Abstract
Abfraction (AF) is the pathological loss of tooth substance caused by biomechanical loading forces that result in flexure and failure of enamel and dentin at a location away from the loading. The theory of AF is based primarily on engineering analyses that demonstrate theoretical stress concentration at the cervical areas of the teeth. However, the theory is not yet proven and there are explanations against it. AF lesions present primarily at the cervical region of the dentition and are typically wedge-shaped, with sharp internal and external line angles. Diagnosis of AF plays a very important role in the management of patients. The aim of the present narrative review is to comprehensively discuss the historical, etiopathogenetic, clinical, and diagnostic and treatment aspects of AF.
Keywords: Abfraction, non-carious cervical lesion, pathogenesis, regressive alteration of teeth
INTRODUCTION
The loss of cervical tooth structure in the absence of caries is termed as a non-carious cervical lesion (NCCL), stress-induced cervical lesion, or abfraction (AF).[1] These lesions vary from shallow grooves to broad dished-out lesions or large wedge-shaped defects, with sharp internal and external line angles.[1,2] AF means ‘to break away’[3] and the term is derived from the Latin words ‘ab,’ or ‘away’ and ‘fractio,’ or ‘breaking’ by Grippo[4,5] It is usually observed on the buccal surface at the cementoenamel junction (CEJ) of the teeth, with prevalence ranging from 27 to 85%.[6]
HISTORY
The origin of non-carious cervical lesions (NCCLs) was revealed when Miller published an article in 1907, on experiments and observations on the wear of teeth variously designated as erosion, abrasion, chemical abrasion, denudation, and so on.[7] The concept that occlusal loading could cause cervical stress, resulting in loss of cervical tooth structure, began evolving in the late 1970s.[8,9,10] Historically, NCCLs have been classified according to their appearance: Wedge-shaped, disk-shaped, flattened, irregular, and figured areas.[1]
The term ‘abfraction’ has evolved from the studies by McCoy,[8] Lee and Eakle,[9] and Grippo.[4] It is described as a theoretical process by which occlusal forces create stresses in enamel and dentin along the cervical area and predispose it to erosion and abrasion. In the early 1980s, McCoy[8,11] questioned the role of toothbrush abrasion in the etiology of what previously had been referred to as ‘cervical erosion.’ Thus, McCoy,[8,11] and in the early 1990s, Grippo,[12] proposed that bruxism may be the primary cause of angled notches at the CEJ.
Grippo[12] concluded that the flexure resulted in damage to the enamel rods at the CEJ, resulting in their loosening and consequent flaking away of the tooth structure. He named this type of damage ‘abfraction’ in his article published in 1991. He suggested that AF is the basic cause of all NCCLs, whereas, Lee and Eakle[9] proposed a multifactorial etiology, with a combination of occlusal stress, abrasion, and erosion. Spranger[13] supported the multifactorial etiology of the cervical lesions and suggested that the wear was related to the anatomy, the distribution of forces calculated from the elastic deformation studies, development of caries, and occlusion and parafunction.
TERMINOLOGY
Grippo[14] has defined AF as the pathological loss of tooth substance caused by the biomechanical loading forces that result in flexure and failure of enamel and dentin at a location away from the loading. He first used the term ‘abfraction’ to refer to a process of cervical tooth structure loss, based on a study completed by McCoy[8] and Lee and Eakle.[9]
The contradictory terminologies for AF used in the literature reflect that the real etiology of AF remains obscure. Miller et al.,[15] stated that NCCLs are also called AF. This statement is misleading because NCCLs have a variety of possible etiologies, of which AF may be the primary one. It is also important to differentiate the term ‘stress corrosion’ from ‘AF’. Stress-corrosion refers to the synergistic effects of stress and corrosion acting simultaneously.[16]
According to Pindborg,[17] abrasion is the loss of tooth substance from factors other than tooth contact. Perceptions relating to the importance of abrasion are geographically polarized and conflict arises from a differing interpretation of the definitions relating to the etiology of tooth wear.[18]
Of late, new terms have been introduced to describe tooth wear. ‘Biodental engineering factors’[19] have been defined as the effect of piezoelectricity[20] at the cervical area, and ‘stress corrosion’[16] has been used to describe a multifactorial physiochemical degradation of the CEJ area. The ‘dental compression syndrome’ is tooth deformation related to malocclusion, parafunctional habits, and temporomandibular joint disorders.[21] It is important that oral health professionals understand that abfraction is still a theoretical concept, as it is not backed up by appropriate clinical evidence.[22]
ETIOPATHOGENESIS
It has been suggested that when a tooth is hyperoccluded, the masticatory forces are transmitted to this tooth, which in turn transfers this energy to the cervical region.[23,24,25,26] However, Gibbs et al.,[27] found that the occlusal force during swallowing and mastication is only approximately 40 percent of the maximal bite force. According to Suit et al.,[28] tooth contact occurs, on an average, for only 194 milliseconds during mastication and for 683 milliseconds during swallowing.
