Abstract
A 35-year-female presented with generalized weakness, weight loss, and progressive pigmentation was worked up for suspicion of Addisons disease. On examination hyper pigmentation was noted on both palmar and dorsal aspect of hands involving knuckles, creases, feet, tongue, oral mucosa and gluteal region. There was no evidence of hypocortisolemia as initially suspected, and literature search revealed a possibility of vitamin B12 deficiency. She had megaloblastic anemia with a low serum vitamin B12, mostly due to poor dietary intake. Her hyper pigmentation resolved with vitamin B12 supplementation. Skin biopsy showed increased pigmentation at stratum spinosum and basal-layer. The mechanism of hyper pigmentation in vitamin B12 deficiency was due to an increase in melanin synthesis.
Keywords: Addisons disease, B12 deficiency, hyper pigmentation, vitamin B12 deficiency
INTRODUCTION
Aetiology of acquired hyper pigmentation are many. In some patients it gives a clue to the diagnosis of systemic disorders. Pigmentation in vitamin B12 deficiency that simulates the pigmentation of Addison's disease is a rare initial presentation and early management can prevent various neurological complications. Herein, we report a rare case of hyper pigmentation due to vitamin B12 deficiency.
CASE REPORT
A 35-year-female presented with generalized weakness, weight loss and nausea along with progressive pigmentation involving both palmar and dorsal aspect of hands including knuckles, creases, feet, tongue, oral mucosa and gluteal region over a period of one year [Figure 1]. There was no history of fever, loose motion or steatorrhea, diabetes mellitus, tuberculosis, seizure disorder or any drug intake. She was unmarried, vegetarian, non-smoker, non-alcoholic and working in a hospital as a HIV counsellor.
Figure 1.

Hyperpigmentation before treatment
On systemic examination the only significant finding was pallor. Haematological and other investigation were done [Table 1]. Her Serum Cortisol level at 8 A.M and 4 P.M was 14.1 μg/dl and 7.01 μg/dl respectively (normal 5-25 μg/dl), which ruled out hypocortisolemia. At this point, a literature search revealed pigmentation in vitamin B12 deficiency can masquerade as addisonian pigmentation. Skin biopsy taken from left great toe showed “Increase pigmentation at stratum spinosum and basal layer” [Figure 2]. Upper gastrointestinal endoscopy was normal and anti parietal cell antibody was weakly positive. Her serum vitamin B12 level was 67 pg/ml (normal 180-900 pg/ml) indicative of severe vitamin B12 deficiency. After treatment improvement in subjective symptoms noticed within two weeks and skin pigmentation completely normalised within twelve weeks [Figure 3].
Table 1.
Biochemical profile of the patient before and 12 weeks after treatment
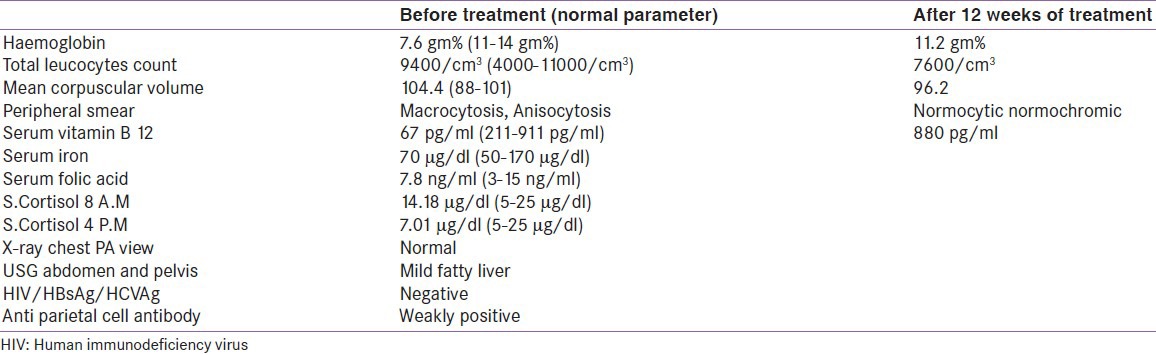
Figure 2.
