Abstract
Primary non-Hodgkin's lymphoma (NHL) is a rare entity. When it does occur, mandibular NHL typically manifests similar to an odontogenic pathology. This results in delayed diagnosis and treatment. We present a 50-year-old female who was erroneously treated for a pyogenic granuloma several months before the correct diagnosis of extranodal primary NHL of the oral cavity was made. Fortunately, the solitary bony lymphoma had not disseminated and management by chemo-radiation allowed for disease eradication and new post-treatment bone formation. The purpose of this report is to describe a rare case of primary NHL of the mandible, explore the diagnosis and work-up and discuss treatment strategies. This case illustrates the need for co-operative diagnostic referrals between physicians and dentists.
Keywords: Cyclophosphamide hydroxydaunorubicin oncovin prednisolone-rituximab therapy, extranodal, mandibular swelling, non-Hodgkin's lymphoma
INTRODUCTION
Lymphomas are malignant neoplasm of the lymphocyte cell lineage. They are mainly classified as either Hodgkin's or non-Hodgkin's lymphoma (NHL). NHL comprises a heterogeneous group of lymphoid neoplasm with a spectrum of behavior ranging from relatively indolent to highly aggressive and potentially fatal.[1] Only extranodal presentation of Hodgkin's disease is rare; among NHL's lymphomas, extranodal presentations are relatively common. Primary lymphomas of the oral cavity are uncommon.[2] The oral cavity, including the palate, gingiva, tongue, buccal mucosa, floor of the mouth and lips is the primary site of approximately 2% of all extranodal lymphomas.[3] The most common clinical appearance of NHL in the mouth is a non-healing, painless ulceration.[4] NHL can affect both bony and soft oral tissue, with the most frequent localization being the palate and the mandible. However, it is rare to find extranodal NHLs in the gingiva.[5]
CASE REPORT
Patient was a 50-year-old female of Indian origin who presented for evaluation of a slowly enlarging anterior mandibular mass, which she stated had been present for at least 12 months. She reported pain and swelling in association with paresthesia in the chin region for 12-14 months. Initially, her symptoms were thought by her dentist, to be a pyogenic granuloma and managed by excision and antibiotics. However, the lesion recurred after six months of excision and rapidly enlarged to the present size. Clinically, the lesion appeared as sessile, soft and friable mass, which bled on palpation [Figure 1]. The mass had displaced the teeth in the affected region and involved the mandibular labial sulcus. At the time of presentation, patient did not report any systemic symptoms and had no fever, weight loss or dysphasia. The patient's previous medical history was non-contributory. She was not on medications at the time of presentation and was a non-drinker and a non-smoker.
Figure 1.

Intra-oral clinical view of the lesion depicting mandibular labial sulcus involvement and displacement of the adjoining teeth
Excisional biopsy was performed to determine the nature of the lesion. The H and E stained soft-tissue section [Figure 2] revealed proliferation of lymphoblastic appearing cells that showed varying degrees of differentiation. Cells had round or oval nucleus with multi-lobed or cleaved nuclei. The section consisted of the population of monotonous proliferation of the lymphoblastic series with minimal cytoplasm. Lymphoblasts were scattered in diffuse pattern in the subepithelial connective tissue. At one area, the section was encapsulated and showed arteritis obliterans, extravasated red blood cells, collagen bundles, fibroblasts, adipocytes, chronic inflammatory cells mainly lymphocytes, calcifications, muscles fibers, eosinophilic material and bone. The epithelium was parakeratinized stratified squamous type, which was thin and atrophic at places.
Figure 2.
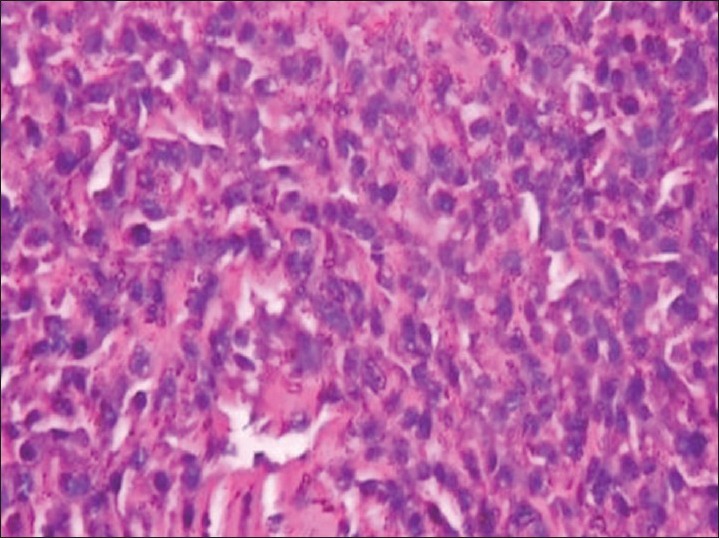
Histologic view of the lesion. Cells have round or oval nucleus with multilobed or cleaved nuclei. Large lymphocytes are more in number than small lymphocytes (H&E stain, ×400)
A diagnosis of primary extranodal non-Hodgkin's diffuse large B-cell type lymphoma of the gingiva with small cleaved nuclei type cells was made as CD20 marker was positive on immunohistochemistry [Figure 3] and patient was then referred to the oncologist for definitive management. The oncologist confirmed that the lymphoma was localized to the anterior mandible only, without any diffuse disease or nodal involvement. She was categorized as stage IAE primary mandibular NHL. It was the recommendation of the oncologist that she should undergo four cycles of Cyclophosphamide hydroxydaunorubicin oncovin prednisolone-rituximab followed by radiotherapy. She attained a complete response and following therapy there appeared to be new healthy bone formation.
Figure 3.
