Abstract
Background
Difficulties with executive function has been found in preterm children, resulting in difficulties with learning and school performance.
Aim
This study evaluated the relationship of early working memory as measured by object permanence items to the cognitive and language scores on the Bayley Scales-III in a cohort of children born extremely preterm.
Study Design
Logistic regression models were conducted to compare object permanence scores derived from the Bayley Scales-III by race/ethnicity and maternal education, controlling for medical covariates.
Subjects
Extremely preterm toddlers (526), who were part of a Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network's multi-center study, were evaluated at 18-22 months corrected age.
Outcome Measures
Object permanence scores derived from the Bayley Developmental Scales were compared by race/ethnicity and maternal education, controlling for medical covariates.
Results
There were no significant differences in object permanence mastery and scores among the treatment groups after controlling for medical and social variables, including maternal education and race/ethnicity. Males and children with intraventricular hemorrhage, retinopathy of prematurity, and bronchopulmonary dysplasia were less likely to demonstrate object permanence mastery and had lower object permanence scores. Children who attained object permanence mastery had significantly higher Bayley Scales-III cognitive and language scores after controlling for medical and socio-economic factors.
Conclusions
Our measure of object permanence is free of influence from race, ethnic and socio-economic factors. Adding this simple task to current clinical practice could help detect early executive function difficulties in young children.
Keywords: Working memory, prematurity, development
1. INTRODUCTION
Executive function is a critical element of neurodevelopment in humans. It encompasses working memory, inhibition, and cognitive flexibility.1,2 Difficulties with executive function have been found in infants born preterm as early as 8 to 18 months, independent of maternal education and cognitive skills.3 Early working memory, an integral component of executive function, requires the ability to selectively attend to information that is important while simultaneously inhibiting interfering information. It also mediates a wide range of activities requiring reasoning and planning.4 Woodward et al (2005) found that 2-year-olds born preterm had more problems encoding new information into working memory than term infants.5 Children born extremely preterm continue to exhibit difficulties in cognition, inhibition, and perceptual-motor skills in kindergarten compared to peers born full term.6 Difficulty with executive function persists into school age, especially in the areas of response inhibition, planning, and verbal and spatial working memory skills.7-10
The Bayley Scales of Infant and Toddler Development (BSID)11-13 are used to determine cognitive function in extremely preterm children prior to the age of 42 months. These scores, however, have been found to be poor predictors of school-age function.14 We have previously reported differences among racial/ethnic groups on the Bayley Scales of Infant and Toddler Development–2nd edition (BSID-II)12 not explained by socioeconomic status or maternal education,15 with White children having a significantly higher mental developmental index than Hispanic or Black children. However, we found that measures of object permanence were similar among these groups as well as across income levels,15 suggesting that object permanence may be a culturally neutral measure of early executive function.
The objective of the current study was to evaluate the relationship of early working memory as measured by object permanence test items to the cognitive and language scores on the Bayley Scales of Infant and Toddler Development–3rd edition (BSID-III) in a large cohort of children born extremely preterm at 18-22 months corrected age. These infants had been enrolled in a randomized, multicenter trial in the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Neonatal Research Network (NRN). We hypothesized that object permanence would not be affected by maternal education or race/ethnicity, in contrast to BSID-III cognitive and language scores, and that object permanence scores would correlate significantly with performance on the BSID-III cognitive and language scores.
2. METHODS
2.1. Study Population
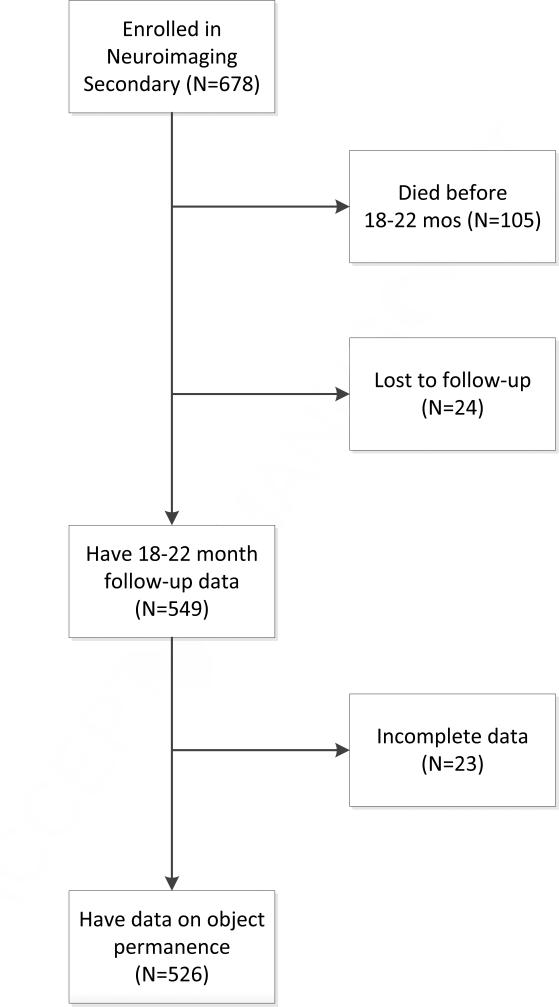
All children in this planned secondary study of object permanence had been enrolled in the Neuroimaging and Neurodevelopmental Outcome (NEURO) secondary study to the NICHD NRN Surfactant Positive Airway Pressure and Pulse Oximetry Trial (SUPPORT) multi-center study.16, 17 The SUPPORT study was a randomized, multicenter, 2x2 factorial trial of oxygenation (lower vs. higher oxygenation saturation target range) and ventilation (continuous positive airway pressure vs. intubation and surfactant) management strategies beginning in the delivery room among 24 to 27+6/7 week estimated gestational age infants. All surviving infants in the SUPPORT study had a comprehensive neurodevelopmental follow-up visit at 18-22 months of age corrected for prematurity.16,17 Object permanence scores were performed and reported only for those children enrolled in this secondary study who were born between June 2005 to February 2009 in one of 15 participating centers of the NRN across the United States (see Figure 1). Ethnicity/race was obtained by maternal self report.