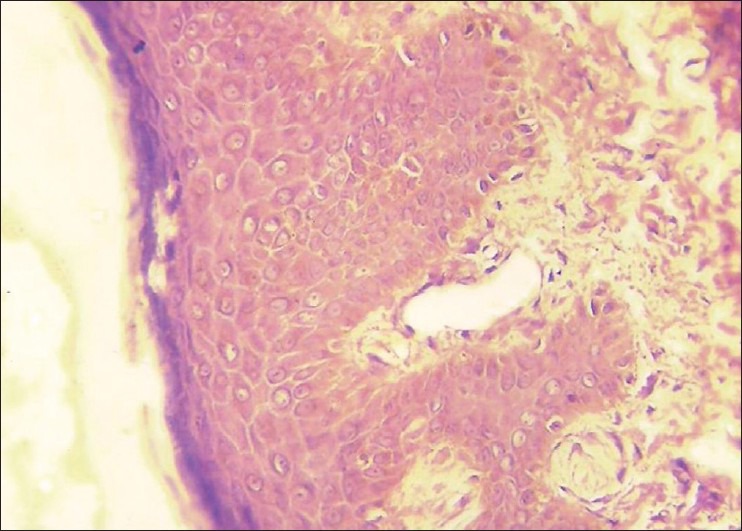
Skin Biopsy (Increased pigmentation in stratum spinosum and basal layer)
Figure 3.

Post treatment reversal of hyper pigmentation after 12 weeks of vitamin B12 supplementation
DISCUSSION
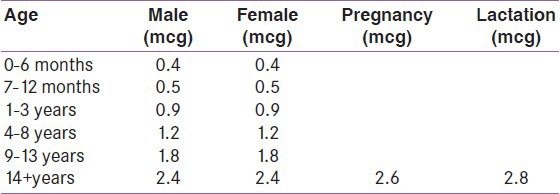
Vitamin B12 deficiency was first described by Cook in 1944 and later by Baker et al., in 1963. Currently, vitamin B12 deficiency was defined as a plasma concentration of <148 pmol/L (200 pg/ml) and marginal status defined as a concentration of 148-221 pmol/L.[1] The main source of vitamin B12 (cobalamin) in humans is the consumption of meat, poultry and dairy products. The Recommended Dietary Allowances (RDA) varies with age [Table 2].[2] Prevalence of B12 deficiency varies from 3% to 5% in the general population and 5% to 20% among people older than 65 years.[3] Inadequate intake and low consumption of animal-source foods with pernicious anemia (low intrinsic factor) in younger adults and food bound cobalamin malabsorption in part due to gastric atrophy in older persons are the main cause of low serum vitamin B12 and likely the main cause in poor populations worldwide.[1,2] In the present case the cause of vitamin B12 deficiency was decrease intake with low intrinsic factor. The common systemic features reported were fatigue, glossitis, weight loss and anorexia that was found in 34%, 31%, 27% and 22% of cases respectively.[4] Hyper pigmentation of skin has been reported only rarely as the presenting manifestation of vitamin B12 deficiency as found in this patient.[5] There are only two such Indian reports found in Indian literature.[6,7] After the treatment, hematologic response begins after several days and, moreover, the final hematologic landmark is the blood count, including mean corpuscular volume (MCV) that should be completely normal by the eighth week.[8] The cutaneous manifestation of vitamin B12 deficiency is skin hyper pigmentation, vitiligo, hair changes, and recurrent angular stomatitis. Hyper pigmentation of the extremities especially over the dorsum of the hands and feet, with accentuation over the inter-phalangeal joints and terminal phalanges associated with pigmentation of oral mucosa is characteristic of vitamin B12 deficiency. Aaron et al., reported that 12 out of 63 (19%) patients had glossitis (31%), which was the most common mucocutaneous manifestation, followed by skin hyper pigmentation (19%), hair changes (9%), angular stomatitis (8%), and vitiligo (3%).[4] However, the present case had hyper pigmentation only. As evidenced by James et al., histology from the hyper pigmented area showed irregular epidermal atrophy, absence of basal orientation of epidermal cells, patchy pigmentation of the lower epidermis, and numerous pigment-laden macrophages in the upper dermis and increase of melanin in the basal layer. It is suggested that deficiency of vitamin B12 causes decrease in intracellular reduction potential that leads to oxidation of the reduced glutathione and decrease in GSH/GSSG ratio. The epidermal melanocytes are then stimulated to produce melanin as the tyrosinase inhibiting effect of GSH has been diminished.[9] So, the predominant mechanism of hyper pigmentation in vitamin B12 is hypothesised as 1) Deficiency of vitminB12 decreases the level of reduced glutathione, which activate tyrosinase and thus leads to transfer to melanosomes. 2) Defect in the melanin transfer between melanocytes and keratinocytes, resulting in pigmentary incontinence.[10] We consider that in present case the dominant mechanism of hyper pigmentation is not a defect in melanin transport but is rather an increase in melanin synthesis.
