Abstract
Background
Studies have demonstrated that physician/pharmacist collaboration can improve management of chronic conditions.
Objective
The purpose of this study was to determine whether a correlation exists between existing clinical pharmacy services within a practice-based research network (PBRN) and provider attitudes and beliefs regarding implementing a new pharmacy intervention based on the Theory of Planned Behavior (TPB).
Methods
A validated survey was completed by one clinical pharmacist from each office. This instrument evaluated the current clinical pharmacy services provided in the medical office. TPB instruments were developed that measured beliefs concerning implementation of a clinical pharmacy intervention for either blood pressure or asthma. The pharmacy services and TPB surveys were then administered to physicians and pharmacists in 32 primary care offices throughout the United States.
Results
Physicians returned 321 (35.9%) surveys, while pharmacists returned 40 (75.5%). The Cronbach’s alpha coefficients generally ranged from 0.65 to 0.98. TPB subscale scores were lower in offices rated with lower pharmacy service scores, but these differences were not statistically significant. There was no correlation between clinical pharmacy service score and providers’ TPB subscale scores. In both the hypertension and asthma groups, pharmacists scores were significantly higher than physicians’ scores on the attitudes subscale in the multivariate analysis (P < 0.001 and P < 0.05, respectively).
Conclusions
Pharmacists consistently scored higher than physicians on the TPB, indicating that they felt the hypertension or asthma intervention would be more straightforward for them to implement than did physicians. There was no significant correlation between clinical pharmacy service scores and attitudes toward implementing a future physician/pharmacist collaborative intervention using the TPB. Future studies should investigate the ability of the TPB instrument to predict implementation of a similar intervention in offices of physicians never exposed to clinical pharmacy services.
Keywords: Physician–pharmacist collaboration, Team-based care, Theory, Theory of planned behavior, Hypertension, Asthma
Introduction
The delivery of primary care is undergoing significant change in an effort to achieve quality improvement and patient-focused care. One approach shown to improve the outcome of chronic conditions is the use of team-based care.1,2 While team-based approaches are now evidence-based, implementation has been uneven within primary care.3-7 A major question about team-based case is whether it will be adopted and scaled up more broadly. There are many barriers to the adoption of team-based care including cost and lack of payment structures. In addition, the lack of positive provider beliefs (or negative beliefs) may create barriers including low levels of trust or role specificity.8,9 As one example of such a barrier, we have found that physicians who work directly with pharmacists in their offices accept 95% of drug therapy recommendations10-12 while recommendations from distant community pharmacists are accepted about 50% of the time.13,14 However, positive provider beliefs and attitudes could partially overcome these barriers, especially when providers work more closely in teams.8,9 Health behavior theory has helped explain a range of provider behaviors and guide implementation of numerous interventions and can be used to help understand changes in health care settings.6,15-18
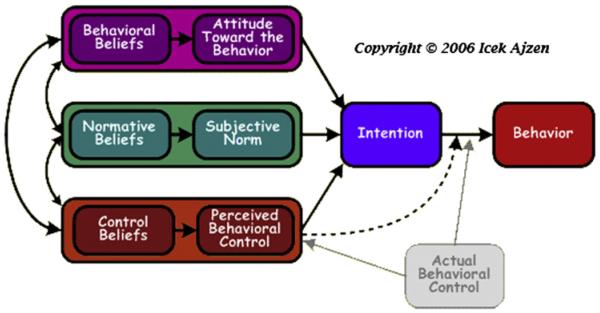
The Theory of Planned Behavior (TPB) has been used to explain physician intentions to perform an activity such as implementation of therapy guidelines.6,17,19,20 Fig. 1 displays the TPB model.20 Behavioral intentions, in turn, are directly influenced by attitudes, subjective social norms, and perceived behavioral control, which are determined by behavioral, normative, and control beliefs, respectively. When attitude and subjective norm are favorable, the provider has greater perceived control and should have a stronger intention to perform the behavior.20 Social norms can be described as a belief regarding whether or not significant peers or groups would approve of the behavior.20 Perceived behavioral control describes the fact that action might not always be under voluntary control due to barriers such as a lack of time or perceived feasibility, thus, restricting the behavior. The TPB has been used primarily to evaluate implementation of evidence-based clinical guidelines for chronic conditions.6,16,17,21 To our knowledge it has not been used to evaluate prospective clinical pharmacy interventions.
Fig. 1.
Theory of planned behavior. Reproduced from Ajzen.20 Note: the web site states: *You may copy and use this diagram for non-commercial purposes. Other uses require permission and payment of a fee.
Quality improvement strategies for management of chronic diseases such as hypertension and asthma may benefit from implementation research driven by theory.22-24 A team-based approach utilizing pharmacists has demonstrated improved blood pressure control.11,12,25-27 While these models have been described for over 30 years, it is not known whether such interventions can be scaled up and implemented more broadly within primary care practices.10,28,29 In fact, the recent move to the patient-centered medical home has resulted in calls for strategies to measure care coordination and care management including by other team members.30 Practice-based research networks (PBRNs) have been established to conduct research in larger numbers of medical offices than traditional research and to include more typical patients from primary care.31 We have conducted prospective interventional studies in hypertension in small networks,12 but there have been no such studies in larger PBRNs. In addition, prior to our ongoing study, the authors are unaware of any PBRNs located in multiple states that have conducted prospective research on hypertension or asthma.
