Abstract
Depression is common among people living with HIV/AIDS in sub-Saharan Africa. Yet, little is known about how depression influences physical health and socioeconomic well-being in the context of antiretroviral therapy (ART). Semi-structured interviews with 40 adult HIV clients receiving ART in Uganda were conducted to assess experiences prior to and after HIV diagnosis and initiation of ART. Content analysis revealed themes that were suggestive of the following patterns: 1) functioning decreased after patients were diagnosed with HIV, but improved following ART, 2) depression is associated with lower physical health functioning and work status levels after both HIV diagnosis and ART, and 3) antidepressant medication is associated with better functioning compared to depressed patients not receiving depression treatment. These findings suggest that depression plays a role in the deleterious effects of HIV on functioning, and that antidepressant treatment provided alongside ART may serve to help individuals regain functioning, particularly employment. These findings highlight the potential value of integrating depression treatment into HIV care.
Keywords: depression treatment, work functioning, antiretroviral treatment, HIV
INTRODUCTION
With over 22 million or two-thirds of the world’s HIV-infected population residing in Sub-Saharan Africa,1 including nearly 1 million in Uganda, and some countries in the region having HIV prevalence rates approaching 20%, the AIDS epidemic has the potential to devastate the social and economic infrastructure of the region. In response to the epidemic, the Uganda AIDS Commission developed a National Strategic Plan for HIV/AIDS to achieve universal access targets for HIV/AIDS prevention, care, treatment and social support and protection by 2015. The National Strategic Plan aims to (a) reduce HIV incidence by 30%, (b) to improve the quality of life of persons living with HIV/AIDS (PLHA) by mitigating the health effects of HIV/AIDS, (c) to improve the level of access of services for PLHA, and (d) to build an effective and efficient system that ensures quality, equitable and timely service delivery. The AIDS Commission plans to increase access to HIV antiretroviral (ART) from 50% to 80% for children and adults with HIV by 2015.2
With the growing momentum of ART scale-up in Uganda specifically and sub-Saharan Africa generally, a better understanding of the effects of ART on economic health is needed to inform evaluations of the cost-effectiveness of ART scale-up and policy decision making for optimizing the effects of ART. Only recently have studies begun to examine whether ART can reverse the negative economic effects of HIV at the level of the individual patient. A recent review of studies conducted in developing countries found promising results, showing that within the first three to six months of treatment, ART is associated with restoration of work productivity and absenteeism to average levels among those who are employed.3 However, in a small qualitative study of ART clients in Uganda, we found that while many were able to return to work with the help of ART and its associated improvement in physical health,4 most were not able to return to work at the same level or intensity as before HIV. These findings suggest that while ART helps people to regain a capacity to work, these gains may be limited, and that other factors are also operating to influence whether or not individuals are able to reestablish their livelihoods.
One factor that may help to explain the relationship between HIV treatment, physical health and work functioning is the psychological well-being of PLHA. Depressive symptoms such as loss of interest and motivation, depressed mood, fatigue, difficulty sleeping and poor concentration can all impede daily functioning and capacity to work. Among PLHA, studies conducted in sub-Saharan Africa have found rates of clinical depression ranging from 8-30%,5,6,7 and rates of elevated depressive symptoms ranging from 30-50%, including in Uganda.8,9 Furthermore, depression is known to decrease adherence to ART and consequently clinical outcomes as well as quality of life.10-13
To maximize the downstream benefits of ART scale-up in sub-Sahara Africa, it is imperative that we understand how depression and mental health treatment interact with HIV treatment to impact socioeconomic outcomes. In our prospective cohort study of HIV clients entering HIV care, patients who were depressed at baseline were half as likely to be working at baseline,14 baseline depression predicted work status one year later, and depression mediated the effects of ART such that those who remained depressed were less likely to gain from HIV treatment with regard to work functioning.15 It is reasonable to hypothesize that depression treatment could enhance the benefits of HIV treatment on socioeconomic outcomes including work functioning. Antidepressants have proven to effectively treat depression in PLHA in the Western world,16,17 and there are some data to suggest that antidepressants and other conventional depression treatments are equally effective in Africa,18 but such studies are few. Qualitative studies are also needed to describe the lived experience of patients with depression and HIV and how ART and depression treatment impact their daily functioning and work activity.
This study builds on our previous work examining the effects of ART treatment on work functioning by exploring the role of depression on work functioning in the context of HIV disease, and how treatment of depression may impact on physical and work functioning for those receiving ART. We conducted semi-structured qualitative interviews with clients attending an HIV clinic in Uganda to explore the impact of HIV and ART on trajectories of work activity across those who were depressed and not depressed. Among those who were depressed, we compared testimonials regarding impact of treatment on their physical and work functioning for those who received antidepressant medication with those that did not receive antidepressants.
