregiver competence, and story coherence in the attachment story. For relationship quality, the coder scored the child’s story on a scale from 1 (intense harmony) to 5 (intense discord). Harmony reflected a high degree of closeness, warmth, or support. Discord was indicated when difficulty in getting along was evident, including prolonged bouts of hostility. Caregiver competence assessed the portrayal of the caregiver as capable, prepared, and resourceful in the distressing situation regardless of the degree of difficulty with the attachment stress, rated on a scale from 1 (very competent) to 5 (very incompetent). Story coherence represents the degree to which the story made sense, flowed logically, and provided a meaningful end to the story. A story was coded as incoherent if it did not follow the story stem or contain internal logic or if the story was based on fantasy behavior (e.g. a giant T-rex comes on the scene and eats the mother, which is an actual example). A story was coded as coherent if it was logical, easily understood, and flowed from the story stem. The coder rated the child’s story on a scale ranging from 0 (incoherent) to 2 (coherent). Latent variables were created for children’s representations for the mother-child attachment relationship and for the father-child attachment relationship, respectively, each including three manifest indicators (i.e., relationship quality, caregiver competence, story coherence).
Children’s representations of warmth in parent-child relationships
Children’s representations of mothers’ and fathers’ warmth at T3 were also assessed by the MSSB-R. Children’s appraisals of parental warmth were coded during a story designed to elicit parental empathy in the context of child injury when disobeying. Separate stories similar in theme for mother and father were administered and coded for parental warmth. Ratings ranged from 0 (no warmth) to 3 (high warmth). A code of no warmth was scored if the parent did not display any evidence of parental warmth. A code of a little warmth (1) was given for one example of warm behavior (e.g. a single kiss or hug or warm tone of voice, putting a band-aid on child, or child sitting on parent’s lap). A code of some warmth (2) was giving for more than one example of warm behavior that was not as creative or sensitive as behaviors indicative of the high warmth code. A code of high warmth (3) was given for several examples of warm, loving, and supportive behavior, and an overall high level of genuine warmth.
Coder reliability was established on 20% of the videos. Intra-class correlations were acceptable for all MSSB-R variables: relationship quality: mother ICC = .92, father ICC = .95; caregiver competence: mother ICC = .90, father ICC = .92; story coherence: mother ICC = .78, father ICC = .82; parental warmth: mother ICC = .81, father ICC = .86.
Adolescent adjustment
Mothers and fathers completed the internalizing and externalizing problems subscales of the Child Behavior Checklist (CBCL; Achenbach, 1991) at T1. The internalizing problems subscale assessed children’s withdrawn, anxious, and depressive symptomatology (30 items), and the externalizing problems subscale assessed children’s aggressive and delinquent behaviors (33 items). For this sample, internal reliabilities were good for mothers and fathers (internalizing: α = .84, α = .88; externalizing: α = .88, α = .90, respectively). Parents’ reports were averaged and a parent-composite report for internalizing and externalizing problems was included as an auto-regressive control of child adjustment at T1 in the present study.
Adolescents completed the conduct problems and peer problems subscales of the Strengths and Difficulties Questionnaire at T4 (SDQ; Goodman, 1997) assessing their own symptomatology. The conduct problems subscale (5 items) reflected delinquent behaviors, and the peer problems scales (5 items) reflected difficulties with same age peers. Although relatively low internal consistencies for the scales of the SDQ have been reported (Palmieri & Smith, 2007), scale construction of the original SDQ was focused on creating scales to maximize clinical significance as well as statistical consistency, resulting typically in elevated predictive validity but at some cost of internal consistency of the SDQ scales. Consistent with the focus on optimizing predictive validity of the SDQ scales, Goodman and Scott (1999) reported the SDQ scales correlated more highly with interview-based ratings of clinical symptoms than the CBCL, and discriminated between high-risk and low-risk samples, further supporting criterion validity. Cronbach’s alphas in the current sample for conduct problems were .63 and for peer problems was .44; the low reliabilities of these scales are expected and are consistently found (Nunnally & Bernstein, 1994), especially for these the peer and conduct problems subscales (Bourdon et al., 2005; McCrory & Layte, 2012; Muris et al., 2003).
RESULTS
Means and standard deviations for all study variables can be seen in Table 1. Notably, parental depressive symptoms were positively correlated (r = .21, p < .05). A paired-samples t test was conducted to compare the level of depressive symptoms reported by fathers (M = 8.40; SD = 7.60) and mothers (M = 8.97; SD = 7.96), results did not indicate a significant difference in reported depressive symptoms, t (231) = −.88, ns. Parent report of children’s externalizing symptoms in kindergarten was significantly associated with higher levels of adolescents’ self-report of conduct problems (r = .31, p < .01) and peer problems (r = .26, p < .01) 7 years later. Moreover, manifest variables of children’s internal representations of the attachment relationships were significantly correlated; for representations of the mother-child attachment relationship, correlations ranged from .31 to .73 (ps < .01) and for representations of the father-child attachment relationship, correlations ranged from .42 to .76 (ps < .01). Analysis of variance indicated a gender difference in children’s externalizing symptoms in kindergarten, F(1,230) = 6.07, p < .05, with parents reporting higher symptoms for boys (M = 5.74; SD = 3.72) than girls (M = 4.65; SD = 3.04). Based on the gender difference in externalizing symptoms, child gender was controlled for in all analyses. Notably, given the complexity and size of the current model, separate models more explicitly testing gender differences were not examined in the present study.
TABLE 1.
