Abstract
Introduction
Surgical management of upper cervical spine (UCS) unstable injuries may be challenging as the number of cases requiring this surgery collected in every single center is small. This retrospective study was conducted to analyze the radiographic and clinical results in 12 patients undergoing a posterior occipito-cervical fusion by a polyaxial screws–rod–plate system.
Methods
There were eight male and four female patients with a mean age of 73.7 years (range 32–89 years). Six patients presented neurologic deficits at admission. Six patients had sustained major trauma. The remaining six patients had suffered a minor trauma.
Results
Two patients died postoperatively in Intensive Care Unit. All surviving patients achieved solid fusion at 6 months. No surviving patient had neurological deterioration postoperatively. There were no instrumentation failures or revision required. Two patients suffered from superficial occipital wound infection.
Conclusions
Although the indication to occipito-cervical fusion decreased since the new C1–C2 posterior fixation techniques were described, it remains a valid and reliable option in UCS post-traumatic instability to be applied even in emergency especially in the elderly.
Keywords: Atlanto-occipital dislocation, Cranio-cervical junction, Occipito-cervical fusion, Upper cervical spine instability
Introduction
Traumatic injuries of the craniovertebral junction and UCS pose considerable difficulties in the operative management regarding surgical approach and technique of fixation. These injuries may cause immediate fatality or delayed deterioration of neurological function therefore they require a sound stabilization to be performed as soon as possible [1].
Posterior OCF is the gold standard in atlanto-occipital dislocation (AOD). The same technique can be used in patients with atlanto-axial dislocation and/or significant fracture of the anterior and posterior elements of C1 and C2, which may preclude C1 or C2 screw placement [2].
OCF is a demanding and severely invalidating surgical procedure, mainly compromising axial rotation of the head above the trunk but also flexion–extension. This multi-joint complex allows for >50 % of all head and neck movements [3].
Indication to OCF can only be an instability causing neurologic impairment or a potential neurologic damage.
In addition to these mobile joints, the sharp angle at which the occiput meets the upper cervical spine creates a significant lever arm that works against surgical fixation devices. Therefore, the most rigid fixation device possible is required to promote fusion [4].
Materials and methods
From September 2006 to June 2011, 12 consecutive patients with acute traumatic upper cervical spinal instability underwent a posterior approach OCF with a plate and screw system. Inclusion criteria for the procedure were: AOD, C1–C2 dislocations and C1 and C2 fractures associated with lateral or vertical dislocation due to major ligamentous injuries.
There were eight male and four female patients with a mean age of 73.7 years (range 32–89 years) (Table 1).
Table 1.
Occipito-cervical fusion in upper cervical spine trauma
| Pz | Age | Sex | Diagnosis | Cause | ASIA | Fusion | Δ T (days) | Halo | FU (months) | Complication |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 88 | M | C1–C2 fracture | LET | E | C0–C5 | 3 | No | 56 | |
| 2 | 76 | M | C2–C3 fracture-dislocation | HET | A | C0–C5 | 0 | No | 50 | |
| 3 | 87 | M | C2 odontoid fracture | LET | E | C0–C2 | 3 | Yes | 46 | |
| 4 | 68 | M | C1–C2–C6–C7–Th1 fracture | HET | D | C0–Th2 | 13 | Yes | 36 | |
| 5 | 71 | M | C1–C2 fracture | HET | D | C0–C4 | 0 | No | 30 | |
| 6 | 89 | F | AOD | HET | A | C0–C5 | 2 | No | 0.2 | DEAD after 6 days |
| 7 | 72 | F | C2–C3 fracture-dislocation | LET | E | C0–C5 | 0 | No | 25 | Occipital wound infection |
| 8 | 58 | M | C0–C1–C2 articular fracture | HET | E | C0–C4 | 53 | Yes | 18 | |
| 9 | 81 | M | C1–C2 fracture-dislocation | LET | A | C0–C4 | 2 | No | 0.3 | DEAD after 8 days |
| 10 | 32 | M | AOD | HET | A | C0–C2 | 85 | Yes | 15 | |
| 11 | 80 | F | C1–C2 fracture-dislocation | LET | E | C0–C5 | 3 | No | 12 | |
| 12 | 82 | F | C1–C2 fracture | LET | E | C0–C5 | 3 | No | 12 | Occipital wound infection |
HET high-energy trauma, LET low-energy trauma
Six patients had sustained a high-energy trauma (falls from high or motor vehicle accidents). The remaining six patients had suffered a minor trauma (falls at home) and they all showed an ankylotic cervical spine on preoperative imaging.
