Abstract
Menorrhagia is the most common menstrual irregularity in hypothyroid women. However, it is an uncommon presentation of congenital hypothyroidism (CH). In the era of newborn screening across the world, when CH is extremely rare, we came across four cases of CH due to delayed diagnosis, presenting in adulthood with severe menorrhagia.
Aims:
To signify the atypical presentation of CH in late adulthood due to delayed diagnosis and its sequelae; and to increase the awareness about this treatable condition.
Settings and Design:
This is a cross-sectional analysis of consecutive patients with CH presenting after 18 years between 2010 and 2012 from the CH registry of Department of Endocrinology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), India.
Subjects and Methods:
Four patients of CH presenting late (>18 years) with atypical presentations out of total 16 cases of CH within a period of 3 years were analyzed for clinical, hormonal, and imaging findings.
Results:
Between the years 2010 and 2012, 16 cases of CH were registered at our center out of which four cases presented in late adolescence and adulthood with menorrhagia. Age range of these patients was 18-30 years. All four patients were females presenting with anemia secondary to menorrhagia and upon evaluation were found to have CH. All of them showed improvement after starting treatment and are currently doing well with regular menstrual cycles.
Conclusions:
Our study demonstrates the importance of thyroid evaluation in a patient presenting with menorrhagia along with short stature. There is need for awareness among clinicians regarding the clinical features of CH and nationwide screening for CH in our country.
Keywords: Congenital hypothyroidism, menorrhagia, neonatal screening, short stature, thyroid dysgenesis
INTRODUCTION
Congenital hypothyroidism (CH) is a disease of protean manifestations. It represents a heterogeneous group of thyroidal disorders leading to decreased or absent thyroid hormone action and clinical sequelae. The primary thyroid stimulating hormone (TSH) screening has become standard in many parts of the world. The incidence of CH as detected by common neonatal screening programs across the world is approximately 1:3,000-1:4,000 in live births.[1] However, newborn thyroid screening is not yet universal in some less developed countries. Studies from Mumbai have suggested that CH is common in India, the disease occurring in 1 out of 2,640 neonates.
Although CH is an easily identifiable and treatable condition, our cases of CH were unique because they remained undiagnosed for more than 18-30 years, until an atypical alarm sign of menorrhagia emerged. Menorrhagia is an uncommon presentation of CH, even though it is the most common menstrual irregularity in hypothyroid women.
SUBJECTS AND METHODS
This is a cross-sectional analysis of CH cases selected from those registered between the years 2010 and 2012 in Endocrinology Department at Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India. Sixteen cases were registered as CH, out of which four cases presented at more than 18 years of age. These cases were analyzed separately.
All the patients in our case series were women aged above 18 years with chief complaint of menorrhagia. At presentation, they all had typical clinical features suggestive of hypothyroidism and they were confirmed to have the same by thyroid function test. In view of aplastic/hypoplastic thyroid gland in the background of nil uptake on technetium 99 m thyroid scintiscan on drug naive CH patients, a diagnosis of CH was made. We hereby describe the clinical presentation, imaging findings, and hormonal profiles of these patients.
RESULTS
Between the years 2010 and 2012, 16 cases of CH were registered at our center. Out of sixteen cases, four were CH presenting late (> 18 years). Their mean age at presentation was 24 years and age range was 18-30 years. All were female patients presenting with anemia secondary to menorrhagia.
None of them had any family history of thyroid disorders or mental retardation. Two of them were born out of second degree consanguineous marriage with normal antenatal and natal history. Developmental milestones were delayed in all four of them. All had poor scholastic performance due to which they ended up as school dropouts currently managing simple household work. In early childhood, stunted growth was noticed by family in two of the patients and was brought to medical attention, but unfortunately it went undiagnosed. Menarche was delayed in three patients. Clinical profiles of all four patients are outlined in [Table 1].
Table 1.