METHODS
Sample
In this case study design, participants represented a convenience sample as all were identified and informed of the study by the clinic psychiatrist or other clinic staff member. All adult (age 18 and over) clients who had been on ART for at least 6 months were eligible. In addition, clients who had been diagnosed with Major Depression were purposively selected. Clients who expressed interest in participating were referred to the study interviewer for written consent procedures. Participants were paid 10,000 Uganda Shillings ($5 USD) to compensate for transportation costs. Nearly all clients who were informed of the study agreed to participate. The study protocol was reviewed and approved by the Institutional Review Boards at both Mildmay and RAND.
We interviewed 40 adult HIV clients receiving ART at Mildmay Center, an HIV primary care clinic just outside Kampala, Uganda in Spring 2009. All participants were currently on ART and had been on treatment for at least 6 months and up to several years; mean time on ART was 33 months and average length of time since HIV diagnosis was 52 months. Participants had wide range of CD4 counts from 11 to 604 cells/cu.mm, with an average count of 204 (SD=147); 69% had counts of 250 or less. Diagnosis of depression was provided by the clinic psychiatrist and abstracted from the clinic chart. Among the 26 depressed patients, with 16 diagnosed after they became HIV positive (pre-ART) and the remaining 10 after they started on ART (post-ART). Eleven were treated with antidepressants, while the other 15 had not yet received depression treatment. Most (n=27) participants were female, which is consistent with the representation of women at ART clinics in Sub-Saharan Africa; half (n=21) were under the age of 40. Fifteen (38%) participants currently had a spouse, while 10 (25%) were single, 9 (23%) were widowed, 3 (8%) were divorced, 3 indicated other; all but one had children living in the household. The sample was relatively well educated; over a quarter received some post-secondary education (n= 11), and half had some secondary education (n=21), while the remaining had primary (n=4) or no education (n=4).
Instrument
Using a grounded approach, semi-structured interviews were conducted to learn how clients experienced changes in their physical health and work status over time in the context of HIV infection and starting ART, as well as the influence of depression and antidepressant therapy (for those who had received such treatment). Unlike traditional ethnography, semi-structured interviews are designed to allow for open-ended elicitation of ideas and experiences while simultaneously allowing for comparisons across interviewees. In this study, we used the interviews to elicit the range of experiences related to physical health and work functioning as well as indicate how common or salient these experiences are within and across different types of groupings (e.g., depressed versus nondepressed). To accomplish these aims, a semi-structured interview guide was developed. To ensure that we did not influence the responses, the interview began with the respondent being asked to describe how their life had changed from before they were HIV-infected to now, in as much detail as possible. After this “grand tour” question, we used a topic-by-stage framework to probe for more specifics. To obtain comparative data, we asked each participant to describe their experience with regard to changes in physical health and functioning, and work. This discussion was divided into three stages or time periods: (a) pre-HIV -- the period prior to noticing any symptoms related to HIV or testing HIV-positive; (b) pre-ART-- the period between onset of HIV and starting ART; and (c) post-ART – the period from 6 months of being on ART to the time of the interview.
Interviews were conducted in the native language of the participant, which was typically Luganda, though some preferred to be interviewed in English. All interviews were conducted by a psychologist, who is a native Ugandan, and who received training in qualitative interviewing (including mock interviews and role playing) from Drs. Ryan and Wagner. All participants agreed to allow the interview to be audio-recorded.
Analysis
Interviews were translated into English and transcribed verbatim. To identify themes, we utilized a staged technique described by Ryan and Bernard (2000).19 First, we used text management software (ATLAS.ti) to mark contiguous blocks of transcript text that pertained to the major topical domains of interest (physical health, work activity, depression), and the three time periods (pre-HIV, pre-ART, post-ART). Four of the authors then pulled out all text associated with a particular domain (e.g., physical functioning, work functioning, depression) and after printing the quotes on slips of paper, sorted the quotes into piles based on their thematic similarities across experiences reported. In the next step, a two-person team coded the level of functioning (e.g., fully functioning, partially functioning, not functioning, etc), and themes related to effects of ART and antidepressants, which were defined and categorized in an explicit codebook to guide analyses. We tabulated counts for these themes, examined their distribution across the time periods, and made comparisons of physical and work functioning by depression and medication status to identify patterns. However, statistical tests were not used due to small sample size. Qualitative data from the interview transcripts were used to illustrate the lived experience of participants and provide context for these findings. The complementary use of quantitative and qualitative methods provides a systematic triangulated approach to gathering information about the relationships being explored,19 and guidance to more rigorous quantitative evaluation in the next phase of our research.
RESULTS
Impact of HIV and ART on physical functioning
One important way in which HIV may impact work functioning is through its potential debilitating effect on the physical strength of the infected individual. Participants most often referenced the lack of strength or weakness (n=16; 40%) and pains/aches (n=8, 20%) as common and most debilitating symptoms following infection. Many cited not being able to move or walk, while some were even immobile or bedridden. Other symptoms included fatigue, fevers, coughing, low appetite, dizziness, and bedsores. Prior to HIV infection, nearly all participants described minimal signs of being physically impaired (32 reported being fully functioning, 6 reported partial functioning); however, after HIV diagnosis, all showed significant decline, with 26 (65%) categorized as partial functioning (i.e., able to physically move about, but still living with physical symptoms) and 11 (28%) considered to have significantly impaired physical functioning, which included being bedridden or immobile. It was common for respondents to describe the devastating impact of HIV, particularly when complicated by other illnesses or medical problems resulting from HIV infection. For example, a 39 year old woman, who suffered a miscarriage and had Tuberculosis, described the severe debilitation and hopelessness she experienced as a result of her infection.