Descriptive Statistics and Correlations
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Maternal Depression | – | |||||||||||||||||||
| 2. Paternal Depression | .21** | – | ||||||||||||||||||
| 3. Punitive Responses – M | .09 | .01 | – | |||||||||||||||||
| 4. Punitive Responses – F | .08 | .24** | .22** | – | ||||||||||||||||
| 5. Distressed Responses – M | .11 | −.03 | .43** | .13 | – | |||||||||||||||
| 6. Distressed Responses – F | .20** | 23** | .09 | .55** | .23** | – | ||||||||||||||
| 7. Minimizing Responses – M | .16* | .05 | .62** | .20** | .29** | .11 | – | |||||||||||||
| 8. Minimizing Responses – F | .10 | .17* | .22** | .71** | .05 | .39** | .28** | – | ||||||||||||
| 9. Maternal Warmth | −.12 | −.02 | −.04 | .07 | −.05 | .01 | .02 | .08 | – | |||||||||||
| 10. Paternal Warmth | .04 | .02 | −.12 | −.01 | −.15* | −.09 | −.10 | .07 | .35** | – | ||||||||||
| 11. Relationship Quality – M | .06 | .10 | −.01 | −.06 | .03 | .07 | .06 | −.03 | −.13 | −.15* | – | |||||||||
| 12. Relationship Quality – F | .18** | .25** | .09 | −.02 | .03 | .03 | .08 | .02 | −.15* | −.16* | .36** | – | ||||||||
| 13. Caregiver Competence – M | .07 | .08 | .13 | −.01 | .09 | .06 | .15* | −.03 | −.16* | −.20** | .73** | .36** | – | |||||||
| 14. Caregiver Competence – F | .15* | .13 | .11 | .03 | .01 | .06 | .16* | .01 | −.06 | −.13 | .29** | .76** | .50** | – | ||||||
| 15. Story Coherence – M | −.01 | .03 | −.04 | .05 | .01 | .02 | −.12 | .05 | .09 | .15* | −.31** | −.23** | −.34** | −.24** | – | |||||
| 16. Story Coherence – F | .06 | −.05 | −.15* | −.11 | −.07 | −.05 | −.08 | −.03 | .35** | .17* | −.21** | −.47** | −.25** | −.42** | .42** | – | ||||
| 17. C4 Conduct Problems | −.06 | .15* | .12 | .26** | .02 | .12 | .10 | .20** | .02 | −.05 | .03 | .17* | .11 | .18* | −.13 | −.19* | – | |||
| 18. C4 Peer Problems | −.06 | .10 | .03 | .12 | −.02 | .02 | .08 | .08 | .01 | .05 | .14 | .09 | .13 | .16* | −.17* | −.18* | .43** | – | ||
| 19. P1 Internalizing Problems | .19** | .23** | .17* | .23** | .24** | .32** | .09 | .23** | −.04 | −.01 | −.02 | .04 | −.03 | −.01 | .04 | .03 | .10 | .14 | – | |
| 20. P1 Externalizing Problems | .14* | .19** | .21** | .21** | .12 | .16* | .18** | .15* | −.08 | −.04 | −.06 | .13 | −.01 | .08 | −.08 | −.11 | .31** | .26** | .56** | – |
| M | 8.94 | 8.41 | 2.20 | 2.54 | 2.96 | 2.91 | 2.50 | 3.06 | .85 | .95 | 2.13 | 2.04 | 2.54 | 2.49 | 1.78 | 1.73 | 1.81 | 1.40 | 13.58 | 5.18 |
| SD | 7.96 | 7.57 | .66 | .85 | .68 | .73 | .80 | .94 | .65 | .82 | .86 | .96 | .93 | 1.02 | .46 | .49 | 1.78 | 1.49 | 10.67 | 3.41 |
| Minimum | 0.00 | 0.00 | 1.00 | 1.00 | 1.00 | 1.50 | 1.00 | 1.00 | .00 | .00 | 1.00 | 1.00 | 1.00 | 1.00 | .00 | .00 | .00 | .00 | .00 | .00 |
| Maximum | 41.00 | 38.00 | 4.42 | 6.50 | 4.67 | 4.92 | 5.25 | 6.58 | 3.00 | 3.00 | 5.00 | 5.00 | 5.00 | 5.00 | 2.00 | 2.00 | 9.00 | 7.00 | 57.00 | 23.25 |
Note. M = Mother; F = Father; for reasons of space where indicated, depression is shorthand for depressive symptoms, maternal parenting for maternal response to child emotion, and paternal parenting for paternal response to child emotion.
p < .05.
p < .01.