Lateral force produces compressive stress on the side toward which the tooth bends and the tensile stress is on the other side. These stresses create microfractures in the enamel or dentin at the cervical region. These fractures propagate in a direction perpendicular to the long axis of the tooth, leading to a localized defect around the CEJ.[26,29]
McCoy[8] proposed that bruxism could be the primary cause for abfraction, and tooth flexure from tensile stresses led to cervical tooth breakdown. Later, Lee and Eakle[9] hypothesized that the primary etiological factor in cervical lesions was the impact of tensile stress from mastication and malocclusion. The lesion is formed by combined bending and barreling deformations. This leads to alternating tensile and compressive stresses, resulting in weakening of the enamel and dentin. If the forces reach a fatigue limit, the tooth cracks or breaks. At the same time, the opposite region is under compressive stress. When the direction of the force changes, the tooth bends in the opposite direction, and the stresses correspondingly reverse at this cervical area. Thus, side-to-side bending of the tooth results in fatigue and fracture of the most-flexed zone. These interocclusal forces create physical microfractures or abfractions at the cervical region [Figures 1–2].
Figure 1.
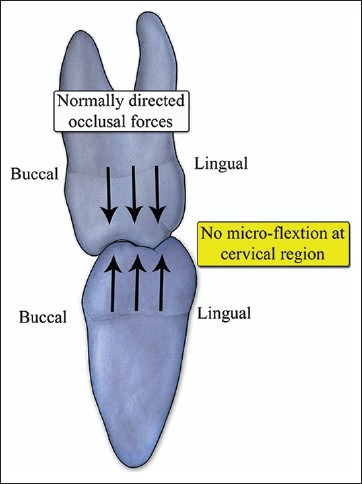
Normally directed occlusal forces on the mandibular molar showing no changes in the cervical region
Figure 2.

Etiopathogenesis of abfraction
Enamel is weak in tension,[30] and thus, the tensile forces may cause disruption of the hydroxyapitite (HA) crystals, allowing water and other small molecules to penetrate between the prisms and prevent re-establishment of the interprismatic bonds on release of the stress. Lee and Eakle[31] suggested that the cervical fulcrum area of a tooth might be subject to unique stress or torque resulting from occlusal function and parafunctional activity. These flexural forces then disrupt the normal crystalline structure.[13,31,32] This process renders these HA crystals more susceptible to chemical and mechanical destruction, and thus, result in AF. Ultimately, the enamel breaks away at the cervical margin and exposes the dentin, and the process continues in this manner.[1]
THEORY OF ABFRACTION
The theory of AF is based primarily on engineering analyses that demonstrate theoretical stress concentration at the cervical areas of the teeth. Few controlled studies demonstrate the relationship between occlusal loading and AF lesions. The role of occlusal loading in NCCLs appears to be part of a multifactorial event that may not necessarily follow the proposed classic AF mechanism.
