Abstract
Co-occurrence of adrenal incidentaloma with hypertension calls for evaluation of endocrine causes including pheochromocytoma, Cushing's disease, and primary aldosteronism. We are reporting 40-years-old man who presented with hypertension and adrenal mass. He had elevated metanephrines, histology of resected adrenal mass revealed adrenal myelolipoma, and immuno-histochemistry was positive for chromogranin A. Both his blood pressure and urinary metanephrines returned to normal after surgery. The association of hypertension and adrenal myelolipoma may not be entirely coincidental, as it may be associated with secreting catecholamine. Literature on such an uncommon association is reviewed briefly as well.
Keywords: Adrenal myelolipoma, chromogranin A, hypertension, metanephrines, pheochromocytoma
INTRODUCTION
Gierke, in 1905, described a lesion of adrenal gland containing fat and myeloid elements.[1] Myelolipomas are uncommon, small, asymptomatic benign lesions of adrenal cortex.[2] Incidence at autopsy has been reported from 0.08 to 0.4%.[3] Most of the lesions are discovered incidentally and are non-functional.
CASE REPORT
A 40-year-old man referred to department of endocrinology with adrenal mass and hypertension. He was diagnosed with hypertension 3 years back, initial BP was 180/110 mm Hg, was started on anti-hypertensive treatment. On examination, there were no neurocutaneous markers or marfanoid habitus, no features of Cushing's syndrome, 24-hour urine metanephrines level was 3000 micrograms/day (normal < 900 micrograms/day, the test was done after stopping all interfering drugs). Ultrasonography revealed 9.8 × 8.5 cms well-defined predominantly hyperechoic lesion, faint hypoechogenicity originating from right suprarenal region abutting the upper pole of right kidney and lower surface of right lobe of liver suggestive of right adrenal mass. CECT of abdomen showed 9.8 × 8.5 cm well-defined, well-circumscribed heterogenous hypoattenuated mass lesion noted in right suprarenal region and minimal enhancement on contrast with −80 to −100 HF units of attenuation suggestive of myelolipoma of right adrenal gland [Figure 1]. Baseline hematological and biochemical investigations and urinalysis were normal. Low-dose dexamethasone suppression test was normal.
Figure 1.
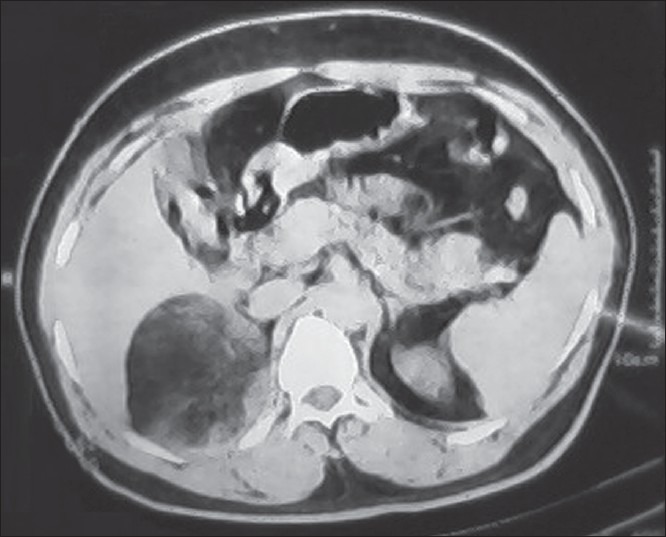
Abdominal contrasted computerized tomography showing well-defined non-homogeneous mass of right adrenal origin
In view of hypertension, adrenal mass, and elevated 24-hour urine metanephrines (>3 times), possibility of pheochromocytoma was considered. Hypertension was brought under control. Patient underwent surgery, and well encapsulated right adrenal tumor (weight: 500 gm) was excised [Figure 2]. Biopsy of specimen was suggestive of adrenal myelolipoma [Figure 3]. Immuno-histochemistry of specimen revealed positive for chromogranin A, suggestive of catecholamine-secreting granules in the tissue [Figure 4].
Figure 2.

Gross specimen of removed mass
Figure 3.
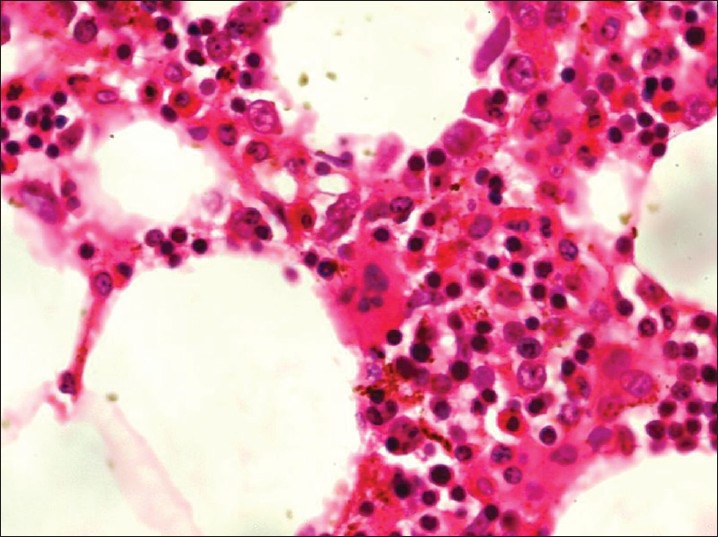
H and E staining revealing features of myelolipoma with mature fat cells, suspended with plenty of normal hematopoitic marrow elements with congested blood vessels. (Original magnification, ×100)
Figure 4.
