Abstract
Aminoglycoside (AMG)-induced renal toxicity is well-known and may manifest with non-oliguric renal failure or renal tubular dysfunction like Fanconi-like syndrome, Barter syndrome-like syndrome or distal renal tubular acidosis (RTA). These phenomena have been described with Gentamycin and Amikacin though rarely with Kanamycin. We present two cases of pulmonary tuberculosis that were treated with Kanamycin and during the course of treatment, developed severe recalcitrant hypocalcemia along with hypomagnesemia.
Keywords: Hypocalcemia, hypomagnesemia, kanamycin, multidrug-resistant tuberculosis
INTRODUCTION
Electrolyte disturbance is one of the most challenging adverse reactions related to multidrug- resistant tuberculosis (MDR-TB) management, in particular because of the paucity of presenting symptoms and potential morbidity associated with this disorder. Reasons for electrolyte disturbance among patients treated for MDR-TB are likely multifactorial. Both potassium and magnesium deficiencies are associated with a number of chronic diseases, such as tuberculosis, malnutrition, alcoholism, and diabetes mellitus.[1,2] In addition, diarrhea and vomiting caused by anti-tuberculous agents can contribute to GI electrolyte loss. There is also evidence that the use of aminoglycosides (AMG) and capreomycin causes renal wasting of electrolytes, including potassium, magnesium, and calcium.[3,4,5] Both aminoglycosides and capreomycin are thought to induce secondary hyperaldosteronism leading to urinary loss of potassium and magnesium. We present two cases of MDR-TB on second line anti-tubercular treatment (ATT) presenting with hypomagnesemia and hypocalcemia.
CASE REPORTS
Case 1
A 34-year-old male, diagnosed case of MDR-TB on second line ATT including kanamycin for six months, came to hospital with tingling sensation of both lower limbs and cramps of hand. He had no history of vomiting, diarrhea or oliguria. On examination, he was emaciated, pale, and had bilateral extensive lung parenchymal disease [Figure 1]. His investigation [Table 1] revealed hypocalcemia, hypomagnesemia, and hypermagnesuria. After detail study, kanamycin was stopped and magnesium and calcium supplementation was started. Within two weeks of treatment, patient showed improvement both biochemically and clinically.
Figure 1.
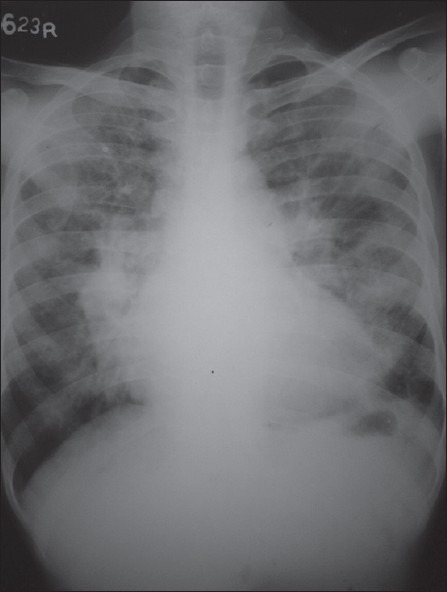
Chest X-Ray of case 1: Bilateral parenchymal shadows
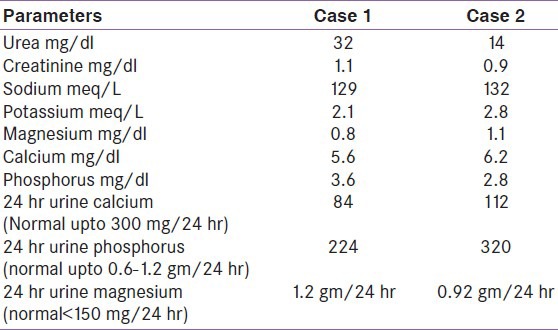
Table 1.
Biochemical pattern of patients
Case 2
A 46-year-old male, a case of MDR-TB who has stopped treatment twice and now on second line ATT including kanamycin for past one year, came to hospital with generalized tonic-clonic convulsion and altered sensorium. He had no history of headache, vomiting or fever at time of admission. On examination, patient was drowsy; however, rest of neurological examination was normal. He also had bilateral pleural effusion with bilateral lower lobe consolidation [Figure 2]. His investigation [Table 1] revealed hypocalcemia, hypomagnesemia, and hypermagnesuria. His treatment was modified, kanamycin was stopped, and magnesium and calcium supplementation was started. Within four weeks of treatment, patient showed improvement both biochemically and clinically.
Figure 2.