Nearly all the research on the relationship between occlusal forces (bruxing) and cervical lesions shows that teeth do indeed flex in the cervical region under bruxing loads, but none seem to cite the actual damage caused by this deformation without an abrasive or erosive component being applied as well. Nevertheless, the AF theory argues that bruxing forces alone can cause the erosion of the tooth structure on the buccal surface, especially in the cervical region.[7]
Many dispute the theory of AF, blaming this type of damage on what is commonly called ‘toothbrush abrasion’.[9] This harks back to the early study of Miller, in 1917. However, it has been confirmed in the more recent studies by Abrahamsen,[33] which have shown that toothpaste (not the toothbrush) is abrasive enough to cause this type of damage if the patient is too aggressive in brushing the teeth in a very hard and vigorous ‘sawing’ motion. Abrahamson suggests that the term ‘toothbrush abrasion’ be replaced with the term ‘toothpaste abuse’.[9,33]
His studies using mechanical ‘tooth brushing’ machines have shown that the toothbrush alone does not cause this type of tooth damage, but the addition of toothpaste to the bristles does. Toothbrushes without toothpaste do cause soft tissue damage, and indeed, overly vigorous brushing of teeth without toothpaste leads to gingival recession.[33]
Grippo[4] has suggested that AF is the basic cause of all NCCLs. There is some evidence supporting the tooth flexure theory: Presence of class V non-carious lesions in some teeth, but the adjacent teeth (not subjected to lateral forces) are unaffected;[7,14] the lesions progress around restorations that remain intact and under the margins of complete crowns;[14] the lesions are rarely seen on the lingual aspect of the mandibular teeth.[7] However, other studies have proposed a combination of occlusal stress, parafunction, abrasion, and erosion in the development of lesions, leading to a conclusion that the progression of AF may be multifactorial.[13,31]
Romeed et al.,[34] investigated the biomechanics of abfraction lesions in the upper canine teeth under axial and lateral loading conditions, using a three-dimensional finite element analysis. It was found that the stresses were concentrated at the CEJ in all scenarios. Lateral loading produced the maximum stress, greater than axial loading, although the pulp tissues experienced minimum levels of stress.
Thus, the theory of AF is not yet proven. The evidence against the theory of AF is as follows:[7]
Few studies demonstrate that the occlusal loading is related to the AF lesions
Buccal surface is the most affected, while the lingual surface is the least affected. If flexure of the teeth is responsible, there would be equal damage to both buccal and lingual surfaces
There is little or no evidence of these lesions in prehistorical skulls. NCCLs are found in historical skulls of the sixteenth century (after the invention of tooth powders and toothbrushes)
Buccal surfaces of the premolars and the canines demonstrate worse lesions, as patients are likely to place the most brushing force on these surfaces. The lesions are progressively worse from the posterior to the anterior teeth
The damage does not progress beyond the gingival crest (instead of at the crest of the bone), which is where the theory suggests the flexure should be the worst
Not all persons with the lesions demonstrate occlusal wear (bruxing), and not all persons with severe occlusal wear exhibit NCCLs
Many cases show the absence of an antagonist to the affected tooth. If the damage continues, or the damage begins after the extraction of the antagonist, then bruxing cannot be the cause.
CLINICAL FEATURES
Abfraction lesions present primarily at the cervical region of the dentition and are typically wedge-shaped, with sharp internal and external line angles [Figure 3]. Subgingival lesions have also been observed.[1] In theory, the shape and size of the lesion are dictated by the direction, magnitude, frequency, duration, and location of forces that arise when the teeth come in contact.[35]
Figure 3.

Abfraction showing various degrees of severity
Lee and Eakle[9] first described the characteristics of the lesions resulting from tensile stresses. They concluded that an AF lesion should be located at or near the fulcrum in the region of greatest tensile stress concentration, be wedge-shaped, and display a size proportional to the magnitude and frequency of the tensile force application [Figure 3].
They proposed that the direction of the lateral forces acting on a tooth, determines the location of the lesion. Two or more lateral forces result in an NCCL composed of two or more overlapping wedge-shaped NCCLs. AF is postulated to be responsible for the chronic sensitivity of the teeth to cold foods and liquids.[9,22]
Non-carious cervical lesions are very common on the anterior and premolar teeth, because of the smaller size of the teeth,[35,36] and are more frequently found on the buccal or lingual surfaces due to the direction of the occlusal or incisal loads, the angling and asymmetry of the tooth buccal–lingual plane, and its relationship with the supporting alveolar bone.[37,38]
The Tooth Wear Index proposed by Smith and Knight[39] is the most accepted index to categorize tooth wear in the cervical region, and it is as follows:
The classifications on this index are as follows [Figure 4]:
Figure 4.