Case P8: “I fell sick to the point of death and I was not able to move or work. My life has greatly changed because I was so sick that I would have been buried in 2006. I was going to die…And so people started saying that I was not going to survive because I had slim chance (of recovery from HIV/AIDS). With every passing day they thought that I would not make it to the next day….By then my feet were swollen. But my abdomen was also swollen so she took me to a hospital in Kiboga and they told her that I had retained fluids. I was not even able to turn….I was bedridden.”
After having been on ART for several months, respondents spoke of diminished HIV symptoms. Specifically, they expressed decreased pain, fever, and cough, as well as renewed “strength” and improved appetite. However, when looking at their overall physical functioning after ART, the health improvements are less robust than they are at the symptom level. Approximately half of the participants improved and half maintained a similar level of overall physical functioning as was present before ART.
Although trends of physical functioning across the HIV and ART time periods do show improvement, participants do not necessarily return to the health status they were once at prior to HIV. Prior to HIV infection, 32 (82%) respondents described that they were fully functional, while only three (8%) reported being fully functional between the time of infection and ART. After HIV infection, the vast majority showed significant decline, with 26 (65%) describing significant physical problems, and 11 (28%) not functioning at all. After ART, only 12 (31%) respondents were fully functioning in terms of physical health; most were partially functioning 23 (59%), and four continued to be immobile. These results suggest that although most improved somewhat, participants did not return to the level of physical functioning they had prior to HIV infection.
The following case highlights improved physical functioning after ART and the ability to return to basic physical tasks such as walking, eating, and household chores, while at the same time revealing residual physical health impediments.
Case P1: “But now (after ART) I am able to (walk) and I am able to even wash my husband’s clothes. Sometime back I was only able to crawl. I was not able to walk then but now I can hold myself against things and then move. I am able to move out of the house. I now have clutches that I use for walking…The only thing I can complain about is the weakness. Otherwise I don’t feel any pains. I feel I am healthy.”
Impact of HIV and ART on work activity
Respondents were asked to describe their work activities prior to HIV to present day. Prior to HIV diagnoses, nearly all participants (n=38) reported being fully engaged in work (typically working 6-10 hours per day). Half of participants (n=19) who were fully employed had formal employment (work that earns a wage or salary): these occupations ranged from being a factory worker (e.g., in maize mill, or textile factory) to a healthcare professional (nurse) to working in a non-specified business abroad. Half (n=19) was self-employed (e.g., running small microenterprises such as selling and trading food such as fish or potatoes in markets or small kiosks; tailoring; haircutting). Two participants reported partial self-employment along with their formal employment, and one participant was a student and unemployed.
Participants reported a sharp decline in work functioning after HIV-infection and before ART. Over half of the participants that were employed became unemployed after testing HIV-positive. Eight (21%) participants reduced their workload to part-time and only nine (24%) were able to maintain full-time work [a substantial reduction from 37 (93%) prior to HIV]. Participants primarily cited the physical debilitation of the illness as causes for why they had to completely stop working, decrease their workload, or shift to self-employment where they had greater flexibility or accommodation for their health problems. Below are examples of the dramatic debilitating effect of HIV disease on ability to engage in work-related activities.
Case P2, 41 year old male was a builder and taxi driver, and owned a hair salon for women, but his salon failed after he became ill. He also had to stop working altogether when he was severely sick.
Case P14, a 39 year old married male from Namasuba worked at a construction site, where he was doing metal fabrication and welding and also had a shop in Katwe. After his HIV diagnosis, his shop in Katwe had to get transferred to his relatives because he fell sick and thought he was going to die.
Of the 9 participants who were able to maintain their full-time work activity after testing HIV-positive, 4 had formal employment and were well-educated (e.g., nurses, teachers, business administrator), 3 were self-employed primarily trading goods or self-selling, and 2 had a short duration between diagnosis and treatment and thus did not have the opportunity to show a decline in their work activity.
The respondents reported some slight improvement in work functioning after being on ART, but by and large there was not a very noticeable difference in work functioning before and after ART. Furthermore, people who were formally employed but had lost their jobs after becoming HIV-infected were often not able to return to the formal labor market after being on ART, but rather, turned to microenterprise or farming. For example, Case P12 worked at a manufacturing company before HIV and then sold fruits and honey after ART.
Influence of depression on physical and work functioning
Sixty percent of the sample was diagnosed with depression by the clinic psychiatrist (N=26; 9=male, 17=female), with 16 diagnosed after they became HIV positive (pre-ART) and 10 more after they started on ART (post-ART). Many of the respondents described their depression in terms of “thinking too much”, somatic complaints such as sleep difficulties, eating problems, and aches, as well as generally feeling bad about a variety of psychosocial adversities related to poverty, stigma from their HIV status, lack of social support, significant grief and loss, and limited economic opportunities20 (for more detail about depression experiences in our sample please see Okello et al., 2012). Experiences related to depression suggest a hopelessness and lack of control over their health and functioning.