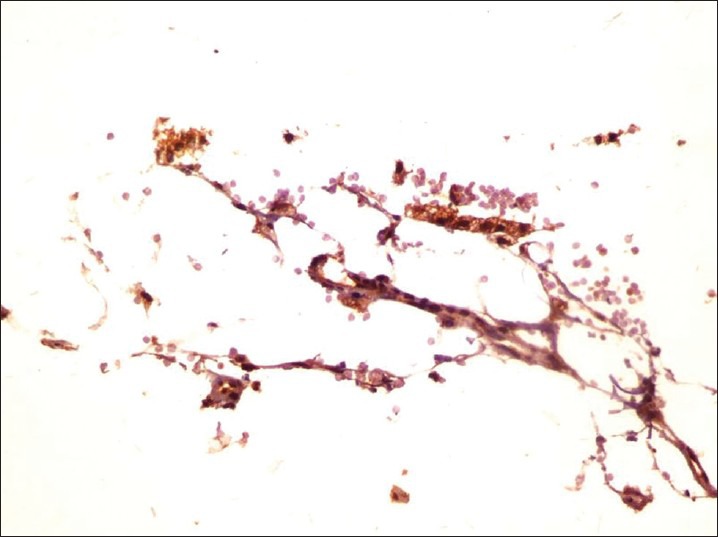
Immuno-histochemistry of specimen revealed positive for chromogranin A
The patient had remission in hypertension. Metanephrine levels became normal after surgery. The patient is normal at the 3-month follow-up.
DISCUSSION
Adrenal myelolipomas are uncommon benign tumors of adrenals, composed of adipose and hematopoietic tissue in varying proportions, a result of metaplasia of reticuloendothelial cells. These occur most commonly in fifth to seventh decade with an equal sex distribution.[4] Most of adrenomyelolipomas are asymptomatic. As these tumors are usually more than 5 cms in diameter, they can be easily detected on ultrasound. CT scan is the most sensitive test for diagnosing myelolipoma.[5] The lesion is typically seen as a well-encapsulated heterogeneous supra-renal mass of low density with negative attenuation values, interspersed by dense myeloid tissue and with or without specks of calcification.[6] The diagnosis of adrenal myelolipoma in our case was suggested by the established CT scan criteria [Figure 1] and the typical histopathological features [Figure 3]. Functionality of the adrenal mass in this patient was suggested by the presence of hypertension and elevated metanephrines. Catecholamine secreting adrenal myelolipoma was confirmed by the absence of any evidence of pheochromocytoma on HPE and documentation of positive staining for chromogranin A on IHC [Figure 4]. Brogna et al.,[7] reported a giant cortisol secreting adrenal myelolipoma,but our patient was clinically and biochemically eucortisolic. To the best of our knowledge, only two case reports are available on catecholamine-secreting adrenal myelolipoma in the world literature. Tamidari et al. have reported a case of a large, right-sided catecholamine, secreting adrenal myelolipoma with increased 24 hours urinary metanephrines.[8] Udupa et al. have reported a large adrenal myelolipoma with increased 24 hours urinary Vanillylmandelic Acid (VMA) levels.[9] All these patients became normotensive and biochemical abnormalities normalized following surgery similar to the patient in our case. The association of adrenal myelolipoma and hypertension may not be entirely coincidental, as it may be associated with catecholamine secretion, as seen in our case. Proper identification of underlying cause and appropriate treatment leads to resolution of hypertension.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Gierke E. Ueber Knochenmarksgewebe in der Nebenniere Beitr. Pathol Anat. 1905;37:311–25. [Google Scholar]
- 2.Amendolara M, Barbarino C, Bucca D, Guarnieri F, Novello GB, Romano FM, et al. Giant and bilateral adrenal myelolipoma. G Chir. 2008;29:85–8. [PubMed] [Google Scholar]
- 3.Lam KY. Lipomatous tumors of the adrenal gland. J Urol Pathol. 1995;3:95. [Google Scholar]
- 4.Doddi S, Singhal T, Leake T, Sinha P. Management of an incidentally found large adrenal myelolipoma: A case report. Cases J. 2009;2:8414. doi: 10.4076/1757-1626-2-8414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akamatsu H, Koseki M, Nakaba H, Sunada S. Giant adrenal myelolipoma; Report of a case. Surg Today. 2004;34:283–5. doi: 10.1007/s00595-003-2682-4. [DOI] [PubMed] [Google Scholar]
- 6.Haque F, Harish S, Ahmad I, Qamar A, Pandey H. Adrenal myelolipoma: A case report. Indian J Radiol Imaging. 2004;14:301–2. [Google Scholar]
- 7.Brogna A, Scalisi G, Ferrara R, Bucceri AM. Giant secreting adrenal myelolipoma in a man: A case report. J Med Case Rep. 2011;5:298. doi: 10.1186/1752-1947-5-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tamidari H, Mishra AK, Gupta S, Agarwal A. Catecholamine secreting adrenal myelolipoma. Indian J Med Sci. 2006;60:331–3. [PubMed] [Google Scholar]
- 9.Udupa S, Usha M, Visweswara RN, Desai MG. Left-sided giant adrenal myelolipoma secreting catecholamine. Indian J Pathol Microbiol. 2012;55:389–91. doi: 10.4103/0377-4929.101755. [DOI] [PubMed] [Google Scholar]


