Abstract
Background
A diagnosis of cervical radiculopathy is based largely on clinical examination, including provocative testing. The most common maneuver was described in 1944 by Spurling and Scoville. Since then, several modifications of the original maneuver have been proposed to improve its value in the diagnosis of cervical radiculopathy.
Questions/Purposes
We assessed the ability of six known variations of the Spurling test to reproduce the complaints of patients diagnosed with cervical radiculopathy.
Methods
We prospectively enrolled 67 patients presenting with cervical radicular-like symptoms and concordant radiographic findings. Each patient underwent six distinct provocative cervical spine maneuvers by two examiners, during which three parameters were recorded: (1) pain intensity (VAS score), (2) paresthesia intensity (0 - no paresthesia, 1 - mild to moderate, and 2 - severe), and (3) characteristic pain distribution (0 - no pain, 1 - neck pain only, 2 - arm pain only, 3 - pain elicited distal to the elbow). The interobserver reliability of the reported VAS score (measured by the intraclass coefficient correlation) ranged from 0.78 to 0.96 and the calculated kappa values of the categorical parameters ranged from 0.58 to 1.0 for paresthesia intensity and from 0.63 to 1.0 for pain distribution. Differences in scores elicited between the two examiners for the 67 patients were resolved by consensus.
Results
A maneuver consisting of extension, lateral bending, and axial compression resulted in the highest VAS score (mean, 7) and was associated with the most distally elicited pain on average (mean, 2.5). The highest paresthesia levels were reported after applying extension, rotation, and axial compression (mean, 1). These maneuvers, however, were the least tolerable, causing discontinuation of the examination on three occasions.
Conclusions
Whenever cervical radiculopathy is suspected our observations suggest the staged provocative maneuvers that should be included in the physical evaluation are extension and lateral bending first, followed by the addition of axial compression in cases with an inconclusive effect.
Level of Evidence
Level II, diagnostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Cervical radiculopathy is a primary disorder of the cervical nerve root, commonly manifesting as pain radiating from the neck to a dermatomal distribution of the affected nerve root. Physical examination, although lacking well-defined criteria [16, 26], remains the mainstay in attempting to differentiate nerve root compression from other disorders capable of mimicking upper limb radicular-like complaints, such as brachial plexitis, shoulder impingement disorders, and posttraumatic pain. Moreover, treatment selection relies heavily on an optimal correlation between the physical examination and various radiographic findings. Additional diagnostic means supplanting physical examination include electrophysiologic and advanced radiologic studies [1, 2, 12, 25]. Nevertheless, the often-diminished availability and expense of these resources frequently cause the primary caretaker to rely on much simpler and accessible diagnostic tools in identifying various disorders.
The maneuver described by Spurling and Scoville in 1944, referred to as the Spurling compression test [27], successfully answers some of the aforementioned issues [4, 9, 17], alongside other provocative maneuvers. Since then, numerous authors have attempted to characterize the diagnostic value of the Spurling compression test, suggesting relatively high specificity and positive predictive value rates [16, 21, 26, 29]. The original description of this test, later adopted by other authors [9, 11, 17, 31], suggested that the provocative maneuver should include use of lateral bending and axial compression to the cervical spine in an attempt to reproduce the patient’s complaints. However, at least five other modifications of this test have been offered: lateral bending, rotation, and compression (also referred to as the maximum cervical compression test) [17, 33]; extension and compression as suggested by Bradley et al. [6]; extension and lateral bending [33]; extension, lateral bending, and compression [29]; and extension, rotation, and compression [6, 31].
Although not included in the original provocative maneuver described by Spurling and Scoville, our clinical experience suggests that adding cervical spine extension may increase the test’s ability to reproduce the complaints of a patient presenting with cervical radiculopathy.
The purposes of the current study were: (1) to evaluate the ability of each of the Spurling test variants to reproduce the radiculopathic complaints in terms of three key variables that can be quantified and reproduced: the level of pain elicited measured by the VAS score, the intensity of paresthesia elicited, and the pattern of pain distribution; (2) to search for a possible association between variables such as patient age and the disorder level and type, and the reported score of the three parameters; (3) to establish a causal relationship between the presenting disorder and the evoked symptoms; and (4) to evaluate the overall tolerability of the Spurling tests variants.
