Abstract
Background
In the Norwegian prospective study on Legg-Calvé-Perthes disease (LCPD), we found varus femoral osteotomy gave better femoral head sphericity at a mean of 5 years postoperative than physiotherapy in children older than 6.0 years at diagnosis with femoral head necrosis of more than 50%. That study did not include separate analyses for hips with 100% necrosis and those with a percentage of necrosis between 50% and 100%.
Questions/purposes
We asked whether (1) femoral osteotomy improves femoral head sphericity at followup in all patients with more than 50% femoral head necrosis or in selected groups only and (2) there is a critical age between 6.0 and 10.0 years over which femoral osteotomy does not improve the prognosis.
Methods
We treated 70 patients with unilateral LCPD, age at diagnosis of more than 6.0 years, and femoral head necrosis of more than 50% with varus femoral osteotomy between 1996 and 2000. We classified necrosis using the Catterall classification. We established a control group of 51 similar children who received physiotherapy. At the 5-year followup visit, the hips were graded according to femoral head shape: spherical, ovoid, or flat.
Results
At 5-year followup, there was no difference between the treatment groups in radiographic outcome in Catterall Group 3 hips. In Catterall Group 4 hips, femoral head sphericity was better in the osteotomy group, with flat femoral heads in 14% compared to 75% after physiotherapy. The same trend toward better head sphericity occurred when the lateral pillar classification was used.
Conclusions
In children aged 6.0 to 10.0 years, in whom the whole femoral head is affected, femoral head sphericity 5 years after femoral osteotomy was better than that after physiotherapy.
Level of Evidence
Level II, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Short- to intermediate-term treatment outcome in Legg-Calvé-Perthes disease (LCPD) is frequently gauged by the degree of femoral head sphericity after healing. Sphericity varies according to well-known prognostic factors such as age and degree to which the femoral head is affected [2, 8, 14]. Thus, studies comparing different treatment methods are reliable only in groups with similar prognostic factors. To compare treatment methods, prospective studies including a large number of patients are needed. Even with many patients, some subgroups can be too small for meaningful analysis. So far, only two prospective multicenter studies have been published, one from the United States in 2004 [7] and one from Norway in 2008 [17]. In the Norwegian study, the 5-year degree of sphericity of the femoral head, in patients older than 6.0 years at diagnosis with more than 50% femoral head necrosis, was better in children treated with femoral varus osteotomy than in those treated with physiotherapy or abduction orthosis [17]. However, that study did not include separate analyses for hips with 100% necrosis and those with a percentage of necrosis between 50% and 100%.
The severity of LCPD can also be classified by the degree of reduction of the lateral bone pillar of the femoral head during the initial phases of the disease [8]. Depending on this classification and age, certain differences in femoral head sphericity between surgical and nonsurgical treatment were reported [7], but further studies using this classification are required before reliable conclusions can be drawn.
Although the prognosis in children older than 6.0 years at diagnosis is worse than in younger children, there is no agreement regarding the relationship between prognosis and age in the age group 6.0 to 10.0 years [1, 7, 15].
The rationale for surgical treatment in LCPD is to improve femoral head coverage (FHC) and thus containment. There is, however, little evidence concerning the development of FHC according to different methods of treatment.
Using data from our multicenter study [17], we addressed the following questions: (1) Does varus femoral osteotomy improve sphericity of the femoral head in all patients with more than 50% femoral head necrosis or in selected groups only? (2) Does osteotomy improve sphericity of the femoral head in patients with less and/or more than 50% reduction of the lateral pillar? (3) Is there any difference between osteotomy and physiotherapy in containment of the affected femoral epiphysis? And (4) are there any differences between osteotomy and physiotherapy in clinical parameters at followup?
