Abstract
Purpose
Posterior-only approach arthrodesis by all-pedicle screw instrumentation has a correction rate similar to correction obtained by traditional combined anterior/posterior approach surgery and avoids the complications associated with the thoracic approach.
Methods
We treated 25 patients, with a mean age 16.5 years, with severe adolescent idiopathic scoliosis by posterior-only approach using all-screw instrumentation arthrodesis. Mean scoliosis curve in Cobb degrees was 95° Cobb. All cases were treated by the same senior surgeon, by free hand technique, without intraoperative neurophysiologic monitoring and spine navigation aids.
Results
Mean scoliosis curve after surgery was 37° Cobb. Mean follow-up was 4 years. No perioperative complications, curve progression or arthrodesis malunion were reported at the follow-up.
Conclusions
Posterior spinal fusion with pedicle screw-only instrumentation obtains a good and stable correction of severe scoliosis; compared to hybrid instrumentation, it allows a greater coronal correction of the deformity and less correction loss at the follow-up.
Keywords: Adolescent idiopathic scoliosis, Posterior approach, All-pedicle screw instrumentation, Severe scoliosis
Introduction
In the past, the treatment of severe idiopathic scoliosis (Main curve over 80° Cobb) was performed by an anterior release with an open thoracotomy [1] followed by posterior instrumented fusion. Halo traction between anterior release and posterior instrumentation was sometimes applied. The correction rate of severe idiopathic curves with the combined treatment was 45–47 %, using Harrington instrumentation or the multiple hook construct [2]; a 52 % correction rate was recorded using Zielke instrumentation with Harrington rod, and this rose to as much as 67 %, using anterior instrumentation and posterior hybrid construct [1]. The combined anterior and posterior procedure was performed in one- or two-stage surgery by different authors with different outcomes. Shufflebarger et al. [2] found that a reduction in hospital stay and operating time led to fewer complications, and better correction in the continuous group compared with the staged one; more recently, Shen et al. [3] concluded that there was no significant difference in the safety or efficacy between the one- or two-stage groups. Additional anterior surgery requires increased time for the general anesthesia and may have a negative impact on pulmonary function. Kim et al. [4] recently reported that an open anterior approach may have a deleterious effect on pulmonary function for as long as 5 years after adolescent idiopathic scoliosis (AIS) surgery. Video-assisted thoracoscopy (VAT), used for the anterior release, followed by posterior instrumentation for scoliosis treatment [5, 6] can minimize, but not eliminate, the negative effect on the pulmonary function, as reported by Newton et al. [7].
Combined anterior and posterior vertebral column resection has been the most frequently used procedure [8] to treat severe and rigid scoliosis. This demanding procedure was used by Bradford and Tribus [8] for seven patients with severe idiopathic curves (mean Cobb angle 91°), and led to an average scoliosis correction rate of 59 %. Suk et al. [9] presented the results of vertebral column resection at the apex of the deformity performed through a single posterior approach in 16 cases (six of them with idiopathic curves) in curves of more than 80° and with a flexibility of less than 25 %; the procedure led to a scoliosis curve correction rate of 59 % with severe complications in four cases.
Recently, some authors [10–13] have used posterior-only fusion for the treatment of severe thoracic AIS. The correction rate of scoliosis was 53.9 % using a hook-only construct [12], 54 % with hybrid instrumentation [10], and 67–68 % with pedicle screws only [13]. Furthermore, two recent studies [14, 15] compared combined treatment (anterior and posterior fusion) with posterior fusion only in severe AIS. Luhmann and Lenke [15] concluded that the patients treated with pedicle screw-only instrumentation presented similar results to those who underwent combined treatment (60.7 vs. 58.5 %), and avoided the negative effects on pulmonary function which the anterior release causes. The use of pedicle screws at all vertebral levels led to the reassessment of the role of posterior-only arthrodesis as treatment for severe scoliosis [16, 17]. Recent studies [18] have shown a correction rate in severe scoliosis treated by all-screw posterior instrumentation to be around 50 %, which is similar to the correction rate obtained by combined approach surgery. Di Silvestre et al. [19] compared two similar series of patients with severe thoracic idiopathic scoliosis (main curve over 80° Cobb), the first treated by posterior hybrid instrumentation fusion and the second by posterior all-screw instrumentation fusion, with a mean follow-up of 6.7 years. They reported a thoracic curve correction rate of 44.52 % in patients treated by hybrid instrumentation versus 52.4 % in patients treated by all-screw instrumentation. The mean loss of correction in patients treated by hybrid instrumentation was −11.3° Cobb compared with −1.9° in patients treated by all-screw instrumentation at the follow-up. Taking account of the previous authors’ findings, we believe that the posterior-only approach avoids the complications associated with the thoracic approach, and reduces the surgery time of the combined procedure as well as morbility and patient hospital recovery.
