Abstract
Objective
Medicaid sterilization policy, which includes a mandatory 30-day waiting period between consent and the sterilization procedure, poses significant logistical barriers for many women who desire publicly-funded sterilization. Our goal was to estimate the number of unintended pregnancies and the associated costs resulting from unfulfilled sterilization requests due to Medicaid policy barriers.
Study design
We constructed a cost effectiveness model from the health care payer perspective to determine the incremental cost over a 1-year time horizon of the current Medicaid sterilization policy compared to a hypothetical, revised policy in which women who desire a post-partum sterilization would face significantly reduced barriers. Probability estimates for potential outcomes in the model were based on published sources; costs of Medicaid-funded sterilizations and Medicaid-covered births were based on data from the Medicaid Statistical Information System and The Guttmacher Institute, respectively.
Results
With the implementation of a revised Medicaid sterilization policy, we estimated that the number of fulfilled sterilization requests would increase by 45%, from 53.3% of all women having their sterilization requests fulfilled to 77.5%. Annually, this increase could potentially lead to over 29,000 unintended pregnancies averted and $215 million saved.
Conclusion
A revised Medicaid sterilization policy could potentially honor women's reproductive decisions, reduce the number of unintended pregnancies, and save a significant amount of public funds.
Implication
Compared to the current federal Medicaid sterilization policy, a hypothetical, revised policy that reduces logistical barriers for women who desire publicly-funded, post-partum sterilization could potentially avert over 29,000 unintended pregnancies annually and therefore lead to a cost savings of $215 million each year.
Key terms: Tubal sterilization, unfulfilled sterilization, cost analysis
Introduction
Female sterilization is the second most commonly used contraceptive method in the US [1]. Despite the relatively high utilization of this method, there is considerable evidence indicating an unmet demand for the procedure among certain segments of the US population [2-8]. In particular, women who rely on Medicaid may face significant policy-related barriers to obtaining a desired sterilization procedure [5-9].
Current Medicaid sterilization policy was established in the 1970s when reports of non-consensual sterilization among minority and low-income women emerged [10-13]. In response, in 1976, the Department of Health, Education, and Welfare established strict regulations and a standardized consent form for all federally-funded sterilizations [14]. These regulations prohibited sterilization of women under age 21 and of mentally incompetent or institutionalized persons. In addition, the policy required women to wait a minimum of 72 hours between the time of signing the standardized consent form and the procedure; the wait time was subsequently extended to 30 days in 1978 [14, 15]. In compliance with regulations developed in the 1970s, women currently desiring sterilization must complete the Consent to Sterilization section of the Medicaid Title XIX form (Title XIX-SCF) at least 30 days and no more than 180 days prior to the sterilization procedure. In addition, a signed copy of the consent form must be available at the time of the procedure.
Although these policies were well-intentioned, accumulating evidence indicates that the 30-day mandatory waiting period and the need for successful transfer of the completed federal consent form to the delivery unit pose significant barriers for women desiring post-partum sterilization [5-9]. Women report that requesting sterilization too late in pregnancy to fulfill the 30-day waiting period, not having the form present at the time of delivery, or delivering before the mandatory waiting period had elapsed precluded them from having their request for sterilization fulfilled at the time of delivery [2, 6, 7, 9]. Preventing women from using their contraceptive method of choice may put them at high risk for unintended pregnancy. In one study at the University of Texas San Antonio, 47% of women who requested but did not undergo a post-partum sterilization became pregnant in the first year after delivery, twice the rate of women who did not request sterilization [16]. Moreover, women most likely to request publicly funded sterilization – low-income and minority women – are precisely those who are at highest risk for having an unintended pregnancy [17].
Given that the public cost of births resulting from unintended pregnancies is high ($11 billion in 2006) [18], reducing system-level barriers that prevent publicly-insured women from undergoing a desired sterilization would likely be cost saving, although this issue has not been examined. In this study, we performed an evidence-based cost analysis to estimate the savings in unintended pregnancy costs attributable to a hypothetical, revised Medicaid sterilization policy that minimizes logistical barriers and, therefore, the number of unfulfilled post-partum sterilization requests.
