Abstract
A total number of 140 type 2 diabetic patients with diabetic retinopathy (DR) were enrolled in the study from diabetic clinic during May 2011 till June 2012 to determine correlation between severity of DR with serum lipid and other modifiable risk factors in type 2 diabetic patients. Information including age, sex, height, body weight, body mass index (BMI), waist-hip ratio (WHR), and systolic and diastolic blood pressure was collected from each patient. Fasting plasma sugar, low density lipoprotein (LDL), triglyceride level (TG), high density lipoprotein (HDL), glycated hemoglobin (HbA1C), creatinine, and 24 h urinary albumin excretion was done for each patient. Estimated glomerular filtration rate (eGFR) was measured by modification of diet in renal disease (MDRD) equation. Patients were divided in five groups according to retinopathy status based on early treatment DR study (ETDRS) disease severity level. Statistical analysis was performed with Statistical Packages for Social Sciences (SPSS) statistical software (version 17.0 for Windows). The alpha level was set at P = 0.05 for all tests. Statistically significant positive correlation between severity of DR with systolic blood pressure P = 0.005 (r = 0.974), diastolic blood pressure P = 0.001(r = 0.994), LDL P = 0.005 (r = 0.976), TG P = 0.001 (r = 0.990), and 24 h urinary albumin P = 0.004 (r = 0.977) was documented. DR was also strongly positively correlated with smoking P = 0.017 (r = 0.941) and duration of diabetes P = 0.003 (r = 0.981). There was strong inverse correlation of DR with HDL P = 0.001 (r = −0.994) and eGFR P = 0.002 (r = −0.987). Serum lipids were significantly correlated with severity of DR.
Keywords: Diabetic retinopathy, fasting blood sugar, low density lipoprotein
INTRODUCTION
Diabetic retinopathy (DR) is a major microvascular complication of diabetes accounting for its leading cause of irreversible blindness worldwide. Assessing the risk factors of DR, particularly modified risk factors, is important for early intervention to reduce the onset and progression of DR. Several population-based epidemiological studies have investigated the risk factors of DR.[1] These studies consistently established that a longer diabetic duration, hyperglycemia, and hypertension were associated with increased risk of DR. High serum lipid levels have also been proposed as a risk factor for DR. High lipid levels are known to cause endothelial dysfunction due to a reduced bioavailability of nitric oxide and this endothelial dysfunction was suggested to play a role in retinal exudate formation in DR.[2] It was also reported that the peroxidation of lipids in lipoproteins in the vascular wall leads to local production of reactive carbonyl species that mediate recruitment of macrophages, cellular activation and proliferation, and also chemical modification of vascular proteins by advanced lipoxidation end-products which affect both the structure and function of the vascular wall.[3] Consequently, it was proposed that, hyperlipidemia might contribute to DR and macular edema (ME) by endothelial dysfunction and breakdown of the blood retinal barrier leading to exudation of serum lipids and lipoproteins.[4]
Objective
To determine correlation between severity of DR with serum lipid and other modifiable risk factors in type 2 diabetic patients.
MATERIALS AND METHODS
This was a retrospective study done in department of endocrinology and metabolism LLRM medical college. A total number of 140 type 2 diabetic patients with DR were recruited from diabetic clinic during May 2011 till June 2012. Information including age, sex, height, body weight (WT), body mass index (BMI), waist-hip ratio (WHR), and systolic and diastolic blood pressure was collected from each patient. Fasting plasma sugar, low density lipoprotein (LDL), triglyceride level (TG), high density lipoprotein (HDL), glycated hemoglobin (HbA1C), creatinine, and 24 h urinary albumin excretion was done for each patient. Estimated glomerular filtration rate (eGFR) was measured by modification of diet in renal disease (MDRD). Patients were divided in five groups according to retinopathy status based on early treatment DR study (ETDRS) disease severity level.[5] Statistical analysis was performed with Statistical Packages for Social Sciences (SPSS) statistical software (version 17.0 for Windows). The alpha level was set at P = 0.05 for all tests.
