Abstract
Introduction
Diarrhea contributed for 17.6% of under-five deaths in Botswana. Oral rehydration salt (ORS) therapy has been the cornerstone in the control of morbidity and mortality secondary to diarrheal diseases. The study was aimed at assessing the household availability of ORS following the nationwide campaign of availing ORS at household level.
Methods
A cross sectional community based study was conducted in August 2012. EPI random walk method was used to identify households. Data was collected using interviewers' administered structured questionnaire. SPSS software was used in data entry and analysis.
Results
Oral Rehydration Salt (ORS) was available in 50.8% of the households with under-five children. Information on ORS is well disseminated whereas only three-fourth of informed participants had adequate knowledge of ORS preparation. The sources of information were predominantly the Child Welfare Clinic (88.8%). Being grandmother as a care taker was a negative predictor of household availability of ORS (AOR 0.25, 95% CI 0.09-0.69) while respondents who are knowledgeable about ORS preparation were more likely to have ORS available at home (AOR 1.92, 95% CI 1.10-3.34).
Conclusion
The campaign has brought a significant coverage in terms of availability of ORS. The health education and community sensitization efforts need to go beyond health facilities via other means like the media and community based approaches. Approaches aimed at improving the knowledge of care takers on the importance of ORS, its preparation, correct use and restocking are of paramount importance. Availing community based outlet for ORS is an alternative to enhance accessibility.
Keywords: Oral, Rehydration, Salt, ORS, availability, Botswana
Introduction
Globally there were 6.9 million deaths of children under the age of five years in 2011. The causes in two-third of the deaths were preventable infectious diseases. The largest global burden of childhood death is found in Sub-Saharan Africa housing 23 countries with Under-five mortality rate above 100 deaths per 1000 live births. The 2011 under-five mortality rate in Botswana was reported to be 26 deaths per 1000 live births [1]. A systematic analysis in 2008 estimated that the contribution of diarrheal diseases towards childhood mortality was 15% globally and 19% in Africa alone [2]. In 2007, Diarrhea and Pneumonia were reported as the major causes of under-five deaths in Botswana (17.6% and 14.7% respectively)[3].
Oral Rehydration Salt (ORS) therapy is one of the recognized evidence based interventions used to reduce child morbidity and mortality in diarrheal diseases worldwide. Other interventions include breast feeding, complementary feeding, water, sanitation, hygiene, Rotavirus vaccine, Antibiotics, Zinc and Vitamin-A [4–13]. Availability of ORS at community level has been shown to reduce diarrhea related mortality among under-five children [4]. Combining ORS with other interventions has also been shown to significantly increase the extent of reduction in diarrhea related morbidity [14].
Oral rehydration therapy has been the cornerstone in the control of morbidity and mortality secondary to diarrhoeal diseases since 1979. With the increased use of ORS around the world, the overall mortality secondary to diarrhoeal disease has dropped dramatically [5]. In April 2012 the Ministry of Health of Botswana launched a national campaign to ensure that all households with children under the age of 5 years have ORS and Zinc tablets readily available at home. This approach was suggested in response to the increasing number of children presenting severely dehydrated to the health facilities with resultant deaths. The aim of this study was therefore to assess the household availability of ORS following the introduction of the nationwide campaign.
Methods
Study site and population
A descriptive cross-sectional study was conducted in Kweneng District of Botswana. According to the 2011 housing and population census, Kweneng district has an estimated total population of 304,674 with a density of 9.8 persons per square kilometer [15]. The study participants were recruited from Molepolole village which is the headquarters of Kweneng district. This village has a population of 67,598 [15]. The study was conducted amongst households in Molepolole with children under the age of 5 years. The participants of this study were parents or guardians of children under the age of 5 years.
Sample size and sampling
The sample size was determined using EpiInfo 3.5.3 software. The coverage of the current ORS availability was assumed to be 25%. There is no estimate for household availability of ORS and one quarter of the households with under-five children were expected to have ORS at the early phase of the nationwide campaign. With margin of error of 5% and 5% level of significance, a sample size of 288 was targeted. In the actual data collection, a sample size of 295 was attained. EPI-random walk method was used to select the households around the areas served by the 4 clinics in Molepolole.
