Abstract
Objective
The aim of this study was to evaluate the effectiveness of Chêneau brace in the management of idiopathic scoliosis.
Methods
This is a retrospective observational study according to SOSORT and SRS (Scoliosis Research Society) recommendations involving 48 girls with documented progressive idiopathic scoliosis, treated with Chêneau brace. A statistical analysis was performed with STATA MP11.2 to validate the obtained results.
Results
No patient needed surgery. The average curve angle measured in Cobb degrees passed from 27° ± 6.7° at the beginning (T0), to 7.6° ± 7.4° in brace (T1) (72 % of correction), to 8.5° ± 8.6° (69 % of correction) at the end of treatment (T2), to 11.0° ± 7.4° (59.3 % of correction) at final follow-up (mean 5 years and 5 months) (T3).
Conclusion
Conservative treatment with Chêneau brace and physiotherapy was effective in our hands for halting scoliosis progression in 100 % of patients.
Keywords: Chêneau brace, Idiopathic scoliosis, Conservative treatment
Introduction
Adolescent idiopathic scoliosis (AIS) is a structural three-dimensional deformity of the spine arising in otherwise normal children during puberty. The 1982 report of the Scoliosis Research Society defined that 2–3 % of children younger than 16 years of age will have a curvature of 10°, but only 0.3–0.5 % will have a curvature of 20° [1]. Long-term follow-ups indicate that patients with scoliosis may have a higher prevalence of back pain and of worsening pulmonary function if the curve becomes extremely large [2]. Therefore, the treatment of AIS during adolescence is mainly an attempt to prevent problems during adulthood by stopping the progression of the curve. The aim of brace treatment is to stop the evolution of the deformity in immature adolescents and is an established method of conservative treatment for AIS [3]. The Chêneau brace is the most widely used in Europe [4] within the group of rigid thoraco-lumbo-sacral orthoses (TLSO). The major mechanism of this orthosis consists of a three-dimensional correction of the spine deformity by a system of multipoint pressure zones and expansion chambers [4, 5]. The Chêneau brace creates pressure on the convexity of the curve, and, on the opposite side, there are wide expansion chambers in the frontal, sagittal and horizontal planes, where the patient has to put his body mass through physiotherapy of deviation from pushes and respiratory kyphotic exercises for at least 1 h every day [6–8]. To correct the flat back, commonly associated with scoliosis [9], a gypsotomy on the cast at T8 is performed and a sternal kyphotic push is applied during the preparation of the brace.
Studies carried out so far show that wearing a brace changes the natural history of scoliosis and probably helps the patient to avoid surgery [6, 10, 11], especially if the brace meets current quality standards [12, 13]. In 2005 a systematic review of literature was carried out focusing on evaluating the effectiveness of conservative treatment methods for scoliosis, including bracing [14]. In 2010 a Cochrane Database of Systematic Reviews publication revealed low-quality evidence in favor of using bracing [15]. For treatment of teenagers with progressive adolescent idiopathic scoliosis in an early stage, many doctors and patients prefer brace treatment because surgery of the spine is generally considered a drastic intervention [16]. Indications for the Chêneau brace are represented by progressive idiopathic scoliosis during growth, with an upper end vertebra caudal to T5 and a Cobb angle between 25° and 45° [4, 17]. The aim of this study was to estimate the incidence of surgery in Chêneau brace-treated patients with AIS and to evaluate the effectiveness of the brace in stopping the progression of scoliosis.
Materials and methods
From 1994 to 2009, 73 subjects with AIS were treated with Chêneau brace. To properly evaluate this brace, the following groups were excluded from the database: eight subjects who prematurely stopped the brace or were not diligent in brace wearing or daily physiotherapy; five subjects who were wearing the Chêneau brace after having used another kind of brace and another seven people who were not more than Risser 4 in 2009. It was important to consider only those people who were compliant with the treatment to have real data about the efficacy of the brace. To create a more homogeneous sample, five cases of double curve were excluded from the database. The Chêneau brace was manually made, without using CAD CAM software, following numerous instructional courses by Dr. J. Chêneau.