Patients and Methods
During the 5-year period between 1996 and 2000, a nationwide prospective study on LCPD in Norway was performed. All 28 hospitals with pediatric orthopaedic service reported all new incidents of LCPD. We obtained informed consent from all parents, and the study was approved by The Norwegian Data Inspectorate and The Norwegian Directorate of Health and Social Affairs. A total of 425 patients were registered, of which 368 had unilateral LCPD.
To classify the amount of femoral head necrosis, the Catterall [2] classification was used. In Catterall Group 3, more than 50% of the femoral head is affected by necrosis, and in Catterall Group 4, the whole epiphysis is involved. Patients with more than 50% necrosis of the femoral head (Catterall Group 3 or 4) and age of more than 6.0 years at the time of diagnosis were allocated according to the choice of the orthopaedic surgeons at the different hospitals to one of three treatment groups: physiotherapy, Scottish Rite abduction orthosis, and proximal femoral varus osteotomy. The decision was based on the surgeons’ preferences and treatment philosophy. All patients belonging to the same hospital were treated by the same method.
The present study group comprised all 70 children with unilateral LCPD, age at the time of diagnosis of more than 6.0 years, and more than 50% femoral head necrosis (Catterall Groups 3 and 4), who had undergone femoral varus osteotomy. The study group was compared with a control group of all 51 children with similar criteria who had received physiotherapy only. There were no differences between the groups in demographic and radiographic parameters at the time of diagnosis (Table 1).
Table 1.
Demographic, clinical, and radiographic data on patients with varus femoral osteotomy and in the control group
| Variable | Femoral osteotomy group | Control group |
|---|---|---|
| Sex (girls/boys) | 19/51 | 12/39 |
| Pain (+/−) | 63/6 | 47/3 |
| Limping gait (+/−) | 64/3 | 47/3 |
| Age (years)* | 7.4 (7.1–7.6) | 7.6 (7.3–8.0) |
| Age group (>/< 8 years) | 52/18 | 31/20 |
| Symptom duration (months)* | 4.7 (3.7–5.9) | 6.4 (4.5–8.3) |
| Affected side (left/right) | 33/37 | 28/23 |
| Catterall group (3/4) | 48/22 | 27/24 |
| Lateral pillar group (B/C) | 36/34 | 30/21 |
| FHC at diagnosis (%)* | 84.8 (81.9–87.6) | 87.2 (83.3–90.3) |
* Values are expressed as mean, with 95% CI in parentheses; the remaining values are expressed as number of patients; FHC = femoral head coverage.
Femoral osteotomy was performed at a mean of 5.6 months (range, 0.5–32 months) after diagnosis and all the osteotomies except eight were performed during the first year. The osteotomy was performed with one of two slightly different techniques. One technique was a transverse subtrochanteric open-wedge osteotomy and fixation with a stainless steel plate that had been prebent according to the desired degree of varization (Fig. 1). Most of these patients had a hip spica cast for 6 to 8 weeks postoperatively. The other technique was a pertrochanteric closed-wedge osteotomy fixed with a blade plate. Usually no postoperative plaster cast was used after this osteotomy. The choice of surgical technique followed the routines at the hospital where the patients were treated. The mean degree of varization was 23° (range, 15°–34°) and the degree of lateral rotation of the osteotomy (22 patients) was 14° (range, 5°–30°). The osteotomies were performed in nine different hospitals. Postoperatively, the patients were instructed by a physiotherapist to perform exercises to maintain strength and mobility of the hip. Weightbearing was not allowed until after radiographic followup at 6 to 8 weeks showed satisfactory healing of the osteotomy. Postoperative complications occurred in three patients. Wound infection was seen in two patients and was successfully treated with antibiotics. In one subtrochanteric osteotomy without additional plaster fixation, the two screws in the proximal fragment loosened, leading to increased varus.
