Abstract
Asian Americans have disproportionately high prevalence of chronic hepatitis B virus infection in the United States and yet have low hepatitis B screening and vaccination rates. We developed three photonovels specifically designed for Chinese, Korean, and Vietnamese Americans and evaluated their cultural relevance and effectiveness in increasing self-efficacy and intention to have a hepatitis B screening. Photonovels' storylines were drawn from focus group themes, and lay people from each community played actors/actresses in community settings. Photonovels were pilot tested, revised, and distributed in a hepatitis B intervention. A two-page process evaluation questionnaire was mailed to 441 participants after one month. Descriptive analysis and multiple logistic regressions were conducted to assess the overall evaluation of the photonovel and to assess factors associated with self-efficacy and intention to have hepatitis B screening. Eighty-four percent of participants responded to the process evaluation. The majority of participants either strongly agreed or agreed that the cancer information in the photonovel was helpful, the story was written by someone who knows the community, and the information was easy to understand. Overall, more than 80% of them thought this photonovel was a good teaching tool. Favorable evaluation of the photonovel was associated with both having intention and self-efficacy to have a hepatitis B screening in the next 5 months. When stratified by level of education and income, the associations were stronger among the lower income and education groups. Culturally appropriate photonovels are useful tools to promote hepatitis B screening among Asian Americans, especially among those of lower socioeconomic status.
Keywords: Asian Americans, community-based participatory research, educational material, hepatitis B, photonovel, screening
Asian Americans have disproportionately high prevalence of chronic hepatitis B virus (HBV) infection in the United States: Asian Americans accounted for nearly half of all persons with chronic HBV infection, whereas they only accounted for 5% of the U.S. total population (Office of Minority Health, 2008; U.S. Census Bureau, n.d.). Chronic HBV infection contributes to nearly 80% of liver cancer cases (World Health Organization, 1983;Yu, Yuan, Govindarajan, & Ross, 2000). However, rates of hepatitis B screening and vaccination have been low among Asian Americans (Ma, Fang, et al., 2007; Ma, Shive, Toubbeh, Tan, & Wu, 2008; Wu, Lin, So, & Chang, 2007). Previous studies have identified common factors associated with the low rates, including (a) low awareness or knowledge about HBV infection (Chao, Chang, & So, 2009; Ma, Fang, et al., 2007; Ma et al., 2008; T. T. Nguyen et al., 2007; Wu et al., 2007); (b) limited English fluency and low health literacy (Chang, Nguyen, & So, 2008; Hu, 2008); (c) limited access to care (Chang et al., 2008; G. T. Nguyen & Bowman 2007; T. T. Nguyen et al., 2007); and (d) cultural barriers (i.e., spiritual beliefs and beliefs about Chinese medicine; Coronado et al., 2007; Tran, 2009). Therefore, culturally and linguistically appropriate education programs are needed for Asian Americans to promote hepatitis B screening and vaccination, and thus reduce the disparity in liver cancer rates (Chen, 2005; Coronado et al., 2007; Hu, 2008; Juon et al., 2008; Kreps & Sparks, 2008; Ma, Shive, et al., 2007; Ma et al., 2008; T. T. Nguyen et al., 2010; Wu et al., 2007).
A photonovel might be a culturally appropriate educational material to promote liver cancer prevention among Asian Americans because it is an educational storybook that incorporates culturally appropriate components, such as photos of faces familiar to the community featured as main characters of the story, daily dialogues used by the community people, and storylines drawn from common life experiences in the community. It has been used as a means of participatory education that maximizes the co-learning experience through active involvement of the target population (Roter, Rudd, Keogh, & Robinson, 2006; Rudd & Comings, 1994). There is a scarcity of studies that have examined the effectiveness of photonovels in promoting health. Early studies have used the photonovel for health promotion among vulnerable populations and demonstrated its effectiveness in increasing self-efficacy of health promoting behaviors (Dick, Van der Walt, Hoogendoorn, & Tobias, 1996; Roter et al., 2006). More recently, photonovels have started to be used as a strategy for health promotion among immigrant populations because of potential effectiveness of delivering important health information without using a large amount of text or difficult medical terms (Nimmon, 2007; Quinn, Hauser, Bell-Ellison, Rodriguez, & Frias, 2006). For example, photonovels (also known as fotonovelas) to promote knowledge and prevention of tuberculosis, dementia, and depression were developed for a Latino population who had limited English proficiency and health literacy. Satisfaction with these educational materials was reported (Cabassa, Molina, & Baron, 2012; Cabrera, Morisky, & Chin, 2002; Velle, Yamada, & Matiella, 2006).
However, there is a lack of research developing and testing photonovels among Asian Americans. The goal of the current study was to examine whether the degree to which participants found the material to be a culturally appropriate, helpful, good teaching tool was associated with self-efficacy and intention to participate in hepatitis B screening in the next 5 months. Specifically targeting for Chinese, Korean, and Vietnamese Americans, the three photonovels were developed based on focus group findings and rich community input. Rarely done in previous studies, the current study also aimed to quantify the effectiveness of the photonovel in increasing participants' self-efficacy and intention to have a hepatitis B screening. Self-efficacy and intention have been identified as important determinants of health behaviors by the health belief model and the theory of planned behavior (Glanz, Rimer, & Viswanath, 2008) and have been used as predictors for cancer screening (Fang, Ma, Tan, & Chi, 2007; Stewart, Rakowski, & Pasick, 2009). Our culturally appropriate education materials were designed to help our study participants increase their intention and self-efficacy to have hepatitis B screening by increasing perceived susceptibility, perceived benefits, motivation to comply, knowledge to overcome perceived barriers, and by providing cue to action.