Clinical profile of the case series
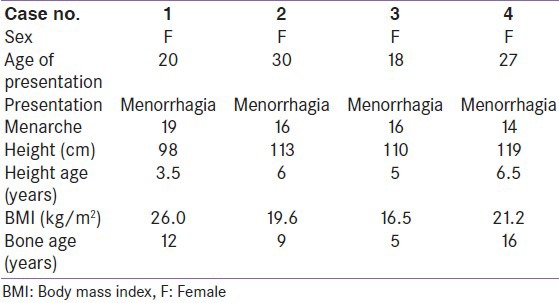
On examination, growth parameters were plotted on standard weight and height charts and all four of them had stunted growth with height and weight < third percentile with short limbs. All had typical features of hypothyroidism of variable degree with facial and periorbital puffiness, coarse thick dry skin, and pseudomyotonic reflexes. None of them had macroglossia or umbilical hernia. No thyroid tissue was palpable in the neck nor visible in the buccal cavity in all four patients. All had poor secondary sexual characteristics with Tanner stage 2-3 breast development and Tanner stage 3-4 in pubic hair development. Short stature and delayed bone age was consistent in all cases of CH, similar to other studies described in literature.
Investigations revealed World Health Organization (WHO) grade 3 (serious anemia) in two patients and grade 4 (life-threatening anemia) in two patients. Peripheral smear picture showed microcytic hypochromic red blood cells (RBCs) with low serum ferritin in all of them. Thyroid profile was suggestive of severe hypothyroidism (TSH > 150 μIU/ml). In view of hypoplastic thyroid gland in ultrasound thyroid, all patients underwent technetium pertechnate thyroid scintiscan which showed CH due to thyroid dysgenesis (case 1, 3, and 4: Agenesis and case 2: Ectopic lingual thyroid). Hormonal and imaging profiles are summarized in Table 2 and Figures 1 and 2.
Table 2.
Investigation profile of cases
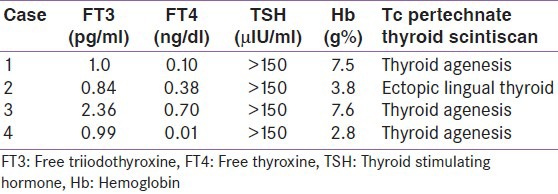
Figure 1.
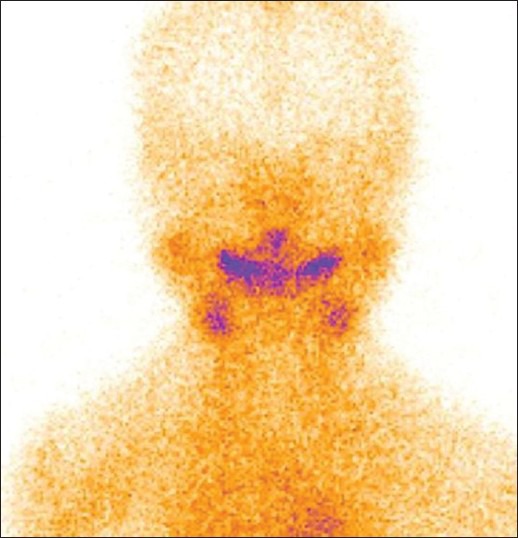
Tc 99m thyroid scan images of thyroid agenesis (case 1)
Figure 2.
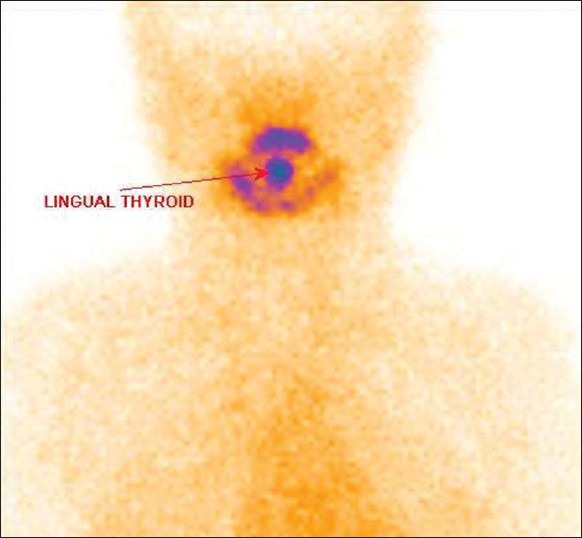
Tc 99m thyroid scan images of ectopic lingual thyroid (case 2)
All four patients were initiated on low dose thyroxine and were gradually titrated. All of them showed improvement after starting treatment and are currently doing well with regular menstrual cycles.