Patients and Methods
We prospectively enrolled 67 patients referred to one institution from May 2005 to May 2006. We included patients presenting with radicular symptoms (ie, pain radiating along a specific dermatome) in the upper extremity, the presence of a cervical disc herniation confirmed by either CT or MRI, and a clinical correlation with the radiographic findings. All patients presented with unilateral complaints. We excluded patients with clinical evidence of substantial myelopathy, prior cervical spine surgery, and any history of major cervical trauma. The patients ranged in age from 23 to 75 years (mean, 46 years); 31 women and 36 men were enrolled in this study. The median duration of symptoms before enrollment was 9 weeks (range, 1–100 weeks). We recorded the age, gender, dermatomal pain distribution, overall duration of pain, and the level of the disorder. On initial neurologic examination, 27 patients had a sensory deficit, 12 had motor weakness, three had both, and the remaining patients were neurologically intact. Clinical evidence of mild to moderate upper motor neuron involvement was evident in 11 patients. The radiographic findings included an isolated lesion, being either a soft (n = 42) or hard disc herniation (n = 9) or a mixed lesion (n = 13) (Table 1). Foraminal stenosis was the main finding in three patients. The most common levels of the disorder were C5-C6 and C6-C7 (n = 30), followed by C4-C5 (n = 5) and C3-C4 (n = 2). In patients with more than one level affected on observed radiographs (n = 6), the level that matched either the patient’s complaints of paresthesia or any neurologic deficit on examination (sensory or motor) was considered for the purpose of statistical analysis. Informed consent for participation in this study, which was approved by our institutional review board, was given by all subjects.
Table 1.
Radiographic findings according to the lesion level and type
| Level | Soft disc | Hard disc | Stenosis | Mixed lesion | Total |
|---|---|---|---|---|---|
| C3-C4 | 0 | 1 | 1 | 0 | 2 |
| C4-C5 | 4 | 0 | 1 | 0 | 5 |
| C5-C6 | 17 | 6 | 1 | 6 | 30 |
| C6-C7 | 21 | 2 | 0 | 7 | 30 |
| Total | 42 | 9 | 3 | 13 | 67 |
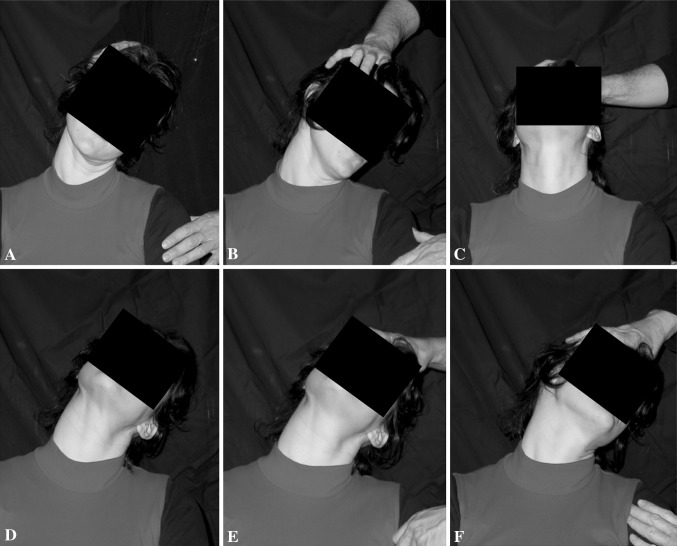
On enrollment, all patients underwent an evaluation of the following items on the physical examination: motor strength of key muscle groups was assessed by manual testing and graded according to the Medical Research Council scale, a measurement with reasonable interobserver and intraobserver reliability [18]; sensory evaluation according to a dermatomal distribution; and the presence of upper motor neuron signs. In addition, the pain level at rest was evaluated using the 100-mm VAS, a tool that is reliable for measuring chronic and acute pain [3, 5]. After the initial examination, each subject, while seated, underwent six distinct provocative maneuvers of the cervical spine in the following order: lateral bending and axial compression, the original test described by Spurling and Scoville [27] (Fig. 1A); lateral bending, ipsilateral rotation and axial compression, also called the maximum cervical compression test (Fig. 1B); extension and axial compression as suggested by Bradley et al. [6] (Fig. 1C); extension and lateral bending [33] (Fig. 1D); extension, lateral bending, and axial compression [29] (Fig. 1E); and extension, rotation, and axial compression [6, 21, 31] (Fig. 1F).
Fig. 1A–F.
Six varieties of the Spurling test are shown, including (A) lateral bending and compression; (B) lateral bending, rotation, and compression; (C) extension and compression; (D) extension and lateral bending; (E) extension, lateral bending, and compression; and (F) extension, rotation, and compression.