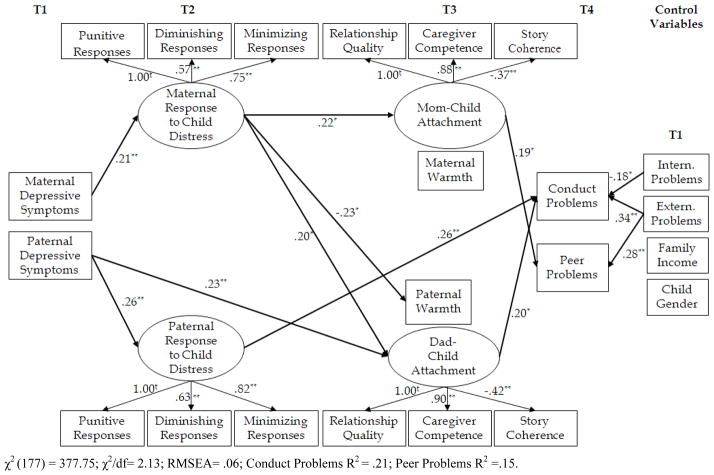
Structural equation modeling was used to examine associations among parents’ depressive symptoms at T1, parents’ negative responsiveness to child distress at T2, children’s internal representations of attachment and parental warmth at T3, and adolescents’ conduct and peer problems at T4. Table 2 displays the measurement model for the study. Latent variables of children’s representations of attachment relationships were created, one for attachment with mother, and one for attachment with father, given the availability of three measures of representations. Latent assessments of negative parenting were also created for mothers’ and fathers’ negative parenting. Manifest assessments of all other study variables were used. Criteria for evaluating model fit were based on the comparative fit index (CFI) approaching 1.0 (Bentler, 1990), a root mean square error of approximation (RMSEA) ≤ .08 (MacCallum, Browne, & Sugawara, 1996), and relative χ2 index (χ2/df) values < 3 (Arbuckle & Wothke, 1999). The model examined relations for mothers and fathers simultaneously (e.g., fathers’ depressive symptoms and mothers’ depressive symptoms were included as separate predictors in the same model). Child gender and family income were included as covariates on adolescent adjustment; reports of children’s internalizing and externalizing symptoms at T1 were included as autoregressive controls for a more stringent test of associations. Table 2 also displays structural components of the SEM model. This model had adequate fit for the data, χ2(177)= 377.75, χ2/df= 2.13, p <.05; RMSEA=.06, Conduct Problems R2 = .21, Peer Problems R2 = .15. Significant pathways in the model are discussed below (see Figure 1). Mothers’ and fathers’ depression were allowed to correlate in the model. Residual error variances of the latent variables were allowed to correlate within each time point across mothers and fathers (mothers’ and fathers’ negative parenting: r = .37, p < .01; mothers’ and fathers’ attachment representations: r = .46, p < .01; mothers’ and fathers’ warmth: r = .34, p < .01). Lastly, error variances of adolescent conduct and peer problems were allowed to correlate in the model (r = .36, p < .01).
TABLE 2.
Parameter Estimates for the Measurement and Structural Model in Figure 1
| Parameter Estimate | Unstandardized (SE) | Standardized β | p value |
|---|---|---|---|
| Measurement Model | |||
| Maternal Parenting → Punitive Responses | 1.00 | .67 | ---- |
| Maternal Parenting → Diminishing Responses | .77 (.11) | .57 | .00 |
| Maternal Parenting → Minimizing Responses | 1.28 (.14) | .75 | .00 |
| Paternal Parenting → Punitive Responses | 1.00 | .80 | ---- |
| Paternal Parenting → Diminishing Responses | .62 (.07) | .63 | .00 |
| Paternal Parenting → Minimizing Responses | 1.09 (.09) | .82 | .00 |
| Mom-Child Attachment → Relationship Quality | 1.00 | .86 | ---- |
| Mom-Child Attachment → Caregiver Competence | 1.12 (.07) | .88 | .00 |
| Mom-Child Attachment → Story Coherence | −.24 (.05) | −.37 | .00 |
| Dad-Child Attachment →Relationship Quality | 1.00 | .86 | ---- |
| Dad-Child Attachment → Caregiver Competence | 1.21 (.07) | .90 | .00 |
| Dad-Child Attachment → Story Coherence | −.28 (.05) | −.42 | .00 |
| Covariance of Maternal and Paternal Depression | 12.65 (4.07) | .21 | .00 |
| Covariance of Internalizing and Externalizing | 21.04 (2.78) | .58 | .00 |
| Structural Model | |||
| Maternal Depression → Maternal Parenting | .01 (.01) | .21 | .01 |
| Maternal Depression → Paternal Parenting | .01 (.01) | .09 | .21 |
| Maternal Depression → Mom-Child Attachment | .00 (.01) | .02 | .84 |
| Maternal Depression → Dad-Child Attachment | .01 (.01) | .10 | .19 |
| Maternal Depression → Maternal Warmth | −.01 (.01) | −.14 | .06 |
| Maternal Depression → Paternal Warmth | .00 (.01) | −.01 | .88 |
| Maternal Depression → Conduct Problems | −.03 (.02) | −.14 | .06 |
| Maternal Depression → Peer Problems | −.02 (.01) | −.11 | .13 |
| Paternal Depression → Maternal Parenting | .00 (.01) | −.02 | .79 |
| Paternal Depression → Paternal Parenting | .02 (.01) | .26 | .00 |
| Paternal Depression → Mom-Child Attachment | .01 (.01) | .13 | .09 |
| Paternal Depression → Dad-Child Attachment | .03 (.01) | .23 | .00 |
| Paternal Depression → Maternal Warmth | .00 (.01) | −.04 | .63 |
| Paternal Depression → Paternal Warmth | .00 (.01) | −.01 | .90 |
| Paternal Depression → Conduct Problems | .01 (.02) | .06 | .45 |
| Paternal Depression → Peer Problems | .01 (.02) | .03 | .70 |
| Maternal Parenting → Mom-Child Attachment | .34 (.16) | .22 | .03 |
| Maternal Parenting → Dad-Child Attachment | .34 (.17) | .20 | .04 |
| Maternal Parenting → Maternal Warmth | −.09 (.13) | −.06 | .49 |
| Maternal Parenting → Paternal Warmth | −.41 (.17) | −.23 | .02 |
| Maternal Parenting → Conduct Problems | .01 (.37) | .00 | .99 |
| Maternal Parenting → Peer Problems | .01 (.32) | .00 | .98 |
| Paternal Parenting → Mom-Child Attachment | −.18 (.10) | −.17 | .08 |
| Paternal Parenting → Dad-Child Attachment | −.20 (.11) | −.17 | .07 |
| Paternal Parenting → Maternal Warmth | .14 (.08) | .16 | .09 |
| Paternal Parenting → Paternal Warmth | .14 (.11) | .12 | .21 |
