Abstract
Introduction
The surgical treatment of adult scoliosis still presents many points of discussion. Decision-making on the type of treatment is mandatory to evaluate all the possible alternatives to surgery.
Materials and methods
From January 2000 to December 2008, 49 cases of adult degenerative scoliosis and kyphoscoliosis were surgically treated. Thirty-six patients were monitored for a mean of 8 years (5–10). There were 10 males and 26 females, with a mean age of 66 years (55–80). Arthrodesis was carried out using pedicle screws at all levels extending to the sacrum in 30 cases and to the ileum in 4. Laminectomy was performed in 20 cases, radicular liberation in 15, PLIF in 10.
Results
After an average term of 8 years (5–10) we record 8 (23 %) excellent cases, 10 (29 %) good, 12 (34 %) satisfactory, 5 (14 %) bad. The VAS in the pre-operative period had a value of 7 (5–9) passed in the post-operative period of 3 (0–6). 13 reoperations were performed (36 %).
Keywords: Adult scoliosis, Degenerative scoliosis, Surgical treatment, Spine surgery
Introduction
Adult scoliosis is a spinal deformity that emerges after skeletal maturity with an angular value >10° [1]. Scoliotic deformity in adulthood can be divided into three main types [1]. The first is represented by the onset of a spinal curve after 50 years of age due to disc degeneration phenomena and is defined as adult degenerative scoliosis; the second is characterized by an evolution of scoliosis present in adolescence (adult idiopathic scoliosis); the third consists of scoliosis that is secondary to metabolic, arthritic and post-traumatic disorders. It is not always possible to establish a correct differential diagnosis between the two diseases. The patient’s medical history can be indicative but the presence of mild adolescent scoliosis that was unrecognized and untreated cannot always be determined and only the possibility of evaluating a prior radiographic examination taken at a young age and which proves the absence of spinal deviation, can allow us to formulate a clear diagnosis.
Epidemiology and clinical features
The incidence of scoliosis in adulthood varies in the literature between 1.4 and 29.4 % [2–5]. For many years in the literature available, the possibility that one could develop spinal deformities in adulthood or old age took backstage. In 1969, Vanderpool et al. [6] predicted that osteoporosis and osteomalacia could produce vertebral instability to a degree that may induce the onset of a spinal deformity, which in most cases is manifested primarily at the lumbar level. This possibility was confirmed in subsequent studies [3, 7], which concluded that scoliosis could appear de novo [8] in adults with degenerative etiology and in most cases was responsible for worsening low back pain. The presence of vertebra L5, below the bisiliac line, and asymmetric discopathy below L3 were considered by Seo et al. [9] to be predictors of worsening scoliosis while gender, age, osteoporosis, management of scoliosis, the presence of spondylolisthesis, the presence of lateral osteophytes and the index of the vertebral body were not related to its development. It should be considered that a curvature of the spine [3, 10] is only present in 7.5 % of the population suffering with low back pain and that the incidence of low back pain in adults with lumbar scoliosis appears in line with the general population [2, 10, 11] although, in the presence of scoliosis, it appears with greater intensity and persistence even after appropriate therapy [2, 10]. The genesis of lower back pain in adult patients with scoliosis is multifactorial. The causes may include: muscle deficiency, facet osteoarthritis, disc degeneration, imbalance of the trunk in the frontal or sagittal plane (kyphosis or Flat back), vertebral slip that may be lateral, posterior (retrolisthesis) or anterior (spondylolisthesis). Lower back pain is often associated with radiating pain in the lower limbs with or without neurological deficits or secondary neurogenic claudication compressing or stretching of the nerve roots or stenosis of the lumbar spinal canal.
The possibility that the extent of radiographic alterations could be related to the severity of the lower back pain has been studied by Schwab et al. [12]. These authors concluded that the presence of a lateral subluxation, thoracolumbar kyphosis and the obliquity of the vertebral units were directly correlated with the intensity of pain. While the angular value of the scoliotic curve and the number of vertebrae affected by the curve showed no significant correlations with the pain.
