Abstract
Introduction
Sagittal imbalance is an important risk factor for spinal disability, pain and loss of health related quality of life. Its correction has a positive impact on these outcomes. Still, it is a very aggressive surgery, with a high revision rate. The aim of this study is to analyze the most important causes of failure of surgery for correction of sagittal imbalance.
Design and methods
In this retrospective observational cohort study twelve patients who previously underwent surgery for sagittal imbalance correction were revised in the period 2009–10. We analyzed angular parameters of sagittal balance before and after primary surgery, type of instrumentation, modality of fusion, implant density, instrumented levels, modality of failure, time from first surgery and angular parameters after revision.
Results and conclusion
Causes of failure were insufficient correction, junctional kyphosis, screw loosening and pseudoarthrosis with rod breakage. In every case, patients presented a new onset or a worsening of sagittal imbalance and pain.
Keywords: Sagittal imbalance, Failure, Rod breakage, Pelvic parameters
Introduction
Sagittal imbalance is a multifactorial pathology that causes back pain and neurological involvement, with a significative decrease in patient’s quality of life. The causes of sagittal imbalance are many, but most commonly these include post-traumatic kyphosis, iatrogenic flat back syndrome, post-laminectomy kyphosis, degenerative lumbar kyphosis, and ankylosing spondylitis [1–3]. All these factors lead to a forward bending of the spine, with a C7 plumbline that falls in front of the hips. A patient with an initial sagittal imbalance tries to maintain C7 plumbline on the posterosuperior corner of S1 endplate balancing the spine with different mechanisms: thoracic spine hypokyphosis and vertebral retrolisthesis, pelvic retroversion, knee flexion. Each of these compensational behaviors can produce pain in mid- to long-term; nerve compression and muscle strain are the most common causes of pain in imbalanced subjects, and positive sagittal balance has been identified as the radiographic parameter most highly correlated with adverse health status outcomes [4]. The surgical treatment of sagittal imbalance is complex and demanding. Long instrumentations and vertebral osteotomies are frequently needed to restore balance of the spine. Different types of vertebral osteotomies can be performed: these include Smith–Petersen osteotomy (SPO), Ponte osteotomy (PO), Pedicle Subtraction Osteotomy (PSO), and Posterior Vertebral Column resection (PVCR). The technique used to correct a sagittal imbalance depends on factors such as the severity and the flexibility of the deformity, and on the shape of the kyphosis [5]. However, the main factor that influences the choice of the vertebral wedge osteotomy is the entity of the sagittal imbalance. These different techniques show a different magnitude of correction, having Ponte and Smith–Petersen osteotomies a potential of 5°–10° of correction per osteotomy site, while PSO can reach a maximum of 35° of lordosis restoration. Blood loss during surgery is generally high, representing a threat to patient’s life. A high rate of complications can be anticipated, especially when PSO or PVCR are performed, reaching short-term rates of nearly 30 % [7] and different patterns of long-term failures and complications [8]. However, sagittal imbalance correction with vertebral osteotomies is a surgical act that improves patient’s quality of life and symptoms [6].
The aim of this study is to evaluate the surgical failure patterns to underline the key problems of this very demanding surgery.
Materials and methods
In this retrospective study we analyzed 12 patients that underwent a surgical revision for sagittal imbalance in our Division between 2009 and 2010, with a total of 14 surgical procedures. We evaluated the mean age of the patients and the time between the first and revision surgery, the area of arthrodesis, the implant density, the use of cross-links, S1 and pelvic stabilization, pelvic parameters, and type of failure.