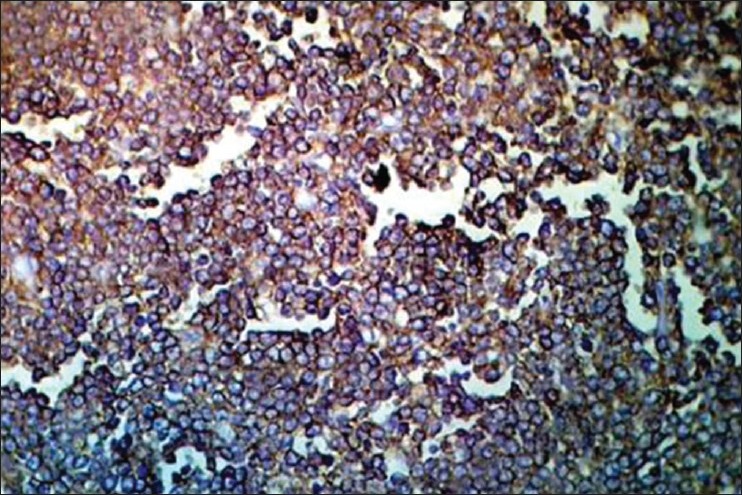
Immunohistochemistry showing pleomorphic cells diffusely positive for CD20 marker (×200)
DISCUSSION
NHL presents up to 40% of the time at an extranodal site. Moreover, 2-3% of these extranodal cases may arise primarily in the oral cavity and jaws. It is generally accepted that the most common site of NHL in orofacial region is Waldeyer's ring.[6] Jaw involvement by NHL is rare, but among jaw lesions, maxilla is more frequently involved than mandible.[7] Primary lymphoma of the bone was first described by Parker and Jackson as primary reticular cell sarcoma of bone.[8] There are no characteristic clinical features when jaw bones are involved, they can present as swelling of the jaw, pain, numbness, tooth mobility or cervical lymphadenopathy.[9] NHL can be managed by chemotherapy, radiotherapy and surgery in various combinations. NHL arising in bone is best treated by radiotherapy and may not require chemotherapy. Survival is excellent in localized disease, whereas disseminated disease seems less favorable.[10] Though lymphoma of mandible is rare, it must be considered in the differential diagnosis of swellings arising in that region. Lymphomas arising in bone may be effectively managed by chemotherapy alone. Radiation alone may be curative in early lesions. Adjuvant radiotherapy is useful especially in histopathologic variants suggesting aggressive behavior. The radiation field should incorporate the ipsilateral mandible and regional lymph nodes. The role of surgery is for biopsy purposes and for the control of persistent or recurrent local disease. Thus, with the rising incidence of extranodal lymphomas, it has become very important for today's dentists to not take any swellings of the orofacial region at face value, but to properly investigate its pathology and treat it judiciously.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Salhany KE, Pietra GG. Extranodal lymphoid disorders. Am J Clin Pathol. 1993;99:472–85. doi: 10.1093/ajcp/99.4.472. [DOI] [PubMed] [Google Scholar]
- 2.Burke JS. Waldeyer's ring, sinonasal region, salivary gland, thyroid gland, Central nervous system, and other extranodal lymphomas and lymphoid hyperplasias. In: Knowles DM, editor. Neoplastic Hematopathology. 2nd ed. Philadelphia: Lippincott Williams and Willkins; 2001. pp. 1351–90. [Google Scholar]
- 3.Ferry JA, Harris NL. Lymphomas and lymphoid hyperplasia in head and neck sites. In: Pilch BZ, editor. Head and Neck Surgical Pathology. 1st ed. Philadelphia: Lippincott Williams and Wilkins; 2001. pp. 476–533. [Google Scholar]
- 4.Richards A, Costelloe MA, Eveson JW, Scully C, Irvine GH, Rooney N. Oral mucosal non-Hodgkin's lymphoma: A dangerous mimic. Oral Oncol. 2000;36:556–8. doi: 10.1016/s1368-8375(00)00047-6. [DOI] [PubMed] [Google Scholar]
- 5.Castellano S, Carbone M, Carrozzo M, Broccoletti R, Pagano M, Vasino MA, et al. Onset of oral extranodal large B-cell non-Hodgkin's lymphoma in a patient with polycythemia vera: A rare presentation. Oral Oncol. 2002;38:624–6. doi: 10.1016/s1368-8375(01)00099-9. [DOI] [PubMed] [Google Scholar]
- 6.Sankaranarayanan S, Chandrasekhar T, Rao PS, Rooban T, Ranganathan K. Maxillary non-Hodgkin's lymphoma. J Oral Maxillofac Pathol. 2005;9:34–6. [Google Scholar]
- 7.Sarda AK, Kannan R, Gupta A, Mahajan V, Jain PK, Prasad S, et al. Isolated involvement of the mandible by non-Hodgkin's lymphoma. J Postgrad Med. 1995;41:90–2. [PubMed] [Google Scholar]
- 8.Parker F, Jackson H. Primary reticulum cell sarcoma of the bone. Surg Gynecol Obstet. 1939;68:45–53. [Google Scholar]
- 9.Rosado MF, Morgensztern D, Peleg M, Lossos IS. Primary diffuse large cell lymphoma of the mandible. Leuk Lymphoma. 2004;45:1049–53. doi: 10.1080/10428190310001625737. [DOI] [PubMed] [Google Scholar]
- 10.Someya M, Sakata K, Nagakura H, Itou K, Nakata K, Oouchi A, et al. Three cases of diffuse large B-cell lymphoma of the mandible treated with radiotherapy and chemotherapy. Radiat Med. 2005;23:296–302. [PubMed] [Google Scholar]