Retrospectively, 48 AIS patients with an age range of 11.3 ± 2.0 years (range 10–15) at the beginning of the treatment were analyzed. They had been treated in our department from 1994 to 2009 with Chêneau brace according to the principles of wearing it for 23 h a day, together with physiotherapy [17]. Inclusion criteria were initial Cobb angle between 20° and 45°, no previous brace treatment and Risser 4 or more at the final evaluation, minimum 2 years follow-up after wearing the brace. All conservatively treated patients with scoliosis of 20° to 29° had radiological evidence of progression (defined as Cobb angle increase of 5° or more after 6 months). Patients with scoliosis of 30° or more started the brace treatment without radiological evidence of progression. All the patients and their parents signed an informed consent to the treatment and accepted our protocol of semestral consultations, bimenstrial evaluation of the brace, daily practice of physiotherapy and full-time (23 h a day) wearing of the brace. Treatment was ended at the end of bone growth, measured by an X-ray of the non-dominant wrist, showing a complete fusion of the distal metaphyseal growing cartilage of the radius. It occurred at a mean age of 16 years and 6 months (min 15–max 18 years). Brace wearing was stopped before the end of the bone growth for eight girls presenting a temporary light hypercorrection of the curve, only if the hypercorrection was confirmed after 6 or more months of reduction of brace wearing.
All patients had a single curve: 8 thoracic (16.7 %; 95 % CI 6.1–27.2), 28 thoracolumbar (58.3 %; 44.4–72.3) and 12 lumbar (25 %; 95 % CI 12.7–37.2).
Standing out-of-brace frontal Cobb angle [18] was measured before treatment (T0), at the end of the treatment (T2) and at the last follow-up (T3) (average 5 years and 5 months; min 2–max 14) by two expert authors on 30 × 90 long X-rays with a distance of 2 m until 2005 and on digital X-rays from 2005. A statistical correlation for inter-rater agreement and inter-observer variability was performed by calculating the Fleiss K (K = 0.70; p < 0.05). For the statistical analysis the mean value of the two obtained measurements was used. In the same period, the vertebral axial rotation was quantified at the level of the apical vertebra according to the Perdriolle method. The sagittal parameters of the spine, like the sacral slope (SS), the lumbar lordosis (LL) and thoracic Kyphosis (CT) were also measured on long-standing X-rays (30 × 90 cm) in pre- and post-treatment and at the last follow-up.
Also in the same periods, the curve values and the C7–S1 balance [19, 20] on the frontal plane were measured. The SRS 22 form was adopted for the clinical evaluation.
Data were recorded on specific forms and inserted into a database created by File Maker Pro. A statistical analysis was performed with STATA MP11.2 (StataCorp LP, College Station, TX, USA) to validate the obtained results. Using a T test for paired samples, mean differences with standard deviation in correction of scoliosis curves (A.V. Cobb degrees and Perdriolle degrees for rotation of the apical vertebra) were determined between values before treatment (T0), in brace (T1), at the end of treatment (T2) and at the final follow-up (T3). A multiple logistic regression model was used to evaluate the influence of age at the beginning of treatment, the menarche and the initial curve values on the final results at follow-up. A p value of less than 0.05 was considered to be significant.
Results
Table 1 shows the average angle at the beginning (T0), in brace (T1), after treatment (T2) and at the final follow-up (T3) with the sample divided into two groups: subjects who began treatment before menarche and after it.
Table 1.
Cobb angle (angular value) of the scoliosis curve
| Cobb angle | Beginning (T0) | In brace (T1) | End of treatment (T2) | Final F.U. (T3) |
|---|---|---|---|---|
| Average A.V. | 27° ± 6.7° | 7.6° ± 7.4° (72 % of correction) (t = 19.8; p < 0.0001) |
8.5° ± 8.6° (69 % of correction) (t = −13.7; p < 0.00001) |
11.0° ± 7.4° (59.3 % of correction) (t = −13.9; p < 0.0001) |
| A.V. before menarche (34) | 28.5° ± 7.1° | 7.4° ± 8.6° (t = 17.6; p < 0.0001) |
7.8° ± 9.5° (t = 13.5; p < 0.0001) |
10.9° ± 7.8 (t = 13.6; p < 0.0001) |
| A. V. after menarche (14) | 23.7° ± 3.9° | 8.3° ± 3.5° (t = 13.2; p < 0.0001) |
10.1° ± 6.1° (t = 6.4; p < 0.0001) |
11.2° ± 6.7 (t = 5.7; p < 0.0001) |
| T | 2.34 | −0.37 | −0.85 | −0.11 |
| p | 0.01 | >0.05 | >0.05 | >0.05 |
In the multiple regression logistic model there is no correlation between the angular Cobb value at final follow-up and menarche
The logistic multivariate regression model showed that the Cobb angle at follow-up was not dependent on menarche, the age at the beginning of treatment, the kind of curve or the duration of treatment (p > 0.05).