Data collection and analysis
A questionnaire was adapted from the standard Demographic and Health Survey questionnaire [16]. The questionnaire was prepared and administered using the local language. Five enumerators trained on the data collection instrument collected the information. The principal investigators were involved in the supervision of the data collection. Data was collected between August 11-13, 2012.
Epi-Info software version 3.5.3 was used for data entry and descriptive data analysis while SPSS software version 20 was used for bi-variate and multi-variate analysis. Frequency, percentage and mean were computed to describe the findings. The crude and adjusted odds ratio (COR/ AOR) and 95% Confidence Interval (CI) were analyzed to explore associations and a p-value of 0.05 or less was considered statistically significant.
Ethical issues
Ethical approval was obtained from the University of Botswana Institutional Review Board and Botswana Ministry of Health Research unit. Permission was granted by the local administrators and written informed consent was secured from each participant before the conduct of the interview.
Results
A total of 295 care takers of children were enrolled in the study with mean age of 35 and a standard deviation of 13 years. The study participants were predominantly females with the large majority reporting some form of formal education. Mothers and grandmothers constituted one-third and one-six of the sample population respectively (Table 1).
Table 1.
Background characteristics of study participations, Molepolole, 2012
| Characteristic | Frequency | Percentage |
|---|---|---|
| Age | ||
| 16-30 | 144 | 48.8% |
| 31-40 | 69 | 23.4% |
| 41 and above | 81 | 27.5 |
| No response | 1 | 0.3% |
| Gender of parent/guardian | ||
| Male | 10 | 3.4% |
| Female | 285 | 96.6% |
| Education Level | ||
| No education | 32 | 10.8% |
| Primary | 69 | 23.4% |
| Junior Secondary | 117 | 39.7% |
| Senior Secondary | 52 | 17.6% |
| Tertiary | 20 | 6.8% |
| No response | 5 | 1.7% |
| Relationship to the child | ||
| Mother | 196 | 66.4% |
| Father | 7 | 2.4% |
| Grandmother | 48 | 16.3% |
| Sister | 2 | 0.7% |
| Uncle | 2 | 0.7% |
| Aunt | 9 | 3.1% |
| Other relatives | 24 | 8.1% |
| Non-relative guardian | 7 | 2.4% |
Over 98% of the participants reported possession of information regarding Oral Rehydration Salt. However the proportion of the participants who have adequate knowledge regarding the preparation and use of ORS were 219 (74.2%). Their source of information was predominantly from the Child Welfare Clinic (88.8%). Other sources of information reported included hospital (3.8%), friends (4.7%), Radio (4.1%), Television (3.1%), Clinic Card (1.8%) and school (1%). Printed materials like Pamphlets, Posters or Books were mentioned as sources of information by 1.7% while electronic media and social mobilization were not mentioned by any one. The large majority (99%) of the study participants reported that their child attended Child Welfare Clinic regularly.
The household availability of ORS and Zinc Sulphate tablets were 50.8% and 30.2% respectively. Of 145 households without ORS at home, 62 (42.7%) reported to have used up the available ORS while 56 (38.6%) never had it at home. Of 206 households without Zinc Sulphate at home, 120 (58.3%) never had access to the tablet and 54 (26.2%) reported to have used up their supply (Table 2).
Table 2.
Availability of ORS and Zinc Sulphate at households, Molepolole, 2012
| Characteristic | Frequency | Percentage |
|---|---|---|
| Availability of ORS at home | ||
| Yes | 150 | 50.8% |
| No | 145 | 49.2% |
| Reason for unavailability of ORS | ||
| Child doesn't have diarrhoea | 19 | 13.1% |
| Expired packets | 1 | 0.7% |
| Never given | 56 | 38.6% |
| Used up | 62 | 42.7% |
| Unsure | 4 | 2.8% |
| No response | 3 | 2.1% |
| Availability of Zinc Sulphate at home | ||
| Yes | 89 | 30.2% |
| No | 206 | 69.8% |
| Reason for unavailability of Zinc Sulphate | ||
| Child doesn't have diarrhoea | 15 | 7.3% |
| Never given | 120 | 58.3% |
| Used up | 54 | 26.2% |
| Unsure | 8 | 3.9% |
| Thrown away | 1 | 0.5% |
| No response | 8 | 3.9% |
The sources of ORS among the 150 households with ORS were the Child welfare Clinic (88%) and a public hospital (8.7%) while 3.3% did not specify the source (Figure 1). Of the 89 households with Zinc Sulphate tablets readily available, they obtained it from Child welfare clinic (89.9%), public hospital (7.9%) and private pharmacy (1.1%).
