Abstract
Obesity in children and adolescents predispose to the development of obesity in adulthood and subsequent cardiovascular disease. High-sensitivity C-reactive protein (hsCRP) is a marker of low grade inflammatory state, which characterizes an atherosclerotic process. The aim of this study was to assess the metabolic abnormalities and its association with hsCRP in obese children and adolescents. A total of 62 obese children and adolescents and 24 healthy children and adolescents with a normal weight were recruited. In all subjects, anthropometric and biochemical parameters were measured. Body mass index (BMI) and blood pressure were significantly higher in the obese children and adolescents than the control. Obese children had significantly higher hsCRP levels (P < 0.001), total cholesterol, triglyceride, low-density lipoprotein-cholesterol (LDL-C) and lower high-density lipoprotein-cholesterol than the control group. Furthermore, homeostatic model assessment-insulin resistance (HOMA-IR) was significantly higher in obese children compared with the normal weight children. Furthermore, hsCRP showed a positive correlation with BMI (r = 0.357; P = 0.028), total cholesterol (r = 0.367; P = 0.008) and LDL-C (r = 0.356; P = 0.01), insulin (r = 0.311; P = 0.026) and not with HOMA-IR (r = 0.244; P = 0.084)). In conclusion, obese children and adolescents have significantly increased hsCRP compared with a normal weight group. Early intervention and prevention of obesity in children and adolescents decreases cardiovascular disease in later life.
Keywords: Cardiovascular risk, high sensitive C-reactive protein, obesity
INTRODUCTION
The global prevalence of overweight and obesity in children and adolescents has increased substantially over the past several decades.[1] These trends are also visible in developing countries like India. Many studies done previously,[2,3] suggest that children and adolescents with risk factors such as obesity, dyslipidemia, elevated blood pressure and impaired glucose metabolism are at increased risk of developing atherosclerosis in adulthood.
High-sensitivity C-reactive protein (hsCRP) has been emerged as a novel biomarker for vascular inflammation associated with atherosclerosis.[4] Accumulating evidence suggests that hsCRP, which is also found within macrophages of atheromatous plaques.[5] However, there is no much data available that guarantee its utility as a marker of cardiovascular risk in obese children and adolescents. Hence, the present study was taken up to assess the metabolic abnormalities and its association with hsCRP in obese children and adolescents.
MATERIALS AND METHODS
A total of 62 obese children and adolescents were consecutively recruited from our Department of Endocrinology and Metabolism, Nellore, Andhra Pradesh, India over a period of 14 months (October 2011 to December 2012).
Obesity was defined based on reference values stated in the Centers for Disease Control and Prevention growth chart (CDC charts). Children with body mass index (BMI) greater than the 95th percentile for age and gender were classified as obese. Those with BMI equal to or exceeding 85th percentile but, below the 95th percentile are defined as overweight. Secondary causes of obesity such as hypothyroidism, Cushing's disease and other causes were excluded. Children with other chronic disease, hereditary disease or systemic inflammation were also excluded. None of the patients was taking any medication at the time of evaluation for the presence of insulin resistance (IR) and impaired glucose tolerance/diabetes mellitus. 24 age-matched healthy children were taken as controls. The criteria for healthy control group were no major medical illness and normal glucose tolerance test according to the American Diabetes Association criteria. The study was approved by the Institutional Ethical Committee and informed consent was taken from parents.
Physical examination included measurements of height (by a stadiometer measuring with accuracy of 0.1 cm), weight (by electronic weighing machine) and blood pressure were obtained. BMI was calculated as the weight in kilograms divided by the height in meters squared. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured at the right arm after 15-min rest in sitting position using manual sphygmomanometer.
Biochemical measurements
After a 10-h overnight fast, venous blood samples were collected for laboratory evaluation of fasting glucose and insulin, triglycerides, total cholesterol and high-density lipoprotein (HDL) cholesterol and hsCRP. Glucose levels were measured by glucose oxidase and peroxidase method; triglycerides, total cholesterol were measured by the enzymatic and cholesterol oxidase methods respectively, HDL-cholesterol (HDL-C) were measured by direct immunoturbidimetry method. Low-density lipoprotein (LDL) were calculated by Friedewald's formula (LDL = TC – [TGL/5 + HDL]). Glucose and lipid levels were measured by commercially available in vitro assay kits from Human GmbH on HUMASTAR 600 (fully automated chemistry analyzer), Max-Planck-Ring 21, Wiesbaden, Germany. hsCRP was measured by immunoturbidimetric method (APTEC technologies) on HUMASTAR 600 (fully automated chemistry analyzer). Insulin was measured by chemilumniscence using Beckman immunoassays on Beckman Coulter Access 2, CA, USA. Both intra-assay and inter-assay coefficient of variations were lesser than 3.6% and 4.8%, respectively. IR was calculated using homeostatic model assessment-IR (HOMA-IR) according to the formula (HOMA-IR = plasma glucose [mg/dL] × insulin [mIU/L]/405).