Materials and methods
From 2006 to 2010, we treated 25 patients (20 females, 5 males) with severe scoliosis by all-screw instrumentation. All patients were affected by AIS without comorbidities. Mean scoliosis curve in Cobb degrees was 95° (85°–135°), mean T5–T12 kyphosis in Cobb degrees was 36° (30°–50°). Offset in the coronal plane was determined by measuring (in cm) the distance between the C7 plumb line and the perpendicular line drawn through the center of the S1 vertebral body [center sacral vertical line (CSVL)] (global coronal balance), for mean 1.3 cm (0.5–4 cm). Mean patients’ age at the time of surgery was 16.5 years (11–18.5 years). Mean Risser sign was 2 (range 0–5). Cases mix included 12 Lenke 1, 8 Lenke 2, 4 Lenke 3, and 3 Lenke 4. A total of 300 screws were inserted at all levels (135 at thoracic level, 165 at the lumbar one)—a mean of 12 screws per patient (range 11–15)—by the same senior surgeon, by free hand technique, without intraoperative neurophysiologic monitoring (IONM) and spine navigation aids; a minimal use of fluoroscopy enabled us to assess the screws’ position. As IONM was not available in our institution, at the time of surgery (we are currently using IONM on a regular basis in spine deformity correction surgery) we performed wake-up tests on all patients, with negative results. Standard X-rays of the spine in anterior–posterior and lateral projections were performed on patients before surgery, as well as lateral bendings in anterior–posterior projections. MRIs of the cord were performed to assess the presence of neural abnormalities. Anterior–posterior X-rays of the whole spine in suspension were performed in some cases (Stagnarà suspension test). We did not routinely use CAT scans to assess diameter and orientation of the pedicles. We operated all patients by “free hand” technique for the placement of the instrumentation, relying completely on the use of visible and palpable anatomic landmarks for the accurate insertion of the pedicle screws, as previously described by the authors [20]. This technique depends on the clear exposition and identification of the posterior elements bony landmarks [21]. We performed an accurate anatomic exposition of posterior bone structure of the spine, beginning with a subperiosteal dissection, to remove muscles insertion with minimal hemorrhaging and to reduce the curve’s stiffness; hemostasis is a meticulous way of reducing blood loss and of maintaining a clear operating field, to determine the correct insertion point for the screw. Contrary to other authors, we believe that there is no need at the thoracic level to insert pedicle screws in all vertebras of the curve, but only at that levels that are considered key points for obtaining curve correction on both the coronal and sagittal planes [17]. We do not routinely perform laminotomy to explore the pedicle direction before screw insertion, and we do not think that this step is usually necessary; we believe that it is generally sufficient to rely on the correct identification of the posterior vertebral elements anatomic landmark. We managed to reduce operating time without compromising correct pedicle screws positioning. Radiologic controls were also reduced to a minimum, as we used radioscopy, usually from a lateral view, only to assess the correct position in the spine and the final pedicle screws position. Mean X-rays exposition for each patient was 1.3 s (0.5–2 s). Mean operative time was 300 min (range 270–400 min), mean perioperative blood loss was 850 ml (range 250–1,100 ml) and mean hospital recovery was 9 days (range 8–12 days).
We experienced no major complications (instrumentation loosening, infection, neurologic or visceral impairment). No other operation (thoracoplastic) was performed.
Results
Mean scoliosis curve after surgery was 37° Cobb (range 25°–60° Cobb), mean T5–T12 kyphosis in Cobb degrees was 29° (25°–40°), and mean global coronal balance was 0.9 cm (0.3–1.8 cm). Mean follow-up was 4 years (3–6 years). All patients were braced for a total of 6 months after surgery, initially in a cast for a mean time of 6 weeks (range 4–12 weeks) and subsequently in a Cheneau brace. Some of the patients we treated came from abroad; the minimum amount of time that they wore casts after returning home after surgery was three months. All patients were evaluated after surgery with clinical exams and anterior posterior and lateral projections X-rays at 1, 3, 6, and 12 months after surgery and then every other year. See Figs. 1 and 2 .
