Abstract
Pulse methylprednisolone therapy is the recommended therapy for moderate to severe and active ophthalmopathy, but high dose pulse methylprednisolone therapy is marred by the chances of fulminant hepatic failure and the high cost of therapy. Dexamethasone pulse therapy can be considered as an alternative to pulse methylprednisolone therapy. A prospective randomized control trial was carried out in 21 patients comparing pulse dexamethasone therapy versus pulse methyprednisolone therapy in Graves's ophthalmopathy. This study proved that pulse dexamethasone therapy is a cheaper and equally effective therapy for Graves's ophthalmopathy and the cost of therapy is reduced to at least 1/8th s. Furthermore, dexa had a better effect on reduction of exophthalmos. The dreaded complication of fulminant hepatic failure, associated with high dose of methylprednisolone, is not seen with dexa therapy.
Keywords: Graves’ ophthalmopathy, pulse dexamethasone therapy, pulse methylprednisolone therapy
INTRODUCTION
Graves’ ophthalmopathy is a potentially site threatening ocular disease, which is seen in patients with auto immune thyroid disease.[1] Pulse methylprednisolone therapy is the recommended therapy for moderate to severe and active ophthalmopathy.[2,3] High dose pulse methylprednisolone therapy is marred by the chances of fulminant hepatic failure and the high cost of therapy.[4] Dexamethasone pulse therapy can prove as a safe and cheaper alternative for pulse methylprednisolone therapy in the treatment of Graves ophthalmopathy.
Objectives
To study the efficacy of pulse dexamethasone therapy in Graves ophthalmopathy
To compare the efficacy and side-effect profile of pulse dexamethasone therapy as compared with pulse methyprednisolone therapy in Graves ophthalmopathy.
MATERIALS AND METHODS
A prospective randomized control trial was performed comparing pulse dexamethasone therapy versus pulse methyprednisolone therapy in Graves's ophthalmopathy. A total of 21 patients, all of whom were having active moderate to severe Graves's ophthalmopathy were recruited for the study. Seventeen patients were biochemically hyperthyroid at the start of the study and four patients were euthyroid (with or without treatment). After getting informed consent, patients were divided into two comparable groups with regard to age, smoking status, activity and severity of Graves's ophthalmopathy and thyroid status [Table 1]. Out of the 21 patients, 10 patients received pulse methyprednisolone therapy, (500 mg intravenous [i.v.] weekly for 6 weeks and 250 mg i.v. weekly for next 6 weeks) and 11 received pulse dexamethasone therapy 100 mg i.v. for 6 weeks followed by 50 mg i.v. for 6 weeks. All patients received pantoprazole injection before the pulse steroid therapy. Patients were followed-up for 12 weeks and the following parameters – clinical activity score, measures of severity - diplopia, lid retraction and exophthalmos and other parameters such as weight, blood pressure, blood glucose, aspartate amino transferase and alanine amino transferase (ALT) were assessed at baseline and 3 months after therapy. A Student t-test and Chi-square test were used to analyze the results using the Statistical Package for the Social Sciences statistical software version 13 (IBM USA).
Table 1.
Baseline characteristics

RESULTS
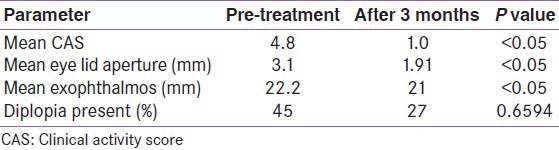
After 3 months of therapy with pulse dexamethasone, there was a statistically significant change in clinical activity score (CAS), with mean CAS falling from 4.8 to 1.0 (P < 0.05). The severity parameters assessed, lid aperture and exophthalmos, also showed a statistically significant difference, with P < 0.05. However, there was no significant improvement in diplopia [Table 2].
Table 2.
Change in parameters-dexa group
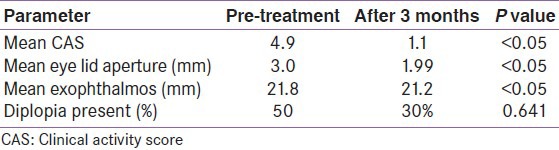
Treatment with methylprednisolone also showed a similar trend, with statistically significant change in CAS, with mean CAS improving from 4.9 to 1.1 (P < 0.05). Lid aperture and exophthalmos, also showed a statistically significant difference, with P values < 0.05 but, diplopia had no significant improvement with P value of 0.641 [Table 3].