Statistical analysis
All data were expressed as mean ± standard deviation. Statistical analysis was performed with SPSS 20.0. A statistically significant difference between two groups was assessed by the Student's unpaired two tailed t-test. Pearson's correlation analysis was performed to assess the relationship between hsCRP and other metabolic variables. A P < 0.05 was considered to be statistically significant.
RESULTS
Table 1 shows anthropometrical and biochemical characteristics of the study subjects. There is no significant difference between the study groups in terms of age and fasting plasma glucose. BMI, SBP and DBP were significantly elevated in obese children and adolescents compared to healthy controls. Fasting insulin levels (P < 0.001) and IR calculated by HOMA-IR (P < 0.001) and hsCRP (P < 0.001) were significantly higher in obese children and adolescents when compared with the healthy control group. Obese children and adolescents had significantly higher serum total cholesterol (P = 0.005), triglycerides (P < 0.001), LDL-cholesterol (LDL-C) (P = 0.006) and decreased HDL-C (P < 0.001) compared to control group.
Table 1.
Anthropometric and biochemical variables of the study subjects
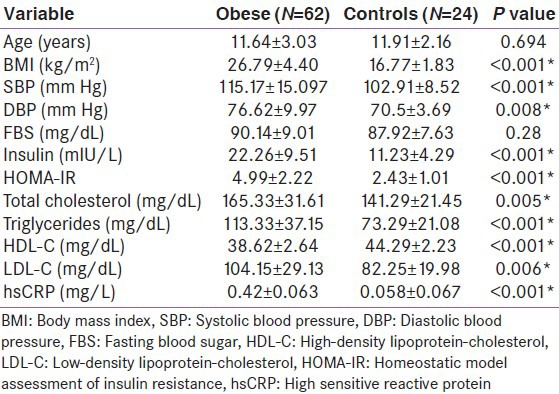
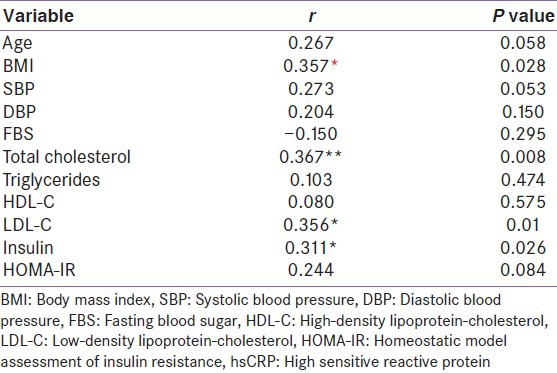
Table 2 shows Pearson's correlation analysis between hsCRP and metabolic variables. hsCRP showed a positive correlation with BMI (r = 0.357; P = 0.028), total cholesterol (r = 0.367; P = 0.008), LDL-C (r = 0.356; P = 0.01), insulin (r = 0.311; P = 0.026) and not with HOMA-IR (r = 0.244; P = 0.084). No significant association was found with BMI, triglycerides, HDL-C and HOMA-IR.
Table 2.
Pearson's correlation analysis between hsCRP and metabolic variable
DISCUSSION
This study is first of its kind from the Indian subcontinent, which shows the evidence for the presence of early cardiovascular risk factors in obese children and adolescents. Many studies,[6,7,8] have demonstrated a high cardiovascular risk profile in overweight and obese children and adolescents compared with a normal weight children.
In this study, compared with age matched and normal weight subjects, obese children and adolescents had higher SBP and DBP, total cholesterol, triglycerides, LDL-C, insulin, IR and hsCRP. In agreement with our study, Meyer et al.,[6] showed higher SBP and DBP, higher concentrations of fasting triglycerides, insulin and hsCRP in obese children compared with the normal weight controls.
Similarly, in another study done by Iannuzzi et al.,[9] demonstrated that obese children had higher levels of blood pressure, triglycerides, glucose, insulin, IR and CRP compared to the control group (100 obese children with 50 non-obese children). The probable mechanisms underlying this association with obesity is as follows; the cytokines such as tumor necrosis factor-α and interleukin-6 are released from adipose tissue and these cytokines stimulate the production of acute-phase proteins such as CRP in the liver.