Figure 1.
Flowchart of the population, detailing numbers enrolled in the study and those included in this specific study
2.2 Test Measures
The BSID-III13 were administered between 18 and 22 months, age adjusted for prematurity. The cognitive and language scales were used for this study (mean 100, standard deviation 15). Examiners at each site were certified to administer the BSID-III through the Neonatal Research Network. Three items (numbers: 40, 45 and 50) within the Cognitive Scale were used as measures of object permanence. The items sequentially increased in difficulty and were each worth 1 point. First, the child was asked to find a toy hidden under one of two cups (item 40). Second, the cups were reversed after the toy was hidden (item 45). Third, double visual displacement was used as the toy was hidden under one cup, removed and hidden a second time under the second cup (item 50). Items were administered according to the standardized instruction, and the three items were within the tests administered with the 18-22 month old children. Object permanence score was defined as the number of items correctly completed (ordinal measure). Object permanence mastery was defined as a score of ≥ 2 (categorical measure).
2.3. Statistical Analyses
Because the object permanence score is an ordinal measure (i.e., number of items correctly completed), Poisson regression models with generalized estimating equations were conducted to compare object permanence scores between children in different racial/ethnic groups and maternal education levels after controlling for SUPPORT randomized treatment group, NRN center, and clinically relevant covariates (gender, gestational age, adjusted age at testing, multiple gestations, intraventricular hemorrhage grade III or IV (IVH III-IV) or cystic periventricular leukomalacia (cPVL) (based on sonogram), severe retinopathy of prematurity (ROP) (defined by threshold retinopathy, ophthalmologic surgery, or the use of bevacizumab treatment), and bronchopulmonary dysplasia (BPD) (defined as infants receiving supplemental oxygen by any means at 36 weeks gestational age)). Similar logistic regression models were conducted to compare object permanence mastery by race/ethnicity and maternal education, controlling for treatment group, center, and medical covariates. Comparable linear regression models were then conducted to examine the relationship between object permanence and BSID-III scores, after accounting for covariates. More detailed definitions of the medical covariates were provided previously in SUPPORT trial studies.16,17 All analyses were conducted using Statistical Analysis Software version 9.3 statistical software and performed by the Data Coordinating Center (RTI International).
RESULTS
Selected demographic and medical characteristics of the 526 children in this study are shown in Table 1. The percentage of children demonstrating object permanence and the mean object permanence scores by demographic and medical characteristics are shown in Table 2. In the bivariate comparisons, males and children with ROP were less likely to demonstrate object permanence mastery and had lower object permanence scores. In addition, those in the lower gestational age strata (24-25 weeks versus 26-27 weeks) had lower object permanence scores.
Table 1.
Sample Characteristics
| Characteristic | N (%) |
|---|---|
| Ventilation | |
| Early Extubation and CPAP | 261 (50) |
| Early Surfactant and Ventilation | 265 (50) |
| Oxygen level | |
| High target SpO2 (91-95%) | 273 (52) |
| Low target SpO2 (85-89%) | 253 (48) |
| Gestational age...mean (SD) | 26 (1) |
| Birth weight...mean (SD) | 853 (192) |
| Male | 293 (56) |
| IVH III-IV/cPVL | 73 (14) |
| Severe ROP | 59 (12) |
| BPD | 196 (37) |
| Corrected age at follow-up visit...mean (SD) | 20 (2) |
| Education | |
| Less than high school | 127 (25) |
| High school graduate | 153 (30) |
| Some college or more | 235 (46) |
| Race/Ethnicity | |
| Black, non-Hispanic | 165 (31) |
| White, non-Hispanic | 229 (24) |
| Hispanic | 115 (22) |
| Other/Unknown | 17 (3) |
Note: N=526.