Neck pain, stiffness or abnormal posture was recorded in all patients at admission. Six patients had neurological deficits, and were graded ASIA A in four cases and D in two.
Preoperative imaging included CT scan in all patients, X-rays in six, and MRI in one.
The type of skeletal injury and related surgical procedure are summarized in Table 1. The time elapsed between the trauma and the day of surgery ranged from 0 to 85 days (average 16.1 days).
In four cases a halo vest was temporary applied before surgical treatment to stabilize the injury. In these cases surgery was done, respectively, after 3, 13, 53 and 85 days. The first two showed loss of reduction few days after treatment and the last two were referred from other hospital with pressure sore in the occipital region due to stiff collar application. The remaining patients were operated within 3 days after trauma.
Treatment was chosen considering a number of different factors, including the general medical condition of the patient, the severity and location of the fracture, compression of the spinal cord, joints stability and neurological status.
In one case we perform an occipital–Th2 fusion to stabilize multiple cervical fractures. Occipital fixation was achieved with a plate fixed in the midline by two 4.5 mm bicortical screws. To achieve fusion a preshaped tricortical autogenous graft was impacted between the suboccipital bone and superior part of the spinous process of C2 and secured in place with suture.
Results
Ten patients were available to follow-up with an average follow-up of 30 months (12–56 months). Two patients died of pneumonia 6 and 8 days after surgery in the Intensive Care Unit.
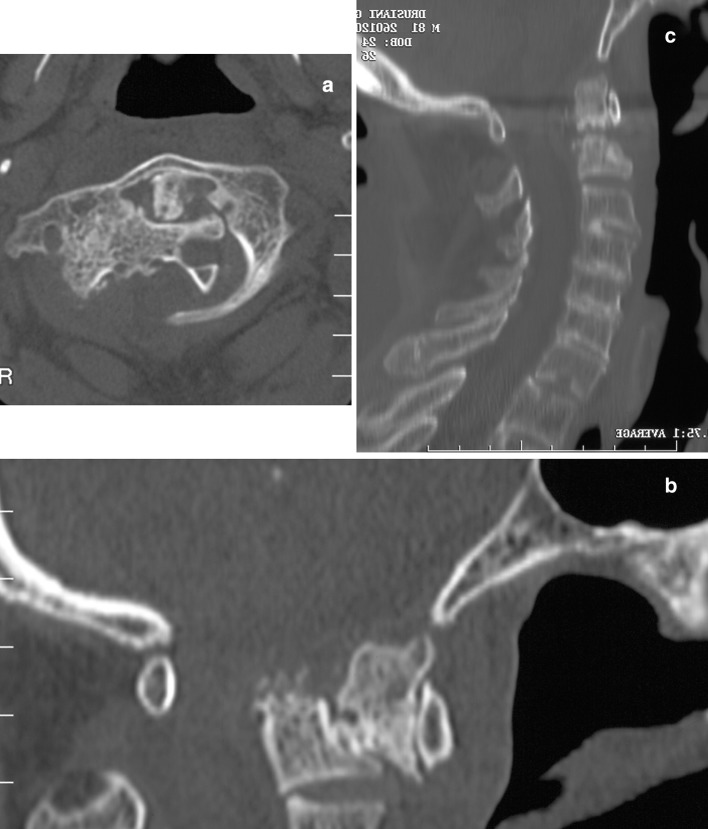
The first case was an 81-year-old man with a C2 fracture-dislocation with a reduction of the spinal canal >50 %, ASIA A at admission. We performed an immediate reduction in emergency room and 2 days later an occipital–C4 fusion (Fig. 1).
Fig. 1.