The purpose of the present study was to determine whether provider attitudes and beliefs regarding implementation of a physician/pharmacist collaborative model are related to actual clinical pharmacy services. This is the first study to use theory to predict the implementation of a pharmacy-based intervention within a large number of primary care offices within a national PBRN. We theorized that a supportive culture (intentions) for implementing new pharmacy services would be related to key aspects of the TPB such as attitudes, normative beliefs and perceived control held by both physicians and pharmacists in a given office. The hypothesis was that there would be more favorable scores on the TPB for physicians and pharmacists (intentions) in medical offices with higher pharmacy structure scores (behavior). It also was theorized that pharmacists as a group would have more favorable attitudes to implement the intervention than physicians.
Methods
The practice-based research network
The Collaboration Among Pharmacists and Physicians to Improve Outcomes Now (CAPTION) trial is a cluster-randomized study being conducted in 32 medical offices within the National Interdisciplinary Primary Care PBRN.32 The study was designed to evaluate determinants of implementation of a pharmacy intervention to improve blood pressure or asthma control. Each medical office employs at least one clinical pharmacist who provides patient care and/or physician education within the office. The study was approved by the University of Iowa Institutional Review Board for human subjects research.
Our previous research had revealed a great deal of diversity in the type of pharmacy services provided in these offices.33 The majority of offices (85.4%) were residency training programs. Pharmacists primarily provided management for anti-coagulation (58%), diabetes (54%), hypertension (40%), hyperlipidemia (40%) or asthma (21%). Pharmacists could order laboratory tests in 56% of the offices. However, large components of the pharmacists’ time was spent with resident education about specific patients (11%) or hallway discussions about drug therapy (25%) rather than in direct patient care. To evaluate the level of pharmacy services in each office, one lead clinical pharmacist in the office was surveyed using a previously validated instrument. A copy of the primary questions comprising this instrument is provided in the Appendix A.34 Other instruments used are available from the authors. The pharmacy services instrument measured the frequency and level of clinical pharmacy services and could range from 0 to160. Offices were grouped into “high clinical pharmacy services” (≥114) or “low clinical pharmacy services” (≥114) categories based on previous validations of the instrument.34 For instance, offices in which clinical pharmacists primarily provided “curbside” consultations such as informal discussion in the hallway or general education to physicians would score low compared to sites in which the pharmacist provided extensive direct patient care much of their time in the office (such as managing conditions like diabetes or anticoagulation).
The CAPTION trial is a cluster, randomized trial. First, each medical office was stratified based on this score as well as on the percentage of minority patients (</≥44%). Following stratification, 32 clinics were randomized to either a hypertension intervention or an asthma intervention. The approach led to equal number of offices with high or low pharmacy structure scores or potential minority subjects in each arm of the study. Further details on the background and study design are available elsewhere.32
Development of the TPB instrument
Determinants of behavior theorized to be associated with the implementation of the intervention based on the TPB were evaluated with a 25-item survey that was constructed by two of the investigators (MVW, BLC). The survey was developed using an operations manual for validated instruments for the TPB obtained from experts in the field.6,17 The initial instrument was pilot tested with 16 family physicians and 11 clinical pharmacists who had previously been involved in physician–pharmacist collaborative intervention studies in 6 family medicine offices in Iowa.11,12 The alpha values for the physicians and pharmacists respectively were: attitudes (0.588, 0.670), social norms (0.829, 0.298), perceived behavioral control (0.825, 0.703), and behavioral intentions (0.821, 0.866). The survey items were reduced in an effort to improve psychometric properties (see below) and then utilized in the present study.
The reliability of this instrument was evaluated using Cronbach’s alpha and both redundant items and those determined to be poorly correlated with other items compromising a given subscale were eliminated since the Cronbach’s alpha values suggested that these items did not measure the same underlying construct.35 The final 16-item version of the instrument included nine questions specifically designed to assess attitudes, social norms, and behavioral intentions and two questions that assessed perceived behavioral control. Of the 16 items, 11 could be quantitatively evaluated and scored on a scale from 1 to 7 where 1 was the least positive response and 7 was the most positive response. To improve internal validity, the scale assessing attitudes was inverted, but was reverse scored to be consistent with the other scales. The remainder of the survey was designed to assess the relationship between the physician and pharmacist and collect demographic information. Two free response questions asking about medical reference sources typically used to answer hypertension questions and reasons why a physician–pharmacist collaborative model was not used in the medical office were also included. The final versions of both the hypertension and asthma instruments contained 16 items.
Distribution of the surveys
The CAPTION trial is designed such that the control group offices conducted an asthma intervention. However, these offices enrolled hypertensive subjects into the hypertension control group. Because CAPTION is an implementation trial, these survey instruments will be repeated at the end of the intervention period. The hypertension instrument was administered to physicians and pharmacists in all arms of the study to hopefully explore if there are differences between the control and intervention groups following implementation of the intervention. This provides the ability to test both within group and between group differences in the hypertension instrument scores at the end of the CAPTION trial in 2014. For the asthma instrument there is no control group so that instrument was used to assess the asthma intervention in those offices that subsequently implemented that intervention. For this instrument, there is the ability only to conduct within-group (pre-, post-) differences at the end of the study.
For providers in offices randomized to the hypertension intervention (n = 20 offices), the surveys for physicians and pharmacists focused on a hypertension intervention. Providers in offices randomized to the asthma intervention (n = 12 offices) received a survey that included questions for implementing both an asthma and hypertension intervention. The TPB surveys were mailed to a site study coordinator (nurse or medical assistant) who distributed them to the providers prior to any on-site training related to the project or intervention.