Method
Formative Research
Eight focus groups were conducted in Chinese, Korean, and Vietnamese American communities in Maryland in 2009 to investigate knowledge, perception, and experience about hepatitis B and liver cancer, and their perceived barriers of prevention. Two focus groups each were conducted in Chinese, Korean, and Vietnamese Americans, and another two focus groups were conducted in English for young English-speaking Asian Americans. Details on the methods of the focus groups and general findings have been reported elsewhere (Philbin, Erby, Lee, & Joun, 2012). At the end of each focus group, half an hour was devoted to eliciting thoughts about content, design, layout and readability of existing educational materials on hepatitis B and liver cancer prevention. These included English and translated versions of educational brochures developed by academic institutions and pharmaceutical companies.
Common themes emerged across the groups, including low knowledge about the disease, low awareness of risk factors, lack of emphasis on prevention, and limited health insurance coverage. This was done by two investigators by comparing content analysis results in each ethnic group. On the other hand, cultural factors unique to each community shaped their perception of the disease (see “Cultural Elements” in Table 1). In commenting on the existing educational brochures, participants were asked to rank the brochures based on how much they had learned from reading them. Plain and succinct language was preferred. Relevance to the target audience was another important attribute of a successful educational brochure; our participants suggested using pictures of Asians and Asian languages on the front cover, and indicating a clear focus on prevention for healthy people as opposed to a focus on patients.
Table 1. The Storyline of the Three Photonovels.
| Ethnicity | Storyline | Cultural Elements |
|---|---|---|
| Chinese |
|
|
| Korean |
|
|
| Vietnamese |
|
|
Production of Photonovel
Based on the findings from the focus groups, the research team developed culturally appropriate photonovels for each ethnic group. The storyline was drafted to capture the major issues or concerns of hepatitis B prevention in each ethnic group as revealed in the focus groups. To reinforce the cultural relevance, all actors and actresses were recruited from each community. All pictures were taken at local places such as nail salons, personal residences, schools, parks, and doctor's offices. One Chinese physician, who has been devoted to hepatitis B advocacy and is well known to Asian communities, volunteered to play the doctor for all three photonovels. They were designed for both English and non-English speakers, with the first half of the booklet in Chinese/Korean/Vietnamese, and the second half in English. “Fact boxes,” created to provide readers with more epidemiological and medical information on hepatitis B and liver cancer, were placed throughout the booklet, with a Q&A (question and answer) section at the end. The information was reviewed by a hepatologist. Storylines for each group are presented in Table 1.
Three photonovels were pilot tested among 30 people, including lay persons from each community, members of our community advisory board, and co-investigators of the project. Pilot testing questions focused on the cultural relevance of the storyline, performance of actors and actresses, understandability of the content, and overall design of the booklet (e.g., size, format, and color). The use of plain language was suggested in the pilot testing, and revisions were made to avoid medical terms and simplify the dialogue; for example, HBsAg (surface antigen) and HBsAb (surface antibody) were replaced by simple terms such as “infected” or “protected.” According to the feedback from the pilot testing, storylines and overall design were slightly modified so that they would be better accepted by the community. These culturally appropriate photonovels were developed in English and translated into each Asian language by a bilingual research assistant. Back-translation was conducted by another bilingual research assistant to ensure accuracy. Also, translation quality was reviewed by participants in pilot testing. Since close to 70% of our participants had poor English proficiency, translation was an important key to making the photonovels accessible to all participants.
Process Evaluation
Photonovels were included as one component of our culturally relevant intervention to increase awareness of hepatitis B and liver cancer and encourage screening behavior. The intervention was a randomized community trial targeting Chinese, Korean, and Vietnamese Americans residing in Maryland. The 90-minute intervention program included a PowerPoint presentation, a role play video, and a Q&A session, and was delivered to participants recruited from community-based organizations, language schools, nail salons, grocery markets, and restaurants. At the end of the intervention session, each participant was encouraged to read a photonovel and was informed that we would follow up on their evaluation of the photonovel 1 month later.
Data collection
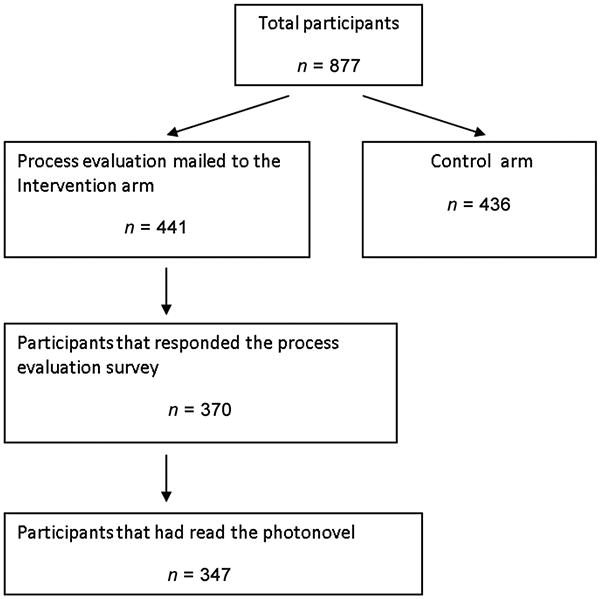
Participants in the intervention arm received a mailed two-page questionnaire to evaluate the photonovels 1 month after the education program. E-mail reminders were sent to those who had not mailed back the questionnaire after 2 weeks. After another 2 weeks, we made phone calls to those who still had not responded for a phone interview and asked the questionnaire questions by phone. Process evaluation questionnaires were mailed to 441 participants who received the intervention (n = 151, n = 148, and n = 142 for Chinese, Korean, and Vietnamese groups, respectively). In total, 370 (84%) participants responded to the questionnaire, among whom 80.7% responded by mail, 18.8% by telephone interviews, and 0.5% by e-mail. The response rates combining mail, telephone, and e-mail were 90.1%, 86.5%, and 74.6% for Chinese, Korean, and Vietnamese groups, respectively. Among the 370 participants who responded to the survey, 347 (94%) indicated that they had read the photonovel and were thus included in our further analysis. (Figure 1)
Figure 1. Participants flowchart.