Case P11: “I was thinking too much and that is going to cause my further deterioration. I have no control over the thinking too much. I try so hard not to but I fail. It comes on its own.…It is mainly those apart from the fact that I also don’t sleep. I have to take some sleeping tablets for me to be able to sleep all the time. And then it is worse when I have not slept during the night. I feel worse….There are the things that I have told you about. I worry about how my children will go to school. You think about this and think about that.”
We compared the physical and work functioning trajectories across time points between patients who had experienced depression since entering HIV care and those who had not. Both groups of respondents described full physical and work-related functioning before HIV, so our examination focused mostly on functioning levels prior to and after ART. Regarding physical health functioning, prior to ART few of either of the groups were fully functioning, but nearly half (n = 7/16; 44 %) of the depressed group remained immobile, while the majority (n = 20/24; 83%) of the non-depressed were at least partially functioning. After ART, both groups reported much improvement but while half (n = 7/14; 50%) of the non-depressed group were partially functioning and the other half were fully functioning, some (n =4/26; 15%) of the depressed group remained immobile and most (n= 16/26; 62%) were only partially functioning (see Figure 1).
Figure 1.
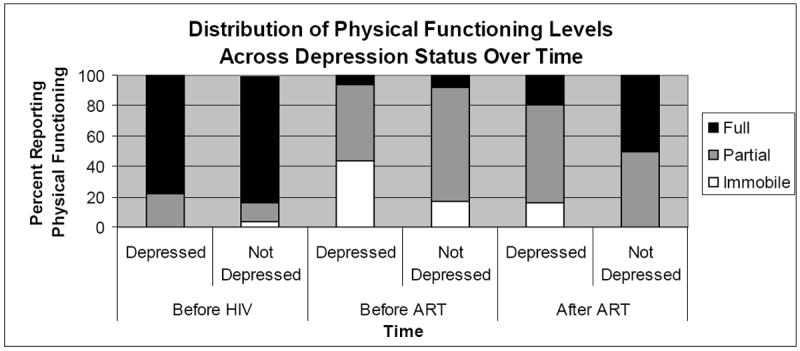
Distribution of Physical Functioning Over Time
asample size: N=39 Before HIV, N=40 Before ART, and N=39 After ART.
With regard to work, prior to ART nearly half (n = 9/22; 41%) of the non-depressed group was not working compared to most (n = 12/16; 75%) of the depressed group. After ART, over half of the depressed group remained unemployed (n=14/26; 54%), whereas most of the non-depressed group was working full-time (n=8/13; 62%; see Figure 2).
Figure 2.
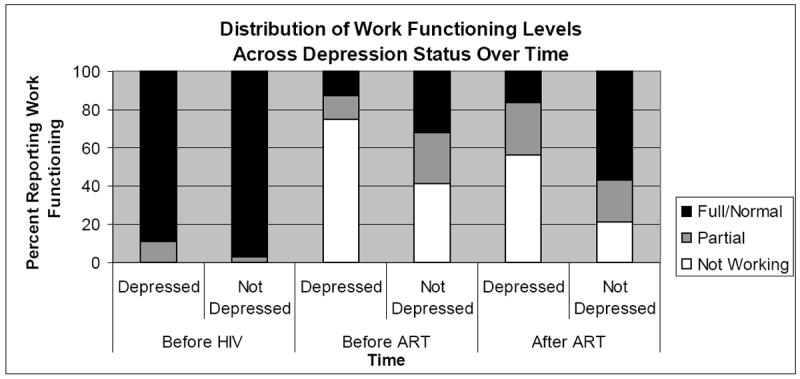
Distribution of Work Functioning Over Time
asample size: N=39 Before HIV, N=38 Before ART, and N=38 After ART.
The influence of antidepressant medications on functioning
Antidepressant medication, which was started after the participants were on ART for those who received the treatment, appears to improve the physical and work functioning of HIV patients suffering from depression. Among the 26 participants who were depressed, 15 had not yet received antidepressant treatment and the other 11 were currently on antidepressants and had been for several months. Figures 3 and 4 show the difference in physical and work functioning trends after starting ART for depressed participants who received antidepressant medication compared with those who did not receive such treatment.
Figure 3.