The demographic information collected from the physician and pharmacist respondents included: age, gender, race, ethnicity, academic affiliation, years of residency training, years in practice, medical specialty (physicians only), patient volume, degree, pharmacy residency training (pharmacists only), certifications (pharmacists only), and number of half days per week providing patient or clinical services in the medical office (pharmacists only). They also were asked about Spanish fluency for future information since many of the offices have subjects who only speak Spanish.
Completed surveys were returned to the University of Iowa College of Pharmacy. In order to increase the response rate, reminder emails were sent directly to the providers on two occasions at about 3 weeks apart. Two research assistants double entered data into an online database built and maintained by the Clinical Trials Statistical & Data Management Center at the University of Iowa. Discrepancies were reconciled by one of the research assistants.
Data analysis
The primary objective of this study was to determine if there was a correlation between scores on the pharmacy structure survey and scores on the TPB survey prior to implementation of the study intervention. Survey data were first analyzed using univariate mixed linear models. The use of mixed linear models allowed similar responses at a given site to be accounted for in order to reduce potential bias and the possibility of false positive results. Backward selection was used to determine a best set of predictors to be used in multivariate mixed linear models. The covariates selected included: treatment group (hypertension models only), pharmacy structure score group, gender, provider (physician or pharmacist), academic affiliation (resident or faculty member), and response rate from a given office (high or low). Backward selection and multivariate mixed linear models were used to assess the impact on multiple predictors. Backward selection with a P < 0.20 criterion was used to determine the best set of the predictors within the model. Responses on the TPB attitude subscale were reverse scored to allow for uniform reporting of results.
Results
Surveys were mailed to 938 physicians and 53 pharmacists. A total of 43 physicians who were mailed surveys had left the clinics prior to the surveys being administered and were excluded from the response rate calculations. To the authors’ best knowledge, none of the pharmacists left the clinics during the survey period. Physicians returned 321 (35.9%) surveys, while pharmacists returned 40 (75.5%) surveys.
Demographic information for the survey respondents is summarized in Table 1. There were 22 offices with high clinical pharmacy service scores and 10 with low scores. The mean and standard deviation for these scores were 125.3 ± 8.4 (range 114–143) and 61.0 ± 37.8 (range 11–113), respectively. The majority of physicians were residents or fellows (53.9%).
Table 1.
Physician and pharmacist demographics
| Pharmacist (n = 40) | Physician (n = 321)a | ||
|---|---|---|---|
| Gender | Missing | 2 (5.0%) | 23 (7.3%) |
| Male | 14 (35%) | 143 (45.3%) | |
| Female | 24 (60.0%) | 149 (47.3%) | |
| Ethnicity | Hispanic | 4 (10.0%) | 19 (6.0%) |
| Non-Hispanic | 27(67.5%) | 195 (61.9%) | |
| Declined or missing | 9 (21.5%) | 101 (32%) | |
| Race | Asian | 3 (7.5%) | 28 (8.8%) |
| Black | 1 (2.5%) | 13 (4.1%) | |
| White | 31(77.5%) | 231 (73.3%) | |
| Declined or missing | 5 (12.5%) | 41 (13.0%) | |
| Multiracial or other | 0 | 2 (0.6%) | |
| Academic affiliation | Missing | 2 (5.0%) | 21 (6.6%) |
| Resident of fellow | 5 (12.5%) | 170 (53.9%) | |
| Full-time faculty | 26 (65%) | 104 (33.0%) | |
| Part-time/adjunct faculty | 7 (17.5%) | 12 (3.8%) | |
| Not academically affiliated | 0 | 8 (2.5%) | |
| Number of patients seen per week by physicians |
Missing | NAa | 19 (6.0%) |
| ≤75 | NA | 245 (77.7%) | |
| 76–100 | NA | 40 (12.6%) | |
| 101–125 | NA | 8 (2.5%) | |
| ≥126 | NA | 3 (0.9%) | |
| Pharmacist degree and certificatesb | Pharm.D. degree | 37 (92.5%) | NA |
| Pharm. residency | 16 (40%) | NA | |
| AmCare residency | 13 (32.5%) | NA | |
| Postdoctoral fellowship | 7 (17.5%) | NA | |
| BCPS | 20 (50%) | NA | |
| BCPP | 1 (2.5%) | NA | |
| CDE | 7 (17.5%) | NA | |
| Other | 9 (22.5%) | NA | |
| Physician specialty | Family medicine | NA | 233 (75.2%) |
| Internal medicine | NA | 59 (19.0%) | |
| Geriatrics | NA | 8 (2.5%) | |
| Other | NA | 10 (3.2%) | |
| Age | Mean | 39.5 | 38.4 |
| Standard deviation | 9.3 | 11.6 | |
| Minimum | 25 | 25 | |
| Maximum | 62 | 78 | |
| Years in medical residency | Mean | NA | 2.1 |
| Standard deviation | NA | 1.3 | |
| Minimum | NA | 0 | |
| Maximum | NA | 6 | |
| Years in practice | Mean | 12.3 | 7.3 |
| Standard deviation | 9.9 | 10.9 | |
| Minimum | 0 | 0 | |
| Maximum | 35 | 50 | |
| Number of ½ days per week providing patient or clinical services (pharmacists only) |
Mean | 4.5 | NA |
| Standard deviation | 2.6 | ||
| Minimum | 1 | ||
| Maximum | 10 |
Some of the physicians did not answer some of the questions or refused to answer.
Each pharmacist could have multiple degrees or certifications: PharmD, doctor of pharmacy degree; Pharm. residency, pharmacy practice residency; AmCare residency, ambulatory care specialty residency; Fellow, postdoctoral research fellowship; BCPS, board certified pharmacotherapy specialist; BSPP, board certified psychiatric pharmacy specialists; CDE, certified diabetes educator.