Materials and methods
Model structure
A cost effectiveness model was developed using TreeAge Pro 2009 (TreeAge Software, Williamstown, MA). The model was constructed from the health care payer perspective to estimate the incremental cost of the current Medicaid sterilization policy compared to a hypothetical, revised policy in which women who desire post-partum sterilization would face no Medicaid policy-related barriers (Figure 1). Such a revised policy would likely require elimination of the 30-day waiting period which would simultaneously address issues around failed transfer of the completed consent document to the delivery unit.
Figure 1.
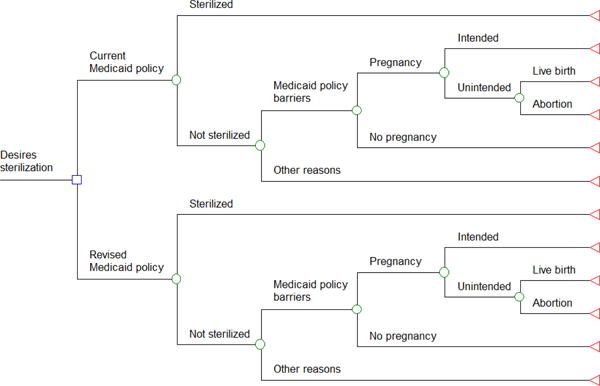
The cost effectiveness model which depicts outcomes and associated costs of the current Medicaid sterilization policy compared to a hypothetical, revised Medicaid policy that minimizes logistical barriers for women who desire publicly-funded, post-partum sterilization
For this analysis, we examined costs related only to publicly-funded, post-partum sterilization procedures. We focused on post-partum sterilization because most of the published and available data on prevalence of sterilization requests, unfulfilled requests, and subsequent pregnancy are for post-partum sterilization requests, as captured when women have entered the healthcare system for prenatal care. Moreover, post-partum procedures represent roughly 80% (and interval procedures about 20%) of the sterilizations completed among Medicaid patients [19].
All women who request a Medicaid-funded post-partum sterilization enter the model, which simulates potential outcomes over a 1-year time horizon. The current policy and revised policy branches of the model are identical except that, in the revised policy branch, the probability of Medicaid policy-related barriers being the reason for unfulfilled sterilization requests is reduced and therefore, the probability that women requesting sterilization actually undergoing the procedure is increased.
Model probabilities and costs
Model probabilities and costs are listed in Table 1 and were based on findings from a comprehensive literature review. For the proportion of unintended pregnancies ending in live birth versus abortion, data on national abortion rates from The Guttmacher Institute were used to determine the proportion of unintended pregnancies in 2008 that ended in abortion among women dependent on Medicaid (special tabulation conducted by Zolna and Finer, The Guttmacher Institute). [20] For the cost of Medicaid-funded sterilizations, we used the Medicaid Statistical Information System (MSIS) to obtain data on Medicaid claims and payment for female sterilization for each state during fiscal year 2010 [21]. At the time of data acquisition, data were available for 46 states, from which we calculated the average cost of a Medicaid-funded sterilization. For the cost of a Medicaid-covered birth, which also varies from state to state, we used a national average estimate for 2008 as reported by The Guttmacher Institute that includes prenatal care, delivery, postpartum care, and infant care for 1 year [22]. This convention is the same as that used in prior studies of cost savings associated with publicly funded contraceptive services [18, 23, 24]. We then inflated the cost of a Medicaid-covered birth to 2010 dollars using the US Consumer Price Index [25].
Table 1. Parameter values used in the model.
| Current Medicaid Policy | Revised Medicaid Policy | ||
|---|---|---|---|
| Parameter | Base case value | Reference | Value a |
| Probability of undergoing sterilization | 53.3% | 7 | 77.5%b |
| Cost of sterilization | $416 | 21 | |
| Probability of not undergoing sterilization | 46.7% | 7 | 22.5% b |
| Reason for not undergoing sterilization due to Medicaid policy barriers | 51.9% | 7 | 0% c |
| Probability of pregnancy | 46.7% | 16 | |
| Probability that the pregnancy is unintended | 100% | Assumption | |
| Probability that unintended pregnancy will end in a live birth | 65% | 20 d | |
| Cost of a live birth | $12,774 e | 22, 25 | |
| Cost of an abortion | $0 | 18, 26 | |
| Reason for not undergoing sterilization unrelated to Medicaid policy barriers | 48.1% | 7 | 100%c |
Only parameter values that changed from the current Medicaid policy base case analysis are shown in this column
The probability of undergoing sterilization under the revised Medicaid policy was calculated by adding the % of women who requested a Medicaid sterilization under the current policy but did not get it due to policy-related barriers (46.7% × 51.9% = 24.2%) to the probability of undergoing sterilization under the current policy (24.2% + 53.3% = 77.5%). The probability of not undergoing sterilization under the revised policy was then calculated by subtracting the probability of undergoing sterilization under the revised policy from 100%
Assumption
Based on a special tabulation conducted by Zolna and Finer (The Guttmacher Institute) indicating that 35% of unintended pregnancies among women relying on Medicaid ended in abortion in 2008
Cost of a Medicaid-funded birth inflated to 2010 dollars (includes costs for prenatal care, delivery, postpartum care and medical care of the infant for one year)
In the absence of published data, we assumed that: 1) all pregnancies occurring after an unfulfilled sterilization request due to Medicaid policy barriers were unintended, and 2) the revised Medicaid policy would reduce Medicaid policy-related logistical barriers to zero.