After each maneuver, performed by two of us (YA and YM), three parameters were recorded, as reported by the patient: intensity of pain elicited (evaluated using the standard 1 to 10 VAS score), intensity of paresthesia elicited (evaluated using a 0 to 2 scale: 0 = no paresthesia, 1 = mild to moderate, 2 = severe), and characteristic pain distribution. For the purpose of statistical analysis, the pain distribution was classified as: 0 = no pain, 1 = neck pain only, 2 = pain provoked only proximal to the elbow, and 3 = pain provoked distal to the elbow. To decrease the potentially sensitizing effect of each maneuver, the pain and paresthesia were allowed to resolve completely before advancing to the next maneuver. To assess the interobserver reliability we constructed an additional sample group, consisting of 10 patients with similar inclusion criteria as the study group. The interobserver reliability was assessed by calculating the intraclass correlation coefficient (ICC) of the sequential parameter (the reported VAS score) and calculating kappa values for the categorical parameters. ICC values ranged from 0.78 to 0.96 and the kappa values ranged from 0.58 to 1.0 for paresthesia intensity and from 0.63 to 1.0 for pain distribution.
To decrease the likelihood of a nonrandomization bias and to associate the patients’ complaints with the radiographic findings, two control groups were added in which the same previously described maneuvers were used. In the first group, 15 patients with complaints of radicular pain and a herniated cervical disc observed on radiographs (ie, similar inclusion criteria as the study group) underwent the six maneuvers only in a reverse manner (6 through 1). In the second group, 15 patients with complaints of axial neck pain and radiographs compatible with spondylotic changes, excluding any evidence of a compressive finding, underwent the six maneuvers in the same order. Exclusion criteria did not differ in the control groups. The pain and paresthesia were allowed to resolve fully in a similar manner between maneuvers.