Treatment
The treatment of adult scoliosis is a continuous challenge even for expert spinal surgeons and in the choice of treatment all the possible alternatives to surgical intervention should be carefully evaluated [13]. According to Bridwell [14], deformity is the main concern of young adults while in older patients the problems of disability and pain are most noted by patients. In patients over 50 years of age, there are numerous issues to address. We are often faced with generally associated diseases that may affect the choice of treatment and affect the results; these are often deformities that are not serious but rigid with ankylosis of joints, anterior lateral osteophytosis of the vertebral units, lateral subluxation, anterior vertebral listhesis and stenosis of the spinal canal. The surgical option for these patients should be taken when there is evidence of clear progression of the deformity with imbalance of the sagittal profile, in the presence of persistent and debilitating pain, which is untreatable with physical medical therapy or external supports, in the presence of radiation to the lower limbs with or without neurological deficits and neurogenic claudication. From the data in the literature, it can be deduced that surgical treatment is burdened with a high percentage of general and mechanical complications [15–18]. Therefore, a decision for surgical treatment must be taken after careful consideration of all possible precautionary, therapeutic treatment options and a valuation of all the general and local conditions that may cause an increased risk of complications [13]. In adult patients, the goals of surgery are: to reach a satisfactory correction of the deformity, mainly on the sagittal plane; a solid fusion that allows the reduction of the incidence of mechanical failures and reoperations; the reduction of pain that allows an improvement in quality of life; the decompression of the neural structures foreseeing the onset of neurological deficits and the prevention of all general diseases secondary to inactivity and being bedridden [10]. Posterior surgical access using pedicle screws permits, in most cases, the stable correction of the deformity, also by using posterior osteotomy (Fig. 1) and the mobilization of the curves. The possibility of combining sublaminar fixing with Universal Clamps permits further stability, in particular in osteoporotic patients in whom the possibility of mobilization appears high. The extension of arthrodesis to the sacrum is a field of open discussion. While on one hand the fusion of the sacrum promotes greater stability and the possibility of better corrections, it is also burdened with a high proportion of mechanical complications and reoperations. Where possible, to reduce the incidence of the above, one should limit the upward extension of arthrodesis [19] and perform L5-S1 arthrodesis with an anterior accessory phase or the use, via posterolateral access, of an anterior support through the same access [20]. This results in prolonged surgical time, more bleeding, more risk of lesions to the nervous structures, increased incidence of infection and related complications.
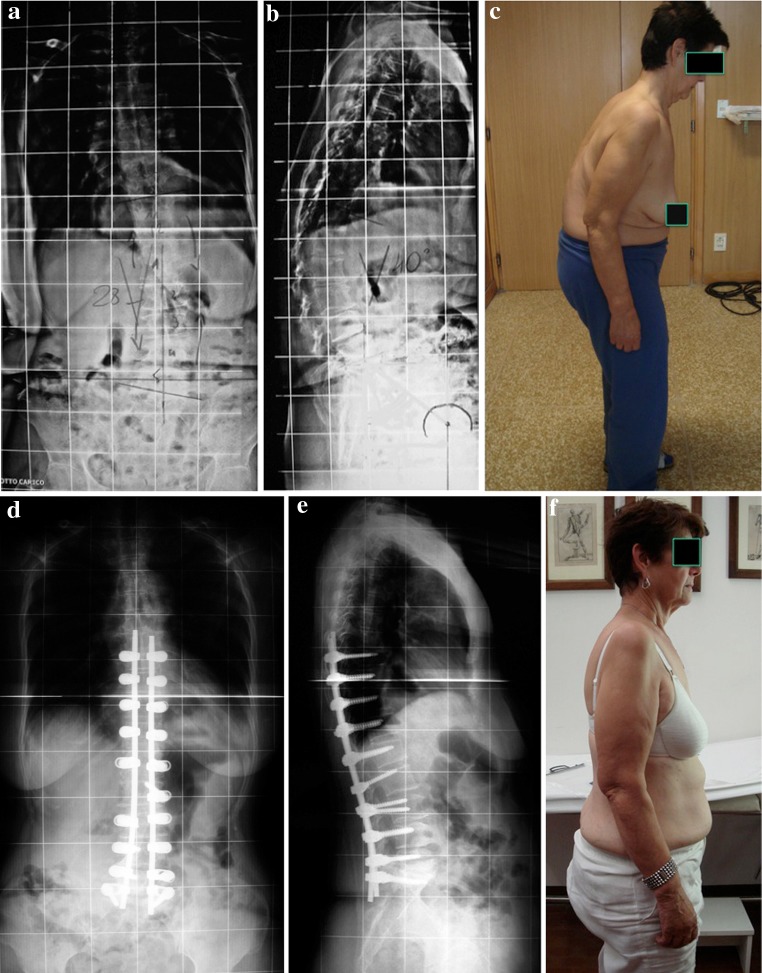
Fig. 1.
