Abstract
The factors that influence caregiver coping mechanism preferences after a child’s diagnosis with cancer are not fully understood. This study examines the relationship between caregivers’ socio-demographic characteristics and the coping strategies they use to adapt to childhood cancer. Sixty caregivers of pediatric cancer patients completed a socio-demographic questionnaire, the Family Environment Scale, and the COPE inventory. There were no significant differences in family environment by income or education. Caregiver educational attainment was positively associated with use of planning and active coping styles, while income was not associated with caregiver coping style. Mothers were more likely than fathers to use active coping, instrumental support, religious coping, and emotional support. Men with lower education engaged in greater substance use coping and lower planning. The findings show that educational attainment and caregiver gender influence caregiver coping styles following a pediatric cancer diagnosis and suggest that educational attainment rather than financial resources drive the association between SES and coping. Programs that address educational gaps and teach caregivers planning and active coping skills may be beneficial for parents with lower educational attainment, particularly men.
Keywords: Socioeconomic status, Coping, Family environment, Gender, Cancer
Introduction
Cancer in children presents a great shock to a family system, and understanding how families adapt to this stress has been a focus of research in oncology, nursing, and the social sciences. Parental coping strategies are important variables in family adaptation to pediatric cancer (Frank, Blount, & Brown, 1997; Gold, Treadwell, Weissman, & Vichinsky, 2011; Hoekstra-Weebers, Jaspers, Kamps, & Klip, 1999; Hoekstra-Weebers, Wijnberb-Williams, Jaspers, Kamps, & van de Wiel, 2011; Klassen et al., 2011; Long & Marsland, 2011). The factors that influence which coping strategies parents use to deal with childhood cancer are, however, incompletely understood.
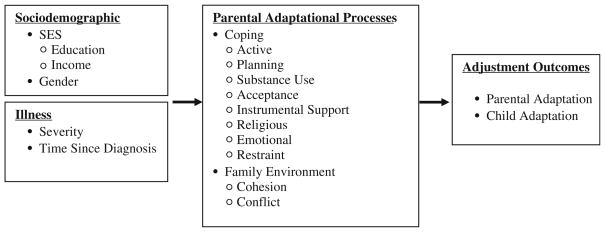
This paper examines the influence of parent and family characteristics on parents’ use of various coping mechanisms after a child is diagnosed with cancer. Thompson’s transactional stress and coping model (Thompson, Gus-tafson, Hamlett, & Spock, 1992), which draws from an ecological-systems theory, was used as an organizing framework for this work. This model views a childhood illness as a potential stressor to which the family system must adapt. Parental and child adjustment is influenced by the interaction of biomedical, developmental, and psychosocial factors. Illness parameters, such as the severity and duration of illness, and socio-demographic parameters, such as socioeconomic status and gender, are proposed to influence parental adaptational processes (i.e., methods of coping, family functioning, and cognitive processing), which in turn influence parental and child adaptation. While there is a broad literature focusing on how parental adaptational processes influence parental and child adjustment, in this paper we are interested in examining socio-demographic predictors of parental adaptational processes. These factors of interest are presented in Fig. 1.
Fig. 1.
Predictors of parental adaptational processes, adapted from Thompson’s Stress and Coping Model of Adjustment (Thompson et al., 1992)
This paper builds upon the extensive literature documenting the role parental coping mechanism plays in shaping family adaptation to pediatric cancer and examines the factors that shape the coping styles parents use after a child is diagnosed with cancer (Ahnis et al., 2012; Lopez-Olivo et al., 2011; Paredes, Pereira, Simoes, & Canavarro, 2012). Coping is a broad concept which encompasses the strategies a person uses to manage stressful life events (Wenninger et al., 2012). When a child is diagnosed with cancer, parents engage in cognitive and behavioral strategies as ways to manage the stress associated with their child’s illness (Folkman, Lazarus, Dunkel-Schetter, DeLongis, & Gruen, 1986). Several models have been developed to categorize individuals’ coping reactions to stress. The approach-avoidance model categorizes individuals as either confronting their stress or retreating from it (Rother & Cohen, 1986). Other models categorize coping reactions as emotion-focused and problem-focused coping strategies (Folkman et al., 1986). The coping strategies parents use to cope with pediatric cancer have been identified as important influences in families’ adaptation to pediatric cancer (Long & Mars-land, 2011). Parental coping style after a child’s cancer diagnosis is associated with levels of parental psychological distress (Hoekstra-Weebers et al., 1999, 2011), parental health-related quality of life (Klassen et al., 2011), child well-being (Frank et al., 1997), and psychosocial outcomes of siblings (Gold et al., 2011). However, the factors that influence the degree to which parents employ various coping mechanisms are not fully understood (Martin et al., 2011).
The characteristics of the family environment also influ-ence adjustment to pediatric cancer (Ashida et al., 2009; Jobe-Shields et al. 2009). The functioning of the family may influence how family members are able to adjust to the emotional, logistical, and interpersonal demands associated with pediatric cancer (Long & Marsland, 2011). High levels of family cohesion and expressiveness are associated with positive psychosocial outcomes, while higher family conflict is associated with negative outcomes (Ashida et al., 2009; Jobe-Shields et al., 2009). While research documents the importance of the family environment in shaping adaptation to stressful life events, less is known about the characteristics that influence the levels of cohesion or conflict in a family.