| Paternal Parenting → Conduct Problems | .65 (.24) | .26 | .01 |
| Paternal Parenting → Peer Problems | .05 (.20) | .02 | .82 |
| Mom-Child Attachment → Conduct Problems | .08 (.22) | .04 | .72 |
| Mom-Child Attachment → Peer Problems | .37 (.18) | .19 | .04 |
| Dad-Child Attachment → Conduct Problems | .44 (.20) | .20 | .03 |
| Dad-Child Attachment → Peer Problems | .11 (.17) | .06 | .53 |
| Maternal Warmth → Conduct Problems | .02 (.20) | .01 | .93 |
| Maternal Warmth → Peer Problems | .00 (.17) | .00 | .99 |
| Paternal Warmth → Conduct Problems | −.07 (.16) | −.03 | .67 |
| Paternal Warmth → Peer Problems | .25 (.14) | .14 | .06 |
| Externalizing Problems → Conduct Problems | .18 (.04) | .34 | .00 |
| Externalizing Problems → Peer Problems | .12 (.04) | .28 | .00 |
| Internalizing Problems → Conduct Problems | −.03 (.01) | −.18 | .03 |
| Internalizing Problems → Peer Problems | .00 (.01) | .00 | .99 |
| Child Age → Conduct Problems | .00 (.00) | .08 | .30 |
| Child Age → Peer Problems | .00 (.00) | −.04 | .61 |
| Child Gender → Conduct Problems | −.06 (.24) | −.02 | .80 |
| Child Gender → Peer Problems | .03 (.20) | .01 | .88 |
| Parenting Residual Covariance | .11 (.03) | .37 | .00 |
| Attachment Residual Covariance | .25 (.05) | .46 | .00 |
| Parental Warmth Residual Covariance | .18 (.04) | .34 | .00 |
| Adolescent Adjustment Residual Covariance | .75 (.15) | .36 | .00 |
Note. Bolded values indicate significant parameters. For reasons of space where indicated, depression is shorthand for depressive symptoms. In addition maternal parenting is shorthand for maternal response to child distress and paternal parenting is shorthand for paternal response to child distress.
Figure 1.
Model examining relations between parental depressive symptoms, negative responsiveness to child distress, children’s representations of attachment, and adolescent adjustment. Significant pathways depicted only. Standardized path coefficients are presented; f superscripts indicate fixed factor loadings for model estimation. Correlations not depicted in figure. *p <. 05. **p < .01.
The primary mediational model was compared to two alternative models. The proposed model fit the data better than an alternative model examining direct effects of parental depression, parenting, and parent-child representations on adolescent adjustment, χ2(197) = 426.78, χ2 difference = 49.03, Δdf = 20, p < .001. Additionally, the primary mediational model also fit the data better than a model examining parent-specific pathways (e.g., no cross-parent pathways; χ2(187)=396.14, χ2 difference = 18.39, Δdf = 10, p < .05). Given comparison of these alternative models, the primary mediational model examining consecutive pathways of parenting and internal parent-child representations for relations between parental depressive symptoms and adolescent adjustment fits the data well.
Mothers’ Depressive Symptoms
As shown in Figure 1, a pathway was identified across mothers’ depressive symptoms, mothers’ responsiveness to distress, children’s representations of mother-child attachment, and adolescent adjustment. Specifically, mothers’ depressive symptoms and mothers’ negative responsiveness to distress were significantly associated, and in turn, mothers’ use of negative responsiveness to emotional distress was associated with children’s insecure representations of both the mother-child attachment relationship and warmth in the father-child relationship. Subsequently, children’s representations of insecure mother-child attachment representations were associated with more adolescent peer problems. In terms of tests of mediation for the various mediational processes found, tests of the indirect effects were examined according to the procedures outlined in MacKinnon, Fritz, Williams, and Lockwood (2007). Specifically, there was (1) an indirect effect of mothers’ depression on mother-child attachment through mothers’ negative parenting (95% CI = .00004, .01), (2) a trend for the indirect effect of mothers’ negative parenting on adolescent peer problems through increased insecurity in the mother-child attachment relationship (90% CI = .01, .29), and (3) an indirect effect of mothers’ depression on fathers’ warmth through mothers’ parenting (95% CI = −.01, −.0003). Additionally, there was a significant pathway between mothers’ depressive symptoms, mothers’ responsiveness to distress, children’s representations of father-child attachment, and adolescent conduct problems. Mothers’ depressive symptoms were significantly associated with mothers’ increased negative responsiveness (β= .21, p < .01), and in turn mothers’ negative responsiveness to children’s emotional distress was associated with children’s insecure representations of father-child attachment. Children’s insecure representations of father-child attachment were associated with increased conduct problems during adolescence. Further tests revealed trends for the indirect effects (1) for mothers’ parenting as a mediator between mothers’ depression and father-child attachment (90% CI = .0003, .01) and (2) the indirect effect of mothers’ parenting on adolescent conduct problems through father-child attachment (90% CI = .01, .35).