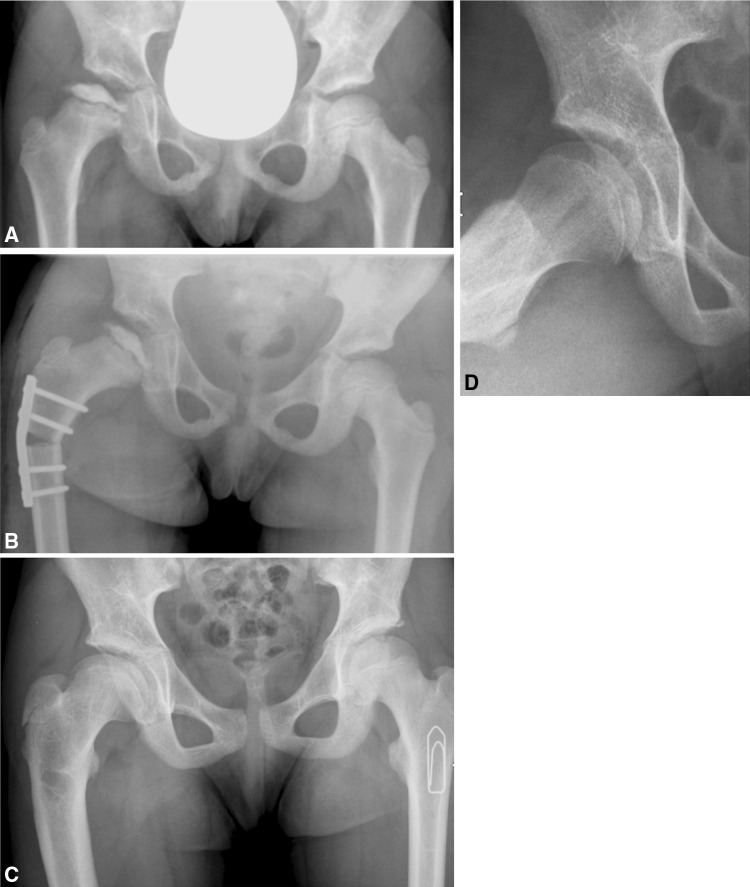
Fig. 1A–D.
Radiographs show the hips of a 7-year-old boy with LCPD of the right hip (Catterall Group 4, Lateral Pillar Group C). He had had symptoms for 2 months before diagnosis. (A) A preoperative AP radiograph and (B) a preoperative radiograph in Lauenstein projection show reduced FHC. (C) A radiograph taken 8 months postoperatively shows containment after subtrochanteric femoral osteotomy with 25° varization and no rotation. (D) A radiograph taken at 5-year followup shows an enlarged but spherical femoral head.
Physiotherapy consisted of ROM exercises and muscle-strengthening exercises. Depending on the ROM, the training sessions took place from once a week to once a month. Although the physiotherapy was supervised, all treatment was local and therefore difficult to standardize.
At the time of diagnosis and at the followup examinations, the patients and their parents were asked about symptoms such as duration and location of pain and whether or not they walked with a limping gait. At 5-year followup, they were also asked about their level of function. Walking distance was considered normal if the patient could walk 5 km; otherwise, it was classified as reduced. Sports activities were classified in four categories: normal, participation in all activities but with reduced function, activities such as swimming only, and no participation. The followup data came from the 5-year followup in all patients. No patients were lost to followup, but there was missing information in one patient in each of the clinical parameters: pain, limping, walking distance, and function. The analysis was performed in the remaining patients.