The family environment and the coping mechanisms parents use to adapt to pediatric cancer may be shaped by parental socio-demographic characteristics. Research examining caregiver coping in reaction to pediatric health issues more broadly has found differences by socio-economic status (SES). SES is a multi-faceted construct which encompasses an individual’s income, education, assets, and occupation (Braveman et al., 2005; Herd, Goesling, & House, 2007; Schnittker, 2004). One study of parents of children awaiting a kidney transplant found that parents with lower income were more likely to use avoidance coping (Zelikovsky, Schast, & Jean-Francois, 2007). Another study of caregivers of youth with spinal cord injury found that caregiver education was inversely associated with use of denial as a coping strategy (Dasch, Russell, Kelly, Gorz-kowski, & Mulcahey, 2011). SES has also been found to be a significant predictor of parental adjustment for parents of children with cancer (Grootenhuis & Last, 1997), but the relationship between SES and specific coping strategies has not been well studied. Mothers of children with cancer from low SES backgrounds have reported higher levels of emotion-focused coping, which was related to worse adjustment (Baskin, Forehand, & Saylor, 1985). For mothers of long-term survivors of childhood leukemia, SES and previous coping were positively correlated with the adequacy of mothers’ coping 10 years post treatment (Kupst et al., 1995). Further, in that same study, only SES was related to good (vs. poor) family coping at 10 years post treatment, suggesting that SES is an important factor in long-term family adjustment (Kupst et al., 1995).
Research also suggests that gender influences both the experience of stress following a child’s cancer diagnosis as well as parents’ coping responses (Enskar, Hamrin, Carlson, & von Essen, 2011; Hill, Higgins, Dempster, & McCarthy, 2009; Palmer et al., 2011; Rodriguez et al., 2012). Mothers have been found to experience more stressors and distress associated with their child’s cancer diagnosis than fathers (Pai et al., 2007; Rodriguez et al., 2012; Yeh, 2002). Mothers and fathers also experience differences in role expectations related to their child’s care, which have been found to shape the coping reactions of parents (Chesler & Parry, 2001; Goldbeck, 2001).
This paper builds upon previous research which documents the role of the family environment and parental coping strategies in shaping adaptation to pediatric cancer and examines the influence of parental socio-demographic characteristics in shaping these processes (Frank et al., 1997; Gold et al., 2011; Hoekstra-Weebers et al., 1999, 2011; Klassen et al., 2011; Long & Marsland, 2011). We hypothesized that caregiver coping would differ by parental income and education. Specifically, we examined differences in the active, problem-focused domains and expected that care-givers with higher income and education would report higher levels of active, planning, and instrumental support than caregivers with lower income and education. We also expected that gender influenced caregiver coping after a pediatric cancer diagnosis, and sought to gather exploratory data on the influence of caregiver gender on coping strategy preferences. Finally, we examined the association between caregivers’ income and levels of education with family environment. Specifically, we hypothesized that caregivers with higher income and education would report higher levels of cohesion and lower levels of family conflict than care-givers with lower income and education. To evaluate these hypotheses, we collected survey data of socio-demographic characteristics, family environment, and caregiver coping from sixty caregivers of pediatric cancer patients.
Method
Participants and Recruitment
Data come from a larger mixed-methods study of parents of children with cancer (for description see Gage, 2013). Caregivers were recruited through the Pediatric Oncology Clinics at an NCI-designated comprehensive cancer center and a children’s hospital in the Northeastern US. Any care-giver of a child diagnosed with cancer was eligible for participation in the study. Data were collected from August 2009 to May 2011. We partnered with individuals at the recruitment site who introduced the study to parents. Parents either signed a contact consent form allowing the recruiting agency to release their information, or were told how to directly let the study team know of their interest in participating. Members of the study team contacted each parent and scheduled a time to administer the survey. Eighty-two caregivers were approached and asked to participate in the study. Six of these potential respondents were not enrolled due to scheduling difficulties or declined to participate. Seventy-six caregivers (93 % of those agreeing to discuss the study with researchers) were enrolled in the study. In the case of families in which both partners participated in the study, individual appointments were scheduled with each respondent. All respondents completed the surveys separately, without their partner in the room.
Seventy-six caregivers (45 mothers, 28 fathers, 3 aunts) of pediatric cancer patients participated in the first phase of research, which included the first survey and qualitative interview. Sixty caregivers (78.9 %) completed both the original and second surveys. Of these 60 participants, 23 families had two caregivers participate (totaling 46 respondents or 76.7 % of our sample), and 20 families had one caregiver participate. Child and caregiver characteristics for the sample of respondents who completed both the initial and second surveys are presented in Tables 1 and 2. Sixty-three percent of the adult caregiver respondents were women and 37 % were men. With respect to child gender, 58 % were girls and 42 % were boys. Fifteen percent of the adult caregiver sample was non-Hispanic black, while the majority of respondents (85 %) were non-Hispanic white.
Table 1.
Demographic characteristics of caregivers
| % (n) or M ± SD N = 60 |
|
|---|---|
| Gender | |
| Women | 63 % (38) |
| Men | 37 % (22) |
| Total | 100 % (60) |
| Race/ethnicity | |
| Non-Hispanic White | 85 % (51) |
| Non-Hispanic Black | 15 % (9) |
| Total | 100 % (60) |
| Marital status | |
| Never married | 12 % (7) |
| Married | 75 % (45) |
| Divorced | 13 % (8) |
| Total | 100 % (60) |
| Education | |
| Less than high school diploma | 2 % (1) |
| High school diploma or equivalency (GED) | 37 % (22) |
| Associate’s degree (junior college) | 8 % (5) |
| Bachelor’s degree | 25 % (15) |
| Master’s degree | 23 % (14) |
| Doctorate or advanced professional degree | 2 % (1) |
| No Response | 3 % (2) |
| Total | 100 % (60) |
| Total household income | |
| $5,000 through $11,999 | 8 % (5) |
| $12,000 through $15,999 | 2 % (1) |
| $16,000 through $24,999 | 12 % (7) |
| $25,000 through $34,999 | 2 % (1) |
| $35,000 through $49,999 | 10 % (6) |
| $50,000 through $74,999 | 16 % (10) |
| $75,000 through $99,999 | 15 % (9) |
| $100,000 and greater | 31 % (19) |
| Don’t know/No response | 4 % (2) |
| Total | 100 % (60) |
| Percent of Federal Poverty Guideline | |
| Below the Federal Poverty Guideline | 18 % (11) |
| 100 % of the Federal Poverty Guideline | 10 % (6) |
| 200 % of the Federal Poverty Guideline | 8 % (5) |
| 300 % of the Federal Poverty Guideline or more | 59 % (35) |
| Don’t know/no response | 5 % (3) |
| Total | 100 % (60) |
Table 2.