To assess differences between each pair of maneuvers in the parametric tests (VAS score and the level of paresthesia), we used Student’s t-test (two-tailed) with the post hoc Bonferroni correction, and the McNemar-Bowker test to analyze the characteristic pain location. VAS scores also were compared with the mean score at rest. Analyses of the parametric tests in the study group in comparison to the control groups were performed using ANOVA with repeated measures and in the nonparametric test (characteristic pain location) using the chi-square test. In addition, we used ANOVA with repeated measures to assess for possible associations between variables such as patient age, disease level and type, and all reported scores. The statistical analysis was performed using SPSS® software version 15.0.1 (SPSS®, Chicago, IL, USA).
Results
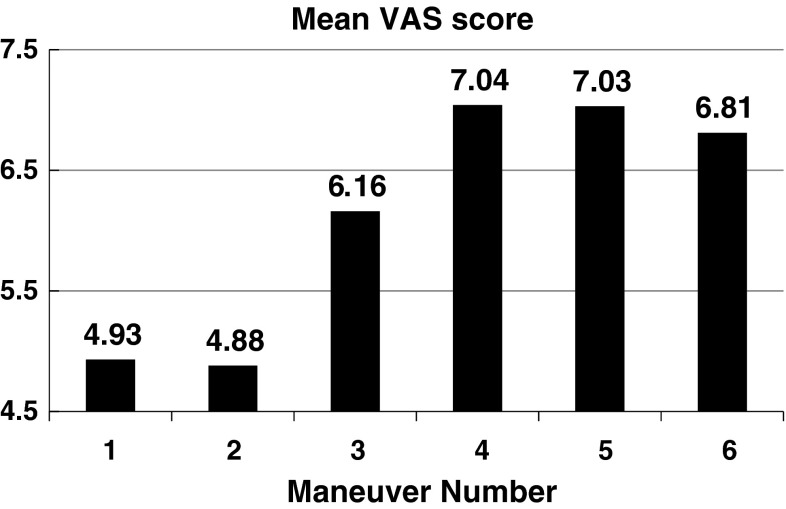
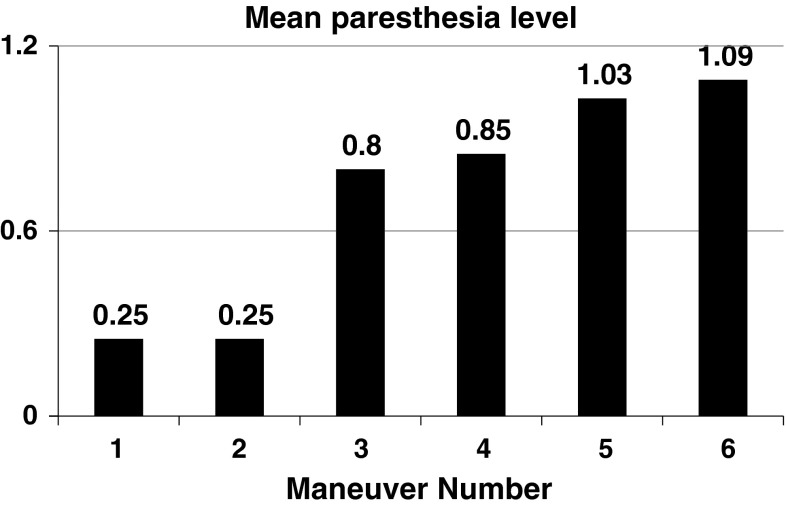
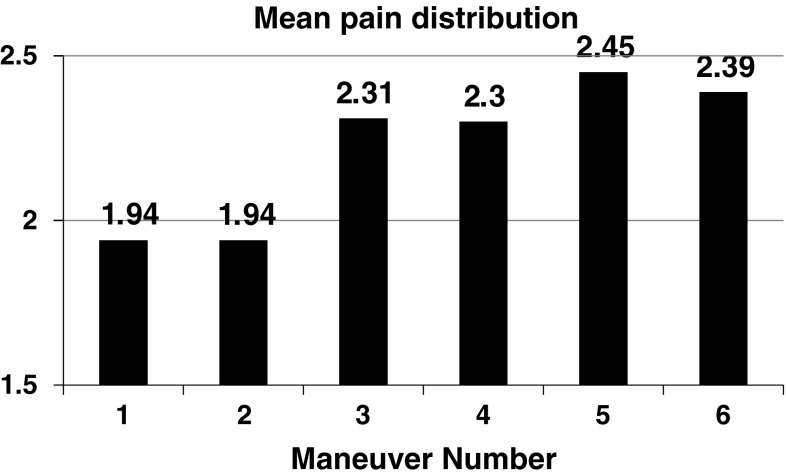
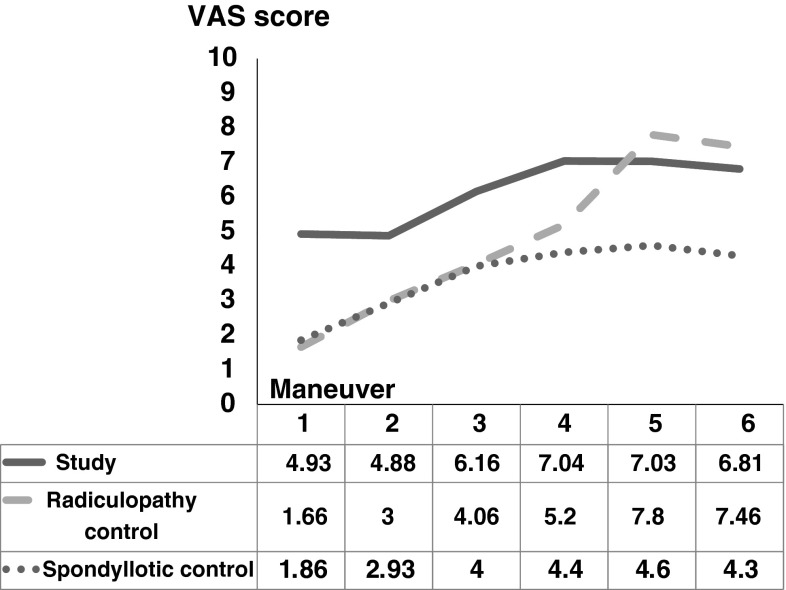
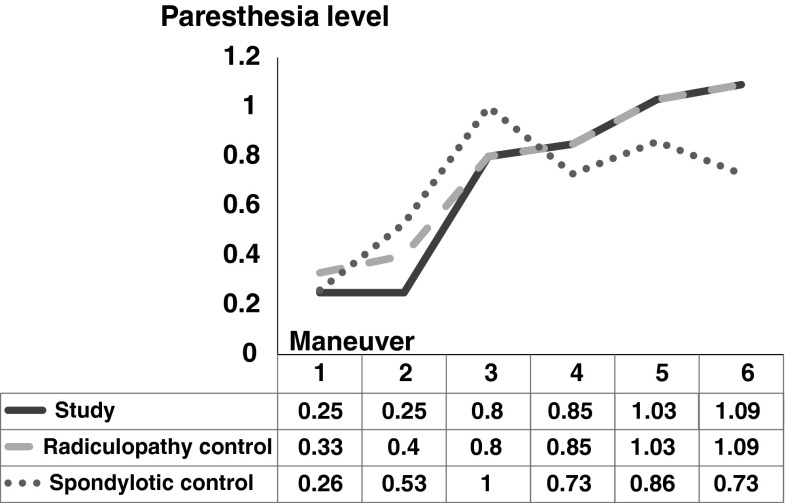
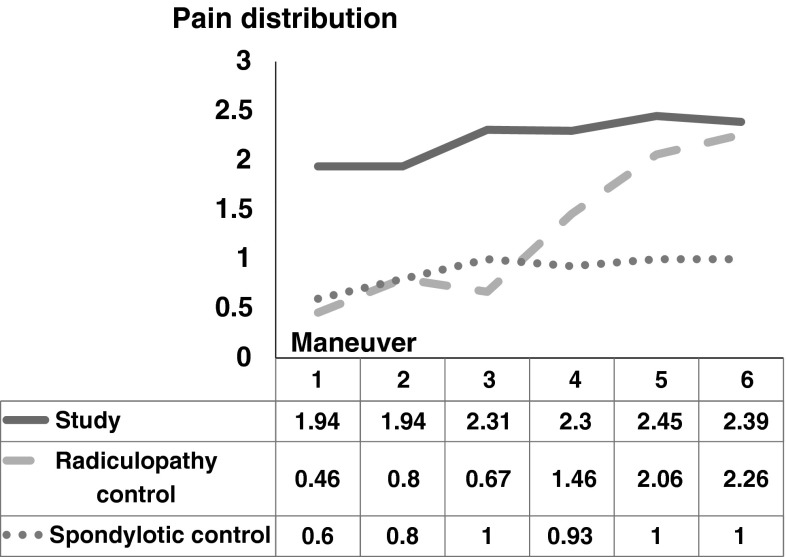
Each of the applied maneuvers provoked pain and paresthesias that were concordant with the patient’s usual complaints. The maneuver resulted in the highest VAS mean score and the most distally elicited pain was extension, lateral bending, and axial compression (Fig. 2). In general, maneuvers incorporating extension (3 through 6) provoked an increased level of paresthesia (p < 0.001) (Fig. 3), and a more distally oriented pain (p = 0.01) (Fig. 4) compared with other maneuvers.
Fig. 2.
The graph shows the mean elicited VAS scores. The highest average VAS score was reported after extension and lateral bending (Maneuver 4).
Fig. 3.
The graph shows the mean elicited paresthesia levels. The level increased (p < 0.001) with the addition of extension to the maneuvers, with the highest level evoked after extension, rotation, and axial compression (Maneuver 6).