Results
The mean age of our population was of 61.5 years (range 40–76). All the patients were females (100 %), and the mean time between the first and the revision surgery is 16.5 months (6–50 months). In mean we treated an area of 10.8 vertebrae (2–15), with 7.8 instrumented vertebrae per patient (2–11). The implant density (the ratio between the number of vertebrae included in the fusion area and the number of instrumented vertebrae) was 0.72 (0.6–1). We used a double cross-link in 13 out of 14 cases (92.9 %). The distal fixation reached the sacrum in 12 cases (85.7 %). In 2 cases iliac screws were implanted to augment the distal fixation (14.3 %). In 4 cases a L5–S1 interbody fusion using cages was performed (28.6 %). We then analyzed the different patterns of failure on the full spine X-rays of patients enrolled in the study. We observed 7 cases of pseudoarthrosis with rod breakage (Figs. 1d, 3a) (50 %)—of these, 3 rods were 5.5 mm in diameter, 4 rods were 6 mm. In addition, 4 of these patients had a Pedicle Subtraction Osteotomy (PSO) during the first surgery, while on three of them no PSO was performed. In 5 cases sagittal imbalance was still present after the primary surgery (35.7 %); three of these patients did not undergo a vertebral osteotomy during the first surgery. We finally observed one case (7.1 %) of proximal pullout/junctional kyphosis (Fig. 2b) and one case (7.1 %) of distal pullout/junctional kyphosis (Fig. 3a).
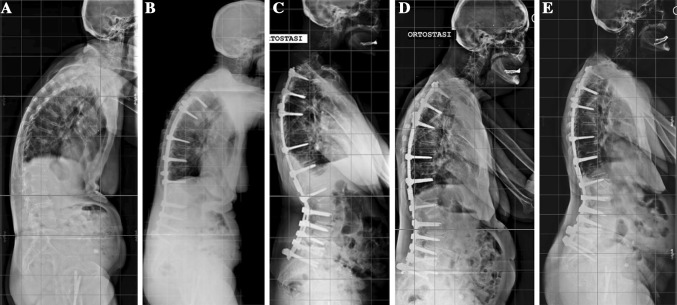
Fig. 1.
a Preoperative lateral full-spine standing films. Sagittal imbalance with anterior translation of C7 plumbline and increased pelvic tilt. b Fusion T3-Sacrum—insufficient correction of lumbar hypolordosis after fusion T2 to S1 causes persistent anterior C7 plumbline and increased pelvic tilt. c After revision (Fusion T2-Pelvis and L2 PSO) sagittal alignment is restored. Notice intact discs around the L2 osteotomy. 6 mm rods are implanted. d Rod Breakage at 6 months postop. Fracture at L1 resulting in loss of correction. e Rod exchange and anterior fusion around the PSO (XLIF L1–L2 and L2–L3) restore sagittal imbalance and continuity of the anterior column and promote final healing
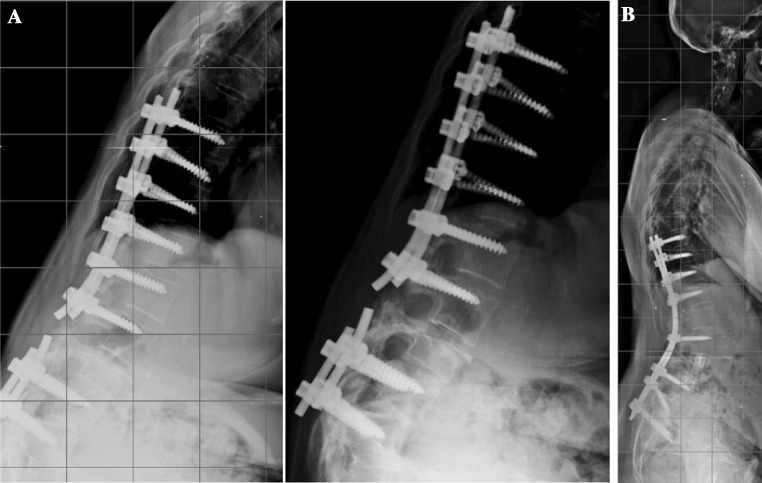
Fig. 3.