Characteristics of pediatric cancer patients
| % (n) or M ± SD | |
|---|---|
| Gender | |
| Male | 42 % (25) |
| Female | 58 % (35) |
| Total | 100 % (60) |
| Age at diagnosis (M ± SD) | 7.9 ± 4.7 years |
| Current age (M ± SD) | 10.2 ± 4.8 years |
| Time since diagnosis (M ± SD) | 2.3 ± 4.3 years |
Measures
Socio-demographic Measures
Demographic and SES measures were captured using the MacArthur Foundation Research Network on Socioeconomic Status and Health socio-demographic questionnaire (Singh-Manoux, Adler, & Marmot, 2003; Singh-Manoux, Marmot, & Adler, 2005). The MacArthur socio-demographic questionnaire includes fourteen items that measure subjective social status, educational attainment, occupational status, income, and assets. To capture educational attainment, we asked respondents, “What is the highest degree you earned?” Response options included: high school diploma or equivalency (GED), Associate’s degree (junior college), Bachelor’s degree, Master’s degree, Doctorate, Professional (MD, JD, DDS, etc.), other, and none of the above (less than high school). Total household income was measured by asking “Which of these categories best describes your total combined family income for the past 12 months? This should include income (before taxes) from all sources, wages, rent from properties, social security, disability and/or veteran’s benefits, unemployment benefits, workman’s compensation, help from relatives (including child payments and alimony), and so on.” Response items included: Less than $5,000, $5,000 through $11,999, $12,000 through $15,999, $16,000 through $24,999, $25,000 through $34,999, $35,000 through $49,999, $50,000 through $74,999, $75,000 through $99,999, $100,000 and greater, Don’t Know, and No Response. The MacArthur scale creates both the income and education variables as ordinal variables, not continuous. To capture household size, we asked “How many people are currently living in your household, including yourself?” Time since diagnosis was measured in years from parent report of the month and year of their child’s initial cancer diagnosis. This was subtracted from the month and year of study participation.
Caregiver Coping
Coping responses were measured using the 60-item COPE Inventory (Carver, Scheier, & Weintraub, 1989). The COPE has fifteen subscales; based on a review of the literature we focused on eight subscales: (1) active coping (e.g., “I concentrate my efforts on doing something about it” and “I keep myself from getting distracted by other thoughts or activities”), (2) planning (e.g., “I make a plan of action” and “I try to come up with a strategy about what to do”), (3) substance use, (e.g., “I use alcohol or drugs to make myself feel better” and “I try to lose myself for a while by drinking alcohol or taking drugs”), (4) acceptance (e.g., “I get used to the idea that it happened” and “I accept that this has happened and that it can’t be changed”), (5) use of instrumental social support (e.g., “I try to get advice from someone about what to do” and “I talk to someone to find out more about the situation”), (6) religious coping (e.g., “I put my trust in God” and “I seek God’s help”), (7) use of emotional social support (e.g., “I discuss my feelings with someone” and “I try to get emotional support from friends or relatives”), and (8) restraint (e.g., “I restrain myself from doing anything too quickly” and “I hold off doing anything about it until the situation permits”). These subscales demonstrated adequate internal reliability in the present sample, α = .69 to .97. The dispositional form of the questionnaire was used, in which respondents were given four response options, including “I usually don’t do this at all,” “I usually do this a little bit,” “I usually do this a medium amount,” and “I usually do this a lot.” Subscale scores could range from 4 to 16, with a high score indicating high use of the coping style.
Family Social Environment
The family social environment was captured using the well-established Family Environment Scale (FES; Moos & Moos, 1994; Ogburn et al., 2010; Pheula, Rhode, & Sch-mitz, 2011; Vachha & Adams, 2009). Each item has a true/ false response option. The FES has 10 subscales measuring three dimensions: Relationship, Personal Growth, and System Maintenance. In this study, we focused on the two most commonly examined relationship subscales—cohesion and conflict. The internal reliability of the cohesion subscale was low, Cronbach’s α = .54; however, we used this subscale because it has strong conceptual and empirical underpinnings (Moos, 1990). The conflict subscale demonstrated adequate internal reliability, α = .74. Sub-scale scores can range from 0 to 9.
Procedures
Study team members met caregivers at locations of the caregiver’s choice, including coffee shops, parents’ homes, or the hospital when their child was inpatient. The study was IRB-approved and participants signed a written informed consent. Each respondent completed a survey composed of the MacArthur socio-demographic survey and the FES, and then completed a qualitative interview. Detailed qualitative data collection procedures are described elsewhere (Gage, 2013). Participants were given a $50 gift card for their time and effort. Six months after their initial participation, respondents were mailed a second survey which consisted of the COPE inventory and questions regarding the child’s diagnosis. Respondents were asked to return their completed survey in a prepaid return envelope. Respondents who returned this second survey were mailed a $25 gift card.