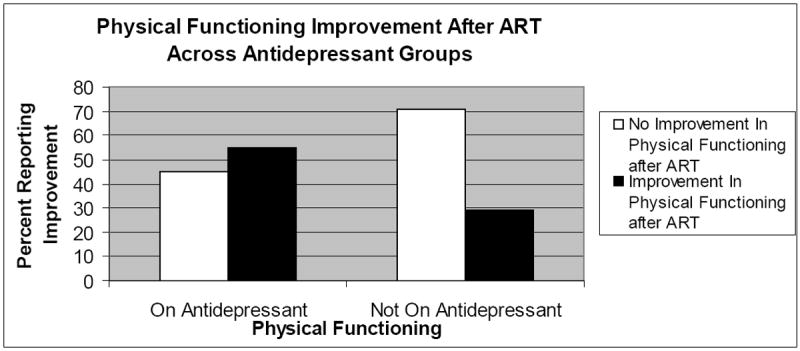
Trend of Physical Functioning for Depressed Patients Across Antidepressant Medication Treatment (N=38)
Figure 4.
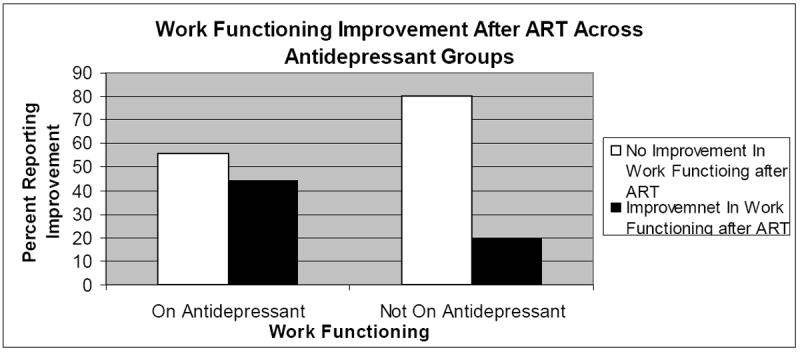
Trend of Work Functioning for Depressed Patients Across Antidepressant Medication Treatment (N=38)
Of the 15 not on antidepressants, only a quarter (n=4) experienced improvement in their physical functioning after being on ART, whereas half (n=6) of the 11 who received antidepressants described improvement, suggesting that depression treatment may play a role in how ART benefits physical functioning among depressed patients.
A similar trend was found for work functioning. Out of the 11 on antidepressants, 4 participants showed improved work functioning after treatment (regained employment), while 5 maintained the same or lower work status (mostly not working) after ART. The example below illustrates a common case of improvement following ART where the respondent was able to regain full employment, however it was below the expectation or wish of the respondent.
Case P6 is a 41-yr old male builder who was able to regain employment after ART. He was a full-time formally employed builder, who stopped working after his HIV infection. He became depressed after HIV and slowly resumed work after ART and depression treatment, although it was not at the level that it was prior to his HIV infection. After ART treatment, he shared, “But even now I have nothing to do because my work was disrupted when I fell sick. I am now doing small things for survival. Before I started building I had apprenticed in carpentry so when I went back I resumed with carpentry because I did not want to stay in the sun for along time. But I haven’t improved to a point where I would say that my work life is good as I would like it to be.”
In contrast to those on antidepressant treatment, only 3 of the 15 participants who did not receive antidepressants regained employment, the remaining 12 maintained the same or had lower work status (mostly not working). Below are examples of untreated cases of depression that continued to decline after ART.
Case P10: 28 year old female who was trained in nursery teaching suffered from maternal depression, which started shortly after she was diagnosed with HIV. She was unable to work with children due to the stressful nature of the work. She did not choose to take medication for her depression and reported significant physical and health problems, which did not improve and resulted in her not working or “doing anything”, even after ART. She shared, “I am so weak and sometimes I wonder why I am continuing to live when I am going through so much pain. From the time that I started on ART, I became so weak. I am always weak with no energy and I just want to lie down all the time…I refuse to eat because I just don’t want to eat. Right now my biggest problem is not having energy. Sometimes I am not even able to wash my own clothes and then I feel pain in all my body. My body is so weak that I even feel pain in all my bones! Then I wonder whether the treatment does not agree with my body.”
Case P26, a 39 year old female teacher declined from full time teaching to not working at all. She suffered from significant trauma related to a miscarriage and an emotionally and sexually abusive relationship that caused her significant distress and hopelessness. Her depression was untreated and she struggled with her adherence to ART. She shares about her difficulties, “It is mainly because of the home issues for example I can not dig and so I worry about what the children are going to eat and then the thought that may be if I died and I wasn’t alive then the thought that I need to see my children grow comes to me and then I begin to think that may be if I could leave home and go and stay somewhere where I would be in control of my life. Then I also start thinking that if I left my children they would be miserable and they would not be able to go to school. That is what makes me feel bad…I cannot do anything because of the children. I think of ending my life but the children. I want them to go to school….I had left them at some point but…They were about to start stealing that time and that is one of the reasons why I decided to go back and suffer with my children. But in a short time after I had come back, the man started coming back and sexually started harassing me.”
As suggested by the experiences described by respondents, many struggled with adversities related to poverty, stigma from HIV status, lack of social support, difficulties managing their family responsibilities, significant grief and loss, as well as limited economic opportunities – all of which contribute to and exacerbate their depression. Among the women, additional fears related to abandonment and abuse, as well as vulnerability due to financial dependency were discussed.