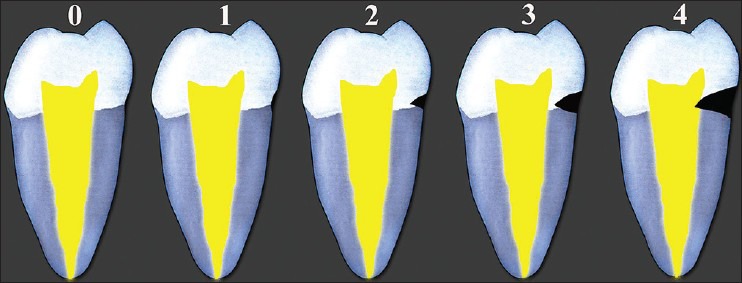
Tooth Wear Index proposed by Smith and Knight
0 = No change in contour
1 = Minimal loss of contour
2 = Defect <1 mm deep
3 = Defect 1 mm to 2 mm deep
4 = Defect >2 mm deep, or pulp exposure, or exposure of secondary dentin.
The following clinical points can be used to diagnose abfraction:
NCCL involving a single tooth [Figure 3] (toothbrush abrasion involves multiple teeth)
Malposed involved tooth
Faulty restoration of an antagonist
Presence of a cervical lesion below the gingival margin, the area which is normally protected from abrasive action
History of bruxism or parafunctional habits.
TREATMENT
Determination of the activity of an AF lesion can be done by using No. 12 scalpel blade. Loss of a scratch made by the blade signifies an active AF lesion. In an attempt to reproduce the phenomenon of stress distribution in teeth and their anatomic support structures, a variety of methodologies have been used.[3] The engineering studies cited by McCoy[8,11] and Lee and Eakle[9] employed finite elemental analysis (FEA), or photoelastic methods. They used computerized geometric or plastic models, respectively. By using FEA, each factor can be rapidly modified and the stress distribution can be investigated in two-dimensional (2D) or three-dimensional (3D) models.[38]
When an AF lesion is less than 1 mm in depth,[22] only monitoring at regular intervals is sufficient. Restoring NCCLs improves the maintenance of oral hygiene by the patient. It also helps in decreasing thermal sensitivity, improving esthetics, and strengthening the teeth. Along with restoration, a variety of treatment strategies have also been proposed like occlusal adjustments, occlusal splints, elimination of parafunctional habits,[14,40] altering tooth brushing techniques, and the like.
For restoring AF, many materials and techniques have been tried to date. The following materials are indicated for restoring the lesions: Glass Ionomer cements (GICs), Resin-Modified GICs (RMGICs), Polyacid-modified resin-based composites (compomers), composite resins, and a combination of the techniques.[41,42,43] According to Tay,[44] RMGIC should be the first preference. An RMGIC/GIC liner or a base with a resin composite should be used wherever esthetics is required.
The most important criterion for restoration is that of retention. Clinical studies have shown that restorations of AF lesions have a higher percentage of failure in the cervical area.[45] Restorations tend to pop off due to the constant deformation of the tooth structure caused by parafunctional habits. As these lesions implicate enamel and dentin margins, they represent a challenge to the dental profession. Heymann et al.[46] reported the association of occlusion, tooth location, and patient's age, with loss of retention, while others blame the technique, marginal shrinkage, properties of the bonding agent, and inadequate adhesive resin thickness for the retention loss.[47,48,49,50,51,52]
Dental hard structures react independently to masticatory stresses. Dentin shows low compressive and high tensile stresses at the CEJ, while enamel demonstrates a reverse trend.[53] Dentin is subjected to continuous changes in composition and microstructure, owing to both physiological and pathological influences.[54,55,56] NCCLs exhibit an increased amount of sclerotic dentin and thus have low permeability and hypermineralization, resulting in a surface that is unsuitable for adhesive bonding agents.[57,58] NCCLs facilitate further tooth structure deterioration because of stress concentration.