The rotation of the apical vertebra measured in Perdriolle degrees is shown in Table 2. Comparing the value of the apical vertebra rotation in brace (T1) and at the end of the treatment (T2), there were no differences between the group “before menarche” (t = −1.6; p = 0.057) and in the group after menarche (t = −1.4; p = 0.09).
Table 2.
Rotation of apical vertebra (angular value in Perdriolle degrees)
| A.V. | Beginning (T0) | In brace (T1) | End of treatment (T2) | Final F.U. (T3) |
|---|---|---|---|---|
| Average rotation | 9.3 ± 4.8 | 2.2 ± 3.8 (t = 10.6; p < 0.0001) |
3.2 ± 3.7 (t = 8.7; p < 0.0001) |
4.1 ± 3.9 (t = 8.4; p < 0.0001) |
| Before menarche (34) | 9.5 ± 4.5 | 2.1 ± 3.9 | 3.1 ± 3.7 | 3.9 ± 3.6 |
| After menarche (14) | 8.9 ± 5.7 | 2.6 ± 3.4 | 3.7 ± 4.0 | 4.4 ± 4.6 |
| T | 0.35 | −0.37 | −0.54 | −0.36 |
| p | >0.05 | >0.05 | >0.05 | >0.05 |
In the multiple regression logistic model there is no correlation between the angular Perdriolle value at final follow-up and menarche
At the end of treatment (T2), there were no statistically significant differences in comparison to the Perdriolle angle obtained in brace (T1).
The results obtained dividing subjects according to the kind of curves are shown in Table 3. Thoracolumbar curves reach the best correction at the final follow-up (61.7 %), but using the Anova test the differences in correction in comparison to other kinds of curve were not statistically significant (F = 0.51; p = 0.68). Nevertheless, there is better correction of thoracolumbar curves when the treatment begins before menarche. The sagittal shape measured with a plumbline at C7, T7, L4 and S2 passed from 40/30/48/13 at the beginning to 36/6/37/0 after treatment and 28/4.5/41/0 at final follow-up. The correction of the flat back ameliorates with the treatment and at final follow-up. Some radiographic results are shown in Figs. 1 (NP) and 2 (DSP).
Table 3.
Kind of curve and corrections of angular value
| Kind of curve | A.V. before treatment | A.V. in brace | A.V. at final follow-up |
|---|---|---|---|
| Thoracolumbar 29 cases | 26.9° ± 4.9° | 6.1° ± 6.7° (77.3 %) | 10.3° ± 7.7° (61.7 %) |
| Lumbar 12 cases | 29.3° ± 10.0° | 11.2° ± 9.9° (61.8 %) | 12.7° ± 8.5° (56.6 %) |
| Thoracic 7 cases | 24.3° ± 5.6° | 7.9° ± 4.1° (67.5 %) | 11.6° ± 4.8° (52, 3.3 %) |
Fig. 1.
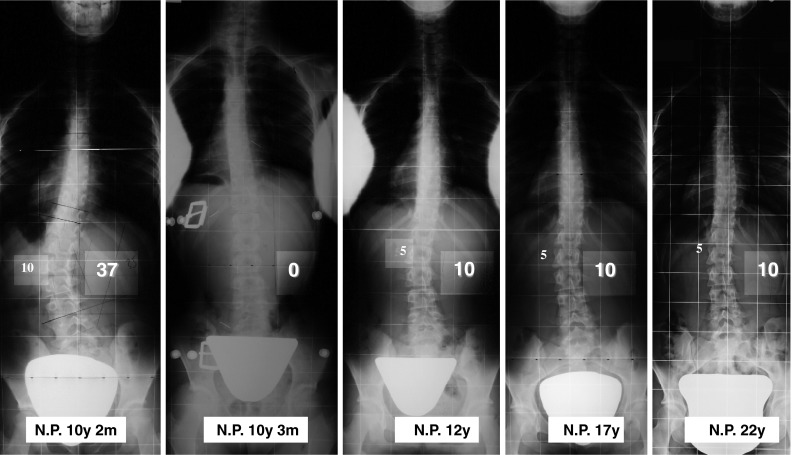
N.P. 10 years beginning of treatment, A.V. in brace, during treatment, at the end of treatment and at final follow-up
Fig. 2.