Radiographs included an AP view with the patient in the supine position with legs parallel and in neutral rotation and a Lauenstein projection with the legs flexed, abducted, and externally rotated. Radiographs were taken at the time of diagnosis and at the followup examinations 1, 3, and 5 years after diagnosis. In addition, radiographs were taken pre- and postoperatively in children who underwent surgical treatment. The radiographs were evaluated and measured by a pediatric orthopaedic surgeon (SS) with long experience in examining radiographs of hips in children. Because the correct amount of involvement can be unreliable in the initial stage of the disease [4, 11], the Catterall grouping for this report (not that for patient selection into the study) was based on both the initial radiographs and those at the 1-year followup. If involvement was more severe after 1 year, the highest Catterall group was used. We also used the lateral pillar classification of Herring et al. [8]. No patient had Lateral Pillar Group A (normal height of the lateral pillar of the femoral head). In Lateral Pillar Group B, more than 50% of the height of the lateral pillar of the femoral head is maintained whereas, in Lateral Pillar Group C, there is reduction of the lateral pillar of more than 50%. The initial radiographs and those after 1 year were used to determine the correct group as explained for the Catterall grouping. The FHC was determined by calculating the percentage of the femoral head medial to Perkins’ line in relation to the width of the femoral head parallel to Hilgenreiner’s line, as described by Heyman and Herndon [9].
There were no differences between the treatment groups in the distribution of Catterall groups and lateral pillar groups (Table 1). There was no difference in Catterall distribution related to sex or age at diagnosis of more than and less than 8.0 years. Children younger than 8.0 years of age had relatively more (p = 0.041) Lateral Pillar B hips than older children.
At 5-year followup, the hips were classified according to Stulberg et al. [14] as modified by Neyt et al. [12]. The Stulberg classification, which originally contained five classes, was modified into a three-group classification [16], where hips in Group A (Stulberg Classes I and II) have spherical femoral heads, those in Group B (Stulberg III) have ovoid femoral heads, and those in Group C (Stulberg IV and V) have flat outlines of the femoral head. The long-term prognosis is best in Group A [14] because no osteoarthritis in such hips was seen after a followup of 30 to 40 years. Group C represents the worst prognostic group since approximately ½ of such hips developed osteoarthritis with narrowing of the joint space [14].
Categorical variables (sex, age group, affected side, pain, limping, Catterall grouping, lateral pillar grouping, and Stulberg grouping) were analyzed by crosstables with the chi-square test to assess differences between the treatment groups. Continuous variables (age, duration of symptoms, and FHC) were analyzed by the t-test for independent samples. Correlations between radiographic outcome and clinical parameters were analyzed by linear correlation (r).
Results
Patients with Catterall Group 3 hips had satisfactory femoral head sphericity (Fig. 2) after 5 years regardless of treatment and age group (Table 2), with only 10% flat femoral heads in the osteotomy group and 7% in the control group. In Catterall Group 4 hips, however, femoral head sphericity was better (p < 0.001) in the osteotomy group, with flat femoral heads in only 14% compared with 75% after physiotherapy; the differences were significant in both children younger than 8.0 years (p = 0.001) and those aged 8.0 to 9.9 years (p = 0.026).
Fig. 2A–D.
Radiographs show the hips of a 7-year-old girl with LCPD of the right hip. She had had pain and limping gait for 5 months before diagnosis. (A) A preoperative radiograph shows LCPD classified as Catterall Group 3 and Lateral Pillar Group C. There is reduced FHC. (B) A postoperative radiograph shows satisfactory FHC after subtrochanteric femoral osteotomy with 25° varization and 20° external rotation. (C) An AP radiograph and (D) a radiograph in Lauenstein projection taken at 5-year followup show a spherical femoral head.
Table 2.