a, b 65-Year-old patient with an adult degenerative left scoliosis and kyphosis. c Severe back pain with sagittal imbalance. d, e Treatment was with instrumented posterior kyphoscoliosis correction and fusion T10-S1. At 5 years follow-up showed solid fusion. f Clinical result with good sagittal profile
Materials and methods
From January 2000 to December 2008, 49 cases of adult degenerative scoliosis and kyphoscoliosis were surgically treated. Thirty-six patients were monitored for a mean of 8 years (5–10) (5 died of natural causes and 8 were lost in follow-up). There were 10 males and 26 females, with a mean age of 66 years (55–80). Ten patients were over 70 years of age (28 %). In all there was scoliosis with an average angular value of 27° (10°–50°), lumbar lordosis with an average angular value of 20° (0°–32°); in 12 patients there was associated thoracolumbar kyphosis with an average angular value of 22° (15–40). In 18 (50 %) cases there was trunk misalignment; in ten with global coronal imbalance C7PL-CSVL > 8 cm (5–20), and in eight sagittal imbalance with C7PL cm +6 (+4/+15). In 15 cases there was degenerative spondylolisthesis at L4-L5 and in 2 at L3-L4. In all cases there was lower back pain resistant to medical therapies and to physiotherapy. All cases had worn an orthopaedic brace in the pre-operative period with improvement of pain in the spine. In 15 there was an associated radiating pain in the lower limbs (sciatica in 10 and cruralgia in 5), while in 20 there was neurogenic claudication and in 20 a peripheral mono or periradicular neurological deficit. In all cases arthrodesis was carried out using pedicle screws at all levels extending to the sacrum in 30 cases and the ileum in 4. There was associated central decompressive laminectomy in 20 cases with stenosis of the lumbar spine and radicular liberation in 15 cases of sciatica; in the 10 cases in which there was degenerative spondylolisthesis, which appeared unstable in the dynamic X-ray projections, intersomatic arthrodesis was performed via posterolateral (PLIF) access with bilateral cage. A minimum of five to a maximum of ten vertebrae were instrumented and an average of 16 screws were implanted (10–20) per patient. In the post-operative, period patients were admitted to intensive care for a day, they would start the static period on day 3–4 and the next day were walking assisted by an orthopaedic brace which was worn for about 2–3 months. Patients were discharged after 8–10 days. For the prevention of deep vein thrombosis all patients wore elasticated stockings combined with anticoagulant therapy (heparin, low molecular weight). Currently anticoagulant therapy is given only to patients who have risk factors (varicose veins, obesity, diabetes) or with a history of venous diseases. In no case it was necessary to place a vena cava filter.
Results
The clinical results were evaluated according to White et al. [21], and using the visual analogue scale VAS. The degree of pain, use of pain medication, the ability to walk and any functional impairment were evaluated. After an average term of 8 years (5–10), we record 8 (23 %) excellent cases, 10 (29 %) good, 12 (34 %) satisfactory, 5 (14 %) bad. The VAS in the pre-operative period had a value of 7(5–9) passed in the post-operative period of 2(0–5). Scoliosis was corrected to a mean value of 12° (0°–27°). The lumbar lordosis had an average value of 32° (15°–45°). The coronal balance was corrected in all cases with the C7PL–CVLS = 1 cm (0–3) with the recovery of a good sagittal profile C7PL 0 (−2/+3). The duration of surgery was on average 240 min, from a minimum of 150 to a maximum of 300 min in cases in which an intersomatic arthrodesis was performed. Blood loss was 340 ml (200–700). Among other complications there were three cases of wound healing pain with revision surgery, three cases of dural lesions complicated in one case by CSF fistula that required reoperation resulting in complete recovery and two cases of screw misplacement that required review of the implant and removal of the screw. Mobilization of sacral screws occurred in five (16.5 %) cases; three of which required lengthening the ileum. In two cases of persistent pain in the absence of mobilization of the instrument, it was removed, resulting in improved pain symptoms in only one case. In two cases of synthesis material rupturing, with pseudoarthrosis, a posterior re-examination and an anterior arthrodesis phase was carried out, with evidence in one case, 2 years after surgery, of a further failure of the instrumentation. In three cases, proximal junctional syndrome was noted, which required lengthening the instrumentation in two cases. In total 13 reoperations were performed (36 %).
