Abstract
Background:
There is dearth of studies related to pattern of disability among persons who availed psychosocial rehabilitation services in India. We studied the pattern of disability among persons who availed half-way home-care services for psychosocial rehabilitation.
Materials and Methods:
Out of 130 case files of discharged patients, 50 files were randomly selected for data collection. Indian Disability Evaluation and Assessment Schedule was used to assess the pattern of disability in the sample.
Results:
The study revealed that only one-third (35%) of the residents had disability in self-care, 41% in communication and understanding and 47% in interpersonal relationship. Overall, majority (76%) of the respondents had moderate level of psychiatric disability at the time of discharge from half-way home. There was no significant relationship between gender and type of psychiatric illness with the level of disability. The overall disability correlated positively with the duration of illness (rs=0.39).
Conclusion:
Three-fourth of the residents who availed half-way home-care services had moderate level of disability.
Keywords: Disability, half-way home, psychiatric disorders, psychosocial rehabilitation
Family fellowship society (FFS) for psychosocial rehabilitation services is an initiative of families of persons suffering mental-illness, which has been advocating self-help movement on the part of the families on the lookout for alternatives care services. Over a period of 18 years, 130 families have availed the alternative care for psychosocial rehabilitation services for their wards. There is dearth of outcome studies on impact of psychosocial rehabilitation services for persons with psychiatric disability in India.
Chowdur et al.[1] reported significant improvement in self-care, communication, interpersonal relationship, vocational activities, family relations, and participation in community and leisure time activities from baseline to discharge among residents who underwent psychosocial rehabilitation program. Furthermore, those who attended a psychosocial rehabilitation program evidenced a greater improvement (54%) in quality of life compared to those who received standard care (34%), and the beneficial effect was maintained for over 2 years after completion of the program.[2] The quality of life in patients receiving home-care programs was significantly higher than those receiving half-way house service and the patients under home-care program showed improvement only for a short-period of time.[3] Studies have shown that majority of patients had success in independent living who underwent half-way home-care treatment and re-hospitalization rates were lower.[4,5,6,7,8,9,10]
In contrast, one study from Hong Kong found that majority of discharged psychiatric patients from a half-way home were having poor living condition, inadequate social life and overall poor quality of life.[11] Cometa et al.[12] in their critical review of half-way house outcomes studies, concluded that the effectiveness of half-way houses in facilitating the independent functioning of psychiatric patients in the community is open to question because of insufficiency in the areas of community adjustment, individual autonomy and employment. Cournos[13] stated that most studies reported environmental variables were better predictors of outcome of psychiatric residential care program than the patient variables. The success of the psychosocial rehabilitation depends upon the processes bridging the half-way house with the outside world.[14] The current study looked into the pattern of disability among persons who availed half-way home-care services for psychosocial rehabilitation services.
MATERIALS AND METHODS
Study design
This observational study was carried out at FFS for psychosocial rehabilitation services, Lakshmi Sagara Village, Anekal Taluk, Bangalore rural district of Karnataka, run by the families of mentally-ill with the help of mental-health professionals and organizations in this field since 1992. The study was approved by local Ethics Committee. Fifty case files were randomly selected from the discharged patients list out of 130 persons who availed alternative care services from 1994 to 2007 at the center using lottery method. Content analysis research design was used in this retrospective file review. All data was collected by second author, SE. Observation notes by nurse, progression notes by social workers and consultation notes by psychiatrist in the file were taken into consideration for purpose of data collection. Information in the case files regarding the residents self-care, interpersonal relationship, communication and understanding, and their behavior problems were corroborated with the staff members of the half-way home.
Therapeutic programs for the clients and family members
Various therapeutic programs such as casework intervention, group and family therapy, social skills and independent living skills training, referral and continuity of care services, vocational guidance, and supported employment were provided to the clients. Family members were trained to equip themselves to address the issues on minimizing the dependency of the patient, identifying their residual abilities, reducing the burden on their families, making them aware of welfare measures provided by the central and state government and the need for joining self-help groups. The basic requirements of rehabilitation intervention were addressed without compromising the quality of services. It was economically viable for families from poor socio-economic strata; per day expenditure cost Rs. 100, compared to Rs. 400 per day in the well-established psychosocial rehabilitation centers in and around Bangalore.
Tools
A pro-forma specially designed for the study was used to gather socio-demographic and clinical details. Indian Disability Evaluation and Assessment Schedule (IDEAS)[15] was used to assess the level of disability of the participants. It has four items: Self-care, interpersonal activities (social relationships), communication and understanding, and work. Each item is scored between 0 (no disability) to 4 (profound disability). Total disability score is the sum of scores on all four items. Global disability score is calculated by adding the total disability score and months in 2 years (MI2Y) score – a score ranging between 1 and 4, depending on the number of months in the last 2 years the patient exhibited symptoms).