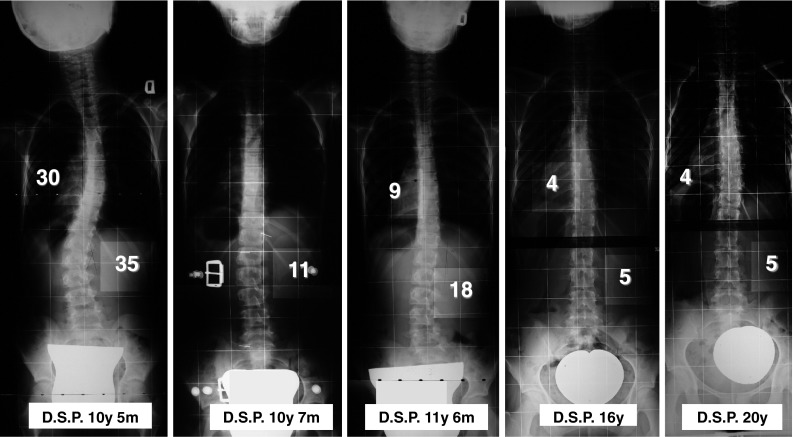
DSP 10 years 5 months beginning of treatment, A.V. in brace, during treatment, at the end of treatment and at final follow-up
In eight cases, a temporary inversion of the curve during treatment demonstrated the efficacy of the brace correction. Thus, the number of hours of brace wearing was reduced and the brace was progressively abandoned before the end of bone growth (Figs. 3 DF, 4 CC).
Fig. 3.
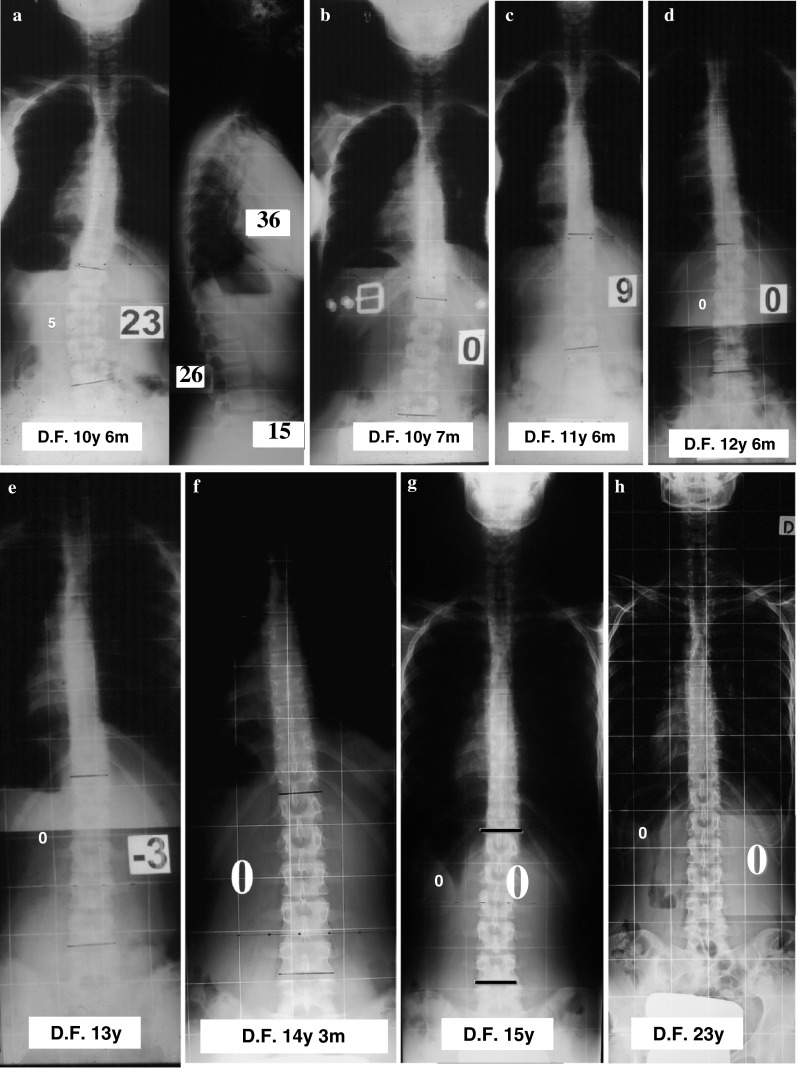
D.F. 10 years 6 months beginning of treatment (a), A.V. in brace (b), during treatment (c–f), at the end of treatment (g) and at final follow-up (h)
Fig. 4.