Case P1: “When my husband started mistreating me then the thoughts would come. Sometimes he would even tell me that he was going to marry another woman”
Case P5: “When I don’t give him the money then he mistreats me. So this one lead to my thinking too much even before I learnt that I had HIV.”
Case P9: “This was a difficult time because the man was claiming that he was not the father of the baby. So I was dependent on friends for food. I would feed the baby on cassava porridge, I would give him water, and his feeding was so poor but I am so thankful to God that when they tested him for HIV, he was free of the virus. After sometime, the man seemed like he would come back and he would help me. Then I conceived again. Then when he learnt that I had conceived he ran away again. So I went through a lot of hardships. He left me when I was three months pregnant and I suffered again. During that difficult time, I wanted to die.”
Although antidepressant treatment did not necessarily address these stressors, it appears that relief from “thinking too much” or even improved sleep helped respondents gain some sense of control, strength and ability to cope with their realities. Typical responses related to benefits of depression treatment are similar to Case P12, who received antidepressants and experienced improved work functioning after ART and antidepressant medication. He described similar hopelessness and loss of control as other depressed respondents prior to his treatment, and greater control and management of depression symptoms such as sleep and worry after his ART treatment.
Case P12, a 53 year old male shared that before antidepressants he worried about how he would manage financially, particularly related to caring for his children. “I was worried, I did not have money! The money that I had saved in the bank was all finished. So that is why I was worried and that is the reason why I was not sleeping! The problems that I had of worrying about how these children would stay in school, about how I would fend for them would make me sad.“ After treatment, he indicated, “I gave up on worrying because Dr. Musisi talked with me and I am now able to sleep….I don’t feel sad now. I don’t feel the sadness because Dr. Musisi sat me down and talked with me so I have improved.”
Another participant described the benefits of depression treatment. For example, Case P6, a 41-year old male builder, who became depressed after his wife left him and subsequent feelings of loneliness, was able to not only regain strength from the ART, but also managed his depression, resumed his carpentry, returned to his village and even joined a group of choir singers who became his main source of support.
Case P6 shared, “The (antidepressant) medicine has been good because it has restored me to a good state. It has restored me to a life that I think is good…When one gets this illness of HIV, it is not curable so most times you think that you are going to die and this is the end of you but considering the counseling that I have received and the medication I have had and the way I was before, and the way I am right now, even though I know that I am not very ok, I have hope that I will continue living for sometime although I have thoughts about the children and I don’t have a regular job….But all in all the medicine has been helpful. When I remember how I was and how I am now, there is a great improvement….Let us say I was weak in the body. I was not able to do anything. Then I gradually regained my strength but in 2008 when I came back from the village, I joined a group of gospel singers and so most of my time is spent with them. So I stopped thinking too much.”
DISCUSSION
In summary, our study provides findings about the role of depression on the trajectory of physical and work functioning outcomes for ART clients in Uganda. Narratives about patient’s process of recovery suggest that individuals who have depression also are more likely to describe poorer physical and work functioning outcomes following HIV diagnosis and ART. However, depressed patients who received antidepressant medication described greater benefit from ART and higher functioning compared with those who had not received antidepressant treatment. These results add to the growing body of work suggesting that depression is associated with poorer health outcomes in the context of HIV disease, and that depression treatment may potentially improve response to and benefits of ART.
While our data highlight a relationship between depression and both physical health and work functioning, this cross-sectional study does not allow us to make any causal inferences. While it is reasonable to expect that depression leads to impaired functioning, it is just as plausible that difficulties with physical health or work functioning result in depression. The likely reality is that there is a bidirectional relationship between depression and functioning level, and that for some patients depression causes impairment in physical functioning and work performance, while for other patients it is impaired physical health functioning or loss of work capacity that leads to the emergence of depression. In either pathway, effective depression care and management has the potential to make a strong impact on the health and well-being of patients.
When examining depression in the context of HIV disease, it is important to acknowledge that somatic symptoms of depression, such as fatigue, poor appetite and sleeping problems are also common symptoms of HIV disease; therefore, it can be difficult to discern whether such symptoms and their effects are attributable to depression and not HIV. Furthermore, cross-cultural studies of depression among PLHA in Uganda have shown that patients are more comfortable presenting their somatic symptoms, rather than emotional or affective symptoms,20 making it even more challenging to distinguish depression from manifestations of HIV disease.
Our findings have implications for HIV care management. ART effectiveness is dependent on a high level of adherence to its dosing instructions.21 Depression management may be critical to adherence to ART, as depression has consistently been found to be an impediment to ART adherence.13 Observational studies have shown that antidepressant treatment for depressed PLHA is associated with improved HIV medication adherence.22-25 Although this qualitative study found narratives suggesting improved functioning outcomes for those who received antidepressant medication, we did not examine the potential mediating role of ART adherence nor tease apart the role of their medical status at each of the time points. Future work should explore the impact of depression treatment on adherence management, particularly in developing countries such as Uganda, where virtually no mental health services are provided and cultural explanatory models for depression and health may differ.