This analysis focused on understanding the cost savings attributable to a change in Medicaid sterilization policy. Therefore, we did not examine outcomes or related costs for women who did not undergo sterilization because of reasons other than Medicaid policy barriers. Furthermore, because in the vast majority of states, Medicaid does not cover abortions except in cases of rape, incest, and life endangerment [26] and because the cost of abortion compared to an unintended birth is relatively small [18], we assigned zero costs to Medicaid for unintended pregnancies ending in abortion.
Estimating the number of unintended pregnancies and annual public cost associated with unfulfilled sterilization requests
To determine the total annual public cost associated with unfulfilled sterilization requests due to Medicaid policy barriers, we first determined the total number of Medicaid-funded post-partum sterilization procedures performed in 2010 using data from the National Hospital Discharge Summary (NHDS) [27]. We then estimated the number of actual requests for sterilization in that year by dividing the number of sterilizations performed by the estimated proportion of requests that were filled under the current policy. We were then able to estimate the total number of women annually who would undergo sterilization under the revised policy and thereby, calculate the total number of unintended pregnancies averted and the resultant annual cost savings.
Sensitivity analyses
We performed one-way sensitivity analyses on all parameter values to identify those that had the greatest impact on the model and determine threshold values. A threshold value is the point at which a change in a variable would alter the model's conclusion. We also performed a two-way sensitivity analysis in which we varied both the probability of pregnancy within the year following an unfulfilled sterilization request and the probability of terminating an unintended pregnancy after an unfulfilled sterilization request.
Results
Under the current policy, 46.7% of sterilization requests are unfulfilled [7], and over half of these unfulfilled requests (51.9%) are due Medicaid policy-related barriers [7]. Thus, we estimate that 24.2% [46.7% × 51.9% = 24.2%] of women seeking a Medicaid-funded sterilization do not undergo sterilization because of logistical hurdles. Given the published data that nearly half (46.7%) of these women will experience an unintended pregnancy in the year after an unfulfilled sterilization request [16], we estimate that there are 113 potentially avoidable unintended pregnancies per 1,000 women requesting a federally-funded sterilization under the current policy [24.2% × 46.7% = 11.3%]. Therefore, for each sterilization desired that does not occur due to Medicaid policy issues, there is an estimated average cost to the state of $3,877 given the probability of experiencing an unintended pregnancy (46.7%) [16], the proportion of unintended pregnancies ending in a live birth among women dependent on Medicaid (65%) [20], and the average cost of a Medicaid-covered birth ($12,774) [22, 25] [46.7% × 65% × $12,774 = $3,877].
With the implementation of the hypothetical, revised Medicaid policy, the number of unfulfilled sterilization requests due to Medicaid policy logistical barriers drops to zero and thus, the estimated 24.2% of women who would not have received a federally-funded sterilization under the current policy would now undergo sterilization, resulting in an estimated increase in the proportion of fulfilled sterilization requests from 53.3% under the current policy to 77.5% under the revised policy [53.3% + 24.2% = 77.5%], an increase of 45%. Because of the expected corresponding decrease in unintended births, the revised Medicaid policy is cost saving compared to the current policy. For each sterilization that occurs under the revised policy, there is an estimated net savings of $3,461 to the state given the savings attributed to unintended births averted ($3,877) minus the cost of each sterilization ($416) [21].