a Combined failure after insufficient correction of sagittal misaligment (improper distal foundation without pelvic fixation and inadequate lordosis). Failure with pullout at S1 and rod breakage. b Revision surgery with extension of fixation to pelvis, multiple SPOs to increase lordosis at L2–L3–L4 and anterior column reconstruction with XLIF at L3–L4–L5 and PLIF at L5–S1
Fig. 2.
a Following short instrumentation and PSO to increase lumbar lordosis (planned lordosis was obtained after first surgery), loss of correction with proximal junctional fracture and kyphosis resulting in axial pain and new imbalance. b Revision surgery included extension to T2, and correction of proximal junctional kyphosis with an excellent clinical outcome
Our last analysis concerned spinopelvic parameters and sagittal balance after the first surgery. This cohort of patients undergoing revision surgery for failure after sagittal realignment had a mean Pelvic Tilt of 28° (range 9–46°) and a mean SVA of 11.8 cm (range 3–30 cm). After the first surgery, 11 patients needing revision (78.6 %) had a Pelvic Tilt higher than 20°, and 11 patients (78.6 %) had an SVA higher than 5 cm (considered as the limit value). All 12 patients had insufficient correction (SVA higher than 5 cm or Pelvic Tilt higher than 20°).
Discussion
Sagittal imbalance correction needs the execution of a high-demanding surgery to obtain a correct restoration of an adequate balance of the spine. This group of surgical techniques is associated with a high ratio of complications, with frequent postoperative failures and subsequent loss of correction and pain. The literature related to complications, failures and revisions after surgery for sagittal imbalance is scarce. The authors feel that failure rate is probably underestimated. In our analysis we found different factors that can influence the outcome of our surgery; all of these should be taken in count when performing a surgical procedure for correction of sagittal imbalance. Hopefully, considering these factors could reduce the failure rate.
Insufficient correction
We observed an insufficient sagittal correction in all the enrolled patients (Figs. 1b, 2b, 3a). This suggests that the final balance obtained with surgery is a key factor in determining the success of the procedure. Sagittal balance has been evaluated with two parameters. The first was Pelvic Tilt, a positional parameter that refers to the orientation of the pelvis. Pelvic retroversion is a known method that imbalanced patients use to bring C7-plumbline on the sacrum; the posterior rotation of the whole pelvis is an efficient way that the patients use to compensate their imbalance. Obviously retroversion of the pelvis creates an increase of the Pelvic Tilt value. However, the different mechanisms of compensation of sagittal imbalance are not sufficient to free patients from pain. Muscular fatigue causes pain in a long-term muscular work, and the progression of sagittal imbalance can lead to a mobilization or a breakage of the implant. The second parameter that had been considered in the evaluation of postoperative sagittal balance was the Sagittal Vertical Axis, the distance of C7-plumbline from the posterosuperior corner of S1. In balanced patients this value must be under 5 cm. In 11 patients out of 14 (78.6 %) SVA was greater than physiologic values.
Both anterior C7 plumbline and increased pelvic tilt express a failure to align posteriorly the gravity line (the vertical line through the body center of mass of the patient) as the C7 plumbline is a gross estimator of the gravity line that runs in normal subjects close posterior to their gravity line. A patient with an anteriorly displaced gravity line has, as a consequence, increased mechanical stress on the posterior implant: the translation of the mass anteriorly causes an increase in the moment arm of the trunk mass with respect to the rod, increasing the cyclic bending stress on it; additionally, tensile forces (that are worst resisted by the rods than neutral or compression forces) are increased posteriorly. Tensile forces through the posterior graft cause bone resorption and reduce the chance of obtaining solid fusion.
A practical consequence is the need to perform an adequate preoperative planning, with calculation of the site and amount of correction necessary to restore the position of the gravity line related to the spine. It is important to calculate precisely the amount of correction needed, and calculation methods had been proposed by different authors [9–11].
Furthermore, the authors strongly suggest intraoperative measurement of the amount of correction obtained before final tightening of the implants. In our experience, most cases need some extra manipulation to obtain the desired correction.