Table 2 displays the Cronbach’s alpha coefficients were calculated to measure the internal consistency of the TPB subscales. These data display the values for pharmacists and physicians for both the blood pressure and asthma/hypertension instruments.
Table 2.
Chronbach’s alpha coefficients for theory of planned behavior physician-pharmacist collaborative subscalesa
| Groupb | Blood pressure intervention |
Asthma/chronic intervention |
||||||
|---|---|---|---|---|---|---|---|---|
| Beh int | Social norms | PBC | Attitudes | Beh int | Social norms | PBC | Attitudes | |
| Pharmacist – BP (n = 26) | 0.678 | 0.579 | 0.440 | 0.914 | – | – | – | – |
| Pharmacist asthma/CC (n = 14) | 0.715 | 0.293 | 1.000c | 0.959 | 0.731 | 0.505 | 0.074 | 0.498 |
| Physician – BP (n = 258) | 0.916 | 0.652 | 0.841 | 0.799 | – | – | – | – |
| Physician – asthma/CC (n = 63) | 0.845 | 0.832 | 0.839 | 0.857 | 0.828 | 0.678 | 0.821 | 0.789 |
There were three questions each for attitudes, social norms, and behavioral intentions and two questions that assessed perceived behavioral control.
Offices were randomized to either hypertension or asthma arms. Beh Int, behavioral intentions; PBC, perceived behavioral control; BP, blood pressure; Asthma/CC, asthma or chronic care intervention.
The determinant of the covariance matrix is zero or approximately zero. Statistics based on its inverse matrix cannot be computed and are displayed as system missing values.
The data in Table 3 display the combined scores for physicians and pharmacists. The data are separated by scores on the pharmacy services instrument (high and low) and by the type of TPB instrument (hypertension versus asthma). As expected, the TPB subscale scores were lower in offices rated as having lower pharmacy service scores but these differences were not statistically significant.
Table 3.
Theory of planned behavior physician–pharmacist collaborative intervention scores by level of clinical pharmacy service scoresa
| Pharmacy services scoresb |
Attitudes |
Social norms |
Perceived behavioral control |
Behavioral intentions |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | Std dev | N | Mean | Std dev | N | Mean | Std dev | N | Mean | Std dev | |
| Blood pressure intervention | ||||||||||||
| High | 234 | 3.62 | 1.7 | 237 | 5.13 | 1.4 | 236 | 5.64 | 1.5 | 236 | 4.90 | 1.8 |
| Low | 116 | 3.61 | 1.6 | 116 | 5.05 | 1.3 | 114 | 5.43 | 1.7 | 115 | 4.61 | 1.8 |
| Asthma/chronic care intervention | ||||||||||||
| High | 52 | 4.88 | 1.5 | 52 | 5.17 | 1.4 | 52 | 5.46 | 1.6 | 52 | 5.09 | 1.6 |
| Low | 22 | 4.70 | 1.6 | 22 | 4.82 | 1.4 | 22 | 4.86 | 2.0 | 22 | 4.61 | 1.6 |
All P values for differences between offices with high and low pharmacy services scores were between 0.15 and 0.98.
Includes physicians and pharmacists combined. There were three questions each for attitudes, social norms, and behavioral intentions and two questions that assessed perceived behavioral control.
Offices were divided into high or low pharmacy structure scores.
In the univariate models, pharmacists answering the hypertension TPB instrument scored significantly higher than their physician colleagues on the TPB subscales (Table 4, P < 0.0001). In the multivariate models, when controlling for the other covariates pharmacists scored significantly higher than physicians (P < 0.0001). In the asthma group, the multivariate model was unable to be fit for the attitude subscale. In this case, multivariate mixed models estimate the effect of covariates on the outcome as well as estimating correlation within site. Since the sample size was small relative to the number of covariates there was not enough information to also estimate the correlation parameter.
Table 4.
Theory of planned behavior collaborative intervention scores for pharmacists and physicians
| Provider | Attitudes |
Social norms |
Perceived behavioral control |
Behavioral intentions |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | Std dev |
Univ./mult. P–value |
N | Mean | Std dev |
Univ./multi. P–value |
N | Mean | Std dev |
Univ./multi. P–value |
N | Mean | Std dev |
Univ./multi. P–value |
|
| Blood pressure | ||||||||||||||||
| Pharmacist | 40 | 5.43 | 1.6 | <0.0001/<0.0001a | 40 | 6.38 | 0.6 | <0.0001/<0.0001b | 40 | 6.79 | 0.4 | <0.0001/<0.0001b | 39 | 6.09 | 1.1 | <0.0001/<0.0001c |
| Physician | 310 | 3.38 | 1.5 | 313 | 4.94 | 1.3 | 310 | 5.41 | 1.6 | 312 | 4.65 | 1.8 | ||||
| Asthma | ||||||||||||||||
| Pharmacist | 13 | 6.49 | 0.6 | <0.0001/NA | 13 | 6.31 | 0.6 | 0.0001/<0.0001d | 13 | 6.38 | 0.4 | 0.02/0.02e | 13 | 5.41 | 1.5 | 0.36/NSf |
| Physician | 61 | 4.48 | 1.4 | 61 | 4.80 | 1.4 | 61 | 5.05 | 1.8 | 61 | 4.85 | 1.6 | ||||
NA, model was unable to be fit; Univ., univariate; Mult., multivariate; NS, nonsignificant. P > 0.2.
Covariables adjusted for included treatment group, gender, response rate, and provider.
Adjusted for treatment group, gender, response rate, interaction treatment by gender, interaction treatment by response rate, and provider.