In 2010, 136,853 Medicaid-funded post-partum sterilizations were performed in the US [27]. Given the published data that only 53.3% of sterilization requests are fulfilled under the current federal policy [7], we calculated that 256,759 women likely requested the procedure. Under the revised policy, an estimated 77.5% of these women would undergo sterilization, resulting in an additional 62,135 procedures performed. This increase in the number of fulfilled sterilizations would lead to approximately 29,000 unintended pregnancies averted in the same year [62,135 × 46.7% chance of experiencing unintended pregnancy], resulting in approximately 10,000 fewer abortions and 19,000 fewer unintended births. We estimated that the resulting annual total cost savings associated with the revised Medicaid policy would thus be $215 million (62,135 × $3,461 in net savings per additional sterilization completed).
In one-way sensitivity analyses, we found that our results were not qualitatively sensitive to changes in any of the parameter values. We also determined the threshold values for several variables in the model for which the revised policy would be more costly than the current policy. These were, among women having an unfulfilled sterilization request: < 6% of women experiencing a pregnancy in the following year, <11% reporting that their pregnancy was unintended, or > 93% of women terminating their unintended pregnancy. The cost of sterilization would have to be over 9 times as high (> $3,880) than the baseline value for the revised policy to be more costly than the current policy. In two-way sensitivity analysis, varying both the probability of pregnancy within the year following an unfulfilled sterilization request and the probability of terminating an unintended pregnancy after an unfulfilled sterilization request, the revised policy will always be cost saving if the probability of pregnancy in this circumstance is 20% or more and the probability of abortion is 83% or less.
Discussion
Using a cost analysis, we were able to estimate the number of unintended pregnancies averted and the resultant cost savings over one year from a health care payer perspective when the current Medicaid policy is replaced with a hypothetical, revised policy that minimizes logistical barriers for women who request a publically-funded, post-partum sterilization procedure. According to our model, a revised policy could potentially avert over 29,000 unintended pregnancies annually and therefore lead to a cost savings of $215 million each year.
We recognize that Medicaid sterilization policy was originally instituted for ethical reasons and not economic ones. However, there is emerging evidence that the Medicaid consent process may not be capable, in fact, of protecting women by ensuring informed consent. Although the current Medicaid consent form contains language to confirm understanding of the risks (including the permanent nature of the procedure) and benefits of the procedure as well as information about the mandatory 30-day waiting period, readability assessments indicate that the format is complicated and the literacy level is much higher than that of the average American adult [28]. In one study that assessed sterilization knowledge after giving women the current Medicaid consent form for review, over a third of women (34%) incorrectly answered a question about the permanence of the procedure [29]. Moreover, the policy creates another ethical tension - because women with private insurance are not subject to the same regulations, the policy creates a two-tiered system of access in which low-income women may not be able to exercise the same degree of reproductive autonomy. Inequitable access is further compounded by the fact that women covered by Medicaid who do not receive a desired post-partum sterilization may not be eligible for coverage of other contraceptive methods as Medicaid coverage often ends shortly after delivery for many women [30]. These issues recently prompted the American College of Obstetrics and Gynecology (ACOG) Committee on Health Care for Underserved Women to recommend that Medicaid sterilization policy be revised to create fair and equitable access [8].
To both honor women's reproductive autonomy and protect vulnerable populations, our efforts should be directed toward enhancing informed decision making rather than impeding access to the procedure. To this end, the development and testing of a decision aid for female sterilization may help ensure that women receive high-quality, comprehensive information and make decisions that align with their personal goals and values. Among those who have then made an informed decision, efforts to facilitate completion of a desired sterilization should ensue. These may necessitate eliminating or drastically shortening the current 30-day mandatory waiting period, a change that would likely also address issues around failed transfer of the completed federal document to the delivery unit. An ideal policy would be one that could facilitate both informed decision making and subsequently fulfilling informed sterilization requests. In doing so, it would respect women's decision-making capacity, create more equitable access to sterilization, prevent unintended pregnancy and the adverse social and health consequences associated with it, and save a significant amount of taxpayer money and healthcare dollars.