Measures
The process evaluation was a 15-item questionnaire translated into Chinese, Korean, and Vietnamese languages. It was developed primarily based on the evaluation questions of the previously developed photonovel by Roter et al. (2006). It centered on the question “How effective and culturally appropriate was our photonovel as liver cancer educational material targeting Asian Americans.” The questions included items such as (a) Do you think that the cancer information presented in the photonovel is helpful? (b) Do you agree the photonovel is written by someone who knows the community? (c) Do you agree that our photonovel is a good teaching tool? (d) After you read the photonovel, are you planning to get hepatitis B screening in the next 5 months? (e) After you read the photonovel, are you confident that you can go for a hepatitis B screening test? The response options for some questions were “yes, no, or not sure”; other questions used a 5-point Likert-type scale from strongly disagree to strongly agree. Additionally, there was an open-ended question at the end of the instrument to accommodate more comments and feedback from participants.
Outcome variables
Having intention to do the screening was defined as answering “yes” to the question “After you read the photonovel, are you planning to get hepatitis B screening in the next 5 months?” Those who answered other than “yes” or “no” (i.e., do not know, had screening before, infected, etc.) to this item were excluded from the regression analysis for intention. On a 5-point Likert-type scale, having self-efficacy for hepatitis B screening was defined as answering very confident or confident to the question “After you read the photonovel, are you confident that you can go for a hepatitis B screening test?” Those who indicated they had screening before, had antibody or had been infected were excluded from the regression analysis for self-efficacy.
Covariates
The covariates were as follows: age, gender (0 = male, 1 = female), education (0 = <high school, 1 = some college, 2 = college graduates or above), household income (0 = <$10,000, 1 = $10,000-$29,999, 2 = $30,000-$49,999, 3 = $50,000-$74,999, 4 = $75,000-$99,999, 5 = ≥$100,000), health insurance coverage (0 = no, 1 = yes), English proficiency (0 = not well, 1 = so-so, 2 = well), ethnicity (0 = Korean, 1 = Chinese, 2 = Vietnamese).
Statistical analysis
Descriptive analysis and chi-square or t tests were conducted to assess and compare sociodemographic characteristics of our respondents. Distribution of response to the survey items was also assessed and compared among three ethnic groups using chi-square tests. Multiple logistic regressions were performed to assess factors associated with self-efficacy and intention to have hepatitis B screening test, adjusting for age, gender, ethnicity, education, income, access to health care, English proficiency, and proportion of life in the United States.
Results
As shown in Table 2, our participants had a mean age of 47 years, with slightly more females than males. In general, more than half the participants had college education or more, with Chinese having the highest college graduate proportion and Vietnamese having the lowest. Participants had a wide range of annual household income, with 20% having <$10,000. The majority of participants had health insurance coverage and most of them did not speak English well. On average, they had spent about one third of their life living in the United States.
Table 2. Participants' Sociodemographic Characteristics by Ethnicity (n = 347).
| Total | Korean | Chinese | Vietnamese | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||
| Sociodemographic Characteristics | n | % | n | % | n | % | n | % | P |
| Age in years (mean ± SE) | 46.8 ± 12.4 | 45.8 ± 12.1 | 46.8 ± 11.5 | 47.8 ± 13.9 | .5 | ||||
| Gender | .09 | ||||||||
| Female | 197 | 56.8 | 73 | 62.4 | 76 | 58.5 | 48 | 48.0 | |
| Male | 150 | 43.2 | 44 | 37.6 | 54 | 41.5 | 52 | 52.0 | |
| Education | <.0001 | ||||||||
| High school or less | 121 | 34.9 | 46 | 39.3 | 22 | 16.9 | 53 | 53.0 | |
| Some college | 30 | 8.7 | 8 | 6.8 | 6 | 4.6 | 16 | 16.0 | |
| College graduate or above | 196 | 56.5 | 63 | 53.9 | 102 | 78.5 | 31 | 31.0 | |
| Annual household income (US$) | <.0001 | ||||||||
| Missing | 10 | 2.9 | 3 | 2.6 | 4 | 3.1 | 3 | 3.0 | |
| <10,000 | 70 | 20.2 | 18 | 15.4 | 20 | 15.4 | 32 | 32.0 | |
| 10,000-29,999 | 54 | 15.6 | 19 | 16.2 | 11 | 8.5 | 24 | 24.0 | |
| 30,000-49,999 | 52 | 15.0 | 26 | 22.2 | 12 | 9.2 | 14 | 14.0 | |
| 50,000-74,999 | 41 | 11.8 | 25 | 21.4 | 5 | 3.9 | 11 | 11.0 | |
| 75,000-99,999 | 38 | 11.0 | 11 | 9.4 | 21 | 16.2 | 6 | 6.0 | |
| ≥100,000 | 82 | 23.6 | 15 | 12.8 | 57 | 43.9 | 10 | 10.0 | |
| Have health care coverage | .12 | ||||||||
| Yes | 244 | 70.3 | 75 | 64.1 | 99 | 76.1 | 70 | 70.0 | |
| No | 103 | 29.7 | 42 | 35.9 | 31 | 23.9 | 30 | 30.0 | |
| English proficiency | .07 | ||||||||
| Well | 108 | 31.1 | 27 | 23.8 | 47 | 36.1 | 34 | 34.0 | |
| Poor | 239 | 68.9 | 90 | 76.9 | 83 | 63.9 | 66 | 66.0 | |
| Proportion of life in the United States | 0.32 ± 0.21 | 0.36 ± 0.23 | 0.26 ± 0.17 | 0.36 ± 0.24 | <.0001 | ||||
Among the participants who read our photonovel, the majority thought highly of our photonovel across the three ethnic groups (see Table 3). The vast majority of participants in all three groups either strongly agreed or agreed that the cancer information in the photonovel was helpful, the story was written by someone who knows the community, and the information was easy to understand. Overall, more than 80% of them thought this photonovel was a good teaching tool. A considerable number of respondents had recommended our photonovel to others: 34% of Koreans, 41% of Chinese, and 62% of Vietnamese. In general, the Vietnamese group rated the photonovel most favorably among the three groups.