Fig. 4.
The graph shows the mean elicited pain distribution. Maneuvers that included extension were more likely (p = 0.01) to provoke a radicular-type pain (pain provoked distal to the elbow).
Analysis of the difference between each possible pair of maneuvers (Table 2) showed the similarity in the mean of all parameters reported after Maneuvers 1 and 2 (containing no extension) and Maneuvers 3 through 6 incorporating extension. Similarly, the mean reported VAS score after applying maneuvers incorporating extension was greater than the VAS at rest after maneuvers 3, 5, and 6 (Table 3).
Table 2.
Differences between each possible pair of maneuvers in all three recorded parameters
| Pair of maneuvers | VAS score | Paresthesia intensity | Pain distribution |
|---|---|---|---|
| p value | p value | p value | |
| 1 and 2 | 0.636 | 0.321 | 1.0 |
| 1 and 4 | 0.1* | < 0.001 | < 0.05 |
| 2 and 4 | 0.08* | < 0.001 | < 0.05 |
| 3 and 4 | 0.265 | 1.0 | 0.343 |
| 3 and 5 | 0.16* | 0.54* | 0.339 |
| 3 and 6 | 0.075 | < 0.001 | 0.236 |
| 4 and 5 | 0.926 | 0.03* | 0.598 |
| 4 and 6 | 0.786 | 0.001 | 0.446 |
| 5 and 6 | 0.226 | 0.167 | 0.392 |
| All other possible pairs | < 0.005 | < 0.001 | < 0.05 |
* After applying the Bonferroni correction.
Table 3.
Differences between the VAS score at rest compared with the average VAS score after each maneuver
| Maneuver number | p value |
|---|---|
| 1 | 0.53 |
| 2 | 0.96 |
| 3 | < 0.001 |
| 4 | 0.08 |
| 5 | < 0.001 |
| 6 | < 0.001 |
We found no association between the three parameters and patient age or disease level and type. The overall tolerability of the first four maneuvers was satisfactory. On the contrary, maneuvers 5 and 6 resulted in reported VAS scores of 9 and 10 in nine subjects. Complete discontinuation of the examination occurred on three occasions, after the patients reported intolerable pain levels during application of Maneuvers 5 and 6.