Statistical analysis
Data were analyzed using student t-test, Chi-square test (or Fisher's exact test), Kruskal–Wallis test, Spearman's correlation, and linear regression analysis. The level of significance was set at P<0.05 (two-tailed).
RESULTS
Socio-demographic and clinical profile
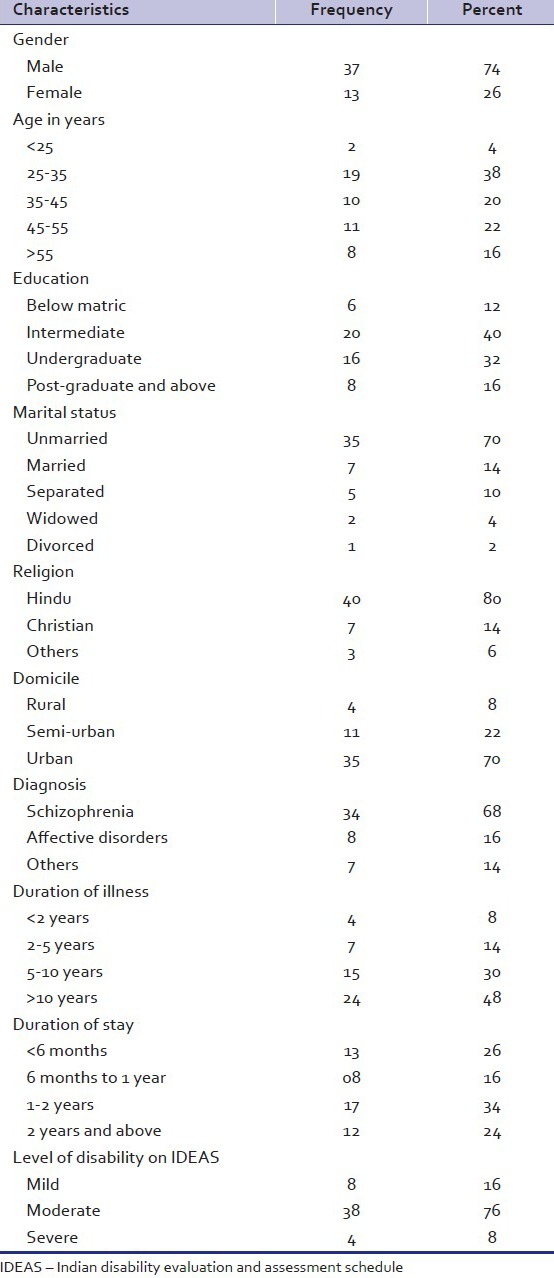
The sample characteristics have been summarized in Table 1. The mean age of the clients was 40 (±13) years and ranged from 19 to 71 years. Three-fourth of the sample was males and nearly half of them (40%) had 10-12 years of formal education. Majority (65%) of the clients was never employed due to the early onset of mental-illness whereas the rest lost their job due to long standing illness. More than half (54%) of the residents were referred by mental-health professionals from National Institute of Mental Health and Neurosciences (NIMHANS). Majority (78%) were from Karnataka, 22% from other states (including 12% from North India). The illness duration ranged from 2 to 35 years with a mean of 16 years, and majority had illness duration of more than 10 years. Average duration of their stay was 18 months. One-third (30%) of persons’ financial needs and care giving needs were looked after by their siblings followed by fathers constituting 12%, mothers 10%, 4% spouses, 2% cousins, and friends.
Table 1.
Sample characteristics
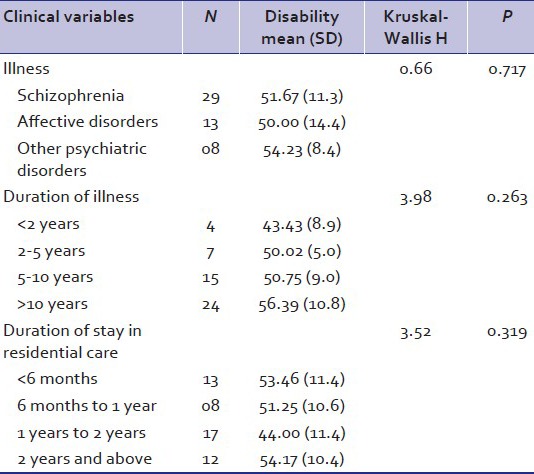
The mean disability score among male and female residents was 51 (±11) and 53 (±12), respectively [Table 2]. There was no significant difference across gender with regard to overall disability (t=0.50, P=0.620). Nearly, one-third of the residents (23%) showed complete improvement in self-care, nearly half (46%) had mild disability and remaining one-third (29%) had moderate disability in self-care at the time of discharge. 15% of the residents showed complete improvement in communication and understanding. Nearly, half of the respondents (44%) had mild disability and 40% had moderate in communication and understanding. 15% of the residents showed improvement in interpersonal relationships. More than one-third (38%) of the residents had mild disability and nearly, one-third (29%) of the residents had moderate disability and 19% of them had severe disability in interpersonal relationships. In summary, it can be said that 65% of the residents showed significant improvement in self-care, 59% of them in communication and understanding, 53% of them in interpersonal relationship. Majority (76%) of the respondents had moderate level of psychiatric disability at the time of discharge after their stay at half-way home.