Radiographic 5-year femoral head sphericity (modified Stulberg classification) in relation to degree of femoral head necrosis and age group in patients treated with femoral osteotomy and in the control group
| Femoral head affection | Age group | Femoral osteotomy group (number of patients) | Control group (number of patients) | p value | ||||
|---|---|---|---|---|---|---|---|---|
| Spherical head | Ovoid head | Flat head | Spherical head | Ovoid head | Flat head | |||
| Catterall group | ||||||||
| 3 | All | 24 (50%) | 19 (40%) | 5 (10%) | 16 (59%) | 9 (33%) | 2 (7%) | 0.731 |
| 6.0–7.9 years | 16 | 13 | 5 | 10 | 5 | 0 | 0.220 | |
| 8.0–9.9 years | 7 | 4 | 0 | 6 | 3 | 2 | 0.330 | |
| 4 | All | 6 (27%) | 13 (59%) | 3 (14%) | 1 (4%) | 5 (21%) | 18 (75%) | < 0.001 |
| 6.0–7.9 years | 6 | 10 | 2 | 1 | 3 | 12 | 0.001 | |
| 8.0–9.9 years | 0 | 3 | 0 | 0 | 2 | 6 | 0.026 | |
| Lateral pillar group | ||||||||
| B | All | 22 (61%) | 13 (36%) | 1 (3%) | 16 (53%) | 9 (30%) | 5 (17%) | 0.148 |
| C | All | 8 (23%) | 19 (56%) | 7 (21%) | 1 (4%) | 5 (24%) | 15 (71%) | 0.001 |
We observed no differences in femoral head sphericity between the femoral osteotomy and control groups (Table 2) in Lateral Pillar Group B hips, regardless of whether all patients or only those older or younger than 8.0 years of age were analyzed. In Lateral Pillar Group C hips, better outcome occurred after femoral osteotomy than in the control group in children 6.0 to 7.9 years (p = 0.005) but not in children 8.0 to 9.9 years (p = 0.091).
There were no differences between the treatment groups in FHC at the time of diagnosis and at the 1-year follow-up (Table 3). At the 5-year followup, FHC was higher (p = 0.015) in hips treated with femoral osteotomy than in the control hips in Catterall Group 4 but not in Catterall Group 3. In hips with osteotomy, the mean FHC decreased until the time of surgery and was 76% on the last radiograph before osteotomy. On the first radiograph after osteotomy had healed, the FHC had increased to 92%. The mean increase in FHC between the post- and preoperative radiographs was 15.5% (range, 2%–39%).
Table 3.
Femoral head coverage according to Catterall group and treatment
| Time | Femoral head coverage (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Catterall Group 3 | Catterall Group 4 | |||||||||
| Femoral osteotomy group | Control group | p value | Femoral osteotomy group | Control group | p value | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| At diagnosis | 86.4 | 9.9 | 90.4 | 8.6 | 0.094 | 81.1 | 14.3 | 83.5 | 15.1 | 0.603 |
| 1-year followup | 86.3 | 14.3 | 81.3 | 6.3 | 0.069 | 83.2 | 15.7 | 75.6 | 7.2 | 0.059 |
| 5-year followup | 79.0 | 11.0 | 81.9 | 6.7 | 0.178 | 77.7 | 12.8 | 69.8 | 8.1 | 0.015 |
At the 5-year followup, walking capacity was better (p = 0.038) in the osteotomy group than in the physiotherapy group. No differences between the treatment groups regarding pain (p = 0.26), limp (p = 0.41), or level of function (p = 0.34) occurred. There were correlations (p < 0.001) between femoral head sphericity and the clinical parameters pain (r = 0.47), limp (r = 0.48), walking capacity (r = 0.39), and physical activities (r = 0.38), with more complaints and worse function in hips with flat femoral heads.
Discussion
The 5-year radiographic results in the Norwegian prospective nationwide study on LCPD were better after varus femoral osteotomy than after physiotherapy and abduction orthosis in children older than 6.0 years at diagnosis with femoral head necrosis of more than 50% [17]. This does not mean all children in this group should undergo surgery because 1/3 of those treated with physiotherapy had spherical femoral head at the last followup. In the present study, we further evaluated patients who had undergone femoral osteotomy. Our aim was to find out whether femoral osteotomy gave better femoral head sphericity in all children with more than 50% femoral head necrosis or in particular groups only. We also wanted to find out whether there was, within the age range 6.0 to 10.0 years, a critical age over which femoral osteotomy did not improve femoral head sphericity.