The current adhesive systems interact with the enamel/dentin using two different techniques; either the etch-and-rinse technique or the self-etch technique. The main reason for the failure of restoration is, difficulty in gaining and maintaining a good seal between the restoration and tooth at the margin.[3,59] The retention rate for restorations with a lower elastic modulus may be significantly better than that for a material with a higher elastic modulus.[46]
Microfilled composites demonstrated a greater elasticity than hybrid composites. Most of the transferred energy was absorbed by the restoration rather than transmitted to the dentin-restoration interface.[26,43,46] However, no significant difference was found in the parameters of retention, recurrent caries, staining or color match in a study comparing GICs and composites, but there was greater surface roughness in the GIC restorations.[60] Matis et al.,[61] found that retention was the same for GIC and microfilled resin. GICs were found to perform better than the composites[62,63] because of their greater resilience in allowing the material to flex with the tooth. RBGICs give better esthetic results than conventional GICs.[60]
Archaeological importance
Studies on precontemporary populations showed an absence of NCCLs in them. No NCCLs were seen in Ancient American skulls or prehistoric and historical skeletal remains from the south of France.[64,65] Interproximal cervical grooving has been observed in pre-contemporary Australian Aboriginals. The lesions were suspected to result from passing an animal tendon between the teeth).[66] Thus, the population demonstrated lack of NCCLs.[67] NCCLs are found in the historical skulls of the sixteenth century, that is, after the invention of tooth powders and toothbrushes.[7]
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Barttlet DW, Shah P. A critical review of non-carious cervical (wear) lesions and the role of abfraction, erosion, and abrasion. J Dent Res. 2006;85:306–12. doi: 10.1177/154405910608500405. [DOI] [PubMed] [Google Scholar]
- 2.Pereira AF, Poiate IA, Poiate E, Jr, Miranda WG., Jr Abfraction lesions reviewed: Current concepts. RGO (Porto Alegre) 2008;56:321–6. [Google Scholar]
- 3.Braem M, Lambrechts P, Vanherle G. Stress-induced cervical lesions. J Prosthet Dent. 1992;67:718–22. doi: 10.1016/0022-3913(92)90178-d. [DOI] [PubMed] [Google Scholar]
- 4.John GO. Abfractions: A new classification of hard tissue lesions of teeth. J Esthet Dent. 1991;3:14–9. doi: 10.1111/j.1708-8240.1991.tb00799.x. [DOI] [PubMed] [Google Scholar]
- 5.Litonjua LA, Andreana S, Bush PJ, Tobias TS, Cohen RE. Noncarious cervical lesions and abfractions: A re-evalution. J Am Dent Assoc. 2003;134:845–50. doi: 10.14219/jada.archive.2003.0282. [DOI] [PubMed] [Google Scholar]
- 6.Levitch LC, Bader JD, Shugars DA, Heymann HO. Non-carious cervical lesions. J Dent. 1994;22:195–207. doi: 10.1016/0300-5712(94)90107-4. [DOI] [PubMed] [Google Scholar]
- 7. [Last accessed on 2013 Nov 12]. Available from: http://www.doctorspiller.com/Tooth_wear/attrition2.htm .
- 8.McCoy G. The etiology of gingival erosion. J Oral Implantol. 1982;10:361–2. [PubMed] [Google Scholar]
- 9.Lee WC, Eakle WS. Possible role of tensile stress in the etiology of cervical erosive lesions of teeth. J Prosthet Dent. 1984;52:374–80. doi: 10.1016/0022-3913(84)90448-7. [DOI] [PubMed] [Google Scholar]
- 10.Brady JM, Woody RD. Scanning microscopy of cervical erosion. J Am Dent Assoc. 1977;94:726–9. doi: 10.14219/jada.archive.1977.0345. [DOI] [PubMed] [Google Scholar]
- 11.McCoy G. On the longevity of teeth. J Oral Implantol. 1983;11:248–67. [PubMed] [Google Scholar]
- 12.Grippo JO. Tooth flexure. J Am Dent Assoc. 1991;122:13. doi: 10.14219/jada.archive.1991.0226. [DOI] [PubMed] [Google Scholar]