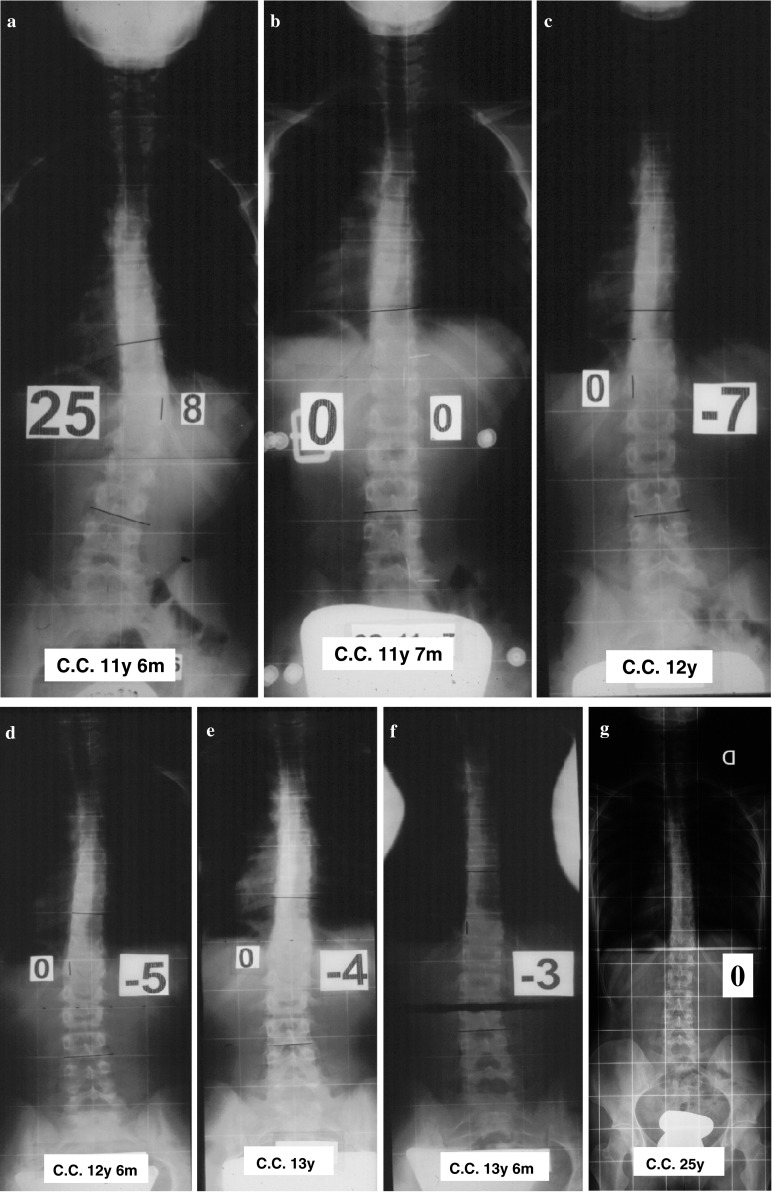
CC 11 years 6 months beginning of treatment (a), A.V. in brace (b), during treatment (c–e), at the end of treatment (f) and at final follow-up (g)
The average value of the SRS22 score at follow-up was 19.4 (min 12–max 22).