Statistical Analysis
Given that SES is a multi-faceted construct, preliminary analyses examined the Spearman rho correlation between the components of SES that we measured—the variables degree earned and percent poverty line. To evaluate our hypotheses regarding the association of socio-demographic factors with caregiver coping and family environment, linear mixed models were conducted using SAS 9.2 PROC MIXED. A mixed model allows for incorporation of fixed and random effects (Brown & Prescott, 2006). This approach accounts for possible correlations between members of the same family. Variance components, comprised of the within- and between-family variance, were estimated using the Restricted Maximum Likelihood (REML) method. The Family–Family variance component was important to include to prevent bias in the hypothesis tests for fixed effects. Hypothesis tests for the fixed effects used the Kenward–Roger degrees of freedom adjustment procedure for small samples (Kenward & Roger, 1997). Missing data were assumed to be missing at random, meaning that missingness of a response can depend on other variables, but does not depend on the actual response that is reported as missing, e.g., due to embarrassment if one were to answer the question. Education (degree earned) and income data from the MacArthur socio-demographic survey used an ordinal scale. For use in mixed linear models, degree earned was dichotomized into less than a bachelor’s degree or bachelor’s degree and greater. Since the value of income is linked to how many individuals rely on the income, we converted income data to percent of the US federal poverty line, accounting for the number of family members in the household. We dichotomized percent poverty line as at or below the poverty line (≤100 % of the poverty line) compared with above the poverty line. We chose to use degree earned and percent poverty line as dichotomous variables for ease of interpretation in the models because of their ordinal scales. Cut points were chosen based on clinically meaningful differences between the two groups; that is, we believe that individuals with a bachelor’s degree or greater have meaningful differences in resources than those with less than a bachelor’s degree. Further, individuals at or below the poverty line also have different resources and challenges than those who have income above the poverty line. We also re-ran analyses with degree earned and income as ordinal variables (results not shown). The pattern of results did not change; therefore, we report results with education and income as dichotomized variables.
To address our first hypothesis, that caregivers’ with higher education and income levels would report greater levels of active, planning, and instrumental support coping strategies, we conducted linear mixed models separately for each outcome. For each coping strategy outcome, a full model with all potential socio-demographic predictors (i.e., degree earned, percent poverty line, gender, time since diagnosis, and whether the caregiver had a partner participate in the study) was run. Family number (to account for multiple caregivers within the same family) was included in each model as a random effect and all other terms were fixed effects. Least squares means (i.e., means after adjustment for all other model terms) are reported for statistically significant dichotomous variables. To address our second hypothesis that gender would be associated with coping strategies, we included gender in the linear mixed models. An interaction term for degree earned and gender was also included to examine whether gender differences were influenced by education, which we hypothesized was possible. To address our final hypotheses that caregivers with higher education and income would report higher family cohesion and lower family conflict, we conducted linear mixed models following the same procedures above with family cohesion and conflict as the outcomes.
Results
Preliminary Results
We first examined the association between the components of SES that we measured using a Spearman rho correlation. The dichotomized variables degree earned and percent poverty line were moderately related, rs = .42, p = .01. A correlation of this size does not pose problems of multi-collinearity in the models.
Socio-demographic Predictors of Caregiver Coping
Results of the linear mixed models are presented in Table 3. For caregivers’ use of active coping, degree earned and gender were significant predictors. After adjusting for other variables, those who had a bachelor’s degree or higher reported higher use of active coping than those who had less than a bachelor’s degree by 2.01 points, p < .01, and women reported higher use of active coping than men by 1.64 points, p = .03 (see Table 3).
Table 3.
Linear mixed models of socio-demographic predictors of caregiver coping
| Coping strategy | Predictor | Parameter estimate | Standard error | p |
|---|---|---|---|---|
| Active | Intercept | 12.54 | 0.72 | – |
| Degree earned | 1.48 | 0.89 | < .01 | |
| Percent poverty line | −0.57 | 0.87 | .52 | |
| Gender | 1.11 | 0.87 | .03 | |
| Time since diagnosis | 0.15 | 0.08 | .08 | |
| Caregiver paired | 0.37 | 0.87 | .67 | |
| Degree earned × gender | 1.07 | 1.45 | .47 | |
| Planning | Intercept | 13.18 | 0.67 | – |
| Degree earned | 0.46 | 0.81 | < .01 | |
| Percent poverty line | −0.57 | 0.81 | .48 | |
| Gender | 0.44 | 0.75 | < .01 | |
| Time since diagnosis | 0.13 | 0.08 | .12 | |
| Caregiver paired | 0.20 | 0.81 | .81 | |
| Degree earned × gender | 3.69 | 1.27 | < .01 | |
| Substance use | Intercept | 4.74 | 0.48 | – |
| Degree earned | −0.17 | 0.59 | .02 | |
| Percent poverty line | 0.80 | 0.53 | .14 | |
| Gender | −0.17 | 0.62 | .02 | |
| Time since diagnosis | −0.07 | 0.05 | .19 | |
| Caregiver paired | −0.13 | 0.57 | .81 | |
| Degree earned × gender | −1.96 | 0.97 | .05 | |
| Acceptance | Intercept | 13.59 | 0.82 | – |
| Degree earned | −0.03 | 0.99 | .93 | |
| Percent poverty line | 0.02 | 0.98 | .99 | |
| Gender | 1.21 | 0.89 | .08 | |
| Time since diagnosis | −0.05 | 0.10 | .61 | |
| Caregiver paired | 0.27 | 0.98 | .78 | |
| Degree earned × gender | 0.21 | 1.53 | .89 | |
| Instrumental | Intercept | 11.02 | 0.91 | – |
| Degree earned | −0.29 | 1.11 | .20 | |
| Percent poverty line | −0.36 | 1.08 | .74 | |
| Gender | 1.45 | 1.03 | < .01 | |