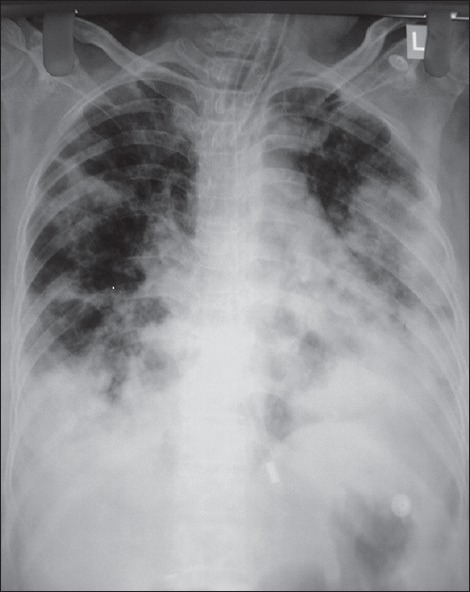
Chest X-Ray of case 2: Bilateral consolidation with effusion
DISCUSSION
Hypokalemia and hypomagnesemia are important adverse reactions of MDR-TB therapy, particularly among patients receiving aminoglycosides and capreomycin. We describe here two cases of electrolyte disorders in MDR-TB patients on Kanamycin therapy. Both the patients received Kanamycin for at least six months and had no other cause for present electrolyte dysfunction. There is evidence that the use of aminoglycosides and capreomycin causes renal wasting of electrolytes, including potassium, magnesium, and calcium. Both aminoglycosides and capreomycin are thought to induce secondary hyperaldosteronism leading to urinary loss of potassium and magnesium. Because magnesium serves as a co-factor in the adenosine triphosphatase-dependent mechanism for active transport of sodium and potassium across the cell membrane, further potassium wasting occurs as a consequence of resultant intracellular magnesium deficiency. Lastly, hypomagnesemia can induce hypocalcemia, in part through the suppressive effect of low magnesium levels on the parathyroid hormone. In our patient, Kanamycin was the culprit drug; it has been rarely reported as cause of electrolyte imbalance in MDR-TB patients. Electrolyte disturbances may be manifested as minor complaints such as fatigue, cramps, nausea, and irritability, or by serious complications, including tetany, seizures, and lethal cardiac arrhythmias. Given the non-specific early symptoms and significant morbidity associated with electrolyte wasting, regular monitoring and replacement is critical.[6] Correction of hypomagnesemia contributes to the normalization of calcium and potassium deficiencies.[7] Hypokalemia may be refractory to treatment if hypomagnesemia is present and not addressed. Spironolactone (100 to 300 mg/d) may also aid in the normalization of serum potassium and magnesium. Normalization of electrolyte values may take up to four months after cessation of the offending agent.[6] To conclude, aminoglycosides are commonly used antibiotics with excellent renal parenchymal penetration. Their clinical effectiveness is counterbalanced with the risk of renal toxicity, which develops in dose-dependent fashion. The toxic potential of individual AMG is directly related to their ability to bind and disrupt plasma membrane.
Electrolyte disturbance is one of the most challenging adverse reaction related to MDR-TB management, in particular because of paucity of presenting symptoms and potential morbidity associated with the disorder. This paper emphasizes upon severity of AMG-induced electrolyte imbalance and to consider it as a potential cause of hypomagnesemia and hypocalcemia in critically ill patients on multiple drug therapy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Aquinas M, Citron K. Rifampicin, ethambutol and capreomycin in pulmonary tuberculosis, previously treated with both first and second line drugs: The results of two years chemotherapy. Tubercle. 1972;53:153–65. doi: 10.1016/0041-3879(72)90012-8. [DOI] [PubMed] [Google Scholar]
- 2.Shah GH, Kirschenbaum MA. Renal magnesium wasting associated with therapeutic agents. Miner Electrolyte Metab. 1991;17:58–64. [PubMed] [Google Scholar]
- 3.Elliott C, Newman N, Madan A. Gentamicin effects on urinary electrolyte excretion in healthy subjects. Clin Pharmacol Ther. 2000;67:16–21. doi: 10.1067/mcp.2000.103864. [DOI] [PubMed] [Google Scholar]
- 4.Bar RS, Wilson HE, Mazzaferri EL. Hypomagnesemic hypocalcemia secondary to renal magnesium wasting. Ann Intern Med. 1975;82:646–9. doi: 10.7326/0003-4819-82-5-646. [DOI] [PubMed] [Google Scholar]
- 5.Vanasin B, Colmer M, Davis P. Hypocalcemia, hypomagnesemia and hypokalemia during chemotherapy of pulmonary tuberculosis. Chest. 1972;61:496–9. doi: 10.1378/chest.61.5.496. [DOI] [PubMed] [Google Scholar]
- 6.Holmes A, Hesling C, Wilson T. Capreomycin-induced electrolyte abnormalities. Thorax. 1970;25:608–11. doi: 10.1136/thx.25.5.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elisaf M, Liberopoulos E, Bairaktari E, Siaomopoulus K. Hypokalaemia in alcoholic patients. Drug Alcohol Rev. 2002;21:73–6. doi: 10.1080/09595230220119282a. [DOI] [PubMed] [Google Scholar]