Table 3. Participants' Response to Process Evaluation by Ethnicity (n = 347).
| Korean | Chinese | Vietnamese | |||||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| Ethnicity | n | % | n | % | n | % | P |
| Do you think that the cancer information presented is helpful? | <.0001 | ||||||
| Strongly agree | 58 | 50.0 | 80 | 61.5 | 81 | 81.0 | |
| Agree | 42 | 36.2 | 27 | 20.8 | 14 | 14.0 | |
| Neutral/disagree/strongly disagree | 16 | 13.8 | 23 | 17.7 | 5 | 5.0 | |
| Do you agree that it is written by someone who knows your community? | .06 | ||||||
| Strongly agree | 43 | 36.8 | 62 | 47.7 | 56 | 56.6 | |
| Agree | 45 | 38.5 | 38 | 29.2 | 24 | 24.2 | |
| Neutral/disagree/strongly disagree | 29 | 24.8 | 30 | 23.1 | 19 | 19.2 | |
| Do you agree that the dialogue is easy to understand? | .01 | ||||||
| Strongly agree | 67 | 57.8 | 83 | 64.3 | 76 | 76.0 | |
| Agree | 34 | 29.3 | 28 | 21.7 | 18 | 18.0 | |
| Neutral/disagree/strongly disagree | 15 | 12.9 | 18 | 14 | 6 | 6.0 | |
| Do you agree that our photonovel is a good teaching tool? | .04 | ||||||
| Strongly agree | 75 | 64.1 | 77 | 59.2 | 75 | 75.0 | |
| Agree | 26 | 22.2 | 35 | 26.9 | 19 | 19.0 | |
| Neutral/disagree/strongly disagree | 16 | 13.7 | 18 | 13.9 | 6 | 6.0 | |
| Have you recommended this photonovel to others? | .0001 | ||||||
| Yes | 40 | 34.2 | 52 | 40.6 | 62 | 62.0 | |
| No | 77 | 65.8 | 76 | 59.4 | 38 | 38.0 | |
After adjusting for age, gender, ethnicity, education, household income, access to health care, English proficiency, and proportion of life in the United States, results from multiple logistic regression showed that favorable evaluation of the photonovel was associated with both having intention and self-efficacy to have a hepatitis B screening in the next 5 months. Compared with those who disagreed that the information provided in the photonovel was helpful, those who agreed were more likely to have intention for screening and have self-efficacy for screening. Those who agreed that the story was written by someone who knows the community were more likely than those who disagreed to have the intention and self-efficacy to get hepatitis B screening. Similarly, those who thought the photonovel was a good teaching tool were more likely to have the intention and self-efficacy to get hepatitis B screening than those who disagreed (see Table 4).
Table 4. Association Between Evaluation of the Photonovel and Intention/Self-Efficacy to Have a Hepatitis B Screening.
| Intention (n = 235)a | Self-Efficacy (n = 322)a | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Unadjusted | Adjustedb | Unadjusted | Adjustedb | |||||
|
|
|
|
|
|||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Information is helpful | 3.9 | [1.7, 9.3] | 3.9 | [1.4, 10.5] | 7.4 | [3.7, 15.0] | 7.2 | [3.3, 15.8] |
| Story is written by someone who knows the community | 2.2 | [1.0, 4.4] | 2.6 | [1.1, 6.1] | 5.8 | [3.3, 10.2] | 7.0 | [3.6, 13.6] |
| It is a good teaching tool | 4.7 | [1.9, 11.4] | 4.3 | [1.5, 11.8] | 5.2 | [2.5, 10.5] | 4.3 | [2.0, 9.3] |
Note. OR = odds ratio; 95% CI = 95% confidence interval.
Participants' missing income information were excluded from the multivariate analysis (missing =7 for intention and missing = 9 for self-efficacy).
Adjusted for age, gender, education, ethnicity, household income, access to health care, English proficiency, and proportion of life in the United States.
The associations were stratified by level of education, income, and length of stay in the United States. After excluding participants in control arm, who did not read photonovel or did not respond to photonovel evaluation, who already had hepatitis B screening or already infected/vaccinated, and who did not answer to the intention question, 235 participants were included in the analysis. Due to the small sample size in some cells, we measured unadjusted associations between the evaluation of photonovel and intention to have a hepatitis B screening in the next 5 months. Participants with lower income (annual household income <$50,000), lower education (high school or less), and shorter length of stay (had lived in the United States <14 years) demonstrated a stronger association between evaluation of photonovel and intention to have the screening than their corresponding counterparts (see Table 5). Because of smaller sample size, confidence intervals tended to be wide; however, most of the associations were statistically significant or marginally significant.