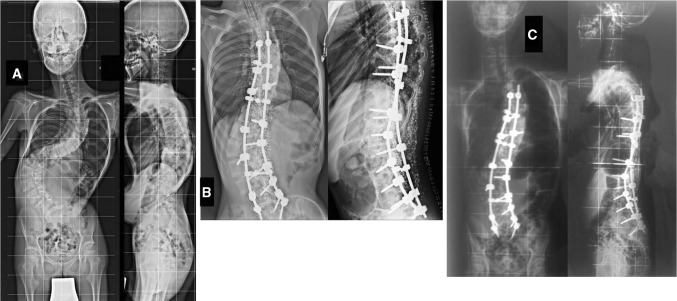
Fig. 1.
MM male age 18 years. a Scoliosis main curve 120° Cobb. b Post-operatory X-rays 41° Cobb. c Follow-up 3 years after operation 43° Cobb
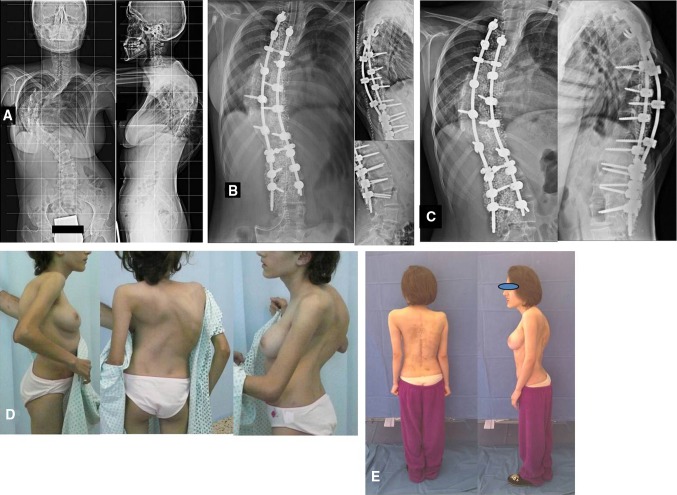
Fig. 2.
AK female age 13 years and 3 months. a Scoliosis main curve 127° Cobb. b Post-operatory X-rays 45° Cobb. c Follow-up 48° Cobb. d Clinical aspect before surgery. e Clinical aspect at follow-up 3 years + 8 months after surgery, good cosmetic result
Mean correction rate was 55 % (range 35–75 %), with mean correction loss of 6° Cobb at follow-up (range 4°–9°). We experienced no cases of arthrodesis malunion or of curve progression after surgery. In two patients (10 %) standard post-operative X-rays showed the malposition of four screws, without any consequence for the arthrodesis, curve correction or these patients’ clinical condition. We did not carry out MRIs or CAT scans on patients after surgery and no revision surgery was performed. See Figs. 3 and 4 .
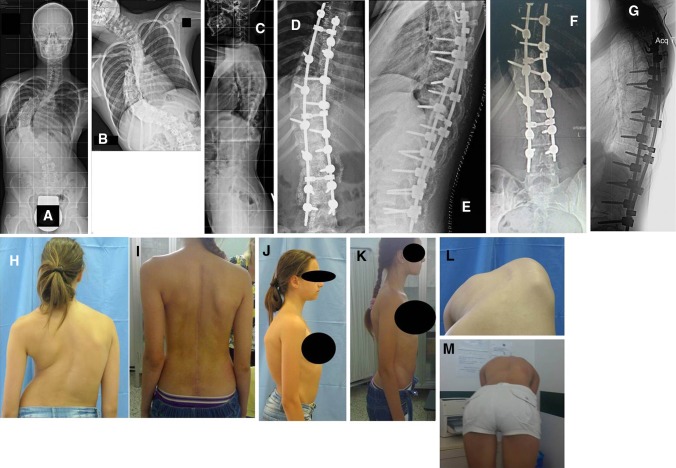
Fig. 3.