| Time since diagnosis | 0.17 | 0.11 | .13 | |
| Caregiver paired | 0.40 | 1.08 | .71 | |
| Degree earned × gender | 2.99 | 1.75 | .10 | |
| Religious | Intercept | 10.49 | 1.36 | – |
| Degree earned | 1.76 | 1.66 | .83 | |
| Percent poverty line | −1.64 | 1.68 | .34 | |
| Gender | 3.99 | 1.46 | .04 | |
| Time since diagnosis | 0.11 | 0.17 | .51 | |
| Caregiver paired | −1.03 | 1.64 | .54 | |
| Degree earned × gender | −2.95 | 2.55 | .26 | |
| Emotional support | Intercept | 11.46 | 0.99 | – |
| Degree earned | 0.04 | 1.22 | .22 | |
| Percent poverty line | 0.09 | 1.11 | .94 | |
| Gender | 1.46 | 1.28 | .01 | |
| Time since diagnosis | 0.02 | 0.11 | .89 | |
| Caregiver paired | 0.43 | 1.18 | .72 | |
| Degree earned × gender | 2.38 | 2.01 | .24 | |
| Restraint | Intercept | 8.30 | 0.75 | – |
| Degree earned | −0.05 | 0.92 | .70 | |
| Percent poverty line | −0.10 | 0.85 | .90 | |
| Gender | −0.34 | 0.96 | .99 | |
| Time since diagnosis | 0.03 | 0.01 | < .01 | |
| Caregiver paired | −1.43 | 0.91 | .12 | |
| Degree earned × gender | 0.69 | 1.51 | .65 |
Note Coping strategies measured using the COPE. Degree earned is coded as less than a bachelor’s degree = 0, bachelor’s degree or greater = 1; percent poverty line is coded as less than or equal to 100 % of the poverty line = 0, greater than 100 % of the poverty line = 1 based on income and number of family members in the household; gender is coded as male = 1, female = 2
With regard to caregivers’ use of planning, there was a significant interaction between degree earned and gender, so we interpret only the interaction rather than the main effects (see Table 3). Men that did not achieve a bachelor’s degree reported lower use of planning than men who achieved a bachelor’s degree or higher (by 4.14 points, p < .01) and than women with or without a bachelor’s degree (by 4.58 points, p < .01 and by 4.12 points, p < .01, respectively). Thus, education influenced men’s use of planning but not women’s.
For caregivers’ substance use coping, there was also a significant degree earned by gender interaction. Men that did not achieve a bachelor’s degree reported higher substance use coping than men with a bachelor’s degree or more (by 2.13 points, p < .01) and than women with or without a bachelor’s degree (by 2.29 points, p < .01, and by 2.12 points, p < .01, respectively). Thus, education influenced men’s substance use but not women’s.
For caregivers’ use of acceptance coping, there were no significant socio-demographic predictors.
For caregivers’ use of instrumental support, gender was the only statistically significant parameter. Women reported higher use of instrumental support than men by 2.95 points, p < .01.
With regard to caregivers’ use of religious coping, gender was the only statistically significant predictor (see Table 3). Women reported higher levels of religious coping than men by 2.52 points, p = .04.
For caregivers’ use of emotional support, gender again was the only statistically significant predictor in the model (see Table 3). Women reported higher use of seeking emotional support than men by 2.65 points, p = .01.
With regard to caregivers’ use of restraint coping, time since diagnosis was a statistically significant predictor, but this appears to be a negligible effect (see Table 3). Spe-cifically, for every 10 years from diagnosis, there was a 0.3 increase in restraint coping.
Socio-demographic Predictors of Family Cohesion and Conflict
Results of the linear mixed models found no statistically significant socio-demographic predictors (i.e., degree earned, percent poverty line, gender, time since diagnosis, and whether the caregiver had a partner participate in the study) of family cohesion or family conflict.
Discussion
Parental coping styles and the family environment influ-ence adaptation to serious pediatric illness (Ashida et al., 2009; Frank et al., 1997; Gold et al., 2011; Hoekstra-Weebers et al., 1999, 2011; Jobe-Shields et al., 2009; Klassen et al., 2011; Long & Marsland, 2011). In this study, we examined the influence of caregivers’ socio-demographic characteristics on caregivers’ coping styles and family environment after a pediatric cancer diagnosis.
Our first hypothesis that caregivers’ income and education would be associated with the use of specific coping mechanisms was partially supported. We found that care-giver educational attainment was associated with three dimensions of coping—active, planning, and substance use coping. Caregivers with a bachelor’s degree or more reported higher use of active coping. The associations between degree earned and planning and substance use coping depended on gender; men with lower educational attainment reported lower use of planning coping and higher substance use coping than men with higher education and than women (regardless of women’s educational attainment). This finding identifies men with lower education as a potentially vulnerable group who may benefit from additional resources related to coping.
Although education was associated with these strategies, contrary to our expectation, income was not associated with caregivers’ use of these problem-focused coping strategies. These findings suggest that there are important differences in the cultural capital attained through education and the financial resources derived from income. The relative importance of financial and educational resources likely vary throughout the disease process, with financial assets being especially important in shaping some aspects of illness experiences, and educational capital being an important influence for other aspects of the illness experience (Schnittker, 2004; Herd et al., 2007). These findings suggest that educational resources play an important role in shaping caregiver coping after a pediatric cancer diagnosis, which should be examined in future research. Educational attainment represents numerous dimensions of social standing that may shape use of different coping styles. An individual’s educational attainment may influence their health-related knowledge, interpersonal skills, problem-solving ability, social networks, social clout, and the characteristics of their occupations. These characteristics may shape individuals’ abilities and propensities to engage in certain coping behaviors. Future research should further examine these nuances of socioeconomic position and their influences on coping processes.