We noted certain limitations of our study. First, the number of patients older than 9.0 years was rather small. Therefore, the analysis in these children might be less reliable for drawing sound conclusions. Second, children who had physiotherapy were used as a control group. Although it could be questioned whether physiotherapy is representative of the natural history of the disease, we believe so, because physiotherapy has not been proven to have any effect on femoral head sphericity in LCPD [7].
What seems most important in long-term followup is to avoid a flat femoral head (Stulberg Classes IV and V) because these hips tend to develop osteoarthritis [14]. Sphericity of the femoral head after LCPD is related to the degree of femoral head necrosis. In his study on nonoperative treatment, Catterall [2] found flat femoral heads in 22% in Catterall Group 3 and in 69% in Catterall Group 4. An even greater discrepancy between Catterall Groups 3 and 4 occurred in the physiotherapy group in the Norwegian multicenter study [15]. This great difference in natural history between Catterall Groups 3 and 4 indicates these subgroups should be analyzed separately. Most previous studies have combined these groups, thus masking the difference.
We found the femoral head sphericity 5 years after femoral osteotomy in Catterall Group 3 hips was similar to that in the control group, with approximately 50% spherical and 10% flat femoral heads. Similar degree of sphericity after varus femoral osteotomy was reported by Coates et al. [3]. Thus, there is a relatively good prognosis in Catterall Group 3 hips and surgical treatment is rarely indicated. At 5 years, Catterall Group 4 hips in the control group had no less than 75% flat femoral heads while in hips treated with femoral osteotomy only 14% had flat femoral heads. Although Coates et al. [3] included some patients younger than 6.0 years, 9% had flat femoral heads after femoral osteotomy in Catterall Group 4 hips. Thus, it seems rational to advice surgical containment treatment in hips with necrosis of the entire femoral head in children in the age range 6.0 to 9.9 years at diagnosis.
We found patients with Lateral Pillar Group B hips had satisfactory femoral head sphericity regardless of treatment. The multicenter study of Herring et al. [7] also showed no difference between operative and nonoperative treatment in patients 6.0 to 8.0 years of age. In patients older than 8.0 years, Herring et al. [7] obtained better femoral head sphericity in children who had undergone femoral or pelvic osteotomy. However, since there were less than 20% flat femoral heads after nonoperative treatment in both prospective multicenter studies [7, 17], we do not recommend surgical treatment in Lateral Pillar Group B hips even in children older than 8.0 years, unless the FHC is substantially decreasing toward subluxation.
In Lateral Pillar Group C hips, we found better femoral head sphericity after surgery in children 6.0 to 7.9 years. This is in contrast to the study of Herring et al. [7] that reported no difference in femoral head sphericity (Table 4). However, when using Table II in their report [7], it is obvious femoral head sphericity in the Group “B/C-border” was quite similar to the results in Lateral Pillar Group C hips. It therefore seems justifiable to combine Groups C and B/C-border. The femoral head sphericity then was better in the surgically treated hips than in those with nonoperative treatment, with only 8% flat femoral heads in the former group and 23% in the latter. A similar degree of femoral head sphericity after surgical treatment of Lateral Pillar Group C hips in children younger than 9.0 years (Table 4) was confirmed by Friedlander and Weiner [5] and Aksoy et al. [1], with flat femoral heads in only 10% and 14%, respectively.
Table 4.