(Case no. 9) C1–C2 fracture-dislocation with a reduction of the spinal canal >50 % in an 81-year-old man (a, b). Reduction and stabilization is achieved by posterior OCF (c)
The second case was an 89-year-old woman with AOD, ASIA A due to collision with a car and operated 2 days later.
No surviving patient had neurological deterioration postoperatively. Of the patients who had myelopathy preoperatively, two improved from ASIA D to ASIA E. The remaining patients were unchanged at final follow-up.
There were no instrumentation failures and no revision was required related to this complication. Two patients suffered from superficial occipital wound infection. One was treated by oral antibiotics and VAC therapy for 4 weeks. The second patient required a surgical revision after 3 weeks of VAC therapy.
All patients were followed with periodic clinical and radiological controls.
At the most recent follow-up examination, all patients had a satisfactory fusion and the patients without neurological deficit were independent in daily activity.
Discussion
Post-traumatic instability of the cranio-cervical junction remains the primary indication for OCF. Traumatic AOD with survival is rare, as the neurological consequences are usually immediately fatal [5]. However, the use of OCF in trauma patients is not limited to the stabilization of AOD in clinical practice, especially in elderly patients [1].
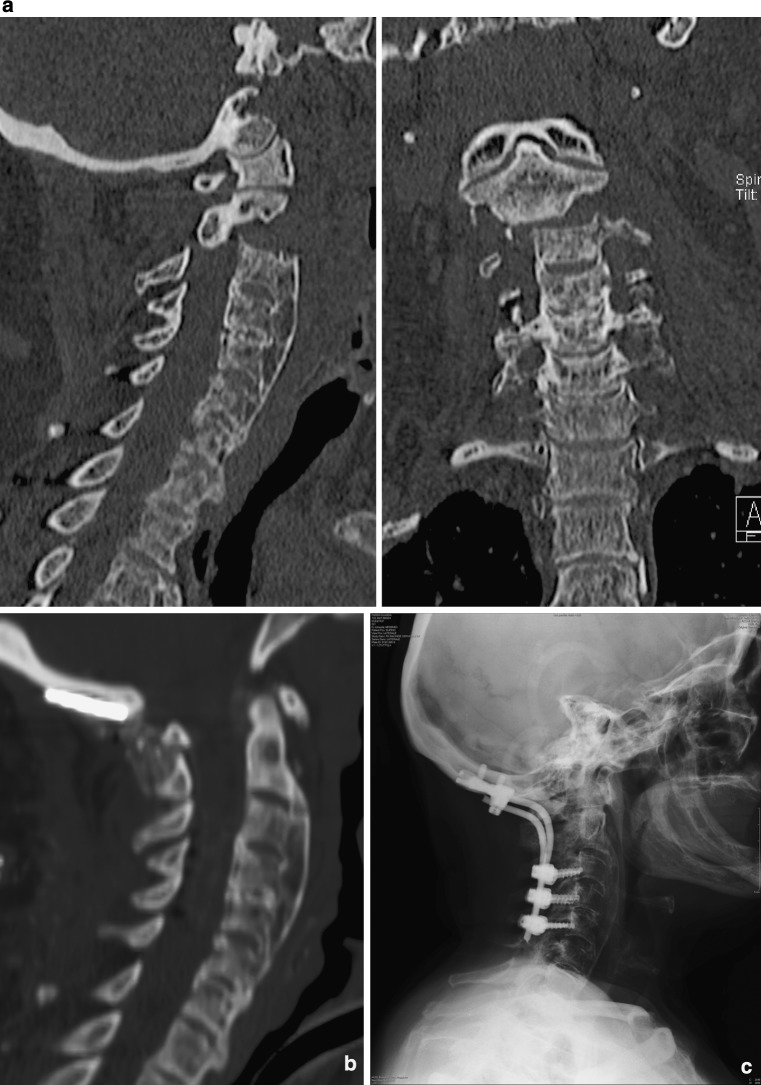
In this series of 12 consecutive patients, only two were treated for AOD. In the remaining cases the patients were elderly, often with minor trauma and complex fractures of the upper cervical spine (Fig. 2).
Fig. 2.