Figure 1.
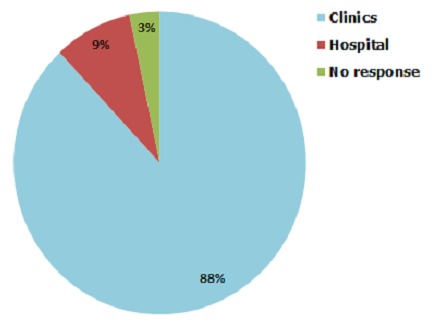
Source of medication among households keeping ORS at home
Being grandmother as a care taker was a negative predictor of household availability of ORS (AOR 0.25, 95% CI 0.09-0.69) while respondents who are knowledgeable about ORS preparation were more likely to have ORS available at home (AOR 1.92, 95% CI 1.10-3.34) (Table 3).
Table 3.
Factors associated with availability of ORS at home, Molepolole, 2012
| Characteristic | ORS available at home | Crude OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|---|---|
| Yes | No | |||
| Age | ||||
| 16-30 | 77 | 67 | 1.00 | 1.00 |
| 31-40 | 33 | 36 | 0.79 (0.45, 1.42) | 0.69 (0.37, 1.28) |
| 41 and above | 40 | 41 | 0.85 (0.49, 1.46) | 1.64 (0.62, 4.39) |
| Relationship of care taker | ||||
| Parent | 111 | 92 | 1.00 | 1.00 |
| Grandmother | 17 | 31 | 0.46 (0.24, 0.87) | 0.25 (0.09, 0.69) |
| Other care takers | 22 | 22 | 0.83 (0.43, 1.59) | 0.68 (0.33, 1.41) |
| Education Level | ||||
| No formal education | 19 | 13 | 1.00 | 1.00 |
| Primary | 31 | 38 | 0.56 (0.24, 1.31) | 0.46 (0.19, 1.13) |
| Secondary and above | 96 | 93 | 0.71 (0.33, 1.51) | 0.53 (0.22, 1.33) |
| Knows how to prepare ORS | ||||
| Yes | 120 | 99 | 1.86 (1.09, 3.16) | 1.92 (1.10, 3.34) |
| No | 30 | 46 | 1.00 | 1.00 |
Discussion
Reducing diarrhea morbidity and mortality isa key to achieving the fourth MillenniumDevelopment Goal of reducing child mortality by two-thirds by 2015 (MDG4) [17]. ORS therapy has been shown to play significant role in the reduction of child mortality secondary to diarrheal disease [4, 5, 14]. The findings from this study highlight the areas that need attention in order to improve knowledge, availability and use of ORS.
It is noted that while information on ORS is widely available, only three-fourth of informed participants had adequate knowledge of ORS preparation. Adequate knowledge refers to acquaintance to the method of reconstitution from the packet and daily preparation. A similar finding was reported by a study conducted in rural Bangladesh in 2002 where two-third of the respondents who recognized ORS packet knew how to prepare ORS correctly [18]. It is an indication that the health education efforts need to go beyond information dissemination. More effective measures are needed to empower caretakers on the preparation and use of ORS.
Health facilities especially the Child Welfare Clinics were the principal sources of information about ORS and Zinc Sulphate. The large majority of the children are regular attendees of Child Welfare Clinics and using such an important opportunity to propagate child health information including correct use of ORS is regarded as crucial to extending knowledge and improving practice and use of ORS. The media, printed material and community mobilization were mentioned as sources of information by the minority. One tenth of the care takers never had a formal education and health education approaches need to take in to account such segments of the population. The health information at the Clinics needs to be augmented by other approaches including community based intervention to maintain knowledge and enhance behavior change. Intervention studies have demonstrated that audio-visual and community based approaches were effective in improving knowledge about ORS, child health and survival [19, 20].