Covariables adjusted for included treatment group, gender, and provider.
Covariables adjusted for included academic affiliation and provider.
Covariables adjusted for included provider only.
Covariables adjusted for included academic affiliation only.
The univariate analysis on the asthma group demonstrated significantly higher pharmacist scores in the attitude subscale. Pharmacists scored significantly higher than physicians in both the social norms (P < 0.0001) and the perceived behavioral control (P = 0.02) subscales for univariate as well as multivariate models. The model did not include an interaction term between gender separately for physicians and pharmacists because there was insufficient power to test large numbers of predictors. Therefore, when physicians and pharmacists were combined, females scored significantly higher than males for the attitudes and intentions subscales in the hypertension group in multivariate models (P < 0.04, data not shown).
Contrary to the study hypotheses, no correlation was found between clinical pharmacy service scores and providers’ TPB subscale scores in either the hypertension or asthma/hypertension groups.
Discussion
This study found that both physicians and pharmacists held positive attitudes about implementing a physician/pharmacist collaborative intervention. Providers in offices with little or no experience with the proposed intervention in their office also held moderately positive attitudes. Pharmacists scored significantly higher suggesting the pharmacists felt the interventions would be more straightforward to implement than their physician colleagues.
It was expected to find that TPB subscale scores for attitudes, social norms, perceived behavioral control, and behavioral intentions for both types of providers would correlate with the level of clinical pharmacy services as a measure of actual behavior (Fig. 1). This hypothesis was based on the idea that providers having more positive intentions about implementation of a physician/pharmacist collaborative intervention for hypertension or asthma management would result in actual positive behaviors or higher levels of pharmacy services as measured by the pharmacy structure scores. Sufficient support from physicians and agreement by pharmacists should have led to a greater scope and breadth of pharmacy services (Appendix A). However, there was no significant correlation between TPB subscale scores and greater levels of clinical pharmacy services suggesting that 1) provider beliefs, intentions or perceived ability did not influence the existing level of pharmacy, or 2) that existing pharmacy services were viewed positively resulting in a ceiling effect for the TPB that limited our ability to observe significant correlations. The high physician scores on the TPB survey suggest that physicians were not opposed to the implementation of a pharmacy intervention. Future studies should survey offices that lack pharmacy services, which may have greater diversity of opinion and ability to predict new pharmacy services.
It is also possible that the instruments lacked validity or that there was measurement error. The instrument used to evaluate the level of pharmacy services was validated in Veterans Affairs ambulatory care clinics.34 However, the questions were designed to measure clinical pharmacy services in any ambulatory care practice (Appendix A) so the instrument should also be valid in the CAPTION study offices.
Another possible explanation for the lack of a correlation is a social desirability bias. In this case, providers may have responded in the manner that they thought was more desired or acceptable, even if it was not entirely consistent with their personal attitudes and preferences.
Pharmacists scored significantly higher than physicians across all four TPB subscales in the hypertension intervention and on several subscales for the asthma intervention (the latter for univariate models only). These findings suggest that pharmacists either were more accepting and willing to initiate a new pharmacy intervention, or they believed it would be more straightforward to implement a new program than did their physician counterparts. Alternatively, these findings might suggest that pharmacists are more willing to participate directly in patient-care than physicians are willing to delegate responsibility. Formative evaluations will be conducted at the end of the CAPTION study (2014) to explore these possibilities.
Because many of the participating offices are residency training programs, the majority of physicians were recent graduates from medical school (<5 years). It is likely that recent graduates have been exposed to interdisciplinary care involving a pharmacist during their medical education or residency training. Physicians who graduated many years ago might not have had the same experiences and might be less willing to delegate clinical responsibilities to a pharmacist. In addition, more experienced physicians might not have as favorable views of a pharmacy intervention. This notion is supported by a study that surveyed physicians and found that more recent graduates from medical school had higher current and future expectations of pharmacists than physicians with a greater number of years since graduation.36
The Cronbach’s alpha values generally support the internal consistency of the subscales. The values for the physician group were promising, with nearly all exceeding 0.7 (Table 2). A Cronbach’s alpha above 0.7 strongly suggests that the individual items comprising a subscale do in fact measure a single unitary construct.35 However, a limitation of the present study was several Cronbach’s alpha scores below 0.7 or 0.65 as recommended by some.37 All of these low alpha’s were observed in the smaller number of control offices that implemented the asthma intervention. Thus, these low subscale scores likely resulted from small sample size. The pharmacists’ surveys, however, had variable findings, with reliability coefficients for some subscales falling below this threshold. These results could have been affected by the small sample of available pharmacists. The alpha coefficients for the attitudes questions were 0.914 for the pharmacists responding to the blood pressure intervention only, and 0.959 and 0.498 for pharmacists responding to implementing a blood pressure or asthma intervention, respectively.
Females scored significantly higher than males for the attitudes and intentions subscales in the hypertension group. We are unable to speculate why females would have higher scores for implementation of the intervention than male providers.
This study has several limitations. This study was conducted in offices with clinical pharmacists so the findings can only be generalized to similar medical clinics. As with most surveys, the findings could be influenced by response bias indicating that those who returned the survey were more in favor of the intervention. Such a bias may have been more likely in the physician group where response rate was lower. However, the physician response rate of 36% is similar to other survey studies (29–39%).8,38 The pharmacists’ response rate of 76% improves the ability to evaluate the instruments in these providers. Surveys were distributed to 45 pharmacists, or an average of 1.67 clinical pharmacists per office. In contrast, the offices included an average of 30.7 physicians. There are fewer pharmacists in each primary care medical office since it is uncommon for a given medical office to employ more than one or two clinical pharmacists. Another limitation is the majority of physicians surveyed were residents. The sample we surveyed may have different views from a sample of more experienced physicians. Finally, most clinics were affiliated with academic medical centers, which may have influenced the findings and reduced the generalizability of the results.