Table 3.
Change in parameters-Methylprednisolone group
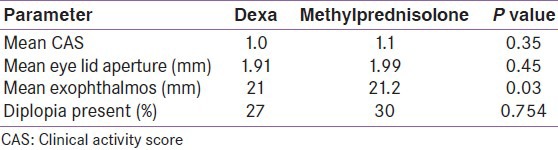
When the efficacy of treatment between groups was compared, there was no significant difference between dexamethasone and methyprednisolone groups with regard to improvement in CAS, change in lid aperture or change in diplopia. But the improvement in exophthalmos was better in the dexa group, with a P value of 0.03 [Table 4].
Table 4.
Change in parameters comparison between groups
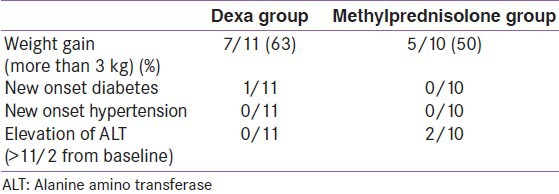
As far as the side-effect profile was concerned, dexa group had more of weight gain and one patient developed diabetes. But, there were two cases of elevation of ALT in the methylprednisolone group while the dexa group had none [Table 5].
Table 5.
Side-effects
DISCUSSION AND CONCLUSIONS
Pulse methylprednisolone therapy is an effective therapy for Graves ophthalmopathy, but has the limiting factors of fulminant hepatic failure and high cost of therapy.[5] Our study proves that pulse dexamethasone therapy is a cheaper and equally effective therapy for Graves ophthalmopathy and the cost of therapy is reduced to at least 1/8th s. Also, dexa has a better effect on reduction of exophthalmos. The dreaded complication of fulminant hepatic failure, associated with high dose of methylprednisolone, is not seen with dexa therapy. Regular monitoring of liver function tests is not required with dexamethasone therapy, reducing the cost of therapy. There is a slightly increased incidence of diabetes and weight gain with dexamethasone therapy, but patient who developed diabetes, reverted to normal blood glucose after 3 months.
Pulse dexamethasone therapy can be considered as a cheaper and safer alternative of pulse methylprednisolone therapy in the treatment of Graves's ophthalmopathy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Bartley GB. The epidemiologic characteristics and clinical course of ophthalmopathy associated with autoimmune thyroid disease in Olmsted County, Minnesota. Trans Am Ophthalmol Soc. 1994;92:477–588. [PMC free article] [PubMed] [Google Scholar]
- 2.Kahaly GJ, Pitz S, Hommel G, Dittmar M. Randomized, single blind trial of intravenous versus oral steroid monotherapy in Graves’ orbitopathy. J Clin Endocrinol Metab. 2005;90:5234–40. doi: 10.1210/jc.2005-0148. [DOI] [PubMed] [Google Scholar]
- 3.van Geest RJ, Sasim IV, Koppeschaar HP, Kalmann R, Stravers SN, Bijlsma WR, et al. Methylprednisolone pulse therapy for patients with moderately severe Graves’ orbitopathy: A prospective, randomized, placebo-controlled study. Eur J Endocrinol. 2008;158:229–37. doi: 10.1530/EJE-07-0558. [DOI] [PubMed] [Google Scholar]
- 4.Weissel M, Hauff W. Fatal liver failure after high-dose glucocorticoid pulse therapy in a patient with severe thyroid eye disease. Thyroid. 2000;10:521. doi: 10.1089/thy.2000.10.521. [DOI] [PubMed] [Google Scholar]
- 5.Marinó M, Morabito E, Brunetto MR, Bartalena L, Pinchera A, Marocci C. Acute and severe liver damage associated with intravenous glucocorticoid pulse therapy in patients with Graves’ ophthalmopathy. Thyroid. 2004;14:403–6. doi: 10.1089/105072504774193276. [DOI] [PubMed] [Google Scholar]