Elevated hsCRP levels may be associated with the development of cardiovascular diseases and diabetes by means of a variety of mechanisms: altered sensitivity to insulin, increased liberation of adhesion molecules by endothelium, increase in hepatic production of fibrinogen and platelet coagulation factor.
In our study, hsCRP showed a positive correlation with BMI (r = 0.357; P = 0.028), total cholesterol (r = 0.367; P = 0.008) and LDL-C (r = 0.356; P = 0.01), insulin (r = 0.311; P = 0.026) and not with HOMA-IR (r = 0.244; P = 0.084). Similar to our study, Hatem et al.,[10] showed a positive correlation between hsCRP with BMI (r = 0.35; P ≤ 0.01) and insulin (r = 0.30; P = 0.01). Furthermore, hsCRP showed significant positive correlation with SBP and DBP and triglycerides. However, in our study, there is no significant association between hsCRP and blood pressure, triglycerides and HDL-C. In another study done by Weiss et al., showed that there exists no statistical relationship between hsCRP levels and metabolic risk factors.[11] The limitations of this study are: (1) Small sample size, (2) measurement of IR by HOMA-IR, not by the gold standard euglycemic glucose clamp technique.
CONCLUSION
Obese children and adolescents have significantly increased hsCRP compared with a normal weight group. Therefore, hsCRP seems to be an excellent cardiovascular marker in obese children and adolescents and could be a useful tool for the early diagnosis of cardiovascular risk factors among this population. Early intervention in these obese individuals can reduce the incidence of comorbidities in adulthood.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1:11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- 2.Raitakari OT, Juonala M, Kähönen M, Taittonen L, Laitinen T, Mäki-Torkko N, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: The cardiovascular risk in young finns study. JAMA. 2003;290:2277–83. doi: 10.1001/jama.290.17.2277. [DOI] [PubMed] [Google Scholar]
- 3.Li S, Chen W, Srinivasan SR, Bond MG, Tang R, Urbina EM, et al. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: The Bogalusa heart study. JAMA. 2003;290:2271–6. doi: 10.1001/jama.290.17.2271. [DOI] [PubMed] [Google Scholar]
- 4.Ridker PM. C-reactive protein and the prediction of cardiovascular events among those at intermediate risk: Moving an inflammatory hypothesis toward consensus. J Am Coll Cardiol. 2007;49:2129–38. doi: 10.1016/j.jacc.2007.02.052. [DOI] [PubMed] [Google Scholar]
- 5.Capuzzi DM, Freeman JS. CRP and cardiovascular risk in the metabolic syndrome. Clin Diabetes. 2007;25:16–22. [Google Scholar]
- 6.Meyer AA, Kundt G, Steiner M, Schuff-Werner P, Kienast W. Impaired flow-mediated vasodilation, carotid artery intima-media thickening, and elevated endothelial plasma markers in obese children: The impact of cardiovascular risk factors. Pediatrics. 2006;117:1560–7. doi: 10.1542/peds.2005-2140. [DOI] [PubMed] [Google Scholar]
- 7.Kapiotis S, Holzer G, Schaller G, Haumer M, Widhalm H, Weghuber D, et al. A proinflammatory state is detectable in obese children and is accompanied by functional and morphological vascular changes. Arterioscler Thromb Vasc Biol. 2006;26:2541–6. doi: 10.1161/01.ATV.0000245795.08139.70. [DOI] [PubMed] [Google Scholar]
- 8.Schiel R, Beltschikow W, Kramer G, Stein G. Overweight, obesity and elevated blood pressure in children and adolescents. Eur J Med Res. 2006;11:97–101. [PubMed] [Google Scholar]
- 9.Iannuzzi A, Licenziati MR, Acampora C, Salvatore V, De Marco D, Mayer MC, et al. Preclinical changes in the mechanical properties of abdominal aorta in obese children. Metabolism. 2004;53:1243–6. doi: 10.1016/j.metabol.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 10.Hatem HE, Ibraheim AG. High-sensitivity C-reactive protein as a marker of cardiovascular risk in obese children and adolescents. Health. 2010;2:1078–84. [Google Scholar]
- 11.Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350:2362–74. doi: 10.1056/NEJMoa031049. [DOI] [PubMed] [Google Scholar]