- 13.Spranger H. Investigation into the genesis of angular lesions at the cervical region of teeth. Quintessence Int. 1995;26:149–54. [PubMed] [Google Scholar]
- 14.Grippo JO. Noncarious cervical lesion the decision to ignore or restore. J Esthet Dent. 1992;4:55–64. doi: 10.1111/j.1708-8240.1992.tb00721.x. [DOI] [PubMed] [Google Scholar]
- 15.Miller N, Penaud J, Ambrosini P, Bisson-Boutelliez C, Briancon S. Analysis of etiologic factors and periodontal conditions involved with 309 abfractions. J Clin Periodontol. 2003;30:828–32. doi: 10.1034/j.1600-051x.2003.00378.x. [DOI] [PubMed] [Google Scholar]
- 16.Grippo JO, Simring M. Dental ‘erosion’ revisited. J Am Dent Assoc. 1995;126:619–20. doi: 10.14219/jada.archive.1995.0241. [DOI] [PubMed] [Google Scholar]
- 17.Pindborg JJ. 1st ed. Copenhagen: Munksgaard; 1970. Pathology of the dental hard tissues. [Google Scholar]
- 18.Bartlett D, Phillips K, Smith BG. A difference in perspective–the North American and European interpretations of tooth wear. Int J Prosthodont. 1999;12:401–8. [PubMed] [Google Scholar]
- 19.Grippo JO, Masi JV. Role of biodental engineering factors (BEF) in the etiology of root caries. J Esthet Dent. 1991;3:71–6. doi: 10.1111/j.1708-8240.1991.tb00813.x. [DOI] [PubMed] [Google Scholar]
- 20.Grippo JO, Masi JV. The role of stress corrison and piezoelectricity in the formation of root caries. In: Foster RR, editor. Vol. 1. Philadelphia, PA: 13th bioengineering conference; University of Pennsylyania; 1987. pp. 93–5. [Google Scholar]
- 21.McCoy G. Dental compression syndrome: A new look at an old disease. J Oral Implantol. 1999;25:35–49. doi: 10.1563/1548-1336(1999)025<0035:DCSANL>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Michael JA, Townsend GC, Greenwood LF, Kaidonis JA. Abfraction: Separating fact from fiction. Aust Dent J. 2009;54:2–8. doi: 10.1111/j.1834-7819.2008.01080.x. [DOI] [PubMed] [Google Scholar]
- 23.Grippo JO, Simring M, Schreiner S. Attrition, abrasion, corrosion and abfraction revisited: A new perspective on tooth surface lesions. J Am Dent Assoc. 2004;135:1109–18. doi: 10.14219/jada.archive.2004.0369. [DOI] [PubMed] [Google Scholar]
- 24.Rees JS. A Review of biomechanics of abfraction. Eur J Prosthodont Restor Dent. 2000;8:139–44. [PubMed] [Google Scholar]
- 25.Hood JA. Experimental studies on tooth deformation: Stress distribution in class V restorations. N Z Dent J. 1972;68:116–31. [PubMed] [Google Scholar]
- 26.Leinfelder KF. Restoration of abfracted lesions. Compendium. 1994;159:1396–400. [PubMed] [Google Scholar]
- 27.Gibbs CH, Mahan PE, Lundeen HC, Brehnan K, Walsh EK, Holbrook WB. Occlusal forces during chewing and swallowing as measured by sound transmission. J Prosthet Dent. 1981;46:443–9. doi: 10.1016/0022-3913(81)90455-8. [DOI] [PubMed] [Google Scholar]
- 28.Suit SR, Gibbs CH, Benz ST. Study of gliding contacts during mastication. J Periodontol. 1976;47:331–4. doi: 10.1902/jop.1976.47.6.331. [DOI] [PubMed] [Google Scholar]
- 29.Tanaka M, Naito T, Yokota M. Finite element analysis of the possible mechanism of cervical lesion formation by occlusal force. J Oral Rehabil. 2003;30:60–7. doi: 10.1046/j.1365-2842.2003.00959.x. [DOI] [PubMed] [Google Scholar]
- 30.Powers JM, Craig RG, Ludema KC. Frictional behavior and surface failure of human enamel. J Dent Res. 1973;52:1327–31. doi: 10.1177/00220345730520063001. [DOI] [PubMed] [Google Scholar]
- 31.Lee WC, Eakle WS. Stress-induced cervical lesions: Review of advances in the past 10 years. J Prosthet Dent. 1996;75:487–94. doi: 10.1016/s0022-3913(96)90451-5. [DOI] [PubMed] [Google Scholar]
- 32.De Las Casas EB, Cornacchia TP, Gouvea PH, Cimini CA. Abfraction and anisotropy–effects of prism orientation on stress distribution. Comput Methods Biomech Biomed Engin. 2003;6:65–73. doi: 10.1080/1025584021000043357. [DOI] [PubMed] [Google Scholar]