Discussion
The importance of this paper lies in the fact that it is a homogeneous case series of patients with only one prescriptor, only one brace maker, effective correction control by X-rays inside the brace and a careful selection of patients with regard to brace wearing and physiotherapy. At final follow-up, the average correction was 59.3 % of the initial values of scoliosis. In the literature, the reported values of correction at average and long follow-up with other braces are less significant than with the Chêneau brace [21–24], but those papers show no certain results with brace wearing. The PASB brace by Aulisa showed a good correction for thoracolumbar and lumbar curves [25]. The Chêneau brace showed a high percentage of correction of all curves and a more important percentage of correction at the final follow-up for thoracolumbar curves. No patient was worse after treatment and all patients’ symptoms ameliorated or were stable at the final follow-up. No patient needed a surgical procedure to correct scoliosis, so in this sample the Chêneau brace was effective in avoiding curve progression and surgery in AIS considering the natural history of the disease. It is important to remember that eight patients who were not compliant with treatment were excluded to avoid confusing results. The mean correction of curves at the final follow-up (T3) was 59.3 % and in thoracolumbar curve it reached 61.7 %. When the Chêneau brace is used for thoracolumbar scoliosis before menarche, there is a real chance of success, with the possibility of hypercorrection of the curve during treatment and the definitive healing of the disease, despite suspension of brace wearing during the years of bone growth. This personal case series demonstrates that it is possible to achieve excellent healing of scoliosis, if treatment is started at a suitable time and with an adequate brace. This is a pilot study, so the conclusions are limited.
The strong points of this paper are that all patients were treated by the senior author and only by a Chêneau brace made by only one experienced brace maker following numerous instructional courses by Dr. J. Chêneau and that the final follow-up was quite high. The weak points are that the sample is quite small, double curves are not considered and the measurements are basically based on Cobb degree measurement. A possible bias can be present in the angular values at the beginning of treatment (T0) between group before menarche and after menarche (the groups are obviously not perfectly homogeneous). The expertise achieved by the brace maker was essential in obtaining good results and this could perhaps be considered another weak point of the study.
The Cobb value on wearing brace (T1) is statistically significantly lower than the Cobb value at the beginning (T0), thus demonstrating the efficacy of the brace correction (t = 19.8; p < 0.0001). The average angle was not different at the final follow-up (T3) and after the treatment (T2) (t = 2.52; p > 0.05), thus demonstrating that there was no loss of correction at the final follow-up and that also future results should be stable [19].
Conclusions
Our pilot study demonstrates that the Chêneau brace can be effective in avoiding curve progression and surgery in AIS considering the natural history of the disease.
Conflict of interest
None.
References
- 1.Nachemson AL, Lonstein JE, Weinstein SL. Report of the prevalence and natural history committee of the scoliosis research society. Denver: Scoliosis Research Society; 1982. [Google Scholar]
- 2.Weinstein SL, Dolan LA, Spratt KF, et al. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA. 2003;289:559–600. doi: 10.1001/jama.289.5.559. [DOI] [PubMed] [Google Scholar]
- 3.Müller C, Fuchs K, Winter C, Rosenbaum D, Schmidt C, Bullmann V, Schulte TL. Prospective evaluation of physical activity in patients with idiopathic scoliosis or kyphosis receiving brace treatment. Eur Spine J. 2011;20(7):1127–1136. doi: 10.1007/s00586-011-1791-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chêneau J. Corset Chêneau. Manuel d’orthopédie des scolioses suivant la technique originale. Ed: Masson; 1994. [Google Scholar]
- 5.Landauer F, Wimmer C. Therapieziel der Korsettbehandlung bei idiopathischer Adoleszentenskoliose. MOT. 2003;123:33–37. [Google Scholar]
- 6.Grivas TB, Vasiliadis E, Chatziargiropoulos T, Polyzois VD, Gatos K. The effect of a modified Boston brace with anti-rotatory blades on the progression of curves in idiopathic scoliosis: aetiologic implications. Ped Rehab. 2003;6:237–242. doi: 10.1080/13638490310001636808. [DOI] [PubMed] [Google Scholar]