Table 2.
Recommended dietary allowances for vitamin B12/daily
This patient was treated with intramuscular injection of vitamin B12 (1000 mg) daily for ten days, then weekly for one month and then monthly for two months. Subsequently, the patient has been receiving a multivitamin tablet daily containing vitamin B12 (1 mg) and showed improvement in her presentation.[7]
CONCLUSION
Though a rare presentation, pigmentation due to vitamin B12 deficiency do mimic Addisons pigmentation. Vitamin B12 deficiency on the background history of vegetarian dietary intake should always be kept in mind after excluding Addisons disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Allen LH. How common is vitamin B-12 deficiency? Am J Clin Nutr. 2009;89:S693–6. doi: 10.3945/ajcn.2008.26947A. [DOI] [PubMed] [Google Scholar]
- 2.Washington DC: National Academy Press; 1998. Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes: Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. [PubMed] [Google Scholar]
- 3.Gupta A, Damji A, Uppaluri A. Vitamin B12 defiency. Prevalence among South Asians in Toronto clinic. Can Fam Physician. 2004;50:743–7. [PMC free article] [PubMed] [Google Scholar]
- 4.Aaron S, Kumar S, Vijayan J, Jacob J, Alexzander M, Gnanamuthu C. Clinical and laboratory features and response to treatment in patients presenting with vitamin B12 deficiency-related neurological syndromes. Neurol India. 2005;53:55–8. doi: 10.4103/0028-3886.15057. [DOI] [PubMed] [Google Scholar]
- 5.Hoffman CF, Palmer DM, Papadopoulos D. Vitamin B12 deficiency: A case report of ongoing cutaneous hyperpigmentation. Cutis. 2003;71:127–30. [PubMed] [Google Scholar]
- 6.Ahuja SR, Sharma RA. Reversible cutaneous hyperpigmentation in vitamin B12 deficiency. Indian Pediatr. 2003;40:170–1. [PubMed] [Google Scholar]
- 7.Srivastava N, Chand S, Bansal M, Srivastava K, Singh S. Reversible hyperpigmentation as the first manifestation of dietary vitamin B 12 deficiency. Indian J Dermatol Venereol Leprol. 2006;72:389–90. doi: 10.4103/0378-6323.27766. [DOI] [PubMed] [Google Scholar]
- 8.Carmel R. How I treat cobalamin (vitamin B12) deficiency. Blood. 2008;112:2214–21. doi: 10.1182/blood-2008-03-040253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gilliam JN, Cox AJ. Epidermal changes in vitamin B12 deficiency. Arch Dermatol. 1973;107:231–6. [PubMed] [Google Scholar]
- 10.Mori K, Ando I, Kukita A. Generalized hyperpigmentation of the skin due to vitamin B12 deficiency. J Dermatol. 2001;28:282–5. doi: 10.1111/j.1346-8138.2001.tb00134.x. [DOI] [PubMed] [Google Scholar]