(Case no. 7) C2–C3 fracture-dislocation through a calcified disk in a 72-year-old lady. Preoperative CT showing malalignment in lateral and AP reconstruction (a). Complete healing in correct alignment at 6 months CT (b) and X-rays (c)
The prevalence of cervical spine injuries in the elderly is expected to progressively increase in Europe and North America, as population demographics change. In elderly patients the injury patterns are different from that among younger patients. This is due to the difference in bone density, injury mechanism and presence of degenerative changes. Injuries due to external causes can result in injury deaths and cases of permanent disability. This is especially true for neck injuries, with the potential to cause spinal cord trauma [6].
Degenerative osseous changes are known to influence the site of cervical spine injuries. Normally, in a younger individual, C4–C7 are the most mobile segments of the cervical spine. With degenerative changes, these same segments become stiffer and the C1–C2 segment becomes the most mobile portion of the cervical spine in elderly patients, predisposing the atlanto-axial segment to injury with relatively insignificant trauma [7, 8].
The indication for OCF in patients with trauma to the upper cervical spine, an extensive posterior instrumentation fixation procedure that sacrifices the motion of the occipital and C1–2 complex and a variable amount of subaxial motility, is still controversial [3, 9, 10].
The management of cervical spine injuries in elderly patients may be complicated by a number of factors, including pre-existing medical conditions such as cardiopulmonary compromise, diminished ability to tolerate external immobilization and reduced potential for osseous union.
Few reports in the literature describe the treatment of these fractures, but they are usually treated non-operatively [11].
Hadley et al. [12] recommended 8–12 weeks of halo vest or similar immobilization for patients with significant fractures of the C2 vertebral body, pedicle or lateral mass. Immobilization with a rigid collar for 6 weeks was recommended for patients with less severe or more stable injuries. But a cumbersome rigid external orthosis, such as a halo vest or Minerva brace, worn for 2–3 months, results in psychological and physical suffering for the patient.
Furthermore, whatever kind of external immobilization does not guarantee healing in the elderly patients and may be relatively contraindicated in those with cranial fractures, bone deficiency, or sepsis [13, 14].
Indication to OC posterior fusion reduced since new “occiput sparing” posterior fusion techniques appeared. In the same period, we performed 30 cases of C1–C2 or C1–C3 arthrodesis in patients with post-traumatic instability of the upper cervical spine, with a ratio of 3 to 1.
But atlanto-axial fixation exposes the patient at high risk of intraoperative bleeding, and is not always feasible in the elderly. Furthermore, fixation to the atlas is technically impossible when this vertebra is also involved.
A variety of techniques for OCF are currently being used, including rod–wire systems, rigid rod–screw fixation, and occipital hooks and cervical claws.
Polyaxial screws–rod–plate constructs, when feasible, may provide superior biomechanical rigidity and immediate postoperative stability, eliminating the need for prolonged external immobilization [15, 16]. Furthermore, when done in emergency is quicker and easier to perform compared to other constructs and to the C1–C2 posterior fixation techniques. The C0–C1 joint sacrifice in an elderly ankylotic spine does not make a relevant clinical difference in the final functional outcome.
Hard collar in the postoperative is not indicated, especially in elderly, for the high risk of wound occipital dehiscence or infection (20 % in our series).
To obtain optimal screw purchase, several authors recommend placing screws into the suboccipital midline ridge, where the occiput is thickest (up to 14 mm in our series), and we agree with it.
Conclusions
AOD remains the primary indication to OCF. The technique can be successfully applied in UCS unstable injuries of the elderly were C1–C2 fixation or odontoid screwing is not indicated.
Poliaxial screw and plate–rod fixation instrumentation confer the highest osseous fusion rate. The major advantages of this technique are immediate rigid stability and rapidity of the procedure. Early mobilization without external orthosis is highly recommended in the elderly patients, as prolonged periods of bed rest are poorly tolerated and burdened by a high incidence of respiratory complications.
Conflict of interest
None.