Conclusions
In suggesting surgical treatment, all the possible alternatives to conservative treatment must be carefully evaluated, understanding that the risk of complications or reoperation is much higher compared to the same surgery in adolescent patients. The objectives that it aims to achieve are: improvement in quality of life through the reduction of pain; decompression of the neural structures; the correction of anterior and lateral slip, although complete resolution of pain is difficult to achieve in that it involves patients whose spinal arthritic degeneration in the zones adjacent to the instrumentation plays a decisive role in the persistence of pain. Posterior surgical treatment with pedicle synthesis, combined with osteotomy and mobilization of the joints allows satisfactory corrections to be obtained in the case of extension of arthrodesis to the sacrum, intersomatic arthrodesis L5-S1 or lengthening the ileum can reduce the incidence of mechanical complications but requires an additional phase with prolongation of surgical episodes, bleeding and the possibility of the symptomatology transferring to the hips [22]. Kim, Bridwell, Lenke et al. [20] reported the results of a study of 144 cases of arthrodesis extended to the sacrum in patients with adult scoliosis and showed, after an average of 27 months, pseudoarthrosis in 31 % of the 16 cases treated with posterior arthrodesis alone and in 23 % of the 128 cases treated with anterior and posterior dual access. While Cho, Suk et al. [23] reported that there were no differences in the incidence of complications between patients submitted to syntheses extended to the sacrum and those extended to L5. Our current approach is to avoid, in most cases, the synthesis of the sacrum that appears, in our experience, more burdened by mechanical complications (16.5 %), reserving the option to extend arthrodesis to the sacrum in case of arthrodesis extended to L5. Surgical treatment of adult scoliosis is a challenge even for experienced spinal surgeons, the increase in life expectancy will lead to an increase in spinal pathologies with evermore pressing requests on the part of patients for an improvement in quality of life and only a decision for correct surgical treatment and an appropriate surgical technique can reduce the incidence of complications.
Conflict of interest
None.
References
- 1.Aebi M. The adult scoliosis. Eur Spine J. 2005;14:92548. doi: 10.1007/s00586-005-1053-9. [DOI] [PubMed] [Google Scholar]
- 2.Kostuick JP, Bentivoglio J. The incidence of low-back pain in adult scoliosis. Spine. 1981;6:268–273. doi: 10.1097/00007632-198105000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Perennou D, Marcelli C, Héricson C, Simon L. Adult lumbar scoliosis. Epidemiological aspects in a low back pain population. Spine. 1994;19:123–128. doi: 10.1097/00007632-199401001-00001. [DOI] [PubMed] [Google Scholar]
- 4.Jimbo S, Kobayashi T, Aono K, Atsuta Y, Matsumo T. Epidemiology of degenerative lumbar scoliosis: community based cohort study. Spine. 2012;37:1763–1770. doi: 10.1097/BRS.0b013e3182575eaa. [DOI] [PubMed] [Google Scholar]
- 5.Robin GC, Span Y, Steinberg R, Makin M, Menczel J. Scoliosis in elderly: a follow-up study. Spine. 1982;7:355–359. doi: 10.1097/00007632-198207000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Vanderpool DW, James JI, Wynne-Davies R. Scoliosis in elderly. J Bone Joint Surg Am. 1969;51:446–455. [PubMed] [Google Scholar]
- 7.Benner B, Ehni G. Degenerative lumbar scoliosis. Spine. 1979;4:548–552. doi: 10.1097/00007632-197911000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Briard J, Jeugou L, Cauchoix D. Adult lumbar scoliosis. Spine. 1979;4:526–532. doi: 10.1097/00007632-197911000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Seo JY, Hwang TH, Kim KW, Kim YH. Risk of progression of degenerative lumbar scoliosis. J Neurosurg Spine. 2011;15:558–566. doi: 10.3171/2011.6.SPINE10929. [DOI] [PubMed] [Google Scholar]