Posterior column discontinuity in PSO
The Pedicle Subtraction Osteotomy (PSO) is a very effective technique to increase lordosis. With this wedge osteotomy it is possible to obtain a correction of as much as 35° per osteotomy site. Though it is a very powerful option to improve lumbar lordosis, PSO shows some limits. One of these is the wide resection of the posterior bony elements needed to perform the osteotomy. This often results in a lack of continuity of the posterior elements. This gap in the posterior column after the correction can cause a failure of the posterolateral fusion process, because insufficient bony bed can be available to incorporate bone graft at the level of osteotomy (Figs. 1e, 2c, 3b). An additional factor of instability is the combination around the osteotomy level of lack of continuity of posterior elements with intact (flexible) discs around. This represents an scenario of huge instability and concentration of mechanical stress, with stiff and long constructs above and below the osteotomy site and an unprotected area where the rods take most of the mechanical stress at the osteotomy level. Furthermore, after a PSO the osteotomized vertebral level cannot be instrumented with pedicle screws, sublaminar wires or hooks, bringing another factor of instability. If pseudoarthrosis occurs, the rods will inevitably break because of cyclic load and fatigue stress (Figs. 1d, 2c, 3a).
Rod diameter
The rods we use in the degenerative pathology have been originally designed for adolescent deformity surgery. The 5.5 mm diameter rods provide an adequate resistance to correction maneuvers during surgery, and can be easily bent in lordosis to connect the screws after PSO. The 6 mm diameter rods have a greater stiffness and resistance to breakage. As shown in this retrospective analysis, the increased stiffness is insufficient when fusion is not obtained. The continuous stress on the rods in case of postoperative unbalanced spine or in case of pseudoarthrosis leads in any case to rod breakage. We observed in our series 7 cases of pseudoarthrosis with rod breakage (Figs. 1d, 2c, 3a) (50 %)—of these, 3 rods were 5.5 mm diameter, 4 rods were 6 mm. This underlines how the instrumentation will fail if balance and fusion are not obtained after surgery. Six millimeter rods are however preferred in this kind of surgery, because of their greater resistance to fatigue stresses. Probably a specific instrumentation for degenerative spine surgery, with new materials and geometry could improve the resistance of the rods, leading to a greater resistance to stresses.
Rod bending
In order to engage the rods on the screws and provide adequate correction, the surgeon frequently needs to perform an aggressive bending of the rods at the level of the osteotomy from straight rods. A case of PSO at the L4 level (our most frequent preference currently to reproduce the physiological curvature of the lumbar spine, that concentrates most of the lordosis between L4 and S1) typically requires bending the rod nearly 90° in a short 4-cm segment. A short radius bending of the rod causes compressive stress in the concavity and distractive stress in the convexity, which can cause stress risers to form. French rod benders frequently fail to provide sufficient bending, and lever benders are frequently necessary. Lever benders create small marks in the rods and these act as stress risers. The combination of a short radius bending, lever marks, distractive forces, increased flexion moment arm on the rod and reduced stiffness of the spine at the level of the osteotomy is probably the cause of the high observed incidence of rod breakage.
Insufficient distal foundation
Twelve of 14 revisions were done in cases with previous surgery extending to S1. Only 2 of these cases (14.3 %) had iliac fixation. Four additional cases had interbody instrumentation at L5–S1. Our current strategy includes pelvic instrumentation in all cases of sagittal imbalance correction with surgery extending to S1. This increases the lever on the pelvis and allows for more aggressive correction of the loss of lordosis, without increasing the risk of acute intraoperative or delayed failure of the fixation at S1. The different orientation in the axial plane of the divergent pelvic screws with respect to the S1 convergent screws is the key in increasing pullout resistance of the construct.