- 7.Green BN, Johnson C, Moreau W. Is physical activity contraindicated for individuals with scoliosis? A systematic literature review. J. Chiropr Med. 2009;8(1):25–37. doi: 10.1016/j.jcm.2008.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kotwicki T, Chêneau J. Biomechanical action of corrective brace on idiopathic scoliosis: Chêneau 2000 orthosis. Disabil Rehabil Assist Technol. 2008;3(3):146–153. doi: 10.1080/17483100801905744. [DOI] [PubMed] [Google Scholar]
- 9.Schmitz A, Kandyba J, Koenig R, Jaeger UE, Gieseke J, Schmitt O. A new method of MR total spine imaging for showing the brace effect in scoliosis. J Orthop Sci. 2001;6(4):316–319. doi: 10.1007/s007760100025. [DOI] [PubMed] [Google Scholar]
- 10.Rigo M, Reiter C, Weiss H-R. Effect of conservative management on the prevalence of surgery in patients with adolescent idiopathic scoliosis. Ped Rehab. 2003;6:209–214. doi: 10.1080/13638490310001642054. [DOI] [PubMed] [Google Scholar]
- 11.Weiss H-R, Weiss G, Scharr H-J. Incidence of surgery in conservatively treated patients with scoliosis. Ped Rehab. 2003;6:111–118. doi: 10.1080/13638490310001593446. [DOI] [PubMed] [Google Scholar]
- 12.Negrini S, Grivas ThB, Kotwicki T, Rigo M, Zaina F. Standards of management of idiopathic scoliosis with corrective braces in everyday clinics and in clinical research: SOSORT Consensus 2008. Scoliosis. 2009;4:2. doi: 10.1186/1748-7161-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Richards BS, Bernstein RM, D’Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine. 2005;30(18):2068–2077. doi: 10.1097/01.brs.0000178819.90239.d0. [DOI] [PubMed] [Google Scholar]
- 14.Lenssinck M, Frijlink A, Berger M, Bierma-Zeimtra S, Verkerk K, Verhagen A. Effect of bracing and other conservative interventions in the treatment of idiopathic scoliosis in adolescents: a systematic review of clinical trials. Phys Ther. 2005;12:1329. [PubMed] [Google Scholar]
- 15.Negrini S, Minozzi S, Bettany-Saltikov J, Zaina F, Chockalingam N, Grivas TB, Kotwicki T, Maruyama T, Romano M, Vasiliadis ES (2010) Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst Rev 1:CD006850 [DOI] [PubMed]
- 16.Bunge EM, Juttmann RE, de Kleuver M, von Biezen FC, de Koning HJ; NESCIO group (2007) Health-related quality of life in patients with adolescent idiopathic scoliosis after treatment: short-term effects after brace or surgical treatment. Eur Spine J 16(1):83–89 [DOI] [PMC free article] [PubMed]
- 17.Chêneau J. Scoliosis treating brace evaluation of our brace since 1970: an evaluation of the normalization of rotation, of rib static and of the wedge shaped vertebrae. Locomot Syst. 2003;1:29–38. [Google Scholar]
- 18.Cobb JR. Outline for the study of scoliosis. AAOS Instr Course Lect. 1948;5:261–275. [Google Scholar]
- 19.Stagnara P (1985) Les déformations du rachis. Masson, Paris
- 20.Lonstein JE. Moe’s textbook of scoliosis and other spinal deformities. Philadelphia: Saunders; 1995. pp. 45–86. [Google Scholar]
- 21.Jonasson-Rajala E, Josefsson E, Lundberg B, Nilsson H. Boston thoracic brace in the treatment of idiopathic scoliosis. Initial correction. Clin Orthop Relat Res. 1984;183:37–41. [PubMed] [Google Scholar]
- 22.Blaha J, Bukac J. Correction of idiopathic scoliotic curves by means of conservative treatment using spinal bracing. Acta Medica. 2005;48(1):31–35. [PubMed] [Google Scholar]
- 23.Weiss HR, Weiss GM. Brace treatment during pubertal growth spurt in girls with idiopathic scoliosis (IS): a prospective trial comparing two different concepts. Pediatr Rehabil. 2005;8(3):199–206. doi: 10.1080/13638490400022212. [DOI] [PubMed] [Google Scholar]
- 24.Von Deimling U, Wagner UA, Schmitt O. Long term effect of brace treatment on spinal decompensation in idiopathic scoliosis. A comparison of Milwaukee brace—Chêneau corset. Z Orthop Ihre Grenzgeb. 1995;133(3):270–273. doi: 10.1055/s-2008-1039447. [DOI] [PubMed] [Google Scholar]
- 25.Aulisa AG, Guzzanti V, Galli M, Perisano C, Falciglia F, Aulisa L. Treatment of thoraco-lumbar curves in adolescent females affected by idiopathic scoliosis with a progressive action short brace (PASB): assessment of results according to the SRS committee on bracing and non operative management standardization criteria. Scoliosis. 2009;18(4):21. doi: 10.1186/1748-7161-4-21. [DOI] [PMC free article] [PubMed] [Google Scholar]