Table 5. Association Between Evaluation of the Photonovel and Intention to Have a Hepatitis B Screening Stratified by Income, Education, and Years of Living in the United States (n = 235).
| Unadjusted | Annual Household Income <$50,000 (n = 125)a | Annual Household Income ≥$50,000 (n = 103)a | ≤High School Education (n = 79) | >High School Education (n = 156) | Lived in the United States <14 Years (n = 119) | Lived in the United States ≥14 Years (n = 116) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Information is helpful | 3.9 | [1.7, 9.3] | 5.1 | [1.4, 18.7] | 2.5 | [0.7, 8.2] | 4.7 | [0.9, 24.0] | 3.6 | [1.3, 9.9] | 6.5 | [1.9, 21.8] | 2.2 | [0.6, 8.2] |
| Story is written by who someone knows the community | 2.2 | [1.0, 4.4] | 3.4 | [1.2, 9.1] | 1.3 | [0.4, 4.3] | 4.3 | [1.3, 15.0] | 1.8 | [0.7, 4.5] | 2.5 | [0.9, 7.5] | 2.1 | [0.8, 5.6] |
| It is a good teaching tool | 4.7 | [1.9, 11.4] | 4.7 | [1.1, 19.1] | 3 | [0.9, 10.1] | 4.7 | [0.9, 24.0] | 4.7 | [1.6, 13.7] | 5.6 | [1.5, 21.6] | 4.3 | [1.3, 14.5] |
Note. OR = odds ratio; 95% CI = 95% confidence interval.
Participants' missing income information were excluded from the multivariate analysis (missing = 7).
In the stratified analysis of self-efficacy, because of small sample size (n = 322), confidence intervals tended to be wide, but all the associations were statistically significant. Those who had lower income and education were more likely to have a stronger association between evaluation of photonovel and self-efficacy in having the screening than their corresponding counterparts, except “story is written by someone knows the community”. However, those who lived in the United States for 14 years or more were more likely than their counterparts to report having self-efficacy for the screening. Trends of associations were less consistent in self-efficacy compared with intention (see Table 6).
Table 6. Association Between Evaluation of the Photonovel and Self-Efficacy in Having a Hepatitis B Screening by Income, Education, and Years of Living in the United States (n = 322).
| Unadjusted | Annual Household Income <$50,000 (n = 167)a | Annual Household Income ≥$50,000 (n = 146)a | ≤High School Education (n = 115) | >High School Education (n = 207) | Lived in the United States <14 Years (n = 159) | Lived in the United States ≥14 Years (n = 163) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Information is helpful | 7.4 | [3.7, 15.0] | 10.2 | [3.5, 29.2] | 5.9 | [2.2, 16.3] | 13.4 | [3.8, 47.2] | 5.5 | [2.3, 13.0] | 5.8 | [2.1, 15.9] | 9.5 | [3.5, 25.6] |
| Story is written by someone who knows the community | 5.8 | [3.3, 10.2] | 4.3 | [2.0, 9.3] | 9.1 | [3.7, 22.5] | 4.8 | [1.9, 11.8] | 7.5 | [3.6, 15.9] | 5 | [2.2, 11.3] | 7.2 | [3.3, 15.8] |
| It is a good teaching tool | 5.2 | [2.5, 10.5] | 5.2 | [1.8, 15.1] | 4.7 | [1.7, 13.2] | 6.6 | [1.9, 22.2] | 4.6 | [1.9, 11.0] | 3.9 | [1.4, 10.8] | 6.8 | [2.5, 18.8] |
Note. OR = odds ratio; 95% CI = 95% confidence interval.
Participants' missing income information were excluded from the multivariate analysis (missing = 9).
Discussion
Results from the current study suggest that the three culturally appropriate photonovels were well received by Chinese, Korean, and Vietnamese Americans in Maryland. The majority thought that the photonovels provided helpful hepatitis B and liver cancer information, were culturally relevant, and easy to understand. In general, they agreed that the photonovel was a good teaching tool. The Vietnamese group viewed the photonovel more favorably than Chinese and Korean groups. We also found that those who rated the photonovel more favorably were more likely to have self-efficacy and intention to have a hepatitis B screening in the next 5 months. Our results further suggest that our photonovels worked better among those who had lower income or lower educational attainment.
To the best of our knowledge, this is the first study to develop a culturally appropriate photonovel for hepatitis B and liver cancer prevention and evaluate its effectiveness among Asian Americans. Previous intervention programs that aimed to increase knowledge and awareness of hepatitis B screening and vaccination have used face-to-face individual education (Taylor et al., 2009), culturally appropriate lectures with or without free screening (Hsu et al., 2007; Taylor et al., 2008), complete screening and vaccination programs (i.e., 3 For Life; Chang, Sue, Zola, & So, 2009; Hutton, Tan, So, & Brandeau, 2007), culturally integrated materials in a faith-based program (Juon et al., 2008), and community coalition with mass media campaign (i.e., San Francisco Hep B Free, the Jade Ribbon Campaign; Bailey et al., 2011; Chao, Chang, Le, et al., 2009). Very few of these programs had developed and tested culturally appropriate educational materials that could be replicated and used for future education. Together with screening, vaccination and treatment services, hepatitis B education is important part of a cost-effective hepatitis B prevention program targeting Asian Americans (Hutton et al., 2007). Promising results from our study suggest that culturally appropriate photonovels may be used alone or in combination with other hepatitis B prevention programs in various Asian American communities to improve knowledge about hepatitis B and increase hepatitis B screening and vaccination.