Fathers’ Depressive Symptoms
Also as shown in Figure 1, multiple pathways were found through which fathers’ depressive symptoms influenced adolescent adjustment. Fathers’ depressive symptoms were significantly associated with fathers’ negative responsiveness to distress (β= .26, p < .01) and in turn adolescents’ conduct problems (β= .26, p < .01). In addition, fathers’ depressive symptoms were also associated with children’s negative representations of the father-child attachment relationship (β= .23, p <.01) which also significantly predicted adolescents’ conduct problems (β= .20, p < .05). Tests of the indirect effect supported both fathers’ negative responsiveness to distress (95% CI = .003, .03) and father-child attachment (95% CI = .001, .03) as mediators between fathers’ depression and adolescent conduct problems.
DISCUSSION
In the present study, longitudinal pathways were identified between parents’ depressive symptoms when children were in kindergarten and children’s socioemotional outcomes in early adolescence. Dimensions of parenting served as intervening variables for both mothers’ and fathers’ depressive symptoms. However, vulnerability to different socioemotional outcomes was indicated as a function of the gender of the parent. That is, when compared within the same model, different pathways were found between mothers’ and fathers’ depressive symptoms and child adjustment.
Both mothers’ and fathers’ depressive symptoms were associated with later conduct problems. Two pathways were identified for fathers in relation with adolescent conduct problems. Fathers’ depressive symptoms were related to fathers’ negative responsiveness to child distress and children’s representation of father-child attachments, respectively, with each of these dimensions of parenting related to children’s conduct problems. Fathers’ lack of responsiveness to child distress and insecure representations of father-child attachment may each reduce children’s motivation to comply with fathers’ disciplinary practices by undermining the quality of the father-child relationship, thereby lessening children’s tendency to comply with family rules and regulations, and increasing risk for conduct problems (Greenberg, Speltz, & Deklyen, 1993).
A pathway to adolescent conduct problems was identified for mothers that involved multiple intervening mechanisms. That is, mothers’ negative responses to children’s emotions were related to adolescent conduct problems as a function of insecure father-child attachment representations. These results further underscore the notion that the effects of relationships with fathers on child outcomes may be related to the broader family context (e.g., Lim et al., 2011). Although links reported between mothers’ depressive symptoms and externalizing problems were replicated (e.g., Allen, Manning & Meyer, 2010), the present results further underscore the possible significance of children’s representations of security in father-child attachment relationships to their eventual conduct problems.
Only mothers’ depressive symptoms were linked with later adolescent peer problems, consistent with cross-sectional relations reported in earlier work (Cummings et al., 2005). Vulnerability to peer problems reflected a complex pathway. That is, mothers’ depressive symptoms were associated with problems in responsiveness to children’s distress, which, over time, related to children’s insecure representations of the parent-child relationship (DeWolf & van IJzendoorn, 1997). In turn, representations of mother-child attachment insecurity were related to the quality of peer relationships in early adolescence. Children’s capacity for peer relationships may be undermined by the lack of emotional and psychological support for exploration and social successes associated with insecure mother-child attachment. Compared to fathers, mothers may be more closely involved in relational issues with children, including fostering or supporting daily relationships with peers (e.g., children’s extra-curricular activities), and therefore have more impact on children’s social functioning in extra-familial contexts (e.g., peer relationships).
Mothers’ depressive symptoms were related to children’s internal representations of both mother-child and father-child attachment through the mother’s negative parenting responsiveness to children’s distress congruent with notions that mothers’ attachment serves to alleviate children’s distress. These findings suggest the significance of mothers’ provision of security in times of stress to children’s relatively global internal working models of the security of attachment relationships in the family (Paquette, 2004). Thus, in situations where mothers respond in negative ways to children’s distress, these parenting behaviors may impact children’s representations of both mothers and fathers as caregivers.
Fathers’ depression was related independently to both fathers’ negative responses to child distress and father-child attachment representations, which each then linked to subsequent adolescent conduct problems. Fathers’ responsiveness to distress did not contribute to children’s internal representations, suggesting children’s representations of fathers as secure attachment figures may be less affected compared to mothers by the ability to respond effectively to the child’s distress. The fact that fathering was not related to adolescent peer problems may reflect lesser involvement by fathers than mothers in fostering or supporting day-to-day peer relationships.
The findings further advance the explanatory role of attachment processes in the context of parental depression (Lyons-Ruth et al., 2002), consistent with notions that (1) children’s internal representations of parent-child attachment may be linked with long-term pathways in the development of adjustment problems (Bretherton & Munholland, 2008), but (2) primarily occurring in the context of other risk factors (DeKlyen & Greenberg, 2008), in this instance, parental depressive symptoms and negative responsiveness to child distress (Lyons-Ruth, Easterbrooks, & Cibelli, 1997). Moreover, a specific role of children’s representations of parent-child attachment security is further supported by the fact that relations for mothers and fathers held even when each parent’s warmth was included in the model. A core proposition of attachment theory from its initial formulation is that children’s sense of emotional security in the parent-child relationship derives from positive parenting experiences. However, attachment is also posited as reflecting a persisting emotional bond that predicts children’s socioemotional outcomes above and beyond specific parenting behaviors. In this study relations with adjustment were found even when children’s representations of parental warmth were included in the model. Children’s representations of father-child and mother-child attachments may each be related to trajectories of risk for negative socioemotional outcomes in the context of parental depressive symptoms (Cowan, Cohn, Cowan, & Pearson, 1996).