DISCUSSION
The differential diagnosis of menorrhagia includes a wide spectrum of benign and malignant, inflammatory and infectious conditions. But the concurrence of short stature and typical clinical features along with menorrhagia helped us to bring out the glaring diagnosis, finally after several years of clinical lethargy. CH affects approximately 1 in 2,000 to 1 in 4,000 newborns. Thyroid dysgenesis encompasses a group of congenital thyroid abnormalities including absence of thyroid tissue (agenesis or athyreosis), hemiagenesis, ectopic thyroid tissue, and hypoplasia of an orthotopic gland. Collectively, these abnormalities account for approximately 85% of cases of CH in iodine sufficient regions. The tongue is the most common site for total thyroid ectopia.[1]
Clinical picture of CH varies according to age of presentation. During first few months of life child may present with failure to thrive, constipation, jaundice, or hoarse cry. In succeeding months, patient may present with protuberant abdomen, delayed teeth eruption, dry skin, and developmental delay. In later ages, the patient may present with short stature, decreased intelligent quotient (IQ), gross/fine motor incoordination, hypotonia, speech disorders, attention deficit, and sensory neural deafness. In women of fertile age, hypothyroidism results in changes in cycle length and amount of bleeding. Hypothyroidism is frequently accompanied by microcytic anemia secondary to iron deficiency from the menorrhagia.[2] Frequency of menstrual disturbances in hypothyroidism is approximately three times greater than in the normal population. Kakuno et al., reported that patients with severe hypothyroidism who had a higher prevalence of menstrual disturbances than mild to moderate cases. However, menorrhagia is an uncommon presentation of CH in adulthood.[3] In myxedema, menorrhagia is observed and in older patients with untreated CH metrorrhagia is sometimes seen. Apart from a few isolated case reports, late presentations of CH is an underreported entity in endocrinology. There is very little published literature to estimate the disease burden due to delayed diagnosis of CH in less developed countries like ours.
An association between hypothyroidism, menorrhagia and blood coagulation abnormalities has been recognized as early as 1975. The pathogenesis of the bleeding tendency associated with thyroid hormone deficiency is usually multifactorial. Menorrhagia is probably primarily due to estrogen breakthrough bleeding secondary to anovulation that accompanies thyroid hormone deficiency. TSH has both follicle stimulating hormone (FSH) and luteinizing hormone (LH) like effects through their shared α subunit. As a result, negative feedback is downregulated, leading to decreased secretion of LH and an ensuing decrease in progesterone. Additionally, due to decreased sex hormone binding globulin, circulating free estrogen levels rise, and its prolonged unopposed effect on endometrium results in anovulation and corpus luteum formation, ultimately leading to menometrorrhagia.[4]
Also myxedematous changes in the extracellular matrix surrounding the superficial blood vessels may play a role. There is also evidence that alterations in platelet and arterial wall prostaglandin production and metabolism may possibly contribute to the platelet dysfunction.[5,6,7] Hypothyroidism has been associated with acquired von Willebrand Syndrome (AVWS) type 1 with a frequency of ~2-5%. In the 47 cases reported in the literature, the low von Willebrand factor (VWF) levels is apparently due to a reduction in its synthesis and/or secretion leading onto decreased platelet plug formation and impaired primary hemostasis.[8,9] These coagulation disorders of severe hypothyroid patients were corrected upon levothyroxine therapy.[8]
Thyroid disorders are different from other diseases in terms of ease of diagnostic investigations and economical, easy accessibility of treatment. However, most of the times, because of the wide variability and vagueness of symptoms, hypothyroidism is usually unsympathetically dismissed by the family and treating doctors. Our case series clearly proves that even patients with severe hypothyroidism with a classical clinical picture may elude diagnosis for many years until they develop some life-threatening symptoms like menorrhagia or multisystem failure which forces them to come for medical help.