Conclusion
Clinical pharmacists practicing in medical offices within a PBRN consistently scored higher on the TPB. These findings suggest that pharmacists perceived fewer barriers to implementation of the intervention than did physicians. However, both physicians and pharmacists held positive attitudes about implementing a new pharmacist-based intervention. There was no significant correlation between clinical pharmacy service scores and attitudes toward implementing a physician/pharmacist collaborative intervention using measures based on the TPB. The TPB instrument will be used at the end of the study (2014) to determine if it can predict the successful implementation of the intervention in an ongoing cluster, randomized implementation trial.
Acknowledgments
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs. All of the authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
The authors would like to acknowledge the assistance and support of the study coordinators, pharmacists and physicians from all of the CAPTION trial medical offices. Fourth & Lewis Medical Office Family Medicine, San Diego, CA; Scripps Ranch Medical Office Family Medicine, San Diego, CA; Family Medicine Center at Asylum Hill, Hartford, CT; University of Florida Family Practice Medical Group, Gainesville, FL; University of South Florida, Department of Family Medicine, Tampa, FL; Genesis Family Medical Center, Davenport, IA; Broadlawns Family Health Center, Des Moines, IA; Northeast Iowa Family Practice Center, Waterloo, IA; Pocatello Family Medicine Clinic at Portneuf Medical Center, Pocatello, ID; University Family Medicine Residency Program, Malden, MA; Jefferson Family Medicine Clinic, Buffalo, NY University of North Carolina Enhanced Care Clinic, Chapel Hill, NC; Duke University Medical Center, Durham, NC; Wake Forest University Baptist Medical Center, Northwest Area Health Education Center, Winston Salem, NC; University of Pittsburgh Medical Center, St. Margaret Family Medicine Residency Program, Pittsburgh, PA; Medical University of South Carolina, Department of Family Medicine Clinic, Charleston, SC; Trident Family Medicine Residency Program, Charleston, SC; Spartanburg Family Medicine Residency Program, Spartanburg, SC; Texas Tech Center for Community and Family Medicine, Amarillo, TX; Blackstock Family Practice, Austin, TX; Texas Tech Community Partnership Clinics, El Paso, TX; University of Texas, Centro San Vicente, Alameda Clinic, El Paso, TX; Memorial Family Medicine Residency Program, Sugar Land, TX; University of Texas Health Science Center at San Antonio, San Antonio, TX; Northeast Family Practice Pharmacy, Madison, WI; Wingra Family Medical Center, Madison, WI; Wheaton Franciscan Medical Group Wisconsin Avenue, Racine, WI.
The research team would also like to offer special thanks to Jeremy Grimshaw, MBChB, PhD, for providing materials to aid in the development of the TPB-based surveys.
Funding: supported by the National Heart, Lung, and Blood Institute, RO1 HL091841 and HL091843. Drs. Carter and Vander Weg are also supported by the Comprehensive Access and Delivery Research and Evaluation (CADRE), Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (HFP 04-149).
Appendix A
Pharmacy structure survey questions
For all remaining questions, consider all of your patients. Consider all the patients you saw in the last 6 weeks.
Use the following scale:
0 = never; 1 ≤ 25% of the time; 2 = 25–50% of the time; 3 = 51–75% of the time; 4 = 75–95% of the time; 5 = always.
-
1
Considering all the patients that you saw in the last 6 weeks, how often did you use informational services (e.g., personal reference library, online searching service, or subscription to drug information service) to assist in your practice when necessary?
Record-screening
-
2
Requested patients’ medical records from physicians and then reviewed them for drug-related problems.
-
3
Checked the patient’s medication profile for potential drug-related problems.
Patient assessment
In general, considering all the patients with chronic conditions that you saw in the last 6 weeks, please indicate the extent to which you performed the following activities by circling the appropriate response.
-
4
Asked the patient to describe his or her medical condition, including a description of medical problems and symptomatology.
-
5
Asked the patient what he or she wanted to achieve from the drug therapy.
-
6
Asked the patient questions to assess actual patterns of use of the medication.
-
7
Asked the patient questions to find out if he or she might be experiencing drug-related problems.
-
8
Asked the patient questions to find out about the perceived effectiveness of drugs he or she was taking.
-
9
Asked the patient questions to evaluate whether the therapeutic objective(s) was (were) being met.
-
10
Composed a complete problem list for the patient.
-
11
Performed physical assessment.
-
12
Personally ordered a laboratory test.
-
13Are you authorized to order laboratory tests?
- No
- Yes, under protocol
- Yes, not restricted by a protocol
Implementation of objectives/monitoring plan
-
14Do you have a formal collaborative practice agreement with any physicians?
- Yes
- No
Considering all the patients with chronic conditions that you saw in the last 6 weeks, please indicate how frequently you provided the following services:
-
15
Implemented a strategy to resolve (or prevent) the drug-related problem(s).
-
16
Established follow-up plans to evaluate the patient’s progress toward his or her drug therapy objectives.
-
17
Carried out the follow-up plans established for the patient’s progress toward his or her drug therapy.
Counseling/instruction
-
18
Instructed the patient on his/her drug therapy.
Referral and consultation
-
19
Made referrals to a physician or another provider when necessary.
-
20
Communicated patients’ progress on their drug therapy to their primary care provider verbally.