Although this qualitative study provides promising results regarding the potential benefits of depression treatment for individuals in HIV care, further work is needed with larger and a more representative sample. Our study focused on HIV-infected individuals on ART, and thus is not representative of all HIV-infected individuals in this setting, where many are not receiving HIV care. Further, our study clinic site was also unique in that psychiatric care was available to HIV clients, which is rare as the availability of mental health specialists is extremely limited in Uganda and most parts of sub-Saharan Africa. Further research is needed to understand the best way to address the integration of psychological, physical, and economic issues in the context of ART scale-up.
CONCLUSIONS
Our mixed methods study provides preliminary findings about the role of depression on the trajectory of physical and work functioning outcomes for ART clients in Uganda. Thematic analyses of narratives regarding HIV patient’s recovery stories suggest that 1) physical and work functioning decreased after patients were diagnosed with HIV, but improved following ART, 2) depression is associated with lower physical health and work functioning levels after HIV diagnosis and after ART, and 3) antidepressant medication, when combined with ART, is associated with better physical and work functioning compared to depressed patients not receiving depression treatment. While causal relationships can not be inferred from our data, our findings suggest that depression plays a role in functioning level and work status and that future longitudinal research is needed to examine whether depression further exacerbates the deleterious effects of HIV on functioning, and whether antidepressant treatment provided alongside ART may serve to help individuals regain functioning, particularly employment.
To the extent that depression influences physical health and work functioning, integration of mental health services into ART programs in sub-Saharan Africa is needed to maximize the benefits of HIV treatment being scaled up in the region. Central to understanding how to effectively deliver depression treatment, attention must be paid to the relationships between the interpersonal, physical, and economic status of individuals living with HIV/AIDS. As seen in our study, respondents attribute their depression to health problems, their inability to work, subsequent financial concerns that make it difficult for them to provide for themselves and their family, and the relationships they have lost. These areas of concern seem to have a debilitating impact on their functioning, as they are inter-related and can easily trigger a downward spiral of hopelessness and despair, which can result in withdrawal, lack of motivation to take care of one’s health, inability to find work, and poor adherence to ART—all of which exacerbate an already fragile state and fatal disease. Given that effectiveness of depression treatment is well established26,27 and may serve to help individuals recover and adjust emotionally, financially, and physically from HIV/AIDS, it is critical that more research is conducted to develop effective strategies to integrate mental health treatment into HIV/AIDS care.
Acknowledgments
This research is supported by a grant from the NIMH (Grant No. 1R01MH083568-01A2; PI: G. Wagner).
References
- 1.UNAIDS. Towards universal access: scaling up priority HIV/AIDS interventions in the health sector. Joint United Nations Programme on HIV/AIDS; Jun, 2008. Progress report. [Google Scholar]
- 2.The Uganda AIDS Commission. The National Piority Action Plan 2012/12-2013/13. Kampala, Uganda: 2011. [Google Scholar]
- 3.Beard J, Feeley F, Rosen S. Economic and quality of life outcomes of antiretroviral therapy for HIV/AIDS in developing countries: a systematic literature review. AIDS Care. 2009;21(11):1343–1356. doi: 10.1080/09540120902889926. [DOI] [PubMed] [Google Scholar]
- 4.Wagner G, Ryan G, Huynh A, Kityo C, Mugyenyi P. A qualitative analysis of the economic impact of HIV and antiretroviral therapy on individuals and households in Uganda. AIDS Patient Care and STDs. 2009;23(9):793–798. doi: 10.1089/apc.2009.0028. [DOI] [PubMed] [Google Scholar]
- 5.Kinyanda E, Hoskins S, Nakku J, Nawaz S, Patel V. Prevalence and risk factors of major depressive disorder in HIV/AIDS as seen in semi-urban Entebbe district, Uganda. BMC Psychiatry. 2011;11:205. doi: 10.1186/1471-244X-11-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brandt R. The mental health of people living with HIV/AIDS in Africa: A systematic review. African Journal of AIDS Res. 2009;8:123–133. doi: 10.2989/AJAR.2009.8.2.1.853. [DOI] [PubMed] [Google Scholar]
- 7.Myer L, Smit J, Roux LL, Parker S, Stein DJ, Seedat S. Common mental disorders among HIV-infected individuals in South Africa: prevalence, predictors, and validation of brief psychiatric rating scales. AIDS patient care and STDs. 2008 Feb;22(2):147–158. doi: 10.1089/apc.2007.0102. [DOI] [PubMed] [Google Scholar]