- 33.Abrahamsen TC. The worn dentition – pathognomonic patterns of abrasion and erosion. Int Dent J. 2005;55:268–76. doi: 10.1111/j.1875-595x.2005.tb00064.x. [DOI] [PubMed] [Google Scholar]
- 34.Romeed SA, Malik R, Dunne SM. Stress analysis of occlusal forces in canine teeth and their role in the development of non-carious cervical lesions: Abfraction. Int J Dent 2012. 2012 doi: 10.1155/2012/234845. 234845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bradley T, Piotrowski, William B, Gillette, Everett B Hancock. Examining the prevalence and characteristics of abfraction like cervical lesions in a population of US veterans. J Am Dent Assoc. 2001;132:1694–701. doi: 10.14219/jada.archive.2001.0122. [DOI] [PubMed] [Google Scholar]
- 36.Khan F, Young WG, Shahabi S, Daley TJ. Dental cervical lesions associated with occlusal erosion and attrition. Aust Dent J. 1999;443:176–86. doi: 10.1111/j.1834-7819.1999.tb00219.x. [DOI] [PubMed] [Google Scholar]
- 37.Borcic J, Anic I, Smojver I, Catic A, Miletic I, Ribaric PS. 3D finite element model and cervical lesion formation in normal occlusion and in malocclusion. J Oral Rehabil. 2005;32:504–10. doi: 10.1111/j.1365-2842.2005.01455.x. [DOI] [PubMed] [Google Scholar]
- 38.Ichim I, Schmidlin PR, Kieser JA, Swain MV. Mechanical evaluation of cervical glass-ionomer restorations: 3D finite element study. J Dent. 2007;351:28–35. doi: 10.1016/j.jdent.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 39.Smith BG, Knight JK. An index for measuring the wear of teeth. Br Dent J. 1984;156:435–8. doi: 10.1038/sj.bdj.4805394. [DOI] [PubMed] [Google Scholar]
- 40.Lyttle HA, Sidhu N, Smyth B. A study of the classification and treatment of noncarious cervical lesions by general practitioners. J Prosthet Dent. 1998;793:342–6. doi: 10.1016/s0022-3913(98)70248-3. [DOI] [PubMed] [Google Scholar]
- 41.Fruits TJ, VanBrunt CL, Khajotia SS, Duncanson MG., Jr Effect of cyclical lateral forces on microleakage in cervical resin composite restorations. Quintessence Int. 2002;33:205–12. [PubMed] [Google Scholar]
- 42.Li Q, Jepsen S, Albers HK, Eberhard J. Flowable materials as an intermediate layer could improve the marginal and internal adaptation of composite restorations in Class-V-cavities. Dent Mater. 2006;22:250–7. doi: 10.1016/j.dental.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 43.Peaumans M, De Munck J, Landuyt V, Kanumilli P, Yoshida Y, Inoue S. Restoring cervical lesions with flexible composites. Dent Mater. 2007;23:749–54. doi: 10.1016/j.dental.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 44.Tay FR, Gwinnett AJ, Pang KM, Wei SH. Structural evidence of a sealed tissue interface with a total etch wet bonding technique in vivo. J Dent Res. 1994;73:629–36. doi: 10.1177/00220345940730030801. [DOI] [PubMed] [Google Scholar]
- 45.Brackett MG, Dib A, Bracket WW, Estrada BE, Reyes AA. One year clinical performance of a resin modigied glass inomoer and a resin composite restorative material in unprepared class V restorations. Oper Dent. 2002;27:112–6. [PubMed] [Google Scholar]
- 46.Heymann HO, Sturdevant JR, Bayne SC, Wilder AD, Sluder TB, Brunson WD. Examining tooth flexure effects on cervical restorations: A two-year clinical study. J Am Dent Assoc. 1991;122:41–7. doi: 10.1016/s0002-8177(91)25015-1. [DOI] [PubMed] [Google Scholar]
- 47.Brackett WW, Gilpatrick RO, Browning WD, Gregory PN. Two year clinical performance of a resin-modified glass-ionomer restorative material. Oper Dent. 1999;24:9–13. [PubMed] [Google Scholar]
- 48.Hansen EK. Five-year study of cervical erosions restored with resin and dentin-bonding agent. Scand J Dent Res. 1992;100:244–7. doi: 10.1111/j.1600-0722.1992.tb01751.x. [DOI] [PubMed] [Google Scholar]