-
21
Communicated patients’ progress on their drug therapy to their primary care provider via a written note (not in the medical record).
-
22
Communicated patients’ progress on their drug therapy to their primary care provider via the medical record.
-
23
Initiated discussion with the primary care provider whenever you believed a patient was experiencing a drug-related problem or might experience a drug-related problem.
-
24
Provided the primary care provider (upon referral) a written summary of the patient’s medication history and any drug-related problems.
-
25
Adjusted doses of medications as needed.
-
26
Added a new medication as needed.
-
27
Deleted an old medication.
Verification of patient understanding
-
28
How often do you verify that a patient understood the information you presented to him or her?
Documentation
-
29Where are pharmacist activities documented? (circle all that apply)
- Electronic medical record
- Paper chart
- Other
- None
In general, considering all the patients with chronic conditions that you saw in the last 6 weeks, please indicate the extent to which you performed the following activities by circling the appropriate response.
-
30
Documented information about the patient’s medical conditions on written records or computerized notes or by other formal mechanisms in a form that could be read and interpreted by another health care practitioner in your absence.
-
31
Documented all medications currently being taken by the patient on written records or computerized notes or by other formal mechanisms in a form that could be read and interpreted by another health care practitioner in your absence.
-
32
Documented the desired therapeutic objectives for the patient.
Now think about any patients you’ve cared for in the last 6 weeks who you discovered were experiencing drug-related problems. Please indicate how often you provided the following activities by circling the appropriate response.
-
33
Documented the drug-related problems, potential or actual, on written notes.
-
34
Documented the desired therapeutic objective(s) for each of the drug-related problems identified.
-
35
Documented any intervention made on the patient’s file, prescription, report, or medical order in a form that could be read and interpreted by another health care professional.
Modified from instrument used in the IMPROVE (Impact of Managed Pharmaceutical Care on Resource Utilization and Outcomes in Veterans Affairs Medical Centers) study, Barry L. Carter, Principal Investigator, “Assessing the structure and process for providing pharmaceutical care in Veterans Affairs medical centers.” Am J Health-Syst Pharm 2000;57:29–39.
Footnotes
Conflict of interest: The authors have no conflicts of interest, including specific financial interests, and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript.
Trial Registration: clinicaltrials.gov Identifier: NCT00935077.
References
- 1.Chisholm-Burns MA, Kim Lee J, Spivey CA, et al. US pharmacists’ effect as team members on patient care: systematic review and meta-analyses. Med Care. 2010;48:923–933. doi: 10.1097/MLR.0b013e3181e57962. [DOI] [PubMed] [Google Scholar]
- 2.Carter BL, Bosworth HB, Green BB. The hypertension team: the role of the pharmacist, nurse, and teamwork in hypertension therapy. J Clin Hypertens (Greenwich) 2012 Jan;14:51–65. doi: 10.1111/j.1751-7176.2011.00542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eccles MP, Grimshaw JM. Selecting, presenting and delivering clinical guidelines: are there any “magic bullets”? Med J Aust. 2004;180(suppl 6):S52–S54. doi: 10.5694/j.1326-5377.2004.tb05946.x. [DOI] [PubMed] [Google Scholar]
- 4.Grimshaw JM, Eccles MP. Is evidence-based implementation of evidence-based care possible? Med J Aust. 2004;180(suppl 6):S50–S51. doi: 10.5694/j.1326-5377.2004.tb05945.x. [DOI] [PubMed] [Google Scholar]
- 5.Grimshaw JM, Thomas RE, MacLennan G, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8:1–72. doi: 10.3310/hta8060. [DOI] [PubMed] [Google Scholar]
- 6.Grimshaw JM, Zwarenstein M, Tetroe JM, et al. Looking inside the black box: a theory-based process evaluation alongside a randomised controlled trial of printed educational materials (the Ontario printed educational message, OPEM) to improve referral and prescribing practices in primary care in Ontario, Canada. Implement Sci. 2007;2:38. doi: 10.1186/1748-5908-2-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grol R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care. 2001;39(8 suppl 2):46–54. doi: 10.1097/00005650-200108002-00003. [DOI] [PubMed] [Google Scholar]
- 8.Zillich AJ, Doucette WR, Carter BL, Kreiter CD. Development and initial validation of an instrument to measure physician-pharmacist collaboration from the physician perspective. Value Health. 2005;8:59–66. doi: 10.1111/j.1524-4733.2005.03093.x. [DOI] [PubMed] [Google Scholar]
- 9.Zillich AJ, McDonough RP, Carter BL, Doucette WR. Influential characteristics of physician/pharmacist collaborative relationships. Ann Pharmacother. 2004;38:764–770. doi: 10.1345/aph.1D419. [DOI] [PubMed] [Google Scholar]
- 10.Carter BL, Helling DK, Jones ME, Moessner H, Waterbury CA., Jr. Evaluation of family physician prescribing: influence of the clinical pharmacist. Drug Intell Clin Pharm. 1984;18:817–821. doi: 10.1177/106002808401801010. [DOI] [PubMed] [Google Scholar]