Studies done in Botswana to assess the practice of keeping ORS and or Zinc sulphate tablets at home prior to the April 2012 national campaign could not be found in the literature. It is however postulated that keeping ORS and/or Zinc Sulphate at household level used to be uncommon practice before the launching of the campaign. The level of availability of ORS and Zinc Sulphate few months after the campaign is encouraging. The availability of ORS was better than that of Zinc Sulphate. This may be explained by Zinc Sulphate tablets being less readily available in the health facilities or health workers not dispensing the tablets as required.
Some caretakers without ORS or Zinc Sulphate were not replenishing the medications once used up. The health educators need to emphasize on the need to replenish the medications once used up. Accessibility of health facilities might also be a hindrance in the re-fill and an alternative way of community outlets for the medications might be helpful as was demonstrated by a study conducted in Bangladesh [4]. A good number of the participants reported never having had access to either ORS or Zinc Sulphate. The opportunity at the Child Welfare Clinic needs to be exploited such that the clinic can distribute and replenish ORS/ Zinc Sulphate at the follow-up visits to all attendants. Care takers who already own the medications can also be used as change agents in mobilizing other households with ORS unavailable at home.
The study demonstrated that grandmother caretakers were less likely to have ORS at home. This calls for targeted health education efforts to increase knowledge and bring about behavior change among the grandmother caretakers. Participants who are knowledgeable about ORS preparation and correct use were more likely to have ORS available at home. Knowledgeable parents or guardians will make sure that ORS is available at home and use it appropriately. This makes increasing parents and guardian's knowledge about ORS much more imperative and a more effective way of ensuring that most households have a knowledgeable caretaker.
The study finding needs to be interpreted with some caution. The study did not directly assess the association between home availability of ORS and the treatment of children with recent history of diarrhea, and positive outcome of morbidity and mortality reduction. The use of non-probability sampling is also another limitation to note which will affect the generalizability of the findings to populations outside of the study area.
Conclusion
The Botswana nationwide ORS distribution campaign appears to have contributed to significant population coverage in terms of availability of ORS at household level. The effort at the Child Welfare Clinics alone might not be sufficient to capitalize on the achievement and sustain the improvement in the coverage. The health education and community sensitization efforts need to be intensified through incorporating other means of communication such as the media and community based approaches. Approaches aimed at improving the knowledge of care takers on the importance of ORS, its preparation, correct use and restocking are of paramount importance. Further attention needs to be paid to sensitizing uneducated and older care takers in order to maximize the potential overall benefits of the health promotion messages. Availing a community based outlet for ORS is an alternative option to enhance accessibility. Further study is recommended to assess the ultimate direct benefit of ORS availability in the reduction of morbidity and mortality from childhood diarrheal disease in Botswana.
Acknowledgments
The authors greatly acknowledge the study participants for their cooperation. The staffs of Child Health Division at the Ministry of Health and Kweneng District Health Management Team deserve recognition for the provision of information. We also would like to thank the Year IV Medical Students, University of Botswana who participated in the data collection.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors were involved in the design, data analysis and interpretation reviewed the draft manuscript and approved the final version of the manuscript. Dereje Habte was involved in the drafting of the manuscript.