Radiographic femoral head sphericity (modified Stulberg classification) at followup according to treatment methods in children older than 6.0 years with Lateral Pillar Group C hips
| Age (years) | Treatment | Study | Number of patients | Femoral head sphericity (% of hips) | ||
|---|---|---|---|---|---|---|
| Spherical head | Ovoid head | Flat head | ||||
| 6.0–7.9 | Nonoperative | Herring et al. [7] (2004) | 30 | 10 | 67 | 23 |
| 6.0–7.9 | Nonoperative | Current study | 9 | 0 | 11 | 89 |
| 6.0–7.9 | Operative | Herring et al. [7] (2004) | 11 | 36 | 55 | 9 |
| 6.0–7.9 | Operative | Current study | 25 | 28 | 48 | 24 |
| < 9.0 | Operative | Friedlander and Weiner [5] (2000) | 40 | 43 | 47 | 10 |
| < 9.0 | Operative | Aksoy et al. [1] (2005) | 14 | 43 | 43 | 14 |
| > 8.0 | Nonoperative | Herring et al. [7] (2004) | 14 | 7 | 29 | 64 |
| 8.0–9.9 | Nonoperative | Current study | 9 | 0 | 33 | 67 |
| > 8.0 | Operative | Herring et al. [7] (2004) | 5 | 0 | 20 | 80 |
| 8.0–9.9 | Operative | Current study | 5 | 0 | 80 | 20 |
| > 9.0 | Operative | Friedlander and Weiner [5] (2000) | 28 | 32 | 50 | 18 |
| > 9.0 | Operative | Aksoy et al. [1] (2005) | 12 | 0 | 67 | 33 |
In children older than 8.0 years with Lateral Pillar Group C hips, the number of patients with surgical treatment was too small for meaningful statistical analysis in both our study and that of Herring et al. [7]. If the surgically treated patients of Friedlander and Weiner [5] and Aksoy et al. [1] older than 9.0 years with Lateral Pillar Group C hips are included in the analysis together with the two multicenter studies (Table 4), femoral head sphericity is better in patients with operative treatment, with 28% flat femoral heads compared with 65% flat heads after nonoperative treatment. Thus, these studies and the two multicenter studies indicate surgical treatment should be recommended in patients between 6.0 and 8.0 years and those older than 8.0 years.
Whether there was an upper age limit above which surgical treatment no longer gave better femoral head sphericity was difficult to evaluate because of the small number of older patients. We did not find any relationship between femoral head sphericity and age in children within the age range 6.0 to 9.9 years. Compared with children older than 9.0 years, markedly better femoral head sphericity in children younger than 9.0 years was reported by Aksoy et al. [1], whereas the effect of age was smaller in the study of Friedlander and Weiner [5]. Noonan et al. [13] reported 1/3 of patients older than 9.0 years with Catterall Groups 3 and 4 hips had spherical femoral heads after osteotomy, but head sphericity was better in patients 9.0 to 10.0 years of age than in older patients. They found it doubtful whether the natural history was changed by surgery in patients older than 10.0 years. More studies on children older than 9.0 years with severe LCPD are needed before reliable conclusions can be drawn.
Reduced FHC is an important factor in the deformation of the femoral head [2, 6, 10], which is the rationale behind the use of containment surgery. The natural history of FHC in patients older than 6.0 years and with more than 50% necrosis was a mean total reduction of 12% during a 5-year period [15]. The reduction (6%) was less in the surgically treated hips and the pattern of change was different. There was a reduction of 9% from diagnosis to the preoperative radiograph, followed by an increase of about 16% caused by the operation. The increase in FHC gives better containment relatively early in the disease when containment is most important for remodeling of the new femoral head. The preoperative FHC was lower in Catterall Group 4 hips, showing these hips were in special need of improved containment.
Acknowledgments
The authors thank the statistician Are Hugo Pripp for help and advice with the statistical analysis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that all investigations were conducted in conformity with ethical principles of research and that informed consent for participation in the study was obtained.
This work was performed at Oslo University Hospital, Oslo, Norway.