Even longitudinal analyses do not fully establish causal pathways, and, in the present instance, autoregressive controls were limited to establishing that parental depressive symptoms were linked with changes in adjustment between kindergarten and early adolescence. The pathways identified in the present model tests may have been affected by unmeasured third variables, and associations between the variables outlined in the model tests cannot be assumed to be unidirectional. Although we found support for our theoretical model in relation to two alternative models, which lends support to the hypothesized intervening mechanisms, autocorrelations across time points for intervening variables were not included, which would have further strengthened interpretation of the role of intervening variables in changes over time. In addition, we examined depressive symptoms in a community sample, not diagnoses of major depression. Although the use of a community sample fosters the generalizability of results, findings may not be generalizable to clinical populations. In addition, alternative methods of assessments of these parenting dimensions may further explicate the impact of these dimensions of family functioning (e.g., observationally based assessments of parental responsiveness to child distress). The relatively low internal consistency of SDQ scales, especially for child-reported peer problems, is a limitation of the study, although consistent with other reports about alpha coefficients for this scale of the SDQ. Relatively low internal consistencies of the SDQ are reported elsewhere, and have been attributed to the aim to emphasize predictive validity over internal consistency in scale construction (Palmieri & Smith, 2007).
Despite these limitations, the results of this study offer intriguing information about the impact of parental depressive symptoms on child and adolescent development in families. Contributions are made about parental responses to children’s distress and parent-child attachment as explanatory mechanisms. In addition, differential effects of fathers’ and mothers’ depressive symptoms were identified. Moreover, cross system relations were found, that is mutual influences of mothers’ and fathers’ depressive symptoms on parents’ relationships with their children.
IMPLICATIONS FOR PRACTICE, APPLICATION, AND POLICY.
One implication is that practitioners may wish to target for change parental behaviors, specifically, parents’ negative responses to children’s emotions, that foster the development of children’s insecure internal representations of parent-child attachments. That is, parents should be encouraged to minimize responding negatively to children’s emotions, which therapists should appreciate may be especially likely when parents have depressive symptoms. In addition, parents should be made aware of the lasting significance for children’s risk for adjustment problems when children’s representations of their relationships with parents are insecure. Once formed, these models may resist change, so that care should be taken in encouraging parents to support children’s emotional security and patience may be required in efforts to ameliorate children’s insecurity. In the contexts of therapy, practitioners should be aware of the possible impact of fathers’ as well as mothers’ depressive symptoms on children’s adjustment and the possibly different implications for children’s adjustment.
Acknowledgments
This research was supported by a grant from the National Institutes of Mental Health (R01 MH57318) awarded to Patrick T. Davies and E. Mark Cummings. We are grateful to the children, parents, and teachers who participated in this project. We express our appreciation to project staff and students at the University of Notre Dame and the University of Rochester. We are grateful to Scott Maxwell for his generous statistical consultation.
Contributor Information
E. Mark Cummings, Email: cummings.10@nd.edu, Department of Psychology, University of Notre Dame, 204 Brownson Hall, Notre Dame, IN 46556, USA.
Melissa R.W. George, University of Notre Dame
Kalsea J. Koss, University of Notre Dame
Patrick T. Davies, University of Rochester
References
- Achenbach TM. Manual for the Child Behavior Checklist: 4–18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Allen JP, Manning N, Meyer J. Tightly linked systems: Reciprocal relations between maternal depressive symptoms and maternal reports of adolescent externalizing behavior. Journal of Abnormal Psychology. 2010;119:825–835. doi: 10.1037/a0021081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbuckle JL. Amos 16.0 user’s guide. Chicago, IL: SPSS; 2007. [Google Scholar]
- Arbuckle JL, Wothke W. Amos 4.0 user’s guide. Chicago, IL: SPSS; 1999. [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Curran PJ. Latent curve models: A structural equation approach. Hoboken, NJ: Wiley; 2006. [Google Scholar]
- Bourdon KH, Goodman R, Rae DS, Simpson G, Koretz DS. The Strengths and Difficulties Questionnaire: US normative data and psychometric properties. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:557–564. doi: 10.1097/01.chi.0000159157.57075.c8. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss. Vol. 1: Attachment. New York: Basic Books; 1969. [Google Scholar]
- Brennan PA, Hammen C, Katz AR, Le Brocque RM. Maternal depression, paternal psychopathology, and adolescent diagnostic outcomes. Journal of Consulting and Clinical Psychology. 2002;70:1075–1085. doi: 10.1037/0022-006X.70.5.1075. [DOI] [PubMed] [Google Scholar]
- Bretherton I. Attachment theory: Retrospect and prospect. Monographs of the Society for Research in Child Development. 1985;50:3–35. doi: 10.2307/3333824. [DOI] [Google Scholar]
- Bretherton I, Munholland KA. Internal working models in attachment relationships: Elaborating a central construct in attachment theory. In: Cassidy J, Shaver PR, editors. Handbook of attachment: Theory, research, and clinical applications. 2. New York: Guilford Press; 2008. pp. 102–127. [Google Scholar]