- 10.Bradford DS, Tay BK, Hu SS. Adult scoliosis: surgical indications. Operative management, complications and outcome. Spine. 1999;24:2617–2629. doi: 10.1097/00007632-199912150-00009. [DOI] [PubMed] [Google Scholar]
- 11.Jackson RP, Simmons EH, Stripinis D. Incidence and severity of back pain in adult idiopathic scoliosis. Spine. 1983;8:749–756. doi: 10.1097/00007632-198310000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy JP, Pagala M. Adult scoliosis. A quantitative radiographic and clinical analysis. Spine. 2002;27:387–392. doi: 10.1097/00007632-200202150-00012. [DOI] [PubMed] [Google Scholar]
- 13.Glassman SD, Schwab FJ, Bridwell Kh, Ondra SL, Breven S, Lenke LG. The selection of operative versus nonoperative treatment in patients with adult scoliosis. Spine. 2007;32:93–97. doi: 10.1097/01.brs.0000251022.18847.77. [DOI] [PubMed] [Google Scholar]
- 14.Bridwell KH, Berven S, Eduards CII, et al. The problems and limitations of applying evidence-based medicine to primary surgical treatment of adult spinal deformity. Spine. 2007;32:S135–S139. doi: 10.1097/BRS.0b013e3181453e22. [DOI] [PubMed] [Google Scholar]
- 15.Daubs KD, Lenke LG, Chen G, Stobbs G, Bridwell KH. Adult spinal deformity surgery. Complications and outcomes in patients over age 60. Spine. 2007;32:2238–2244. doi: 10.1097/BRS.0b013e31814cf24a. [DOI] [PubMed] [Google Scholar]
- 16.Cho KJ, Suk S-II, Park SR, Kim JH, Kim SS, Choi WK, Lee KY, Lee SR. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine. 2007;32:2232–2237. doi: 10.1097/BRS.0b013e31814b2d3c. [DOI] [PubMed] [Google Scholar]
- 17.Charosky S, Guigui P, Blamoutier A, Roussouly P, Chopin D, Study Group on Scoliosis Cpmplications and risk factors of primary adult scoliosis surgery: a multicentre study of 306 patients. Spine. 2012;37:693–700. doi: 10.1097/BRS.0b013e31822ff5c1. [DOI] [PubMed] [Google Scholar]
- 18.Sansur CA, Smith JS, Coe JD, Glassman SD, Breven SH, Polly DW, Jr, Perra JH, Boachie-Adjei O, Schaffrey CL. Scoliosi research society morbility and mortality of adult scoliosis surgery. Spine. 2011;36:E593–E597. doi: 10.1097/BRS.0b013e3182059bfd. [DOI] [PubMed] [Google Scholar]
- 19.O’Shaughnessy BA, Bridwell KH, Lenke LG, Cho W, Baldus C, Chang MS, Auerbach JD, Crawford CH. Does a long fusion “T3-sacrum” ported a worse outcome than fusion “T10-sacrum” in primary surgery for adult scoliosis? Spine. 2012;37:884–890. doi: 10.1097/BRS.0b013e3182376414. [DOI] [PubMed] [Google Scholar]
- 20.Kim YJ, Bridewll KH, Lenke LG, Rhim SR, Chen G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of the 144 cases. Spine. 2006;31:2329–2336. doi: 10.1097/01.brs.0000238968.82799.d9. [DOI] [PubMed] [Google Scholar]
- 21.White AH, von Rogov P, Zucherman J, Heiden D. Lumbar laminectomy for herniated disc: a prospective controlled comparison with internal fusion. Spine. 1987;12:3057. doi: 10.1097/00007632-198704000-00021. [DOI] [PubMed] [Google Scholar]
- 22.O’shaughnessy BA, Lenke LG, Bridwell KH, Cho W, Zebala LP, Chang MS, Auerbach JD, Crawford CH, Koester LA. Should symptomatic iliac screw be electively removed in adult spinal deformity patients fused to the sacrum? Spine. 2012;37:1175–1181. doi: 10.1097/BRS.0b013e3182426970. [DOI] [PubMed] [Google Scholar]
- 23.Cho KJ, Suk S-II, Park SR, Kim JH, Choi SW, Yoon YH, Won MH. Arthrodesis to L5 versus S1 in long instrumentation and fusion for degenerative scoliosis. Eur Spine J. 2009;18:531–537. doi: 10.1007/s00586-009-0883-2. [DOI] [PMC free article] [PubMed] [Google Scholar]