- 11.Carter BL, Bergus GR, Dawson JD, et al. A cluster randomized trial to evaluate physician/pharmacist collaboration to improve blood pressure control. J Clin Hypertens. 2008;10:260–271. doi: 10.1111/j.1751-7176.2008.07434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carter BL, Ardery G, Dawson JD, et al. Physician and pharmacist collaboration to improve blood pressure control. Arch Intern Med. 2009;169:1996–2002. doi: 10.1001/archinternmed.2009.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chrischilles EA, Carter BL, Lund BC, et al. Evaluation of the Iowa Medicaid pharmaceutical case management program. J Am Pharm Assoc. 2004;44:337–349. doi: 10.1331/154434504323063977. [DOI] [PubMed] [Google Scholar]
- 14.Park JJ, Kelly P, Carter BL, Burgess PP. Comprehensive pharmaceutical care in the chain (pharmacy) setting. J Am Pharm Assoc. 1996;NS36:443–451. doi: 10.1016/s1086-5802(16)30099-7. [DOI] [PubMed] [Google Scholar]
- 15.Designing theoretically-informed implementation interventions. Implement Sci. 2006;1:4. doi: 10.1186/1748-5908-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McKenzie JE, French SD, O’Connor DA, et al. IMPLEmenting a clinical practice guideline for acute low back pain evidence-based manageMENT in general practice (IMPLEMENT): cluster randomised controlled trial study protocol. Implement Sci. 2008;3:11. doi: 10.1186/1748-5908-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Francis JJ, Grimshaw JM, Zwarenstein M, et al. Testing a TheoRY-inspired MEssage (TRY-ME): a sub-trial within the Ontario Printed Educational Message (OPEM) trial. Implement Sci. 2007;2:39. doi: 10.1186/1748-5908-2-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davies P, Walker AE, Grimshaw JM. A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluations. Implement Sci. 2010;5:14. doi: 10.1186/1748-5908-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Armitage CJ, Conner M. Efficacy of the theory of planned behaviour: a meta-analytic review. Br J Soc Psychol. 2001;40(Pt 4):471–499. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 20.Ajzen I. [Accessed 09.01.13];Behavioral Interventions Based on the Theory of Planned Behavior. http://people.umass.edu/aizen/tpb.html.
- 21.Ceccato NE, Ferris LE, Manuel D, Grimshaw JM. Adopting health behavior change theory throughout the clinical practice guideline process. J Contin Educ Health Prof. 2007;27:201–207. doi: 10.1002/chp.138. [DOI] [PubMed] [Google Scholar]
- 22.Keenan NL, Shaw KM. Coronary heart disease and stroke deaths – United States, 2006. MMWR Surveill Summ. 2011;60(suppl):62–66. [PubMed] [Google Scholar]
- 23.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 24.Walsh JM, McDonald KM, Shojania KG, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006;44:646–657. doi: 10.1097/01.mlr.0000220260.30768.32. [DOI] [PubMed] [Google Scholar]
- 25.McKenney JM, Slining JM, Henderson HR, Devins D, Barr M. The effect of clinical pharmacy services on patients with essential hypertension. Circulation. 1973;48:1104–1111. doi: 10.1161/01.cir.48.5.1104. [DOI] [PubMed] [Google Scholar]
- 26.Carter BL, Rogers M, Daly J, Zheng S, James PA. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med. 2009;169:1748–1755. doi: 10.1001/archinternmed.2009.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zillich AJ, Sutherland JM, Kumbera PA, Carter BL. Hypertension outcomes through blood pressure monitoring and evaluation by pharmacists (HOME study) J Gen Intern Med. 2005;20:1091–1096. doi: 10.1111/j.1525-1497.2005.0226.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carter BL. Pharmacotherapy and the primary care physician. Prim Care. 1990;17:469–477. [PubMed] [Google Scholar]
- 29.Dickerson LM, Denham AM, Lynch T. The state of clinical pharmacy practice in family practice residency programs. Fam Med. 2002;34:653–657. [PubMed] [Google Scholar]
- 30.Stange KC, Nutting PA, Miller WL, et al. Defining and measuring the patient-centered medical home. J Gen Intern Med. 2010;25:601–612. doi: 10.1007/s11606-010-1291-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fagnan LJ, Handley MA, Rollins N, Mold J. Voices from left of the dial: reflections of practice-based researchers. J Am Board Fam Med. 2010 Jul-Aug;23:442–451. doi: 10.3122/jabfm.2010.04.090189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carter BL, Clarke W, Ardery G, et al. A cluster-randomized effectiveness trial of a physician-pharmacist collaborative model to improve blood pressure control. Circ Cardiovasc Qual Outcomes. 2010;3:418–423. doi: 10.1161/CIRCOUTCOMES.109.908038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dickerson LM, Kraus C, Kuo GM, et al. Formation of a primary care pharmacist practice-based research network. Am J Health Syst Pharm. 2007;64(19):2044–2049. doi: 10.2146/ajhp060650. [DOI] [PubMed] [Google Scholar]
- 34.Billups SJ, Okano G, Malone D, et al. Assessing the structure and process for providing pharmaceutical care in Veterans Affairs medical centers. Am J Health Syst Pharm. 2000;57:29–39. doi: 10.1093/ajhp/57.1.29. [DOI] [PubMed] [Google Scholar]
- 35.Bland JM, Altman DG. Cronbach’s alpha. BMJ. 1997;314:572. doi: 10.1136/bmj.314.7080.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith WE, Ray MD, Shannon DM. Physicians’ expectations of pharmacists. Am J Health Syst Pharm. 2002;59:50–57. doi: 10.1093/ajhp/59.1.50. [DOI] [PubMed] [Google Scholar]
- 37.Nunnally JC. Psychometric Theory. 2nd ed. McGraw-Hill Inc; New York: 1978. [Google Scholar]
- 38.Levy BT, Joshi M, Xu Y, Daly J, James PA. Perceptions of Iowa family physicians regarding colorectal cancer screening. Med Care. 2008;46(9 suppl 1):S103–S108. doi: 10.1097/MLR.0b013e31817c6100. [DOI] [PubMed] [Google Scholar]