NS female age 14 years and 4 months. a–c Scoliosis main curve 112° Cobb. b Bending reduces to 90° Cobb. d, e Post-operatory X-rays 32° Cobb. f, g Follow-up 4 years after operation 36° Cobb. h, j, l Clinical aspect before surgery. i, k, m Clinical aspect at follow-up 4 years after surgery, good cosmetic result
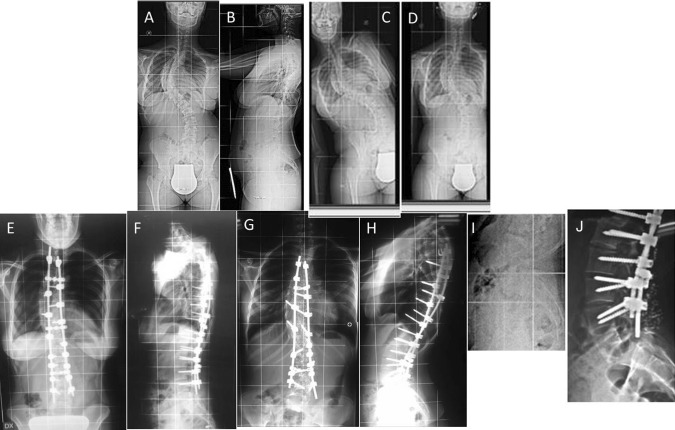
Fig. 4.
RG female age 13 years. a, b Scoliosis main curve 90° Cobb. c, d Curve stiffness at bending. e, f Post-operatory X-rays 30° Cobb. g, h Follow-up 5 years after surgery 34° Cobb. i Associated spondylolisthesis before surgery. j Spondylolisthesis stable 5 years after surgery
The patients operated by posterior approach with all-screw instrumentation at thoracic level were compared with the 15 patients operated before 2006 using a combined anterior–posterior approach with hybrid instrumentation, with a mean follow-up of 11.6 years (range 7–14 years). We recorded better correction, 59 % (using Halo traction after an anterior approach operation), with mean curve correction loss of 3° Cobb (range 0°–5° Cobb) at the follow-up. These results are only marginally better than the ones obtained by posterior approach all-screw instrumentation correction and, in our opinion, do not justify the longer hospital recovery and the double surgical approach envisaged by the first procedure. Our series is undoubtedly numerically low and is not statistically significant; we believe, however, that it offers reliable information concerning the choice of posterior approach using only all-screw instrumentation when treating these patients.
Discussion
All-screw instrumentation allows better correction than wires/hooks and hybrid instrumentation and lesser correction loss at follow-up [22]. This is due to the screws better and deeper grip in the vertebral body, which offers a better and more prolonged vertebral control than hooks/wires. Screws have better initial stability which determines a more effective arthrodesis distribution and maturation after correction has been obtained; arthrodesis maturation in hooks/wires and hybrid instrumentation could be compromised by the hooks’ minimum mobilization. As international literature has highlighted the hooks’ arthrodesis loss of correction is worse than the screws’ arthrodesis loss of correction. The use of screws at thoracic level also, not only improves the deformity correction and minimizes the loss of correction at follow-up, but has also become an essential technical necessity and an obligatory step in vertebral disease treatment, as the use of pedicle screws in severe thoracic deformity allows successful corrections more than any other type of instrumentation. The absence of vertebral canal intrusion in correctly placed pedicle screws compared with other instrumentations is a key aspect of the effectiveness of pedicle screws use in every vertebral area. Although pedicle wall violation is possible, permanent complications are rare [23], particularly if the technique is correct and the misplacement is not redundant. The occurrence of pedicle violation in the literature is inversely correlated with the size of the pedicle [13, 16], therefore the technique must be particularly accurate in the thoracic spine. In our experience, an accurate anatomic landmark preparation during surgery allows a safe positioning of thoracic pedicle screws, and therefore we do not normally use CAT scans to assess pedicles morphology before surgery. We performed free hand procedure without IONM, and we experienced no neurologic impairment in our series. IONM was not available at our institution at the time of surgery; we have subsequently introduced this technical support and we are routinely using it in posterior approach all-screw instrumentation operations; in our opinion, our experience shows that this technical support is useful and increases the safety of the operation, and reduces surgery time as it avoids the wake-up test. A minimal malposition of a pedicle screw is not particularly risky, particularly if the screw has an adequate length, and it does not compromise arthrodesis stability due to multi-segmental stabilization [24]. The intrinsic rigidity of all-screw instrumentation in posterior approach-only surgery minimizes the crankshaft phenomenon due to residual anterior vertebral growth in very young patients [25], even if our cases mix did not include patients under 11 years of age. In our series, we experienced no curve progression and even in cases where post operation X-rays showed a screw malposition (10 %) this had no consequence on the outcome of our treatment. We experienced no case of malunion, and this result is most probably due to prolonged bracing of patients after surgery.