The reported VAS score was higher in the study group compared with the control group with spondylosis throughout maneuvers and similar to that of the control group with radiculopathy (the reversed order) after Maneuvers 5 and 6 (Fig. 5). The reported paresthesia level followed a similar pattern in the study and group with radiculopathy and was lower in the control group with spondylosis after Maneuvers 5 and 6 (Fig. 6). Finally, patients in the study group reported a more distally elicited pain throughout maneuvers compared with the group with spondylosis, whereas the group with radiculopathy reported similar pain distribution after Maneuvers 5 and 6 (Fig. 7).
Fig. 5.
The diagram shows the mean VAS score in the study group compared with both control groups. The study group reported higher VAS scores (p = 0.004) compared with the group with spondylosis (dotted line) and similar VAS scores (p = 0.09) compared with the group with radiculopathy (dashed line).
Fig. 6.
The diagram shows the mean paresthesia level in the study group compared with both control groups. No difference was noted between the study group and either the group with spondylosis (p = 0.85) or the group with radiculopathy (p = 0.13).
Fig. 7.
The diagram shows the mean pain distribution in the study group compared with both control groups. The group with spondylosis reported pain which was more often (p < 0.001) proximally located in response to the maneuvers compared with the study group. In patients with radiculopathy, performing the maneuvers in the reverse order provoked similar pain distribution in Maneuvers 5 and 6 (p = 0.33 and p = 0.46, respectively), but more often (p < 0.001) elicited proximally located pain thereafter (for Maneuvers 4 through 1).
Discussion
Cervical disc herniation causing neural compression was first described by Key in 1838 [15]. Thereafter, the clinical syndrome of cervical cord myelopathy related to a ruptured disc greatly evolved owing to the work of early 20th century researchers [19, 28]. With identification of cervical radiculopathy as a primary disorder of the cervical nerve root [23, 27], an ongoing effort was made to develop diagnostic criteria differentiating it from other common disorders affecting the upper limbs [22]. Despite extensive use of imaging modalities and electrophysiology studies, considered to be better-validated compared with physical examination [14, 20], no universally accepted criteria appear to exist for the diagnosis of cervical radiculopathy [32]. Consequently, the patient’s complaints and physical examination retain their pivotal roles in diagnosing cervical radiculopathy. The numerous modifications of the Spurling test described thus far simultaneously reiterate its important role in the diagnostic process of cervical radiculopathy and show the disagreement regarding the most appropriate way in which it should be performed. We therefore: (1) evaluated the ability of each of the Spurling test variants to reproduce the radiculopathic complaints in terms of three key variables that can be quantified and reproduced: the level of pain elicited measured by the VAS score, the intensity of paresthesia elicited, and the pattern of pain distribution; (2) searched for a possible association between variables such as patient age and the disorder level and type, and the reported score of the three parameters; (3) explored a causal relationship between the presenting disorder and the evoked symptoms; and (4) evaluated the overall tolerability of the Spurling tests variants.
There were limitations to our study. First, the fact that the maneuvers were performed in an identical order instead of being randomized as a preferred methodology might have resulted in an additive effect in the hypersensitized patient. In a pilot study including 10 patients, adding extension to the originally described Spurling maneuver seemed to increase the degree of pain and paresthesia reported, resulting in longer recovery periods. Starting the examination with the least painful maneuvers therefore could enable a shorter and more tolerable examination. The lack of a difference in reported pain and paresthesia level after the maneuvers were performed in reverse order in the control group with radiculopathy also may compensate for the lack of randomization. Second, the study group does not provide a clear causal relationship between the presumed underlying disorder (ie, cervical nerve root compression) and the elicited symptoms. A difference in the scores of the reported pain level and location among patients in the control group with spondylosis may assist in establishing such an association. Third, defining the efficacy of any physical examination usually requires comparing the observed results with those of an accepted gold standard. In the case of cervical radiculopathy, candidates for such a gold standard include evidence of root compression intraoperatively, radiographically (MRI, CT), or in electrophysiologic studies. We believe documented root compression on advanced imaging meets this requirement. Finally, the limited setting in which the current study was conducted may further impair its validity. The design of future multicenter larger-scale studies may overcome this disadvantage.