References
- 1.Lee SC, Chen JF, Lee ST. Clinical experience with rigid occipitocervical fusion in the management of traumatic upper cervical spinal instability. J Clin Neurosci. 2006;13(2):193–198. doi: 10.1016/j.jocn.2005.03.031. [DOI] [PubMed] [Google Scholar]
- 2.Abumi K, Takada T, Shono Y, Kaneda K, Fujiya M. Posterior occipitocervical reconstruction using cervical pedicle screws and platerod systems. Spine. 1999;24:1425–1434. doi: 10.1097/00007632-199907150-00007. [DOI] [PubMed] [Google Scholar]
- 3.Lu DC, Roeser AC, Mummaneni VP, Mummaneni PV. Nuances of occipitocervical fixation. Neurosurgery. 2010;66(Suppl 3):141–146. doi: 10.1227/01.NEU.0000365744.54102.B9. [DOI] [PubMed] [Google Scholar]
- 4.Wang JC, Mummaneni PV, Haid RW., Jr . Fixation options in the occipitocervical junction. In: Mummaneni PV, Lenke LG, Haid RW Jr, editors. Spinal deformity: a guide to surgical planning and management. St Louis: Quality Medical Publishing; 2008. pp. 223–240. [Google Scholar]
- 5.Papadopoulos SM, Dickman C, Sonntag VKH, Rekate HL, Spetzler RF. Traumatic atlantooccipital dislocation with survival. Neurosurgery. 1991;28:574–579. doi: 10.1227/00006123-199104000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Malik SA, Murphy M, Connolly P, O’Byrne J. Evaluation of morbidity, mortality and outcome following cervical spine injuries in elderly patients. Eur Spine J. 2008;17(4):585–591. doi: 10.1007/s00586-008-0603-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson RM, Hart DL, Simmons EF, Ramsby GR, Southwick WO. Cervical orthosis; a study comparing their effectiveness in restricting cervical motion in normal subjects. J Bone Jt Surg (Am) 1977;59A:332–339. [PubMed] [Google Scholar]
- 8.Lomoschitz FM, Blackmore CC, Mirza SK, Mann FA. Cervical spine injuries in patients 65 years old and older. AJR. 2002;178:573–577. doi: 10.2214/ajr.178.3.1780573. [DOI] [PubMed] [Google Scholar]
- 9.Lieberman IH, Webb JK. Occipito-cervical fusion using posterior titanium plates. Eur Spine J. 1998;7(4):308–312. doi: 10.1007/s005860050080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Finn MA, Bishop FS, Dailey AT. Surgical treatment of occipitocervical instability. Neurosurgery. 2008;63(5):961–968. doi: 10.1227/01.NEU.0000312706.47944.35. [DOI] [PubMed] [Google Scholar]
- 11.Greene KA, Dickman CA, Marciano FF, Drabier J, Hadley MN, Sonntag VKH. Acute axis fractures: analysis of management and outcome in 340 consecutive cases. Spine. 1997;22:1843–1852. doi: 10.1097/00007632-199708150-00009. [DOI] [PubMed] [Google Scholar]
- 12.Hadley MN, Browner C, Sonntag VKH. Miscellaneous fractures of the second cervical vertebra. BHI Q. 1985;1:34–39. [Google Scholar]
- 13.Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffi WG. Halo vest immobilization in the elderly: a death sentence? J Trauma. 2005;59(2):350–356. doi: 10.1097/01.ta.0000174671.07664.7c. [DOI] [PubMed] [Google Scholar]
- 14.Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma. 2006;60(1):199–203. doi: 10.1097/01.ta.0000197426.72261.17. [DOI] [PubMed] [Google Scholar]
- 15.Vaccaro AR, Lim MR, Lee JY. Indications for surgery and stabilization techniques of the occipito-cervical junction. Injury. 2005;36(Suppl 2):B44–B53. doi: 10.1016/j.injury.2005.06.014. [DOI] [PubMed] [Google Scholar]
- 16.Steinmetz MP, Mroz TE, Benzel EC. Craniovertebral junction: biomechanical considerations. Neurosurgery. 2010;66(Suppl 3):7–12. doi: 10.1227/01.NEU.0000366109.85796.42. [DOI] [PubMed] [Google Scholar]