Table 2.
Group differences in mean disability scores
Gender differences in disability
Self-care
One-fourth of the male residents showed complete improvement in self-care, 42% had mild disability, 31% had moderate disability, whereas, 17% of the female residents showed complete improvement, more than half of them (58%) had mild disability and one-fourth (25%) had moderate disability. The difference was not statistically significant (χ2=0.44, P=0.503).
Communication and understanding
More male residents (17%) showed improvement in communication and understanding when compared to female residents (8%). Half of females (50%) had mild disability when compared to males (42%), and 42% of males had moderate disability compared to only one-third of the females (33%); the differences were not statistically significant (Fisher's exact P=0.313).
Interpersonal relationship
More male residents (17%) showed improvement and did not have disability in interpersonal relationship when compared to female residents (8%). More than one-third of the male (39%) and one-third (33%) female residents had mild disability. More male residents (31%) had moderate disability when compared to females (25%). One-third of the female residents have severe disability when compared to 14% of the males.
Association of disability with socio-demographic and clinical variables
Kruskal–Wallis test revealed that there was no difference between the schizophrenia, affective disorders, and other disorders with regard to level disability among residents at the time of discharge from half-way home. Duration of illness, duration of stay in residential care services did not have any influence on pattern of disability at the time of discharge from half-way home. Spearman's correlation analysis revealed that there was positive correlation between duration of illness and the overall level of disability (rs=0.39, P=0.014). It also showed that age and education were not related to pattern of disability. Subsequently, linear regression analysis revealed that duration of illness predicts 20% of variation in level of disability in residents availing half-way home-care services (R2=0.202, t=3.22, P=0.002).
Behavioral problems among inmates
Most of the inmates had either one or the other following behavioral problems such as lack of initiative, drowsiness, suicidal tendency, aggressive, irritable, talking to self, drooling of mouth, compulsive washing, poor personal hygiene, smoking, suspiciousness, loss of sleep, frequent bathing, frequent urination, decreased food intake, poor drug compliance, poor socialization, restlessness, wandering and escaping tendency, and lack of interest in vocational activities.
DISCUSSION
In this study, mean age of the inmates was 40 (±13) years, which was similar to that of the study by Kamlesh et al.[16] where the mean age of residents who were undergoing psychosocial rehabilitation services was 37 (±8) years. In the present study, male residents (76%) out-numbered female respondents (24%). This finding was very similar to the findings reported by Chowdur et al.[1] in their study 74% of the male and 26% of the female availed half-way home-care services, whereas, Kamlesh et al.[16] study reported that 63% were males and 37% were females.
Mean years of education of the residents was 13 (±4) years; this in concordance with Kamlesh et al.[16] study where they reported it was 14 (±2) years. Present study had shown majority of the inmates had average illness duration of more than 10 years. This finding was in concordance with the Chowdur et al.[1] in contrast, Kamlesh et al.[16] study reported mean duration of illness to be 15 (±7) years. More than half of the residents who availed half-way home-care services were diagnosed to have schizophrenia (58%) followed by affective disorders (26%), the most common conditions requiring rehabilitation services. Our study found that at the time of discharge, majority (76%) were having moderate of level of disability. This is in concordance with Praveen et al.[17] study who reported that majority of the inmates were having moderate level of disability at the time of discharge from half-way home.
This model of FFS would ease the burden of the families who have been on the lookout for alternatives to home-care services. It was observed that this residential care rehabilitation services would be viable and economical for the population hailing from lower- and middle-socio-economic strata. Collaborative efforts of mental-health professionals and family forums would ensure the quality of life of persons with mental-illness. By and large, the active participation of family members in the programs of this kind, would eradicate the stigma attached to the mental illness.
The major limitation of our study was its retrospective nature. Baseline data on level of disability at the time of admission was not available in the case files. Furthermore, IDEAS was not a suitable tool measure the work domain of the half-way home residents at the time of discharge, because of which most of the residents scored severe disability in the domain of work. In future, outcome studies can be undertaken to find the factors associated with the outcome of the psychosocial rehabilitation services in a half-way home. However, the replication of FFS model had got multifarious limitation at present; the preparation of family forums to address the felt needs in collaboration with the mental-health professionals would certainly pave way for better outcome of schizophrenia illness and enhancing the quality of life persons with mental-illness.