- Bretherton I, Oppenheim D, Prentiss C, Buschsbaum H, Emde R, Lundquist A, et al. The MacArthur Story Stem Battery. 1990 Unpublished Manuscript. [Google Scholar]
- Campbell SB, Cohn JF, Meyers T. Depression in first-time mothers: Mother-infant interaction and depression chronicity. Developmental Psychology. 1995;31:349–357. doi: 10.1037/0012-1649.31.3.349. [DOI] [Google Scholar]
- Cassidy J, Kirsh SJ, Scolton KL, Parke RD. Attachment and representations of peer relationships. Developmental Psychology. 1996;32:892–904. doi: 10.1037/0012-1649.32.5.892. [DOI] [Google Scholar]
- Colin VL. Human attachment. New York: McGraw-Hill; 1996. [Google Scholar]
- Conger RD, Patterson GR, Ge X. It takes two to replicate: A mediational model for the impact of parents’ stress on adolescent adjustment. Child Development. 1995;66:80–97. doi: 10.2307/1131192. [DOI] [PubMed] [Google Scholar]
- Cowan PA, Cohn DA, Cowan CP, Pearson JL. Parent’s attachment histories and children’s externalizing and internalizing behaviours: Exploring family systems models of linkage. Journal of Consulting and Clinical Psychology. 1996;64:53–63. doi: 10.1037/0022-006X.64.1.53. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Cicchetti D. Towards a transactional model of relations between attachment and depression. In: Greenberg M, Cicchetti D, Cummings EM, editors. Attachment in the preschool years: Theory, research, and intervention. Chicago: The University of Chicago Press; 1990. pp. 339–372. [Google Scholar]
- Cummings EM, Davies PT, Campbell SB. Developmental psychopathology and family processes: Theory, research, and clinical implications. New York: Guilford Press; 2000. [Google Scholar]
- Cummings EM, Keller PS, Davies PT. Towards a family process model of maternal and paternal depressive symptoms: Exploring multiple relations with child and family functioning. Journal of Child Psychology and Psychiatry. 2005;46:479–489. doi: 10.1111/j.1469-7610.2004.00368.x. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Schermerhorn AC, Keller PS, Davies PT. Parental depressive symptoms, children’s representations of family relationships, and child adjustment. Social Development. 2008;17:278–305. doi: 10.1111/j.1467-9507.2007.00425.x. [DOI] [Google Scholar]
- Davies PT, Winter MA. University of Rochester Story Stem Narrative Coding System. University of Rochester; 2003. Unpublished manuscript. [Google Scholar]
- DeKlyen M, Greenberg MT. Attachment and psychopathology in childhood. In: Cassidy J, Shaver PR, editors. Handbook of attachment: Theory, research, and clinical applications. 2. New York: Guilford Press; 2008. pp. 637–665. [Google Scholar]
- De Wolff M, van Ijzendoorn MH. Sensitivity and attachment: A meta-analysis on parental antecedents of infant attachment. Child Development. 1997;68:571–591. doi: 10.2307/1132107. [DOI] [PubMed] [Google Scholar]
- Dix T, Meunier LN. Depressive symptoms and parenting competence: An analysis of 13 regulatory processes. Developmental Review. 2009;29:45–68. doi: 10.1016/j.dr.2008.11.002. [DOI] [Google Scholar]
- Eisenberg N, Cumberland A, Spinrad TL. Parental socialization of emotion. Psychological Inquiry. 1998;9:241–273. doi: 10.1207/s15327965pli0904_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8:430–457. doi: 10.1207/S15328007SEM0803_5. [DOI] [PubMed] [Google Scholar]
- Fabes RA, Eisenberg N, Bernzweig J. The Coping with Children’s Negative Emotions Scale: Description and scoring. Department of Family Resources and Human Development, Arizona State University; 1990. Unpublished scale. [Google Scholar]
- Fabes RA, Poulin RE, Eisenberg N, Madden-Derdich DA. The Coping with Children’s Negative Emotions Scale (CCNES): Psychometric properties and relations with children’s emotional competence. Marriage & Family Review. 2002;34:285–310. doi: 10.1300/J002v34n03_05. [DOI] [Google Scholar]
- Farmer A, McGuffin P, Williams J. Measuring psychopathology. Oxford: Oxford University Press; 2002. [Google Scholar]
- Goodman R. The strengths and difficulties questionnaire: A research note. Journal of Child Psychology and Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295X.106.3.458. [DOI] [PubMed] [Google Scholar]
- Goodman R, Scott S. Comparing the Strengths and Difficulties Questionnaire and the Child Behavior Checklist: Is small beautiful? Journal of Abnormal Psychology. 1999;27:17–24. doi: 10.1023/A:1022658222914. [DOI] [PubMed] [Google Scholar]
- Greenberg MT, Speltz ML, DeKlyen M. The role of attachment in the early development of disruptive behavior problems. Development and Psychopathology Special Issue: Toward a developmental perspective on conduct disorder. 1993;5:191–213. doi: 10.1017/S095457940000434X. [DOI] [Google Scholar]
- Grych JH, Wachsmuth-Schlaefer T, Klockow LL. Interparental aggression and young children’s representations of family relationships. Journal of Family Psychology. 2002;16:259–272. doi: 10.1037/0893-3200.16.3.259. [DOI] [PubMed] [Google Scholar]
- Hammen C. Adolescent depression: Stressful interpersonal contexts and risk for recurrence. Current Directions in Psychological Science. 2009;18:200–204. doi: 10.1111/j.1467-8721.2009.01636.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harnish JD, Dodge KA, Valente E. Mother-child interaction quality as a partial mediator of the roles of maternal depressive symptomatology and socioeconomic status in the development of child behavior problems. Child Development. 1995;66:739–753. doi: 10.1111/j.1467-8624.1995.tb00902.x. [DOI] [PubMed] [Google Scholar]