This analysis is not without limitations. First, probability estimates for unfulfilled sterilization requests, reasons for unfulfilled sterilization requests, and unintended pregnancy after an unfulfilled sterilization request were based on single studies and may not be generalizable. However, another study by Thurman et al. that examined the incidence of unfulfilled sterilization requests and how often an unfulfilled sterilization request was due to Medicaid policy barriers in a Texas hospital had comparable estimates [6]. We did not use these Texas data because the estimates included women with CHIP-perinate insurance that requires women to pay for post-partum sterilizations, constituting an additional barrier for these women. Furthermore, sensitivity analyses indicated that even with large changes in these probabilities, the current policy will always be more costly than the revised policy. Second, estimates of the overall public costs of unintended pregnancies did not include costs related to abortion or costs related to children's medical care beyond their first year of life. We also did not include the costs associated with unintended pregnancies occurring beyond the first year after an unfulfilled sterilization request. Thus, our findings likely significantly underestimate the true public cost of unfulfilled sterilization requests. We also did not include costs of alternative contraceptive methods for women who did not undergo sterilization, but these costs would likely be negligible compared to the costs of unintended pregnancy over one year. Third, our estimates are based on current demand for sterilization among low-income women. It is entirely possible that if the Medicaid Title XIX consent form is revised or replaced with a consent process that truly ensures comprehension (as per our description of an ideal policy), more women may choose alternative forms of highly-effective contraception, and the demand for sterilization will decrease.
In conclusion, the current Medicaid sterilization policy has led to a substantial unmet demand for sterilization among low-income women. It is unclear that the current Medicaid consent policy protects vulnerable women, but it does cost the US a significant amount of money due to missed opportunities for sterilization among women who desire it. Current pressing societal issues include an unacceptably high unintended pregnancy rate and rising health care costs. With states now examining Medicaid spending closely, re-visiting and modifying Medicaid sterilization policy (both the consent form and the mandatory waiting period) represents an opportunity to simultaneously serve patients' interests, reduce the number of unintended pregnancies, and save public dollars.
Acknowledgments
This work was supported by the National Center for Research Resources and the National Center For Advancing Translational Sciences of the National Institutes of Health through Grant Number 2KL2 RR024154-06. The funding agency had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript. This work was also supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development grant for Infrastructure for Population Research at Princeton University, Grant R24HD047879.
Footnotes
Disclosures: None
This is a PDF file of an unedited manuscript that has been accepted for publication.As a service to our customers we are providing this early version of the manuscript.The manuscript will undergo copyediting, typesetting, and review of the resulting proofbefore it is published in its final citable form. Please note that during the productionprocess errorsmaybe discovered which could affect the content, and all legal disclaimersthat apply to the journal pertain.
References
- 1.Mosher WD, Jones J. Use of contraception in the United States: 1982-2008. National Center for Health Statistics Vital Health Statistics. 2010;23 [PubMed] [Google Scholar]
- 2.Potter JE, White K, Hopkins K, et al. Frustrated demand for sterilization among low-income Latinas in El Paso, Texas. Perspect Sex Reprod Health. 2012;44:228–235. doi: 10.1363/4422812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Borrero S, Nikolajski C, Rodriguez KL, Creinin MD, Arnold RM, Ibrahim SA. “Everything I know I learned from my mother…or not”: Perspectives of African-American and white women on decisions about tubal sterilization. J Gen Intern Med. 2009;24:312–9. doi: 10.1007/s11606-008-0887-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zite N, Wuellner S, Gilliam M. Failure to obtain desired postpartum sterilization: Risk and predictors. Obstet Gynecol. 2005;105:794–9. doi: 10.1097/01.AOG.0000157208.37923.17. [DOI] [PubMed] [Google Scholar]
