Description
A 77-year-old man presented to the emergency room with a 3-week history of progressive abdominal discomfort. His medical history revealed hypertension and chronic obstructive pulmonary disease (COPD). His symptoms consisted of nausea, anorexia, weight loss, constipation and dyspnoea d'effort.
Clinical examination revealed jaundice and a diffusely painful abdomen. Laboratory results included elevated C reactive protein (51 (<10) mg/L) and erythrocyte sedimentation rate (13 (1–7) mm/h), renal insufficiency (urea 18 (2.9–7.5) mmol/L and creatinine 180 (62–106) µmol/L) and elevated liver enzymes (bilirubin 135 (<17) µmol/L, with conjugated bilirubin 117 (<5) µmol/L, alkaline phosphatase 353 (<115) U/L, GGT 1050 (<55) U/L, alanine transaminase 154 (<45) U/L, aspartate aminotransferase 190 (<35) U/L, lactate dehydrogenase 425 (<220) U/L). An abdominal ultrasound showed an inhomogeneously enlarged liver which was suspected to be metastatic disease. Subsequently, a diagnostic ascitic fluid sample was taken and a CT was performed (figure 1).
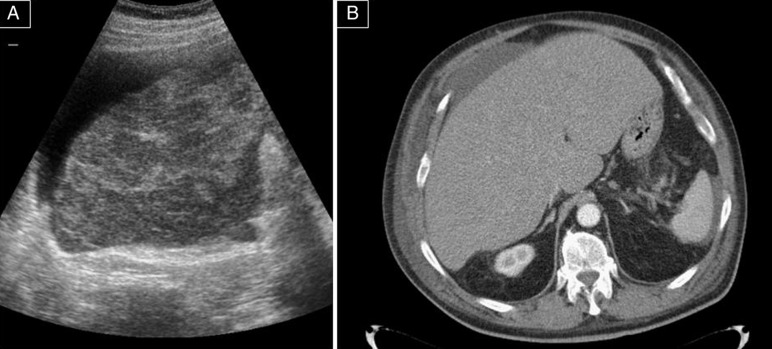
Figure 1.
Imaging studies: ultrasound and CT scan. (A) Abdominal ultrasound shows an enlarged and very inhomogeneous liver with ascites. No normal liver parenchyma is recognisable. (B) Contrast-enhanced CT of the abdomen showing an enlarged but almost homogeneous liver, despite the numerous lesions.
The next day, the patient developed a severe lactic acidosis (lactic acid 13 mmol/L, pH 7.14, pCO2 1.9 kPa, HCO3 4.8 mmol/L, BE −21.1 mmol/L), with impending respiratory exhaustion, and he was admitted to the intensive care unit. He was resuscitated and a liver biopsy was performed which revealed a small cell carcinoma. Cytology of the ascites also showed signs of metastases of small cell carcinoma.
Considering the very poor prognosis, treatment was restricted to pain control and comfort care, after which the patient soon passed away. Autopsy revealed an enlarged liver that was almost fully superseded by primary small cell carcinoma (figure 2), metastatic disease in the bone marrow and lymph nodes and extensive ischaemia of the small intestine and colon.
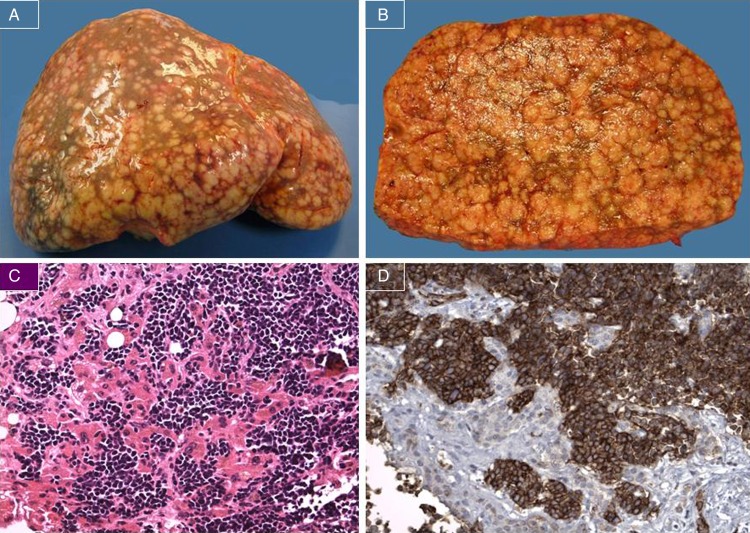
Figure 2.
Histology: macroscopy and microscopy. (A) and (B) Grossly enlarged liver (5406 g) with multiple, irregular small nodules. (C) H&E staining; liver with infiltration of malignant cells with a solid growth pattern. The tumour cells have hyperchromatic nuclei, ‘salt and pepper’-chromatin and inspicious nucleoli (original magnification ×20). (D) Immunohistochemical staining for CD56 showing a strongly positive reaction consistent with a small cell carcinoma (original magnification ×20).
Learning points.
Small cell carcinoma (SCC) usually arises in the lung, but can also originate in a wide range of extrapulmonary sites, including the liver, oesophagus, stomach, colon, gallbladder, cervix and skin. However, extrapulmonary SCCs are extremely rare.1–3
Malignant disease can present with intestinal ischaemia.
Lactic acidosis is suggestive, although not specific, for intestinal ischaemia.
Abdominal ultrasound can be more sensitive than CT in cases like these with widespread metastatic liver disease when the liver was entirely superseded, leaving almost no normal liver parenchyma.
Footnotes
Contributors: MO, SS, KvE and LH contributed significantly towards the writing of the manuscript and approved the final manuscript for publication.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Frazier SR, Kaplan PA, Loy TS. The pathology of extrapulmonary small cell carcinoma. Semin Oncol 2007;2013:30–8 [DOI] [PubMed] [Google Scholar]
- 2.Kaman L, Iqbal J, Pall M, et al. Primary small cell carcinoma of liver: A rare tumor. Gastroenterology Res 2010;2013:180–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim YH, Kwon R, Jung GJ, et al. Extrapulmonary small-cell carcinoma of the liver. J Hepatobiliary Pancreat Surg 2004;2013:333–7 [DOI] [PubMed] [Google Scholar]