In addition to the interaction effects of gender and education on planning coping and substance use coping, we found main effects (with no interactions) of gender on the use of several coping styles. Women were more likely than men to use instrumental support, religious coping, and emotional support. These findings support previous research that has found gender differences in parental coping after a pediatric cancer diagnosis (Grootenhuis & Last, 1997). For example, mothers have been found to report more frequent and more effective coping compared with fathers (Goldbeck, 2001). Hoekstra-Weebers et al. (2011) found that mothers’ use of a passive reaction pattern and support seeking placed them at increased risk for psychological distress in the first year after their child’s cancer diagnosis, while fathers’ were at increased risk for distress when their coping styles included avoidance, a passive reaction pattern, expression of emotions, and decreased active problem focusing. Our findings contribute further insight into gender differences in caregiver coping, expanding our knowledge of how gender and education interact. In particular, men with lower levels of education may be at risk for higher substance use coping and lower planning coping. Our results also show that women were more likely to engage in several active coping behaviors such as seeking instrumental support. Women were also more likely to use religion and seek emotional support while coping with their child’s cancer diagnosis. These findings are consistent with other studies which have found that women and men perceive different role expectations related to their child’s cancer diagnosis (Chesler & Parry, 2001; Goldbeck, 2001) and that women are more likely to engage in support seeking after a pediatric cancer diagnosis (Hoekstra-Weelbers et al., 2011). It may be that women perceive more responsibility for the direct management of their child’s cancer care and are therefore more likely to engage in these active coping styles. Women may also be in established patterns of seeking emotional support from their networks and may feel more comfortable seeking this support after their child’s cancer diagnosis.
In our sample, time since diagnosis was positively associated with caregivers’ use of the restraint coping style. It may be that after the crisis of a child’s initial diagnosis passes, caregivers take more time to make decisions or act in a manner consistent with restraint coping. However, this effect was quite small in our sample and the clinical sig-nificance of this finding is uncertain.
Our hypothesis that caregivers with lower income and education would have greater family conflict and lower cohesion than caregivers with higher income and education was not supported. We did not find any significant differences by income or education for either family cohesion or conflict.
Limitations
There are several limitations to the present study. First, all data were collected in the same city in the Northeastern US and may not represent the experiences of families in other regions or settings. Second, the design does not permit comparison of this sample of caregivers of pediatric cancer patients to a general population of caregivers. It may be that these coping experiences are characteristic of the experiences of families more broadly and not related to the experience of caring for a child diagnosed with cancer. Third, the sample is small and not uniform. In an effort to include fathers’ experiences in the study, we attempted to recruit two caregivers in each family. As a result, two caregivers represent some families in the sample, and one caregiver represents other families. In addition, three of the caregivers in the sample are aunts. While these elements add richness to the data, they also introduce heterogeneity. Future research should attempt to recruit a greater number of pairs of parents to enable comparison of parent perspectives, but also to establish homogeneity in family representation across the sample. Future research should also examine these processes using a coping measure that is specifically designed to capture health-related coping. Since the COPE is a measure of general coping responses, we were not able to examine nuanced health-related coping behaviors in this study. Finally, although our model suggests that socio-demographic factors would be related to coping mechanisms, which in turn would relate to caregiver and child adaptation, our data do not allow these coping mechanisms to be linked to caregiver or child outcomes. Future research examining the relationship between SES, coping, and psychological and physical health outcomes would expand our understanding of these processes.
Conclusion
This study sought to examine the relationships between SES, caregiver coping, and family environment after a pediatric cancer diagnosis. Results indicate that educational attainment and gender influence how caregivers cope with childhood cancer. That is, caregivers with higher educational attainment engaged in higher use of active coping styles, and women engaged in higher use of active, instrumental support, emotional support, and religious coping styles. Men with low educational attainment reported lower use of planning and higher substance use coping than men with higher education and than women. While further research is needed to explore how these differences in coping responses impact family adaptation to pediatric cancer and health outcomes, these results have implications for clinical practice. Results show that mothers and fathers cope with their child’s cancer differently, and mothers are more likely to employ active coping strategies and seek social support. Fathers may benefit from tailored initiatives designed to meet the specific needs of men, particularly fathers who have less than a bachelor’s degree education. Our results also show that caregivers with lower educational attainment are less likely to use active coping strategies. Programs to address gaps in education, such as those that provide information about resources available, health care engagement, and strategies for navigating the health care system, may be beneficial for this sub-population of families. Problem-solving skills training might also be beneficial.
Acknowledgments
This research was supported by the National Institutes of Health, grants R21CA141165, R25CA114101 and R25CA10618. We would like to thank Martin Brecher, Deborah Erwin, Michael Farrell, James Marshall, Debra Street, Robert Wagmiller, Michael Zevon, Gary Morrow, and the anonymous reviewers for their extensive and helpful feedback throughout this project. This research would not have been possible without our dedicated research team, Christina Panagakis, Nikia Clark, Jessica Keaton, Brandee Aquilino, Kristen Fix and all of the families who generously participated in the study.