- 5.Davidson A, Philliber S, Graves W, Rulin M, Cushman L. Sterilization decision making and regret: The determinants and consequences of unfulfilled sterilization plans. Annual Meeting of the Population Association of America 1990; Toronto, Canada. [Google Scholar]
- 6.Thurman AR, Harvey D, Shain RN. Unfulfilled postpartum sterilization requests. J Reprod Med. 2009;54:467–72. [PubMed] [Google Scholar]
- 7.Zite N, Wuellner S, Gilliam M. Barriers to obtaining a desired postpartum tubal sterilization. Contraception. 2006;73:404–7. doi: 10.1016/j.contraception.2005.10.014. [DOI] [PubMed] [Google Scholar]
- 8.Committee on Health Care for Underserved Women. Access to Postpartum Sterilization. The American College of Obstetricians and Gynecologists. 2012 Committee Opinion Number 530. [Google Scholar]
- 9.Gilliam M, Davis SD, Berlin A, Zite NB. A qualitative study of barriers to postpartum sterilization and women's attitudes toward unfulfilled sterilization requests. Contraception. 2008;77:44–9. doi: 10.1016/j.contraception.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 10.Relf v. Weinberger. Civ. A. Nos. 73-1557. DC: 1973. [Google Scholar]
- 11.Cox v. Stanton. 1974;381 F(Supp):349. [Google Scholar]
- 12.Schoen J. Choice and control: Birth control, sterilization, and abortion in public health and welfare. Chapel Hill, NC: University of North Carolina Press; 2005. [Google Scholar]
- 13.Washington H. Medical apartheid: The Dark history of medical experimentation on black Americans from colonial times to the present. New York: Doubleday; 2006. [Google Scholar]
- 14.Department of Health, Education, and Welfare. 42 Code of Federal Regulations. 1976:441.257. [Google Scholar]
- 15.Department of Health, Education, and Welfare. 42 Code of Federal Regulations. 1978:441.253. [Google Scholar]
- 16.Thurman AR, Janecek T. One-year follow-up of women with unfulfilled postpartum sterilization requests. Obstet Gynecol. 2010;116:1071–7. doi: 10.1097/AOG.0b013e3181f73eaa. [DOI] [PubMed] [Google Scholar]
- 17.Finer L, Zolna M. Unintended pregnancy in the United States: Incidence and disparities, 2006. Contraception. 2011;84:478–85. doi: 10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sonfield A, Kost K, Benson Gold R, Finer L. The public costs of births resulting from unintended pregnancies: National and state-level estimates. Perspect Sex Reprod Health. 2011;43:94–102. doi: 10.1363/4309411. [DOI] [PubMed] [Google Scholar]
- 19.Potter JE, Stevenson AJ, White K, Hopkins K. Hospital variation in postpartum tubal sterilization rates in California and Texas. Obstet Gynecol. 2013;121:152–8. doi: 10.1097/aog.0b013e318278f241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Special tabulation used data from the following sources: The 2006-2010 National Survey of Family Growth; the Guttmacher Institute's 2008 Abortion Patient Survey. Martin JA, Hamilton BE, Sutton PD, et al. Births Final data for 2008. Natl Vital Stat Rep. 2010;59(1):1–72. [Google Scholar]; Jones RK, Kooistra K. Abortion incidence and access to services in the United States, 2008. Perspect Sex Reprod Health. 2011;43(1):41–50. doi: 10.1363/4304111. [DOI] [PubMed] [Google Scholar]
- 21.Medicaid Statistical Information System (MSIS) state summary datamarts. [Accessed February 18, 2013]; at www.cms.gov.
- 22.Frost J, Henshaw S, Sonfield A. Contraceptive needs and services: National and state data,2008 update. New York: Guttmacher Institute; 2010. [Google Scholar]
- 23.Frost J, Sonfield A, Gold R. Estimating the impact of expanding medicaid eligibilty for family planning services. New York: Guttmacher Institute; 2006. [Google Scholar]
- 24.Frost JJ, Finer LB, Tapales A. The impact of publicly funded family planning clinic services on unintended pregnancies and government cost savings. J Health Care Poor Underserved. 2008;19:778–96. doi: 10.1353/hpu.0.0060. [DOI] [PubMed] [Google Scholar]
- 25.Consumer Price Index. United States Department of Labor, Bureau of Labor Statistics. [Accessed February 18, 2013]; at http://www.bls.gov/cpi/
- 26.Guttmacher Institute. State funding of abortion under Medicaid. State Policies in Brief. 2012 [Google Scholar]
- 27.National Hospital Discharge Survey (NHDS) [Accessed August 2, 2012]; at http://www.cdc.gov/nchs/index.htm.
- 28.Zite NB, Philipson SJ, Wallace LS. Consent to Sterilization section of the Medicaid-Title XIX form: Is it understandable? Contraception. 2007;75:256–60. doi: 10.1016/j.contraception.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 29.Zite N, Wallace L. Use of a low-literacy informed consent form to improve women's understanding of tubal sterilization: A randomized controlled trial. Obstet Gynecol. 2011;117:1160–6. doi: 10.1097/AOG.0b013e318213cbb1. [DOI] [PubMed] [Google Scholar]
- 30.Pregnant women. [Accessed March 6, 2013]; at www.medicaid.gov.