Like the Spurling test, many other provocative, and relief tests, are available when neural compression is suspected. However, in contrast to the modifications offered to the Spurling test, which have attempted to increase the patients’ characteristic symptoms, modifications to other provocative tests have been offered to serve other purposes [17]. In the cervical spine, variations of joint position during application of the upper limb tension test, for example, have been offered in an attempt to increase stress on various neural tissue [8]. Similarly, modifications of the slump test or Laségue’s test in the evaluation of sciatic pain serve to assess various neural elements, but also to differentiate true sciatic pain from symptoms related to secondary gain [7, 17]. Although various modifications to existing provocative maneuvers have been described, it appears that reports attempting to quantify the clinical effect of these modifications, to evaluate the association of the clinical effect with demographic and radiographic parameters, and to assess the tolerability of these modifications are lacking.
Several reports have established a clear causal relationship between a positive Spurling test and the presence of cervical root compression, evident either on radiographs [24] or in electrodiagnostic studies [29]. The decreased VAS score and dissimilar pain distribution reported in the control group with spondylosis compared with the study group corroborate with previous findings. The added advantage of extension in enhancing the reported complaints is supported by biomechanical studies that have shown an increase in neuroforaminal [10] and intradiscal [13] pressures in response to extension of the cervical spine.
One study assessing the interexaminer reliability of the Spurling test found an association between the patient’s position and reliability [30], with kappa values ranging from 0.47 to 0.80 in the sitting position and from 0.28 to 0.63 in the supine position. The reliability found in our study is similar to those found in the sitting position in that study.
Previously described maneuvers, including the one originally described by Spurling and Scoville and the maximum cervical compression test, were inferior to other maneuvers incorporating extension in provoking radiculopathic complaints. As an alternative, we suggest that a maneuver consisting of extension and lateral bending, which reproduced the patient’s complaints in a tolerable fashion, be done first followed by addition of axial compression in the case of an inconclusive effect.
Footnotes
Each author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent-licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained from all subjects.
References
- 1.Ahlgren BD, Gardin SR. Cervical radiculopathy. Orthop Clin North Am. 1996;27:253–263. [PubMed] [Google Scholar]
- 2.Bartlett RJ, Hill CR, Gardiner E. A comparison of T2 and gadolinium enhanced MRI with CT myelography in cervical radiculopathy. Br J Radiol. 1998;71:11–19. doi: 10.1259/bjr.71.841.9534693. [DOI] [PubMed] [Google Scholar]
- 3.Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analogue scale for measurement of acute pain. Acad Emerg Med. 2001;8:1153–1157. doi: 10.1111/j.1553-2712.2001.tb01132.x. [DOI] [PubMed] [Google Scholar]
- 4.Bland JH. Clinical methods. In: Bland JH, ed. Disorders of the Cervical Spine. Diagnosis and Medical Management. Philadelphia, PA: WB Saunders; 1987:79–112.
- 5.Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res. 2008;31:165–169. doi: 10.1097/MRR.0b013e3282fc0f93. [DOI] [PubMed] [Google Scholar]
- 6.Bradley JP, Tibone RE, Watkins RG. History, physical examination, and diagnostic tests for neck and upper extremity problems. In: Watkins RG, editor. The Spine in Sports. St Louis, MO: Mosby-Year Book Inc; 1996. pp. 71–81. [Google Scholar]
- 7.Butler DA. Mobilisation of the Nervous System. Melbourne, Australia: Churchill Livingstone; 1991. [Google Scholar]
- 8.Elvey RL. The investigation of arm pain: signs of adverse responses to the physical examination of the brachial plexus and related tissues. In: Boyling JD, Palastanga N, editors. Grieve’s Modern Manual Therapy: The Vertebral Column. 2. Edinburgh: Churchill Livingstone; 1994. pp. 577–585. [Google Scholar]
- 9.Evans RC, Evans RC. Illustrated Orthopedic Physical Assessment. 3. St Louis, MO: Mosby/Elsevier; 2009. [Google Scholar]
- 10.Farmer JC, Wisneski RJ. Cervical spine nerve root compression: an analysis of neuroforaminal pressures with varying head and arm positions. Spine (Phila Pa 1976). 1994;19:1850–1855. doi: 10.1097/00007632-199408150-00010. [DOI] [PubMed] [Google Scholar]
- 11.Frymoyer JW. The Adult Spine: Principles and Practice. 2. Philadelphia, PA: Lippincott-Raven; 1997. [Google Scholar]
- 12.Han JJ, Kraft GH. Electrodiagnosis of neck pain. Phys Med Rehabil Clin N Am. 2003;14:549–567. doi: 10.1016/S1047-9651(03)00036-6. [DOI] [PubMed] [Google Scholar]
- 13.Hattori S, Oda H, Kawai S. Cervical intradiscal pressure in movements and traction of the cervical spine. Z Orthop. 1981;119:568–569. [Google Scholar]
- 14.Jahnke RW, Hart BL. Cervical stenosis, spondylosis, and herniated disc disease. Radiol Clin North Am. 1991;29:777–791. [PubMed] [Google Scholar]
- 15.Key CA. On paraplegia depending on disease of the ligaments of the spine. Guys Hosp Rep. 1838;3:17–34. [Google Scholar]
- 16.Levine MJ, Albert TJ, Smith MD. Cervical radiculopathy: diagnosis and nonoperative management. J Am Acad Orthop Surg. 1996;4:305–316. doi: 10.5435/00124635-199611000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Magee D. Orthopedic Physical Assessment. 2. Philadelphia, PA: WB Saunders; 1992. [Google Scholar]
- 18.Medical Research Council of the UK. Aids to the Investigation of Peripheral Nerve Injuries. Memorandum No. 45. London, UK: Pendragon House; 1976, 6–7.