CONCLUSION
Three-fourth of the residents availing half-way home-care services had moderate level of disability. It was found that majority of the beneficiaries are from mild to moderate category of disability. The welfare states need to motivate and encourage the family forums to participate actively along with mental-health professionals at every mental-health services, thereby to ensure the quality of services for the facilitating the quality of life as well.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Chowdur R, Dharitri R, Kalyanasundaram S, Suryanarayana RN. Efficacy of psychosocial rehabilitation program: The RFS experience. Indian J Psychiatry. 2011;53:45–8. doi: 10.4103/0019-5545.75563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whitty P, Lydon C, Turner N, O’Callaghan E. The influence of psychosocial rehabilitation on patients with a first episode of psychosis. Int J Psychosoc Rehabil. 2006;10:17–27. [Google Scholar]
- 3.Shu BC, Lung FW, Lu YC, Chase GA, Pan P. Care of patients with chronic mental illness: Comparison of home and half-way house care. Int J Soc Psychiatry. 2001;47:52–62. doi: 10.1177/002076400104700205. [DOI] [PubMed] [Google Scholar]
- 4.Meissner A. Rehabilitation of psychiatric patients by half-way house admission – A catamnestic study. Rehabilitation (Stuttg) 1998;37:199–204. [PubMed] [Google Scholar]
- 5.Holman T, Shore MF. Halfway house and family involvement as related to community adjustment for ex-residents of a psychiatric halfway house. J Community Psychol. 1978;6:123–9. doi: 10.1002/1520-6629(197804)6:2<123::aid-jcop2290060204>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 6.Rog DJ, Raush HL. The psychiatric halfway house: How is it measuring up? Community Ment Health J. 1975;11:155–62. doi: 10.1007/BF01420353. [DOI] [PubMed] [Google Scholar]
- 7.Yeung FK, Chan SH. Clinical characteristics and objective living conditions in relation to quality of life among community-based individuals of schizophrenia in Hong Kong. Qual Life Res. 2006;15:1459–69. doi: 10.1007/s11136-006-0006-z. [DOI] [PubMed] [Google Scholar]
- 8.Pach J, Lodemann E. Rehabilitation of psychiatric patients in the halfway house – A 10-year retrospective study. Rehabilitation (Stuttg) 1999;38:233–9. [PubMed] [Google Scholar]
- 9.Friedlob SA, Janis GA, Deets-Aron C. A hospital-connected halfway house program for individuals with long-term neuropsychiatric disabilities. Am J Occup Ther. 1986;40:271–7. doi: 10.5014/ajot.40.4.271. [DOI] [PubMed] [Google Scholar]
- 10.Wilder JF, Gadlin W. A halfway house in a mental health center. Community Ment Health J. 1977;13:168–74. doi: 10.1007/BF01410886. [DOI] [PubMed] [Google Scholar]
- 11.Mak KY, Gow L. The living conditions of psychiatric patients discharged from half-way houses in Hong Kong. Int J Soc Psychiatry. 1991;37:107–12. doi: 10.1177/002076409103700205. [DOI] [PubMed] [Google Scholar]
- 12.Cometa MS, Morrison JK, Ziskoven M. Halfway to where? A critique of research on psychiatric halfway houses. J Community Psychol. 1979;7:23–7. doi: 10.1002/1520-6629(197901)7:1<23::aid-jcop2290070105>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 13.Cournos F. The impact of environmental factors on outcome in residential programs. Hosp Community Psychiatry. 1987;38:848–52. doi: 10.1176/ps.38.8.848. [DOI] [PubMed] [Google Scholar]
- 14.Brücher K. Therapy and daily life in a halfway house – Excerpts from an ethnography. Fortschr Neurol Psychiatr. 1988;56:193–203. doi: 10.1055/s-2007-1001784. [DOI] [PubMed] [Google Scholar]
- 15.Indian Disability Evaluation and Assessment Scale, 2002. Guidelines for evaluation and assessment of mental illness and procedure for certification. Published in the Gazette of India (Extraordinary) 2002. [2002 Feb 27]. Part I, Section I.
- 16.Kamlesh KS, Sophia CA, Dharitri R, Kalyanasundaram S. Met and unmet needs of persons with severe mental illness in a half way home. Int J Psychosoc Rehabil. 2010;15:13–22. [Google Scholar]
- 17.Praveen K, Gopinath R, Bhat SM. Self-stigma, self-esteem and recovery orientation among residents of a psychiatric rehabilitation centre. M. Phil. Phil Psychiatric Social Work Dissertation Submitted to Manipal University. 2011 [Google Scholar]