Contributor Information
Elizabeth A. Gage-Bouchard, Email: eagage@buffalo.edu, Department of Community Health and Health Behavior, The School of Public Health and Health Professions, University at Buffalo, 320 Kimball Tower, Buffalo, NY 14214-8028, USA
Katie A. Devine, Department of Radiation Oncology, University of Rochester Medical Center, Rochester, NY, USA
Charles E. Heckler, Department of Radiation Oncology, University of Rochester Medical Center, Rochester, NY, USA
References
- Ahnis A, Riedl A, Rigura A, Steinhagen-Thiessen E, Liebl ME, Klapp BF. Psychological and socio-demographic predictors of premature discontinuation of a 1-year multimodal outpatient weight-reduction program: An attrition analysis. Journal of Patient Preference and Adherence. 2012;6:165–177. doi: 10.2147/PPA.S28022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashida S, Hadley DW, Vaughn BK, Kuhn NR, Jenkins JF, Koehly LM. The impact of familial environment on depression scores after genetic testing for cancer susceptibility. Clinical Genetics. 2009;75:43–49. doi: 10.1111/j.1399-0004.2008.01104.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baskin CH, Forehand R, Saylor C. Predictors of psychological adjustment in mothers of children with cancer. Journal of Psychosocial Oncology. 1985;3:43–54. [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, et al. Socioeconomic status in health research: One size does not fit all. JAMA. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Brown H, Prescott R. Applied mixed models in medicine. West Sussex, England: Wiley; 2006. [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56:267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Chesler MA, Parry C. Gender roles and/or styles in crisis: An integrative analysis of the experiences of fathers of children with cancer. Qualitative Health Research. 2001;11:363–384. doi: 10.1177/104973230101100307. [DOI] [PubMed] [Google Scholar]
- Dasch KB, Russell HF, Kelly EH, Gorzkowski JA, Mulcahey MJ. Coping in caregivers of youth with spinal cord injury. Journal of Clinical Psychology in Medical Settings. 2011 doi: 10.1007/s10880-011-9258-z. (e-pub ahead of print, August 22, 2011) [DOI] [PubMed] [Google Scholar]
- Enskar K, Hamrin E, Carlson M, von Essen L. Swedish mothers and fathers of children with cancer: Perceptions of well-being, social life, and quality of life. Journal of Psychosocial Oncology. 2011;29:51–66. doi: 10.1080/07347332.2011.534026. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ. Dynamics of a stressful encounter: Cognitive appraisal, coping, an encounter outcomes. Journal of Personality and Social Psychology. 1986;50:992–1003. doi: 10.1037//0022-3514.50.5.992. [DOI] [PubMed] [Google Scholar]
- Frank NC, Blount RL, Brown RT. Attributions, coping and adjustment in children with cancer. Journal of Pediatric Psychology. 1997;22:563–576. doi: 10.1093/jpepsy/22.4.563. [DOI] [PubMed] [Google Scholar]
- Gage EA. The dynamics and processes of social support: Families’ experiences coping with a serious pediatric illness. Sociology of Health and Illness. 2013;35(3):405–418. doi: 10.1111/j.1467-9566.2012.01491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold JI, Treadwell M, Weissman L, Vichinsky E. The mediating effects of family functioning on psychosocial outcomes in healthy siblings of children with sickle cell disease. Pediatric Blood Cancer. 2011 doi: 10.1002/pbc.22933. (Epub ahead of print, February 25 2011) [DOI] [PubMed] [Google Scholar]
- Goldbeck L. Parental coping with the diagnosis of childhood cancer: Gender effects, dissimilarity within couples, and quality of life. Psycho-Oncology. 2001;10:325–335. doi: 10.1002/pon.530. [DOI] [PubMed] [Google Scholar]
- Grootenhuis MA, Last BF. Adjustment and coping by parents of children with cancer: A review of the literature. Supportive Care in Cancer. 1997;5:466–484. doi: 10.1007/s005200050116. [DOI] [PubMed] [Google Scholar]
- Herd P, Goesling B, House JS. Socioeconomic position and health: The differential effects of education versus income on the onset versus progression of health problems. Journal of Health and Social Behavior. 2007;48:223–238. doi: 10.1177/002214650704800302. [DOI] [PubMed] [Google Scholar]
- Hill K, Higgins A, Dempster M, McCarthy A. Fathers’ views and understanding of their roles in families with a child with acute lymphoblastic leukaemia: An interpretive phenomenological analysis. Journal of Health Psychology. 2009;14:1268–1280. doi: 10.1177/1359105309342291. [DOI] [PubMed] [Google Scholar]
- Hoekstra-Weebers JEHM, Jaspers JPC, Kamps WA, Klip EC. Risk factors for psychological maladjustment of parents of children with cancer. Journal of the American Academy of Child Adolescent Psychology. 1999;38:1526–1535. doi: 10.1097/00004583-199912000-00014. [DOI] [PubMed] [Google Scholar]
- Hoekstra-Weebers JEHM, Wijnberb-Williams BJ, Jaspers JPC, Kamps WA, van de Wiel HBM. Coping and its effect on psychological distress of parents of pediatric cancer patients: a longitudinal prospective study. Psycho-Oncology. 2011 doi: 10.1002/pon.1987. (Epub ahead of print, May 24, 2011) [DOI] [PubMed] [Google Scholar]
- Jobe-Shields L, Alderfer MA, Barrera M, Vannatta K, Currier JM, Phipps S. Parental depression and family environment predict distress in children prior to stem-cell transplantation. Journal of Developmental and Behavioral Pediatrics. 2009;30:140–146. doi: 10.1097/DBP.0b013e3181976a59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53:983–997. [PubMed] [Google Scholar]