References
- 1.Aksoy MC, Cankus MC, Alanay A, Yazici M, Caglar O, Alpaslan AM. Radiological outcome of proximal femoral varus osteotomy for the treatment of lateral pillar group-C Legg-Calvé-Perthes disease. J Pediatr Orthop B. 2005;14:88–91. doi: 10.1097/01202412-200503000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Catterall A. The natural history of Perthes’ disease. J Bone Joint Surg Br. 1971;53:37–53. [PubMed] [Google Scholar]
- 3.Coates CJ, Paterson JM, Woods KR, Catterall A, Fixsen JA. Femoral osteotomy in Perthes’ disease. J Bone Joint Surg Br. 1990;72:581–585. doi: 10.1302/0301-620X.72B4.2380208. [DOI] [PubMed] [Google Scholar]
- 4.Dickens DR, Menelaus MB. The assessment of prognosis in Perthes’ disease. J Bone Joint Surg Br. 1978;60:189–194. doi: 10.1302/0301-620X.60B2.659461. [DOI] [PubMed] [Google Scholar]
- 5.Friedlander JK, Weiner DS. Radiographic results of proximal femoral varus osteotomy in Legg-Calvé-Perthes disease. J Pediatr Orthop. 2000;20:566–571. doi: 10.1097/01241398-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Green NE, Beauchamp RD, Griffin PP. Epiphyseal extrusion as a prognostic index in Legg-Calvé-Perthes disease. J Bone Joint Surg Am. 1981;63:900–905. [PubMed] [Google Scholar]
- 7.Herring JA, Kim HT, Browne R. Legg-Calvé-Perthes disease. Part II. Prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg Am. 2004;86:2121–2134. [PubMed] [Google Scholar]
- 8.Herring JA, Neustadt JB, Williams JJ, Early JS, Browne RH. The lateral pillar classification of Legg-Calvé-Perthes disease. J Pediatr Orthop. 1992;12:143–150. doi: 10.1097/01241398-199203000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Heyman CH, Herndon CH. Legg-Perthes disease. J Bone Joint Surg Am. 1950;32:767–778. [PubMed] [Google Scholar]
- 10.Joseph B, Varghese G, Mulpuri K, Rao N, Nair NS. Natural evolution of Perthes disease: a study of 610 children under 12 years of age at disease onset. J Pediatr Orthop. 2003;23:590–600. doi: 10.1097/01241398-200309000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Kelly FB, Canale ST, Jones RR. Legg-Calvé-Perthes disease: long-term evaluation of non-containment treatment. J Bone Joint Surg Am. 1980;62:400–407. [PubMed] [Google Scholar]
- 12.Neyt JG, Weinstein SL, Spratt KF, Dolan L, Morcuende J, Dietz FR, Guyton G, Hart R, Kraut MS, Lervick G, Pardubsky P, Saterbak A. Stulberg classification system for evaluation of Legg-Calvé-Perthes disease: intra-rater and inter-rater reliability. J Bone Joint Surg Am. 1999;81:1209–1216. doi: 10.2106/00004623-199909000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Noonan KJ, Price CT, Kupiszewski SJ, Pyevich M. Results of femoral varus osteotomy in children older than 9 years of age with Perthes disease. J Pediatr Orthop. 2001;21:198–204. doi: 10.1097/00004694-200103000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Stulberg SD, Cooperman DR, Wallensteen R. The natural history of Legg-Calvé-Perthes disease. J Bone Joint Surg Am. 1981;63:1095–1108. [PubMed] [Google Scholar]
- 15.Terjesen T, Wiig O, Svenningsen S. The natural history of Perthes disease: risk factors in 212 patients followed for 5 years. Acta Orthop. 2010;81:708–714. doi: 10.3109/17453674.2010.533935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wiig O, Terjesen T, Svenningsen S. Inter-observer reliability of the Stulberg classification in the assessment of Perthes disease. J Child Orthop. 2007;1:101–105. doi: 10.1007/s11832-007-0020-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wiig O, Terjesen T, Svenningsen S. Prognostic factors and outcome of treatment in Perthes’ disease: a prospective study of 368 patients with five-year follow-up. J Bone Joint Surg Br. 2008;90:1364–1371. doi: 10.1302/0301-620X.90B10.20649. [DOI] [PubMed] [Google Scholar]