RESULTS
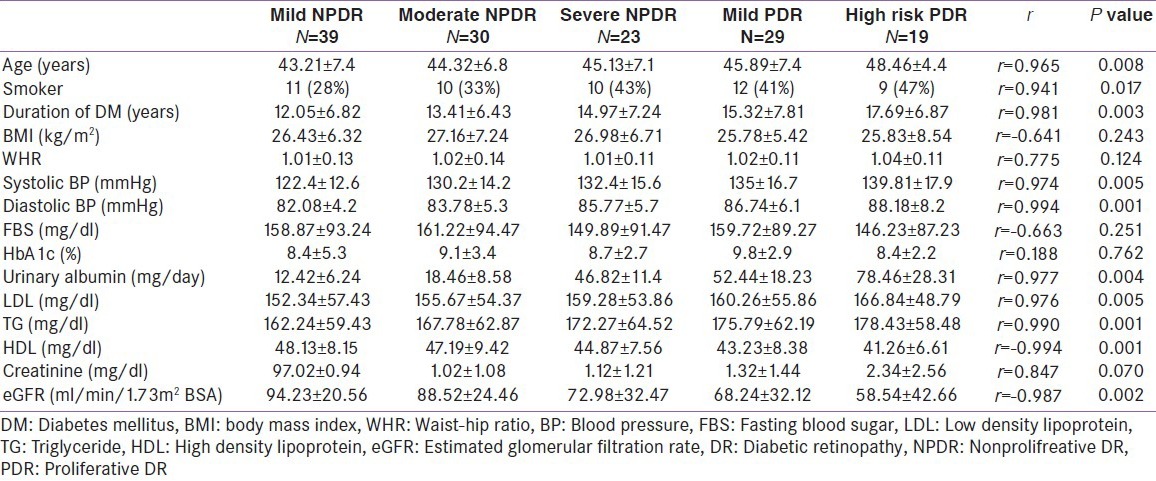
As shown in Table 1 there was statistically significant positive correlation between severity of DR and systolic blood pressure P = 0.005 (r = 0.974), diastolic blood pressure P = 0.001 (r = 0.994), LDL P = 0.005 (r = 0.976), TG P = 0.001 (r = 0.990), and 24 h urinary albumin P = 0.004 (r = 0.977). DR was also strongly positively correlated with smoking P = 0.017 (r = 0.941) and duration of diabetes P = 0.003 (r = 0.981). There was strong negative correlation of DR with HDL P = 0.001 (r = -0.994) and eGFR P = 0.002 (r = -0.987).
Table 1.
Clinical characteristic of different groups of DR
DISCUSSION
Endothelial dysfunction is a well-known finding in hypercholesterolemic patients and it was proposed that, hyperlipidemia might contribute to DR and ME by endothelial dysfunction and breakdown of the blood retinal barrier leading to exudation of serum lipids and lipoproteins.[4] In this study we have evaluated the modifiable risk factor of DR and there correlation with severity of DR. There are conflicting reports in the literature regarding the effect of lipid profile on retinopathy or maculopathy. In ETDRS it was shown that patients with high total cholesterol and LDL levels were more likely to have retinal hard exudates compared to patients with normal lipid profile.[6] In our study, we found a significant correlation between serum lipids and DR, but there was no association between HbA1c and DR. Similarly, Chennai Urban Rural Epidemiology Study showed that mean cholesterol, triglyceride, and non-HDL levels were higher in patients with DR compared to those without DR.[7]
CONCLUSION
Hypercholesterolemia, systolic and diastolic blood pressure, renal function, and urine albumin excretion is significantly associated with progression of DR.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Meta-Analysis for Eye Disease (META-EYE) Study Group. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landmesser U, Hornig B, Drexler H. Endothelial dysfunction in hypercholesterolemia: Mechanisms, pathophysiological importance, and therapeutic interventions. Semin Thromb Hemost. 2000;26:529–37. doi: 10.1055/s-2000-13209. [DOI] [PubMed] [Google Scholar]
- 3.Baynes JW, Thorpe SR. Glycoxidation and lipoxidation in atherogenesis. Free Radic Biol Med. 2000;28:1708–16. doi: 10.1016/s0891-5849(00)00228-8. [DOI] [PubMed] [Google Scholar]
- 4.Benarous R, Sasongko MB, Qureshi S, Fenwick E, Dirani M, Wong TY, et al. Differential association of serum lipids with diabetic retinopathy and diabetic macular edema. Invest Ophthalmol Vis Sci. 2011;52:7464–9. doi: 10.1167/iovs.11-7598. [DOI] [PubMed] [Google Scholar]
- 5.Early Treatment Diabetic Retinopathy Study design and baseline patient characteristics. ETDRS report number 7. Ophthalmology. 1991;98:741–56. doi: 10.1016/s0161-6420(13)38009-9. [DOI] [PubMed] [Google Scholar]
- 6.Chew EY, Klein ML, Ferris FL, 3rd, Remaley NA, Murphy RP, Chantry K, et al. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy. Early Treatment Diabetic Retinopathy Study (ETDRS) Report 22. Arch Ophthalmol. 1996;114:1079–84. doi: 10.1001/archopht.1996.01100140281004. [DOI] [PubMed] [Google Scholar]
- 7.Rema M, Srivastava BK, Anitha B, Deepa R, Mohan V. Association of serum lipids with diabetic retinopathy in urban South Indians-the Chennai Urban Rural Epidemiology Study (CURES) Eye Study-2. Diabet Med. 2006;23:1029–36. doi: 10.1111/j.1464-5491.2006.01890.x. [DOI] [PubMed] [Google Scholar]