Conclusions
Posterior spinal fusion with pedicle screw-only instrumentation obtains a good and stable correction of severe scoliosis; compared to hybrid instrumentation, it allows a greater coronal correction of deformity and less correction loss at follow-up. Neurological and visceral complications in pedicle screw instrumentation of scoliosis are rarely reported in literature and, while medial pedicle wall violation by the screws misplacement is a concern particularly at thoracic level, the procedure when performed by an experienced spine surgeon is safe. “Free hand” pedicle—screw insertion is an effective technique, which relies only on posterior anatomic landmarks and on a very limited use of radioscopy to assess the screws positioning. It does not envisage the use of anatomic navigation aids or IONM. The technique’s learning curve is long and requires time. Some authors advocate the risk of developing crankshaft phenomenon when posterior-only instrumented fusion is performed in younger patients with severe idiopathic scoliosis, but experience suggests that an all-screw posterior construct is stiffer than hybrid instrumentation and completely avoids the necessity for an anterior procedure.
Conflict of interest
None.
References
- 1.Bullmann V, Halm HFH, Schulte T, Lerner T, Weber TP, Liljenqvist UR. Combined anterior and posterior instrumentation in severe and rigid idiopathic scoliosis. Eur Spine J. 2006;15:440–448. doi: 10.1007/s00586-005-1016-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shufflebarger HL, Grimm JO, Bui V, Thomson JD. Anterior and posterior spinal fusion. Staged versus same day surgery. Spine. 1991;16:930–933. doi: 10.1097/00007632-199108000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Shen J, Qiu G, Wang Y, Zhang Z, Zhao Y. Comparison of 1-stage versus 2-stage anterior and posterior spinal fusion for severe and rigid idiopathic scoliosis—a randomized prospective study. Spine. 2006;31:2525–2528. doi: 10.1097/01.brs.0000240704.42264.c4. [DOI] [PubMed] [Google Scholar]
- 4.Kim YJ, Lenke LG, Bridwell KH, Kim KL, Steger-May K. Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure. J Bone Joint Surg Am. 2005;87:1534–1541. doi: 10.2106/JBJS.C.00978. [DOI] [PubMed] [Google Scholar]
- 5.Arlet V. Anterior thoracoscopic spine release in deformity surgery: a meta-analysis and review. Eur Spine J. 2000;9:S17–S23. doi: 10.1007/s005860000186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Niemeyer T, Freeman BJ, Grevitt MP, Webb JK. Anterior thoracoscopic surgery followed by posterior instrumentation and fusion in spinal deformities. Eur Spine. 2000;J9:499–504. doi: 10.1007/s005860000181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Newton PO, Marks M, Faro F, Betz R, Clements D, Haher T. Use of video-assisted thoracoscopic surgery to reduce perioperative morbidity in scoliosis surgery. Spine. 2003;28:S249–S254. doi: 10.1097/01.BRS.0000092475.04293.F5. [DOI] [PubMed] [Google Scholar]
- 8.Bradford DS, Tribus CB. Vertebral column resection for the treatment of rigid coronal decompensation. Spine. 1997;22:1590–1599. doi: 10.1097/00007632-199707150-00013. [DOI] [PubMed] [Google Scholar]
- 9.Suk SI, Chung ER, Kim JH, Kim SS, Lee JS, Choi WK. Posterior vertebral column resection for severe rigid scoliosis. Spine. 2005;30:1682–1687. doi: 10.1097/01.brs.0000170590.21071.c1. [DOI] [PubMed] [Google Scholar]
- 10.Arlet V, Jiang L, Ouellet J. Is there a need for anterior release for 70°–90° thoracic curves in adolescent scoliosis? Eur Spine J. 2004;13:740–745. doi: 10.1007/s00586-004-0729-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burton DC, Sarna AA, Asher MA. The treatment of large(>70°) thoracic idiopathic scoliosis curves with posterior instrumentation and arthrodesis: when is anterior release indicated? Spine. 2005;30:1979–1984. doi: 10.1097/01.brs.0000176196.94565.d6. [DOI] [PubMed] [Google Scholar]