- Klassen AF, Raina P, McIntosh C, Sung L, Klaassen RJ, O’Donnell M, et al. Parents of children with cancer: which factors explain differences in health-related quality of life. International Journal of Cancer. 2011;129:1190–1198. doi: 10.1002/ijc.25737. [DOI] [PubMed] [Google Scholar]
- Kupst MJ, Natta MB, Richardson CC, Schulman JL, Lavigne JV, Das L. Family coping with pediatric leukemia: Ten years after treatment. Journal of Pediatric Psychology. 1995;20:601–617. doi: 10.1093/jpepsy/20.5.601. [DOI] [PubMed] [Google Scholar]
- Long KA, Marsland AL. Family adjustment to childhood cancer: A systematic review. Clinical Child and Family Psychology Review. 2011;14:57–88. doi: 10.1007/s10567-010-0082-z. [DOI] [PubMed] [Google Scholar]
- Lopez-Olivo MA, Landon GC, Siff SJ, Edelstein D, Pak C, Kallen MA, et al. Psychosocial determinants of outcomes in knee replacement. Annals of the Rheumatic Diseases. 2011;70:1775–1781. doi: 10.1136/ard.2010.146423. [DOI] [PubMed] [Google Scholar]
- Martin S, Calabrese SK, Wolters PL, Walker KA, Warren K, Hazra R. Family functioning and coping styles in families of children with cancer and HIV disease. Clinical Pediatrics. 2011 doi: 10.1177/0009922811417300. (Epub ahead of print August 25, 2011) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos R. Conceptual and empirical approaches to developing family-based assessment procedures: Resolving the case of the Family Environment Scale. Family Process. 1990;29:199–208. doi: 10.1111/j.1545-5300.1990.00199.x. [DOI] [PubMed] [Google Scholar]
- Moos R, Moos B. Family Environment Scale manual: Development, applications, research. 3. Palo Alto, CA: Consulting Psychologist Press; 1994. [Google Scholar]
- Ogburn KM, Sanches M, Williamson DE, Caetano SC, Olvers RL, Pliszka S, et al. Family environment and pediatric major depressive disorder. Psychopathology. 2010;43:312–318. doi: 10.1159/000319400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai ALH, Greenley RN, Lewandowski A, Drotar D, Youngstrom E, Peterson CC. A meta-analytic review of the influence of pediatric cancer on parent and family functioning. Journal of Family Psychology. 2007;21:407–415. doi: 10.1037/0893-3200.21.3.407. [DOI] [PubMed] [Google Scholar]
- Palmer SL, Lesh S, Wallace D, Bonner MJ, Swain M, Chapieski L, et al. Hoe parents cope with their child’s diagnosis and treatment of an embryonal tumor: Results of a prospective and longitudinal study. Journal of Neuro-oncology. 2011;105:253–259. doi: 10.1007/s11060-011-0574-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paredes T, Pereira M, Simoes MR, Canavarro MC. A longitudinal study on emotional adjustment of sarcoma patients: the determinant role of demographic, clinical and coping variables. European Journal of Cancer Care. 2012;21:41–51. doi: 10.1111/j.1365-2354.2011.01269.x. [DOI] [PubMed] [Google Scholar]
- Pheula GF, Rhode LA, Schmitz M. Are family variables associated with ADHD, inattentive type? A case-control study in schools. European Child and Adolescent Psychiatry. 2011;20:137–145. doi: 10.1007/s00787-011-0158-4. [DOI] [PubMed] [Google Scholar]
- Rodriguez EM, Dunn MJ, Zuckerman T, Vannatta K, Gerhardt CA, Compas BE. Cancer-related sources of stress for children with cancer and their parents. Journal of Pediatric Psychology. 2012;37:185–197. doi: 10.1093/jpepsy/jsr054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rother S, Cohen LJ. Approach, avoidance, and coping with stress. American Psychologist. 1986;41:813–819. doi: 10.1037//0003-066x.41.7.813. [DOI] [PubMed] [Google Scholar]
- Schnittker J. Education and the changing shape of the income gradient in health. Journal of Health and Social Behavior. 2004;45:286–305. doi: 10.1177/002214650404500304. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Adler NE, Marmot MG. Subjective social status: Its determinants and its association with measures of ill-health in the Whitehall II study. Social Science and Medicine. 2003;56:1321–1333. doi: 10.1016/s0277-9536(02)00131-4. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Marmot MG, Adler NE. Does subjective social status predict health and change in health status better than objective status? Psychosomatic Medicine. 2005;67:855–861. doi: 10.1097/01.psy.0000188434.52941.a0. [DOI] [PubMed] [Google Scholar]
- Thompson RJ, Jr, Gustafson KE, Hamlett KW, Spock A. Stress, coping, and family functioning in the psychological adjustment of mothers of children with cystic fibrosis. Journal of Pediatric Psychology. 1992;17:573–585. doi: 10.1093/jpepsy/17.5.573. [DOI] [PubMed] [Google Scholar]
- Vachha B, Adams R. Implications of family environment and language development: Comparing typically developing children to those with spina bifida. Child: Care, Health and Development. 2009;35:709–716. doi: 10.1111/j.1365-2214.2009.00966.x. [DOI] [PubMed] [Google Scholar]
- Wenninger K, Helmes A, Bengel J, Lauten M, Volkel S, Niemeyer CM. Coping in long-term survivors of childhood cancer: relations to psychological distress. Psycho-Oncology. 2012;28 doi: 10.1002/pon.3073. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- Yeh CH. Gender differences of parental distress in children with cancer. Journal of Advanced Nursing. 2002;38:598–606. doi: 10.1046/j.1365-2648.2000.02227.x. [DOI] [PubMed] [Google Scholar]
- Zelikovsky N, Schast AP, Jean-Francois D. Parent stress and coping: Waiting for a child to receive a kidney transplant. Journal of Clinical Psychology in Medical Settings. 2007;14:320–329. [Google Scholar]