- 8.Olley B, Seedat S, Stein D. Persistence of psychiatric disorders in a cohort of HIV/AIDS patients in South Africa: a 6-month follow-up study. Journal of Psychosomatic Research. 2006;61(4):479–484. doi: 10.1016/j.jpsychores.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 9.Kaharuza F, Bunnell R, Moss S, et al. Depression and CD4 cell count among persons with HIV infection in Uganda. AIDS and Behavior. 2006;10:105–111. doi: 10.1007/s10461-006-9142-2. [DOI] [PubMed] [Google Scholar]
- 10.Pence B. The impact of mental health and traumatic life experiences on antiretroviral treatment outcomes for people living with HIV/AIDS. Journal of Antimicrobial Chemotherapy. 2009;63(4):636–640. doi: 10.1093/jac/dkp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Whetten K, Reif S, Whetten R, Murphy-McMillan L. Trauma, mental health, distrust, and stigma among HIV-positive persons: implications for effective care. Psychosomatic Medicine. 2008;70(5):531–538. doi: 10.1097/PSY.0b013e31817749dc. [DOI] [PubMed] [Google Scholar]
- 12.Byakika-Tusiime J, Crane J, Oyugi JH, et al. Longitudinal antiretroviral adherence in HIV+ Ugandan parents and their children initiating HAART in the MTCT-Plus family treatment model: role of depression in declining adherence over time. AIDS Behav. 2009 Jun;13(Suppl 1):82–91. doi: 10.1007/s10461-009-9546-x. [DOI] [PubMed] [Google Scholar]
- 13.Ammassari A, Antinori A, Aloisi MS, et al. Depressive symptoms, neurocognitive impairment, and adherence to highly active antiretroviral therapy among HIV-infected persons. Psychosomatics. 2004 Sep-Oct;45(5):394–402. doi: 10.1176/appi.psy.45.5.394. [DOI] [PubMed] [Google Scholar]
- 14.Wagner GJ, Holloway I, Ghosh-Dastidar B, Kityo C, Mugyenyi P. Understanding the influence of depression on self-efficacy, work status and condom use among HIV clients in Uganda. Journal of psychosomatic research. 2011 May;70(5):440–448. doi: 10.1016/j.jpsychores.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Linnemayr S, Wagner G. Physical and mental health as mediators of the impact of ART on economic capacity: evidence from a prospective cohort study. Paper presented at: The 6th IAS Conference on HIV Pathogenesis, Treatment and Prevention; July 17-20, 2011; Rome, Italy. [Google Scholar]
- 16.Ferrando S, Wapenyi K. Psychopharmacological treatment of patients with HIV and AIDS. Psychiatric Quarterly. 2002;73(1):33–49. doi: 10.1023/a:1012840717735. [DOI] [PubMed] [Google Scholar]
- 17.Wagner G, Rabkin J, Rabkin R. A comparative analysis of standard and alternative antidepressants in the treatment of human immunodeficiency virus patients. Comprehensive Psychiatry. 1996;37(6):402–408. doi: 10.1016/s0010-440x(96)90023-1. [DOI] [PubMed] [Google Scholar]
- 18.Collins P, Holman A, Freeman M, Patel V. What is the relevance of mental health to HIV/AIDS care and treatment programs in developing countries? A systematic review. AIDS. 2006;20(12):1571–1582. doi: 10.1097/01.aids.0000238402.70379.d4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ryan G, Bernard H. Data management and analysis methods. 2. Thousand Oaks: Sage Publications; 2000. [Google Scholar]
- 20.Okello ES, Ngo VK, Ryan G, et al. Qualitative study of the influence of antidepressants on psychological health of patients on antiretroviral therapy in Uganda. African Journal of AIDS Res. 2012;11(1):37–44. doi: 10.2989/16085906.2012.671260. [DOI] [PubMed] [Google Scholar]
- 21.Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000 Jul 4;133(1):21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 22.Kumar V, Encinosa W. Effects of antidepressant treatment on antiretroviral regimen adherence among depressed HIV-infected patients. Psychiatric Quarterly. 2009;80(3):131–141. doi: 10.1007/s11126-009-9100-z. [DOI] [PubMed] [Google Scholar]
- 23.Walkup J, Wei W, Sambamoorthi U, Crystal S. Antidepressant treatment and adherence to combination antiretroviral therapy among patients with AIDS and diagnosed depression. Psychiatric Quarterly. 2008;79(1):43–53. doi: 10.1007/s11126-007-9055-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Horberg M, Silverberg M, Hurley L, et al. Effects of depression and selective serotonin reuptake inhibitor use on adherence to highly active antiretroviral therapy and on clinical outcomes in HIV-infected patients. Journal of Acquired Immune Deficiency Syndromes. 2008;47(3):384–390. doi: 10.1097/QAI.0b013e318160d53e. [DOI] [PubMed] [Google Scholar]
- 25.Yun L, Maravi M, Kobayashi J, Barton P, Davidson A. Antidepressant treatment improves adherence to antiretroviral therapy among depressed HIV-infected patients. Journal of Acquired Immune Deficiency Syndromes. 2005;38(4):432–438. doi: 10.1097/01.qai.0000147524.19122.fd. [DOI] [PubMed] [Google Scholar]
- 26.Gilbody S, Bower P, Fletcher J, Richards D, Sutton A. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Archives of Internal Medicine. 2006;166(21):2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 27.Patel V, Aroya R, Chatterjee S, et al. Global Mental Health 3-Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet. 2007;370:991–1005. doi: 10.1016/S0140-6736(07)61240-9. [DOI] [PubMed] [Google Scholar]