- 49.Sidhu SK. A comparative analysis of techniques of restoring cervical lesions. Quintessence Int. 1993;24:553–9. [PubMed] [Google Scholar]
- 50.Van Dijken JW. Clinical evaluation of four dentin bonding agents in class V abrasion lesions: A four-year follow-up. Dent Mater. 1994;10:319–24. doi: 10.1016/0109-5641(94)90040-x. [DOI] [PubMed] [Google Scholar]
- 51.Maneenut C, Tyas MJ. Clinical evaluation of resin-modified glassionomer restorative cements in cervical ‘abrasion’ lesions: One-year results. Quintessence Int. 1995;26:739–43. [PubMed] [Google Scholar]
- 52.Neo J, Chew CL, Yap A, Sidhu S. Clinical evaluation of tooth colored materials in cervical lesions. Am J Dent. 1996;9:15–8. [PubMed] [Google Scholar]
- 53.Goel VK, Khera SC, Singh K. Clinical implications of the response of enamel and dentin to masticatory loads. J Prosthet Dent. 1990;64:446–54. doi: 10.1016/0022-3913(90)90041-a. [DOI] [PubMed] [Google Scholar]
- 54.Pashley DH. Dentin: A dynamic substrate: A review. Scanning Microsc. 1989;3:161–74. [PubMed] [Google Scholar]
- 55.Stanley HR, Pereira JC, Spiegel E, Broom C, Schultz M. The detection and prevalence of reactive and physiologic sclerotic dentin, reparative dentin and dead tracts beneath various types of dental lesions according to tooth surface and age. J Oral Pathol. 1983;12:257–89. doi: 10.1111/j.1600-0714.1983.tb00338.x. [DOI] [PubMed] [Google Scholar]
- 56.Duke ES, Lindemuth J. Variability of clinical dentin substrates. Am J Dent. 1991;4:241–6. [PubMed] [Google Scholar]
- 57.Burrow MF, Takakura H, Nakajima M, Inai N, Tagami J, Takatsu T. The influence of age and depth of dentin on bonding. Dent Mater. 1994;10:241–6. doi: 10.1016/0109-5641(94)90068-x. [DOI] [PubMed] [Google Scholar]
- 58.Tagami J, Hosoda H, Burrow MF, Nakajima M. Effect of aging and caries on dentin permeability. Proc Finn Dent Soc. 1992;88:149–54. [PubMed] [Google Scholar]
- 59.Van Meerbeek BV, De Munck J, Yoshida Y, Inoue S, Vargas M, Vijay P. Adhesion to enamel and dentin: Current status and future challenges. Oper Dent. 2003;28:215–35. [PubMed] [Google Scholar]
- 60.Burke FJ, Whitehead SA, McCauguey AD. Contemporary concepts in the pathogenesis of the Class V non-carious lesion. Dent Update. 1995;22:28–32. [PubMed] [Google Scholar]
- 61.Matis BA, Cochran MA, Platt JA, Oshida Y, Choi K. Microtensile bond strength of GIC to artificially created carious dentin. Oper Dent. 2006;31:590–7. doi: 10.2341/05-108. [DOI] [PubMed] [Google Scholar]
- 62.Tyas MJ. Clinical evaluation of glass-ionomer cement resorations. J Appl Oral Sci. 2006;14:10–3. doi: 10.1590/s1678-77572006000700003. [DOI] [PubMed] [Google Scholar]
- 63.Lambrechts P, Braem M, Vanherle G. Evaluation of clinical performance for posterior composite resin adhesives. Oper Dent. 1987;12:53–78. [PubMed] [Google Scholar]
- 64.Aaron GM. M.S. thesis. Florida: The University of Florida; 2004. The prevalence of non-carious cervical lesions in modern and ancient American skulls: Lack of evidence for an occlusal aetiology. [Google Scholar]
- 65.Aubry M, Mafart B, Donat B, Brau JJ. Brief communication: Study of noncarious cervical tooth lesions in samples of prehistoric, historic, and modern populations from the South of France. Am J Phys Anthropol. 2003;121:10–4. doi: 10.1002/ajpa.10210. [DOI] [PubMed] [Google Scholar]
- 66.Brown T, Molnar S. Interproximal grooving and task activity in Australia. Am J Phys Anthropol. 1990;81:545–53. doi: 10.1002/ajpa.1330810410. [DOI] [PubMed] [Google Scholar]
- 67.Kaidonis JA. Tooth wear: The view of the anthropologist. Clin Oral Investig. 2008;12:S21–6. doi: 10.1007/s00784-007-0154-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