References
- 1.You D, Jin NR, Wardlaw T. New York: United Nations Children's Fund; Levels and Trends in Child Mortality. Report 2012. [Google Scholar]
- 2.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375(9730):1969–1987. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 3.CSO. Botswana: CSO; 2010. Botswana Causes of Mortality, 2008. [Google Scholar]
- 4.Mujibur Rahaman M, Patwari Y, Aziz KMS, Munshi MH. Diarrhoeal mortality in two Bangladeshi villages with and without community-based oral rehydration therapy. The Lancet. 1979;314(8147):809–812. doi: 10.1016/s0140-6736(79)92172-x. [DOI] [PubMed] [Google Scholar]
- 5.Victora CG, Bryce J, Fontaine O, Monasch R. Reducing deaths from diarrhoea through oral rehydration therapy. Bulletin-World Health Organization. 2000;78(10):1246–1255. [PMC free article] [PubMed] [Google Scholar]
- 6.Arifeen S, Black RE, Antelman G, Baqui A, Caulfield L, Becker S. Exclusive breastfeeding reduces acute respiratory infection and diarrhea deaths among infants in Dhaka slums. Pediatrics. 2001;108(4):67–e67. doi: 10.1542/peds.108.4.e67. [DOI] [PubMed] [Google Scholar]
- 7.Quigley MA, Cumberland P, Cowden JM, Rodrigues LC. How protective is breast feeding against diarrhoeal disease in infants in 1990s England: A case-control study. Archives of disease in childhood. 2006;91(3):245–250. doi: 10.1136/adc.2005.074260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gross R, Giay T, Sastroamidjojo S, Schultink W, Lang NT. Premature complementary feeding is associated with poorer growth of Vietnamese children. The Journal of nutrition. 2000;130(11):2683–2690. doi: 10.1093/jn/130.11.2683. [DOI] [PubMed] [Google Scholar]
- 9.Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. The Lancet infectious diseases. 2005;5(1):42–52. doi: 10.1016/S1473-3099(04)01253-8. [DOI] [PubMed] [Google Scholar]
- 10.Vesikari T, Isolauri E, D'Hondt E, Delem A, André F, Zissis G. Protection of infants against rotavirus diarrhoea by RIT 4237 attenuated bovine rotavirus strain vaccine. The Lancet. 1984;323(8384):977–981. doi: 10.1016/s0140-6736(84)92323-7. [DOI] [PubMed] [Google Scholar]
- 11.Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS. How many child deaths can we prevent this year. Lancet. 2003;362(9377):65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- 12.Baqui AH, Black RE, Arifeen SE, Yunus M, Chakraborty J, Ahmed S, Vaughan JP. Effect of zinc supplementation started during diarrhoea on morbidity and mortality in Bangladeshi children: community randomised trial. BMJ. 2002;325(7372):1059. doi: 10.1136/bmj.325.7372.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ross DA, Dollimore N, Smith PG, Kirkwood BR, Arthur P, Morris SS, et al. Vitamin A supplementation in northern Ghana: effects on clinic attendances, hospital admissions, and child mortality. The Lancet. 1993;342(8862):7–12. [PubMed] [Google Scholar]
- 14.Gutieérrez G, Tapia-Conyer R, Guiscafreé H, Reyes H, Martinez H, Kumate J. Impact of oral rehydration and selected public health interventions on reduction of mortality from childhood diarrhoeal diseases in Mexico. Bulletin of the World Health Organization. 1996;74(2):189–197. [PMC free article] [PubMed] [Google Scholar]
- 15.Central Statistics Office. Gaborone: Central Statistics Office; 2011. Botswana 2011: Population and housing census, Preliminary Results Brief. [Google Scholar]
- 16.MEASURE DHS. Calverton, MD: ICF Macro; 2008. Demographic and Health Surveys: DHS Model Questionnaires. http://www.measuredhs.com/What-We-Do/Survey-Types/DHS-Questionnaires.cfm. Accessed August 20 2012. [Google Scholar]
- 17.Walker CLF, Fontaine O, Young MW, Black RE. Zinc and low osmolarity oral rehydration salts for diarrhoea: a renewed call to action. Bulletin of the World Health Organization. 2009;87(10):780–6. doi: 10.2471/BLT.08.058990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taha AZ. Assessment of mother's knowledge and practice in use of oral rehydration solution for diarrhea in rural Bangladesh. Saudi Medical Journal. 2002;23(8):904–8. [PubMed] [Google Scholar]
- 19.Pahwa S, Kumar GT, Toteja GS. Performance of a Community-based Health and Nutrition-education Intervention in the Management of Diarrhoea in a Slum of Delhi, India. Journal of health population and nutrition. 2010;28(6):553. doi: 10.3329/jhpn.v28i6.6603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ali M, Asefaw T, Byass P, Beyene H, Pedersen FK. Helping northern Ethiopian communities reduce childhood mortality: population-based intervention trial. Bulletin of the World Health Organization. 2005;83(1):27–33. [PMC free article] [PubMed] [Google Scholar]