Previous studies have recommended using photonovels to approach immigrant populations for different health outcomes (Nimmon, 2007; Quinn et al., 2006). Our study confirmed that culturally appropriate photonovels were effective in increasing self-efficacy and intention to have a hepatitis B screening among multiple Asian American groups. Community-based participatory research strategies, such as storyline developed by people from each ethnic group, having community people playing actors and actresses, using community settings (i.e., nail salon), having stories in both Asian languages and English, and rich community input through community advisory board meetings, enabled our photonovels to have high cultural relevance, and this might partially explain the effectiveness observed in the study and positive feedback from our participants. For example, in the open-ended question in the process evaluation, one participant wrote “This photonovel gave me good information about hepatitis B testing and risk. The story is realistic.” Readers might see themselves in the photonovel story and feel ownership, which is a major benefit of the photonovel format (Dick et al., 1996; Roter et al., 2006). Nimmon (2007), who developed a photonovel for ESL (English as second language)–speaking women, also emphasized the involvement of participants to increase health literacy. Vietnamese participants reported more favorable evaluation of the photonovel overall and this may be due to their relatively low screening or vaccination rate at baseline compared with Chinese and Koreans in our sample, indicating less previous exposure to and more need for hepatitis B prevention knowledge (Strong et al., in press). Therefore, they might have been more interested in sharing the information with others or find the information more valuable.
Furthermore, in our study, Vietnamese participants were less likely to be highly educated than Chinese or Korean participants, and therefore, our photonovel with many pictures and less text might have worked well for them. Other studies have found that picture-based instructions promote better understanding for people with low literacy and low numeracy (Hawley et al., 2008; Houts, Witmer, Egeth, Loscalzo, & Zabora, 2001; Kripalani et al., 2007) and for people with limited English proficiency (Cabassa et al., 2012; Cabrera et al., 2002).
Though previous studies have used photonovels in vulnerable populations, few had conducted quantitative analysis to evaluate the effectiveness of the products (Nimmon, 2007; Quinn et al., 2006; Roter et al., 2006; Rudd & Comings, 1994). One important finding from our study was that our photonovels were more effective among Asian Americans with lower socioeconomic status and shorter length of residence in the United States. We used several strategies identified by a formative study as key factors to help the readers understand health educational materials (Estey, 1991) including the readable contents presented in plain language, Q&A at the end of the photonovel to summarize key facts and interact with readers, and use of lots of pictures instead of text in our photonovels. The evaluation of the photonovel confirmed that the understandability level of the contents was appropriate for our target population, and it supports the previous finding that plain language may be a key part of the solution to increase health literacy in people with low health literacy (Stableford & Mettger, 2007). This might explain the more favorable results observed among participants of low socioeconomic status in our study.
It is important to note that the current study has several limitations and caution is needed when interpreting our results. First, part of our data collection method for process evaluation was different from others: majority of our participants mailed back their responses (80.7%), but 18.8% responded by phone, and 0.5% by e-mail. The results may be different between phone interviews and mail responses due to desirability bias; however, we do not think less than 20% influenced our findings in a major way. Second, given that our target population was a hard-to-reach population group, we did not use probability sampling to recruit participants. Instead, participants were recruited through community organizations and other community channels in Maryland to maximize the outreach of the study. Therefore, the sample in our study might not represent all Asian Americans living in Maryland, and our results may not be generalizable to other Asian populations in the United States or those with different socioeconomic status. Third, the photonovel was used as one component of a hepatitis B prevention program and the photonovel was distributed to participants after a culturally appropriate presentation. Information learned in the presentation might encourage participants to read the photonovel and help them to appreciate the contents more than they would have if they had not been previously exposed to other components of the intervention program.
Implications for Practice
Despite its limitations, our photonovel has been demonstrated to have useful information, to be easily understandable, and culturally relevant, for use as hepatitis B education material for Asian Americans. Also, an association was observed between exposure to photonovel and self- efficacy/intention among participants to have a hepatitis B screening in near future, particularly among those who had lower socioeconomic status. Our study is among the first to show that the photonovel format may be a good health communication and educational method for Asian Americans to prevent hepatitis B infection and liver cancer. Inclusion of multiple Asian subgroups in Maryland and use of community-based participatory research methods throughout the development phase and intervention phase of the study also made our study unique compared with other similar studies. Findings of our study may provide useful information for other hepatitis B prevention programs targeting immigrant populations in the use of culturally relevant educational materials. Photonovels developed by our research project have been made available on our project website and can be used for hepatitis B prevention education among Chinese, Korean, and Vietnamese Americans living in other areas of the United States.
Acknowledgments
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article:
This project, Asian American Liver Cancer Education Program, was funded by the National Cancer Institute (R25CA129042).