- 12.De Giorgi G, Stella G, Becchetti S, Martucci G, Miscioscia D. Cotrel-Duboysset instrumentation for the treatment of severe scoliosis. Eur Spine J. 1999;8:8–15. doi: 10.1007/s005860050120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuklo TR, Lenke LG, O’Brien MF, Lehman RA, Polly DW, Schroeder BS. Accuracy and efficacy of thoracic pedicle screws in curve more than 90°. Spine. 2005;20:222–226. doi: 10.1097/01.brs.0000150482.26918.d8. [DOI] [PubMed] [Google Scholar]
- 14.Dobbs MB, Lenke LG, Kim YJ, Luhmann SJ, Bridwell KH. Anterior/posterior spinal instrumentation versus posterior instrumentation alone for the treatment of adolescent idiopathic scoliotic curves more than 90°. Spine. 2006;31:2386–2391. doi: 10.1097/01.brs.0000238965.81013.c5. [DOI] [PubMed] [Google Scholar]
- 15.Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M. Thoracic adolescent idiopathic scoliosis curves between 70° and 100°. Is anterior release necessary? Spine. 2005;30:2061–2067. doi: 10.1097/01.brs.0000179299.78791.96. [DOI] [PubMed] [Google Scholar]
- 16.Lenke LG, Kuklo TR, Ondra S, Polly DW. Rationale behind the current State-of-the-Art treatment of scoliosis (in the pedicle screw era) Spine. 2008;33(10):1051–1054. doi: 10.1097/BRS.0b013e31816f2865. [DOI] [PubMed] [Google Scholar]
- 17.Suk S, Kim JH, Kim SS, Lim DJ. Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS) Eur Spine J. 2012;21:13–22. doi: 10.1007/s00586-011-1986-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Min K, Sduzy C, Farshad M. Posterior correction of thoracic adolescent idiopathic scoliosis with pedicle screw instrumentation: results of 48 patients with minimal 10-year follow up. Eur Spine J. 2013;22(2):345–354. doi: 10.1007/s00586-012-2533-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Di Silvestre M, Bakaloudis G, Lolli F, Vommaro F, Martikos K, Parisini P. Posterior fusion only for thoracic adolescent idiopathic scoliosis of more than 80°: pedicle screws versus hybrid instrumentation. Eur Spine J. 2008;17:1336–1349. doi: 10.1007/s00586-008-0731-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crostelli M, Mazza O, Mariani M. Free-hand pedicle screws insertion technique in the treatment of 120 consecutive scoliosis cases operated without use of intraoperative neurophysiological monitoring. Eur Spine J. 2012;21(Suppl 1):S43–S49. doi: 10.1007/s00586-012-2218-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Modi HN, Suh SW, Hong JY, Yang JH. Accuracy of thoracic pedicle screw using ideal pedicle entry point in severe scoliosis. Clin Orthop Relat Res. 2010;468:1830–1837. doi: 10.1007/s11999-010-1280-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kadoury S, Cheriet F, Beausèjour M, Stokes IA, Parent S, Labelle H. A three-dimensional retrospective analysis of the evolution of spinal instrumentation for the correction of adolescent idiopathic scoliosis. Eur Spine J. 2009;18:23–37. doi: 10.1007/s00586-008-0817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gang C, Haibo L, Fancai L, Weinshan C, Qixin C. Learning curve of thoracic pedicle screw placement using the free-hand technique in scoliosis: how many screws needed for an apprentice? Eur Spine J. 2012;21:1151–1156. doi: 10.1007/s00586-011-2065-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sarlak AY, Buluc L, Sarisoy HT, Memisoglu K, Tosun B. Placement of pedicle screws in thoracic idiopathic scoliosis: a magnetic resonance imaging analysis of screw placement relative to structures at risk. Eur Spine J. 2008;17:657–662. doi: 10.1007/s00586-008-0639-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Suk SI, Kim JH, Cho KJ, Kim SS, Lee JJ, Han TY. Is anterior release necessary in severe scoliosis treated by posterior segmental pedicle screw fixation? Eur Spine J. 2007;16:1359–1365. doi: 10.1007/s00586-007-0334-x. [DOI] [PMC free article] [PubMed] [Google Scholar]