Screening programs have been established in most developed countries to detect and treat this disorder. Worldwide, it is estimated that 25% of the live born population of 130 million babies undergo newborn screening for SC (NSCH).[10] Population-based biochemical screening of newborn infants for CH became possible in the 1970s after the development of methods for assaying thyroxine (T4) and thyrotropin (TSH) in blood collected on filter paper.[3] Routine neonatal screening is not available in India even in tertiary care centers, so the main stay for diagnosis is clinical awareness of this condition. In the absence of a universal screening program, diagnosis of CH, an important cause of preventable mental retardation is often delayed in India.[11] The reasons for the delayed diagnosis are the uneducated parents/caretakers, who overlook the deviation of physical and mental growth and attribute it to something constitutional or some unacceptable cause. Even if they notice, they are unaware regarding the importance of early diagnosis and commencement of therapy. It is the awareness which needs to be enhanced among general practitioners and parents regarding the importance of early diagnosis and commencement of therapy to prevent the effects of delayed diagnosis.
All these are easily said, than done. In countries like ours the problems for nonimplementation of screening is not due to lack of scientific or technical knowhow, but are related to economic and population burden.[10] Prescribing a simple tablet of thyroxine, when indicated by neonatal screening, have the potential to prevent future national morbidity from mental and physical handicaps. Simple thyroid function tests can easily pick up the disease in later life, if missed in neonatal life. In conclusion, this calls for increased awareness of the condition in both general public and primary care physicians of our country.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Nikiforov YE, Biddinger PW, Thompson LD. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; Diagnostic pathology and molecular genetics of the thyroid; p. 16. [Google Scholar]
- 2.Becker KL. 3e. Philadelphia: Lippincott Williams and Wilkins; 2001. Principles and practice of endocrinology and metabolism; p. 1932. [Google Scholar]
- 3.Braverman LE, Cooper DS. 10th ed. Philadelphia: Lippincott Williams and Wilkins; Werner and Ingbar's the thyroid: A fundamental and clinical text; p. 586. [Google Scholar]
- 4.Moragianni VA, Somkuti SG. Profound hypothyroidism-induced acute menorrhagia resulting in life-threatening anemia. Obstet Gynecol. 2007;110:515–7. doi: 10.1097/01.AOG.0000275285.04825.07. [DOI] [PubMed] [Google Scholar]
- 5.Ford HC, Carter JM. Haemostasis in hypothyroidism. Postgrad Med J. 1990;66:280–4. doi: 10.1136/pgmj.66.774.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Edson JR, Fecher DR, Doe RP. Low platelet adhesiveness and other hemostatic abnormalities in hypothyroidism. Ann Intern Med. 1975;82:342–6. doi: 10.7326/0003-4819-82-3-342. [DOI] [PubMed] [Google Scholar]
- 7.Franchini M, Montagnana M, Manzato F, Vescovi PP. Thyroid dysfunction and hemostasis: An issue still unresolved. Semin Thromb Hemost. 2009;35:288–94. doi: 10.1055/s-0029-1222607. [DOI] [PubMed] [Google Scholar]
- 8.Chadarevian R, Jublanc C, Bruckert E, Giral P, Ankri A, Leenhardt L, et al. Effect of levothyroxine replacement therapy on coagulation and fibrinolysis in severe hypothyroidism. J Endocrinol Invest. 2005;28:398–404. doi: 10.1007/BF03347217. [DOI] [PubMed] [Google Scholar]
- 9.Desai MP. Congenital hypothyroidism: Screening dilemma. Indian J Endocrinol Metab. 2012;16:S153–5. doi: 10.4103/2230-8210.104027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seth A, Aggarwal V, Maheshwari A. Hypothyroidism in children beyond 5 y of age: Delayed diagnosis of congenitalhypothyroidism. Indian J Pediatr. 2012;79:891–5. doi: 10.1007/s12098-011-0678-4. [DOI] [PubMed] [Google Scholar]
- 11.Desai MP. Disorders of the thyroid gland in India. Indian J Pediatr. 1997;64:11–20. doi: 10.1007/BF02795771. [DOI] [PubMed] [Google Scholar]