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Bailey MB, Shiau R, Zola J, Fernyak SE, Fang T, So SK, Chang ET. San Francisco hep B free: A grassroots community coalition to prevent hepatitis B and liver cancer. Journal of Community Health. 2011;36:538–551. doi: 10.1007/s10900-010-9339-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabassa LJ, Molina GB, Baron M. Depression fotonovela: Development of a depression literacy tool for Latinos with limited English proficiency. Health Promotion Practice. 2012;13:747–754. doi: 10.1177/1524839910367578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabrera DM, Morisky DE, Chin S. Development of a tuberculosis education booklet for Latino immigrant patients. Patient Education and Counseling. 2002;46:117–124. doi: 10.1016/s0738-3991(01)00156-2. [DOI] [PubMed] [Google Scholar]
- Chang ET, Nguyen BH, So SK. Attitudes toward hepatitis B and liver cancer prevention among Chinese Americans in the San Francisco Bay Area, California. Asian Pacific Journal of Cancer Prevention. 2008;9:605–613. [PubMed] [Google Scholar]
- Chang ET, Sue E, Zola J, So SK. 3 For Life: A model pilot program to prevent hepatitis B virus infection and liver cancer in Asian and Pacific Islander Americans. American Journal of Health Promotion. 2009;23:176–181. doi: 10.4278/ajhp.071025115. [DOI] [PubMed] [Google Scholar]
- Chao SD, Chang ET, Le PV, Prapong W, Kiernan M, So SK. The Jade Ribbon Campaign: A model program for community outreach and education to prevent liver cancer in Asian Americans. Journal of Immigrant and Minority Health. 2009;11:281–290. doi: 10.1007/s10903-007-9094-2. [DOI] [PubMed] [Google Scholar]
- Chao SD, Chang ET, So SK. Eliminating the threat of chronic hepatitis B in the Asian and Pacific Islander community: A call to action. Asian Pacific Journal of Cancer Prevention. 2009;10:507–512. [PubMed] [Google Scholar]
- Chen MS., Jr Cancer health disparities among Asian Americans: What we do and what we need to do. Cancer. 2005;104:2895–2902. doi: 10.1002/cncr.21501. [DOI] [PubMed] [Google Scholar]
- Coronado GD, Taylor VM, Tu SP, Yasui Y, Acorda E, Woodall E, Hislop TG. Correlates of hepatitis B testing among Chinese Americans. Journal of Community Health. 2007;32:379–390. doi: 10.1007/s10900-007-9060-x. [DOI] [PubMed] [Google Scholar]
- Dick J, Van der Walt H, Hoogendoorn L, Tobias B. Development of a health education booklet to enhance adherence to tuberculosis treatment. Tubercle and Lung Disease. 1996;77:173–177. doi: 10.1016/s0962-8479(96)90034-9. [DOI] [PubMed] [Google Scholar]
- Estey AL. Evaluating educational materials for patients. Journal of Nursing Staff Development. 1991;7:290–291. [PubMed] [Google Scholar]
- Fang CY, Ma GX, Tan Y, Chi N. A multifaceted intervention to increase cervical cancer screening among underserved Korean women. Cancer Epidemiology, Biomarkers & Prevention. 2007;16:1298–1302. doi: 10.1158/1055-9965.EPI-07-0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. San Francisco, CA: Jossey-Bass; 2008. [Google Scholar]
- Hawley ST, Zikmund-Fisher B, Ubel P, Jancovic A, Lucas T, Fagerlin A. The impact of the format of graphical presentation on health-related knowledge and treatment choices. Patient Education and Counseling. 2008;73:448–455. doi: 10.1016/j.pec.2008.07.023. [DOI] [PubMed] [Google Scholar]
- Houts PS, Witmer JT, Egeth HE, Loscalzo MJ, Zabora JR. Using pictographs to enhance recall of spoken medical instructions II. Patient Education and Counseling. 2001;43:231–242. doi: 10.1016/s0738-3991(00)00171-3. [DOI] [PubMed] [Google Scholar]
- Hsu CE, Liu LC, Juon HS, Chiu YW, Bawa J, Tillman U, Wang M. Reducing liver cancer disparities: A community-based hepatitis-B prevention program for Asian-American communities. Journal of the National Medical Association. 2007;99:900–907. [PMC free article] [PubMed] [Google Scholar]
- Hu KQ. Hepatitis B virus (HBV) infection in Asian and Pacific Islander Americans (APIAs): How can we do better for this special population? American Journal of Gastroenterology. 2008;103:1824–1833. doi: 10.1111/j.1572-0241.2008.01878.x. [DOI] [PubMed] [Google Scholar]
- Hutton DW, Tan D, So SK, Brandeau ML. Cost-effectiveness of screening and vaccinating Asian and Pacific Islander adults for hepatitis B. Annals of Internal Medicine. 2007;147:460–469. doi: 10.7326/0003-4819-147-7-200710020-00004. [DOI] [PubMed] [Google Scholar]
- Juon HS, Strong C, Oh TH, Castillo T, Tsai G, Oh LD. Public health model for prevention of liver cancer among Asian Americans. Journal of Community Health. 2008;33:199–205. doi: 10.1007/s10900-008-9091-y. [DOI] [PubMed] [Google Scholar]
- Kreps GL, Sparks L. Meeting the health literacy needs of immigrant populations. Patient Education and Counseling. 2008;71:328–332. doi: 10.1016/j.pec.2008.03.001. [DOI] [PubMed] [Google Scholar]
- Kripalani S, Robertson R, Love-Ghaffari MH, Henderson LE, Praska J, Strawder A, Jacobson TA. Development of an illustrated medication schedule as a low-literacy patient education tool. Patient Education and Counseling. 2007;66:368–377. doi: 10.1016/j.pec.2007.01.020. [DOI] [PubMed] [Google Scholar]
- Ma GX, Fang CY, Shive SE, Toubbeh J, Tan Y, Siu P. Risk perceptions and barriers to hepatitis B screening and vaccination among Vietnamese immigrants. Journal of Immigrant and Minority Health. 2007;9:213–220. doi: 10.1007/s10903-006-9028-4. [DOI] [PubMed] [Google Scholar]