Conclusions
Correction of sagittal imbalance in adults requires demanding surgery with unique challenges and differ from problems encountered in adolescent idiopathic scoliosis. Long fusions, often associated with vertebral osteotomies, are needed to restore an adequate alignment of the spine. Many factors can have a role in the final outcomes and can influence the risk of failure, with need of revision surgery. Adequate preoperative planning and calculation of the amount of correction needed is of paramount importance, as is intraoperative measurement to assure the final achievement of planning. The choice of rod diameter and rod alloy and a careful contouring, avoiding the creation of stress risers, restoration of bone continuity both in the posterior and anterior column, solid distal foundation with iliac screws in fusions extending to the sacrum, are suggested to increase the chance of success. In future, design of specific implants for this pathology can provide increased stability and fusion rate.
Conflict of interest
None.
References
- 1.Booth KC, Bridwell KH, Lenke LG, Baldus CR, Blanke KM. Complications and predictive factors for the successful treatment of flatback deformity (fixed sagittal imbalance) Spine(Phila Pa 1976) 1999;24:1712–1720. doi: 10.1097/00007632-199908150-00013. [DOI] [PubMed] [Google Scholar]
- 2.Casey MP, Asher MA, Jacobs RR, Orrick JM. The effect of Harrington rod contouring on lumbar lordosis. Spine(Phila Pa 1976) 1987;12:750–753. doi: 10.1097/00007632-198710000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Farcy JP, Schwab FJ. Management of flatback and related kyphotic decompensation syndromes. Spine(Phila Pa 1976) 1997;22:2452–2457. doi: 10.1097/00007632-199710150-00025. [DOI] [PubMed] [Google Scholar]
- 4.Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine(Phila Pa 1976) 2005;30:682–688. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 5.Bridwell KH. Decision making regarding Smith–Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine(Phila Pa 1976) 2006;31(19 Suppl):S171–S178. doi: 10.1097/01.brs.0000231963.72810.38. [DOI] [PubMed] [Google Scholar]
- 6.Kim KT, Lee SH, Suk KS, Lee JH, Jeong BO. Outcome of pedicle subtraction osteotomies for fixed sagittal imbalance of multiple etiologies. A retrospective review of 140 patients. Spine(Phila Pa 1976) 2012;37(19):1667–1675. doi: 10.1097/BRS.0b013e3182552fd0. [DOI] [PubMed] [Google Scholar]
- 7.Smith JS, Sansur CA, Donaldson WF, III, Perra JH, Mudiyam R, Choma TJ, Zeller RD, Knapp DR, Noordeen HH, Berven SH, Goytan MJ, Boachie-Adjei O, Shaffrey CI. Short-term morbidity and mortality associated with correction of thoracolumbar fixed sagittal plane deformity. A report from the Scoliosis Research Society morbidity and mortality committee. Spine. 2011;36(12):958–964. doi: 10.1097/BRS.0b013e3181eabb26. [DOI] [PubMed] [Google Scholar]
- 8.Hyun SJ, Rhim SC. Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients: a long-term follow-up data. Korean Neurosurg Soc. 2010;47:95–101. doi: 10.3340/jkns.2010.47.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lamartina C, Berjano P, Petruzzi M, Sinigaglia A, Casero G, Cecchinato R, Damilano M, Bassani R. Criteria to restore the sagittal balance in deformity and degenerative spondylolisthesis. Eur Spine J. 2012;21(Suppl 1):S27–S31. doi: 10.1007/s00586-012-2236-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Le Huec JC, Leijssen P, Duarte M, Aunoble S. Thoracolumbar imbalance analysis for osteotomy planification using a new method: FBI technique. Eur Spine J. 2011;20(Suppl 5):S669–S680. doi: 10.1007/s00586-011-1935-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang PB, Ondra SL. A method for calculating the exact angle required during Pedicle Subtraction Osteotomy for fixed sagittal deformity: comparison with the trigonometric method. Neurosurgery. 2006;59(4 Suppl 2):ONS458–ONS463. doi: 10.1227/01.NEU.0000232628.46247.15. [DOI] [PubMed] [Google Scholar]