Abstract
A 36-year-old woman presented with haematuria and a bladder mass on ultrasonogram. Cystoscopy revealed a tumour, cauliflower in shape with smooth stalk coming out from the ureteric orifice. Stalk of the polyp was identified in proximal ureter by ureteroscopy. The mass was excised endoscopically.
Background
Fibroepithelial polyp is a benign neoplasm that originates from the connective tissue elements in the genitourinary system.1 2 It is an uncommon lesion and can present as a diagnostic dilemma. The presenting symptoms are vague and non-specific and hence it can be difficult to diagnose preoperatively. We present a case of a fibroepithelial polyp in a young woman which could be diagnosed and treated endoscopically.
Case presentation
A 35-year-old woman was admitted with painless haematuria and occasional right flank pain which was self-limiting, non-radiating and mild in intensity. Her general physical examination was within normal limits.
Investigations
Abdominal ultrasound examination demonstrated an echogenic, polypoid mass in the bladder.
At cystoscopy, a tumour was seen protruding from the ureteral orifice. The surface of the tumour was smooth and it did not bleed on touch. On application of pressure on the ipsilateral flank, the mass could be seen extruding out from the ureteric orifice on its stalk. Ureteroscopy was performed with a semirigid scope, which revealed a polypoid ureteral lesion starting from the proximal right ureter and protruding into the bladder.
Differential diagnosis
The differential diagnosis, on imaging, may range from conditions like transitional cell carcinoma of the ureter, bladder tumour involving the vesicoureteric junction, blood clot due to bleeding from the upper tract, etc.3
Treatment
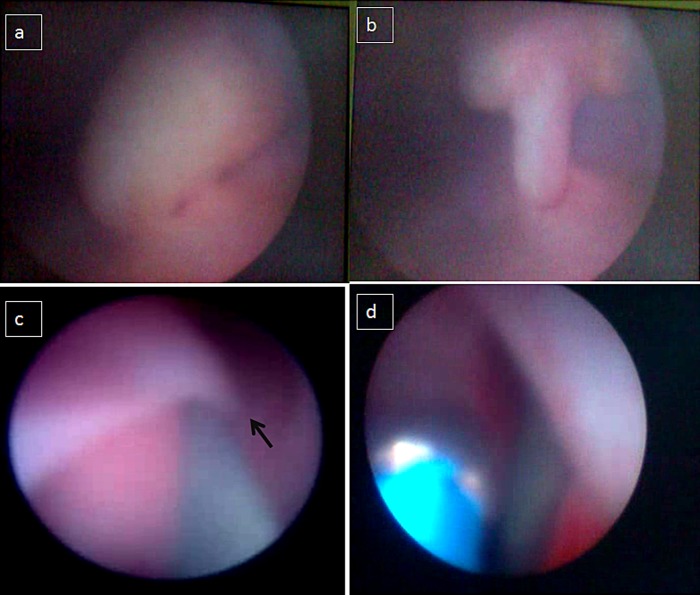
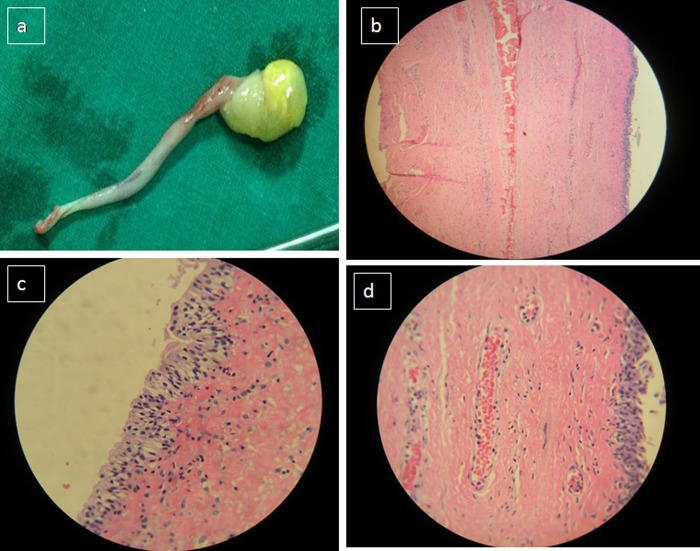
The stalk of lesion was fulgurated with bugbee electrode and the lesion was avulsed from its base by a grasping forceps (figure 1). The base was fulgurated and a double J stent was inserted. The histopathological examination confirmed the diagnosis of fibroepithelial polyp (figure 2).
Figure 1.
(A) The lesion as seen on cystoscopy. (B) The stalk of the tumour seen coming out of the right ureteric orifice. (C) The base of the stalk as seen on ureteroscopy with a semirigid ureteroscope (arrow). The guide wire is also seen in the ureter. (D) The origin of the stalk being fulgurated by a bugbee electrode.
Figure 2.