- Ma GX, Shive SE, Fang CY, Feng Z, Parameswaran L, Pham A, Khanh C. Knowledge, attitudes, and behaviors of hepatitis B screening and vaccination and liver cancer risks among Vietnamese Americans. Journal of Health Care for the Poor and Underserved. 2007;18:62–73. doi: 10.1353/hpu.2007.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma GX, Shive SE, Toubbeh JI, Tan Y, Wu D. Knowledge, attitudes, and behaviors of Chinese hepatitis B screening and vaccination. American Journal of Health Behavior. 2008;32:178–187. doi: 10.5555/ajhb.2008.32.2.178. [DOI] [PubMed] [Google Scholar]
- Nguyen GT, Bowman MA. Culture, language, and health literacy: Communicating about health with Asians and Pacific Islanders. Family Medicine. 2007;39:208–210. [PubMed] [Google Scholar]
- Nguyen TT, McPhee SJ, Stewart S, Gildengorin G, Zhang L, Wong C, Chen MS., Jr Factors associated with hepatitis B testing among Vietnamese Americans. Journal of General Internal Medicine. 2010;25:694–700. doi: 10.1007/s11606-010-1285-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen TT, Taylor V, Chen MS, Jr, Bastani R, Maxwell AE, McPhee SJ. Hepatitis B awareness, knowledge, and screening among Asian Americans. Journal of Cancer Education. 2007;22:266–272. doi: 10.1007/BF03174128. [DOI] [PubMed] [Google Scholar]
- Nimmon LE. Within the eyes of the people: Using a photonovel as a consciousness-raising health literacy tool with ESL-speaking immigrant women. Canadian Journal of Public Health. 2007;98:337–340. doi: 10.1007/BF03405414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Minority Health. National hepatitis B initiative for Asian Americans and Pacific Islanders. 2008 Retrieved from http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlid=190.
- Philbin MM, Erby LAH, Lee S, Joun HS. Hepatitis B and liver cancer among three Asian American sub-groups: A focus group inquiry. Journal of Immigrant and Minority Health. 2012;14:858–868. doi: 10.1007/s10903-011-9523-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn GP, Hauser K, Bell-Ellison BA, Rodriguez NY, Frias JL. Promoting pre-conceptional use of folic acid to Hispanic women: A social marketing approach. Maternal and Child Health Journal. 2006;10:403–412. doi: 10.1007/s10995-006-0074-2. [DOI] [PubMed] [Google Scholar]
- Roter DL, Rudd RE, Keogh J, Robinson B. Worker produced health education material for the construction trades, 1986-87. International Quarterly of Community Health Education. 2006;27:231–243. doi: 10.2190/IQ.27.3.d. [DOI] [PubMed] [Google Scholar]
- Rudd RE, Comings JP. Learner developed materials: An empowering product. Health Education Quarterly. 1994;21:313–327. doi: 10.1177/109019819402100304. [DOI] [PubMed] [Google Scholar]
- Stableford S, Mettger W. Plain language: A strategic response to the health literacy challenge. Journal of Public Health Policy. 2007;28:71–93. doi: 10.1057/palgrave.jphp.3200102. [DOI] [PubMed] [Google Scholar]
- Stewart SL, Rakowski W, Pasick RJ. Behavioral constructs and mammography in five ethnic groups. Health Education & Behavior. 2009;36(5 Suppl):36S–54S. doi: 10.1177/1090198109338918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong C, Lee S, Chung T, Chen L, Tran H, Juon HS. Prevalence and factors associated with hepatitis B screening and vaccination among Asian Americans. Journal of Community Health. doi: 10.1007/s10900-012-9541-4. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Coronado G, Acorda E, Teh C, Tu SP, Yasui Y, Hislop TG. Development of an ESL curriculum to educate Chinese immigrants about hepatitis B. Journal of Community Health. 2008;33:217–224. doi: 10.1007/s10900-008-9084-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Hislop TG, Tu SP, Teh C, Acorda E, Yip MP, Yasui Y. Evaluation of a hepatitis B lay health worker intervention for Chinese Americans and Canadians. Journal of Community Health. 2009;34:165–172. doi: 10.1007/s10900-008-9138-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran TT. Understanding cultural barriers in hepatitis B virus infection. Cleveland Clinic Journal of Medicine. 2009;76(Suppl 3):S10–S13. doi: 10.3949/ccjm.76.s3.03. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (n.d.) Selected population profile in the United States: Asian alone or in combination with one or more other races. 2007-2009 American Community Survey 3-year estimates. Retrieved from http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_10_1YR_S0201&prodType=table.
- Velle R, Yamada A, Matiella A. Fotonovelas: A healthy literacy tool for educating Latino older adults about dementia. Clinical Gerontologist. 2006;30:71–88. [Google Scholar]
- World Health Organization. Prevention of liver cancer: Report of a WHO meeting. Vol. 691. Geneva, Switzerland: Author; 1983. [Google Scholar]
- Wu CA, Lin SY, So SK, Chang ET. Hepatitis B and liver cancer knowledge and preventive practices among Asian Americans in the San Francisco Bay Area, California. Asian Pacific Journal of Cancer Prevention. 2007;8:127–134. [PubMed] [Google Scholar]
- Yu MC, Yuan JM, Govindarajan S, Ross RK. Epidemiology of hepatocellular carcinoma. Canadian Journal of Gastroenterology. 2000;14:703–709. doi: 10.1155/2000/371801. [DOI] [PubMed] [Google Scholar]