- Kane P, Garber J. The relations among depression in fathers, children’s psychopathology, and father-child conflict: A meta-analysis. Clinical Psychology Review. 2004;24:339–360. doi: 10.1016/j.cpr.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Lewis G, Rice F, Harold GT, Collishaw S, Thapar A. Investigating environmental links between parent depression and child depressive/anxiety symptoms: Using an assisted conception design. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50:451–459. doi: 10.1016/j.jaac.2011.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim J, Wood BL, Miller BD, Simmens SJ. Effects of paternal and maternal depressive symptoms on child internalizing symptoms and asthma disease activity: Mediation by interparental negativity and parenting. Journal of Family Psychology. 2011;25:137–146. doi: 10.1037/a0022452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y. An examination of three models of the relationships between parental attachments and adolescents’ social functioning and depressive symptoms. Journal of Youth and Adolescence. 2008;37:941–952. doi: 10.1007/s10964-006-9147-1. [DOI] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/S0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Easterbrooks AM, Cibelli CD. Infant attachment strategies, infant mental lag, and maternal depressive symptoms: Predictors of internalizing and externalizing problems at age 7. Developmental Psychology. 1997;33:681–692. doi: 10.1037/0012-1649.33.4.681. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Lyubchik A, Wolfe R, Bronfman E. Parental depression and child attachment: Hostile and helpless profiles of parent and child behavior among families at risk. In: Goodman SH, Gotlib IH, editors. Children of depressed parents: Mechanisms of risk and implications for treatment. Washington, DC: American Psychological Association; 2002. pp. 89–120. [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1:130–149. doi: 10.1037/1082-989X.1.2.130. [DOI] [Google Scholar]
- MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: Program PRODCLIN. Behavior Research Methods. 2007;39:384–389. doi: 10.3758/BF03193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins C, Gaffan EA. Effects of early maternal depression on patterns of infant–mother attachment: A meta-analytic investigation. Journal of Child Psychology and Psychiatry. 2000;41:737–746. doi: 10.1111/1469-7610.00661. [DOI] [PubMed] [Google Scholar]
- McCrory C, Layte R. Testing competing models of the Strengths and Difficulties Questionnaire’s (SDQ’s) factor structure for the parent-informant instrument. Personality and Individual Differences. 2012;52:882–887. [Google Scholar]
- Muris P, Meesters C, van den Berg F. The Strengths and Difficulties Questionnaire (SDQ) – further evidence for its reliability and validity in a community sample of Dutch children and adolescents. European Child and Adolescent Psychiatry. 2003;12:1–8. doi: 10.1007/s00787-003-0298-2. [DOI] [PubMed] [Google Scholar]
- Nunnally JC, Bernstein IH. Psychometric theory. 3. New York: McGraw-Hill; 1994. [Google Scholar]
- Oppenheim D, Emde RN, Warren S. Children’s narrative representations of mothers: Their development and associations with child and mother adaptation. Child Development. 1997;68:127–138. doi: 10.2307/1131930. [DOI] [PubMed] [Google Scholar]
- Oppenheim D, Nir A, Warren S, Emde RN. Emotion regulation in mother–child narrative co-construction: Associations with children’s narratives and adaptation. Developmental Psychology. 1997;33:284–294. doi: 10.1037/0012-1649.33.2.284. [DOI] [PubMed] [Google Scholar]
- Owens E, Shaw DS. Predicting growth curves of externalizing behavior across the preschool years. Journal of Abnormal Child Psychology. 2003;31:575–590. doi: 10.1023/A:1026254005632. [DOI] [PubMed] [Google Scholar]
- Palmieri PA, Smith GC. Examining the structural validity of the Strengths and Difficulties Questionnaire (SDQ) in a U.S. sample of custodial grandmothers. Psychological Assessment. 2007;19:189–198. doi: 10.1037/1040-3590.19.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paquette D. Dichotomizing paternal and maternal functions as a means to better understand their primary contributions. Human Development. 2004;47:237–238. doi: 10.1159/000078726. [DOI] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Ramchandani PG, Stein A, O’Connor TG, Heron J, Murray L, Evans J. Depression in men in the postnatal period and later child psychopathology: A population cohort study. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:390–398. doi: 10.1097/CHI.0b013e31816429c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Restifo K, Bögels S. Family processes in the development of youth depression: Translating the evidence to treatment. Clinical Psychology Review. 2009;29:294–316. doi: 10.1016/j.cpr.2009.02.005. [DOI] [PubMed] [Google Scholar]
- Shamir H, DuRocher-Schudlich T, Cummings EM. Marital conflict, parenting styles, and children’s representations of family relationships. Parenting: Science and Practice. 2001;1:123–151. doi: 10.1207/S15327922PAR011&2_7. [DOI] [Google Scholar]
- Shelton KH, Harold GT. Interparental conflict, negative parenting, and children’s adjustment: Bridging links between parents’ depression and children’s psychological distress. Journal of Family Psychology. 2008;22:712–724. doi: 10.1037/a0013515. [DOI] [PubMed] [Google Scholar]
- Silberg JL, Maes H, Eaves LJ. Genetic and environmental influences on the transmission of parental depression to children’s depression and conduct disturbance: An extended children of twins study. Journal of Child Psychology and Psychiatry. 2010;51:734–744. doi: 10.1111/j.1469-7610.2010.02205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Warner V, Wickramaratne P, Moreau D, Olfson M. Offspring of depressed parents: 10 years later. Archives of General Psychiatry. 1997;54:932–940. doi: 10.1001/archpsyc.1997.01830220054009. Retrieved from http://search.proquest.com/docview/619195536?accountid=12874. [DOI] [PubMed] [Google Scholar]
- Wilson S, Durbin CE. Effects of paternal depression on fathers’ parenting behaviors: A meta-analytic review. Clinical Psychology Review. 2010;30:167–180. doi: 10.1016/j.cpr.2009.10.007. [DOI] [PubMed] [Google Scholar]