- 19.Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med. 1934;211:210–215. doi: 10.1056/NEJM193408022110506. [DOI] [Google Scholar]
- 20.Partanen J, Partanen K, Oikarinen H, Niemitukia L, Hernesniemi J. Preoperative electroneuromyography and myelography in cervical root compression. Electromyogr Clin Neurophysiol. 1991;31:21–26. [PubMed] [Google Scholar]
- 21.Polston DW. Cervical radiculopathy. Neurol Clin. 2007;25:373–385. doi: 10.1016/j.ncl.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 22.Radhakrishnan K, Litchy WJ, O’Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy: a population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994;117:325–435. doi: 10.1093/brain/117.2.325. [DOI] [PubMed] [Google Scholar]
- 23.Semmes REMM. The syndrome of unilateral rupture of the sixth cervical intervertebral disk with compression of the seventh cervical nerve root: a report of four cases with symptoms simulating coronary disease. JAMA. 1943;121:1209–1214. doi: 10.1001/jama.1943.02840150023006. [DOI] [Google Scholar]
- 24.Shabat S, Leitner R, David R, Folman Y. The correlation between Spurling test and imaging studies in detecting cervical radiculopathy. J Neuroimaging. 2011 Sep 1. [Epub ahead of print]. [DOI] [PubMed]
- 25.Shafaie FF, Wippold FJ 2nd, Gado M, Pilgram TK, Riew KD. Comparison of computed tomography myelography and magnetic resonance imaging in the evaluation of cervical spondylotic myelopathy and radiculopathy. Spine (Phila Pa 1976). 1999;24:1781–1785. [DOI] [PubMed]
- 26.Shah KC, Rajshekhar V. Reliability of diagnosis of soft cervical disc prolapse using Spurling’s test. Br J Neurosurg. 2004;18:480–483. doi: 10.1080/02688690400012350. [DOI] [PubMed] [Google Scholar]
- 27.Spurling RS, Scoville WB. Lateral rupture of the cervical intervertebral discs: a common cause of shoulder and arm pain. Surg Gynecol Obstet. 1944;78:350–358. [Google Scholar]
- 28.Stookey B. Compression of the spinal cord due to ventral extradural cervical chondromas: diagnosis and surgical treatment. Arch Neurol Psychiatry. 1928;20:275–291. [Google Scholar]
- 29.Tong HC, Haig AJ, Yamakawa K. The Spurling test and cervical radiculopathy. Spine (Phila Pa 1976). 2002;27:156–159. doi: 10.1097/00007632-200201150-00007. [DOI] [PubMed] [Google Scholar]
- 30.Viikari-Juntura E. Interexaminer reliability of observations in physical examinations of the neck. Phys Ther. 1987;67:1526–1532. doi: 10.1093/ptj/67.10.1526. [DOI] [PubMed] [Google Scholar]
- 31.Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine (Phila Pa 1976). 2003;28:52–62. doi: 10.1097/00007632-200301010-00014. [DOI] [PubMed] [Google Scholar]
- 32.Wainner RS, Gill H. Diagnosis and non-operative management of cervical radiculopathy. J Orthop Sports Phys Ther. 2000;30:728–744. doi: 10.2519/jospt.2000.30.12.728. [DOI] [PubMed] [Google Scholar]
- 33.White AA, 3rd, Panjabi MM. Clinical Biomechanics of the Spine. 2. Philadelphia, PA: JB Lippincott Company; 1990. [Google Scholar]