(A) The excised tumour. (B) The microscopic examination (H&E, ×10) reveals a well-formed epithelium and a loose fibrovascular stroma. (C and D) The microscopic examination (H&E, ×40) reveals a well-formed transitional epithelium and the fibrovascular core.
Outcome and follow-up
The stent was removed at 4 weeks. Ultrasonography 2 month later did not reveal any abnormality. The patient should be on a long-term follow-up as occasional recurrences have been reported.
Discussion
Primary ureteral tumours are probably the rarest in the spectrum of genitourinary tumours and are most often malignant. Benign primary ureteral tumours are exceptionally rare and among them, fibroepithelial polyps are considered to be the commonest lesions.2 Though the exact aetiopathogenesis of fibroepithelial polyps is not known, they are presumed to be a result of chronic or recurrent infection and inflammation of the urinary tract. Though they most commonly present in young adults substantiating their acquired nature, they can rarely be congenital.2 In majority of the cases, upper ureter is the most common site of origin of these tumours.4 The clinical presentation is non-specific. The radiological signs are also not confirmatory. The intravenous urogram or a CT scan may show a filling defect in the ureter and bladder but there are no signs that can conclusively point towards the diagnosis.5 Endoscopic examination by a cystoureteroscope may aid in the diagnosis by showing the nature of the tumour and the site of origin.6 If there is a doubt about the diagnosis, a biopsy of the lesion with the help of biopsy forceps or resectoscope can be performed.
The management of these tumours varies. A few decades ago, nephroureterectomies have been performed in patients with these tumours because of the uncertainty of the diagnosis and lack of substantial literature regarding their management.7 There is still a lack of consensus regarding the optimal management of these tumours due to their rarity. The current management depends on the site, size and the clinical expertise. Smaller lesions can be simply fulgurated endoscopically while larger lesions need a formal surgical excision.8 The excision has been conventionally performed by open or laparoscopic techniques. These range from excision by doing a ureterotomy, excision of a cuff of the ureter containing the base of the tumour followed by ureteroureterostomy, etc.6 A formal, dismembered pyeloplasty may be needed in cases where the tumour originates from the ureteropelvic junction, especially if associated with the narrowing of the junction.9 Lesions in the renal pelvis have also been managed by percutaneous modalities.10 Lesions from bladder and urethra can be managed by transurethral resection. Of late, endoscopic excision has been described to be of success in the treatment. This can be performed by endoscopic avulsion with the help of grasping forceps, excision by the help of electrocautery.5 Some of the authors have recently recommended the use of Holmium laser for the endoscopic excision of these tumours.10
Learning points.
Patients with fibroepithelial polyps of the ureter present with non-specific signs and symptoms.
Endoscopic examination clears the diagnosis.
Endoscopic excision is an excellent modality of treatment.
Footnotes
Contributors: RKS was involved in data collection, data interpretation, writing, editing and review of the manuscript. TJ was involved in writing, review and editing of the manuscript. MRK was involved in data collection. DK was involved in review and editing of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kim H, Kim DK, Lee SJ, et al. Fibroepithelial ureteral polyp: a case report; endoscopic removal of large ureteral polyp. J Korean Med Sci 1996;2013:80–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turunc T, Kuzgunbay B, Canpolat T. Ureteral fibroepithelial polyps with calculi: a case series. J Med Case Rep 2008;2013:280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang ZJ, Meng MV, Yeh BM, et al. Ureteral fibroepithelial polyp. J Ultrasound Med 2008;2013:1647–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams TR, Wagner BJ, Corse WR, et al. Fibroepithelial polyps of the urinary tract. Abdom Imaging 2001;2013:217–21 [DOI] [PubMed] [Google Scholar]
- 5.Childs MA, Eric C, Umbreit EC, et al. Fibroepithelial polyps of the ureter: a single-institutional experience. J Endourol 2009;2013:1415–19 [DOI] [PubMed] [Google Scholar]
- 6.Seçkin B, Bedir S, Sumer F, et al. Fibroepithelial polyp of the ureter in a young adult. J Ankara Med Sch 2003;2013:161–4 [Google Scholar]
- 7.Chang HH, Ray P, Ockuly E, et al. Benign fibrous ureteral polyps. Urology 1987;2013:114–18 [DOI] [PubMed] [Google Scholar]
- 8.Bolton D, Stoller ML, Irby P., III Fibroepithelial ureteral polyps and urolithiasis. Urology 1994;2013:582–7 [DOI] [PubMed] [Google Scholar]
- 9.Romesburg JW, Stein RJ, Desai MM, et al. Treatment of child with bilateral ureteropelvic junction obstruction due to fibroepithelial polyps and review of the literature. Urology 2009;2013:929.e9–11 [DOI] [PubMed] [Google Scholar]
- 10.Lam JS, Bingham JB, Gupta M. Endoscopic treatment of fibroepithelial polyps of the renal pelvis and ureter. Urology 2003;2013:810–13 [DOI] [PubMed] [Google Scholar]