Table 2.
Mean Object Permanence Scores and Percentages of Study Children with Object Permanence Mastery by Treatment and Demographic Characteristics
| Characteristic | Object permanence mastery |
Object permanence scores |
||
|---|---|---|---|---|
| N (%) | p | Mean (SD) | P | |
| Ventilation | ||||
| Early Extubation and CPAP | 165 (63) | 0.752 | 1.88 (1.15) | 0.489 |
| Early Surfactant and Ventilation | 164 (62) | 1.81 (1.16) | ||
| Oxygen level | ||||
| High target SpO2 (91-95%) | 173 (63) | 0.686 | 1.85 (1.18) | 0.876 |
| Low target SpO2 (85-89%) | 156 (62) | 1.83 (1.13) | ||
| Gestational age | ||||
| 24-25 weeks | 117 (59) | 0.165 | 1.71 (1.16) | 0.046 |
| 26-27 weeks | 212 (65) | 1.92 (1.15) | ||
| Gender | ||||
| Male | 170 (58) | 0.016 | 1.75 (1.14) | 0.042 |
| Female | 159 (68) | 1.96 (1.16) | ||
| IVH III-IV/cPVL | ||||
| Yes | 41 (56) | 0.230 | 1.61 (1.23) | 0.075 |
| No | 287 (64) | 1.88 (1.14) | ||
| Severe ROP | ||||
| Yes | 25 (42) | < 0.001 | 1.41 (1.15) | 0.003 |
| No | 304 (65) | 1.88 (1.15) | ||
| BPD | ||||
| Yes | 113 (58) | 0.074 | 1.71 (1.19) | 0.050 |
| No | 216 (65) | 1.92 (1.13) | ||
| Education | ||||
| Less than high school | 86 (68) | 0.308 | 1.92 (1.18) | 0.643 |
| High school graduate | 90 (59) | 1.79 (1.21) | ||
| Some college or more | 148 (63) | 1.85 (1.11) | ||
| Race/Ethnicity | ||||
| Black | 101 (61) | 0.717 | 1.85 (1.14) | 0.349 |
| White | 149 (65) | 1.68 (1.20) | ||
| Hispanic | 68 (59) | 1.82 (1.24) | ||
| Other/Unknown | 11 (65) | 1.92 (1.14) | ||
Note: N=526
There were no significant differences in object permanence mastery and scores among the treatment groups after controlling for medical and social variables (Table 3). There were also no significant differences in object permanence mastery and scores by gestational age, IVH III-IV/cPVL, maternal education or race/ethnicity after controlling for other medical and social factors. Similar to findings in the bivariate model, significant differences were found for male gender, children with younger adjusted age at testing and ROP, even after accounting for other factors. In addition, those children diagnosed with BPD had significantly lower object permanence mastery and scores when controlling for other factors.
Table 3.
Regression Models of Object Permanence Mastery and Scores
| Characteristic | Object Permanence Mastery |
Object Permanence Score |
||
|---|---|---|---|---|
| Adjusted OR (95% CI) | p | Adjusted mean difference (SE) | p | |
| Ventilation | ||||
| Early Extubation and CPAP | 1.01 (0.65, 1.58) | 0.950 | 0.05 (0.05) | 0.334 |
| Early Surfactant and Ventilation | REF | REF | ||
| Oxygen level | ||||
| High target SpO2 (91-95%) | 1.16 (0.74, 1.82) | 0.498 | 0.05 (0.05) | 0.313 |
| Low target SpO2 (85-89%) | REF | REF | ||
| Gestational age | 0.90 (0.72, 1.13) | 0.357 | −0.02 (0.03) | 0.475 |
| Male | 0.53 (0.34, 0.83) | 0.007 | −0.18 (0.06) | 0.003 |
| IVH III-IV/cPVL | 0.76 (0.40, 1.44) | 0.385 | −0.18 (0.12) | 0.143 |
| Severe ROP | 3.01 (1.41, 6.45) | 0.006 | 0.30 (0.15) | 0.045 |
| BPD | 0.56 (0.34, 0.94) | 0.030 | −0.15 (0.08) | 0.044 |
| Corrected age at follow-up visit | 1.21 (1.05, 1.40) | 0.011 | 0.03 (0.01) | <0.001 |
| Education | ||||
| Less than high school | 1.31 (0.72, 2.39) | 0.364 | 0.05 (0.07) | 0.532 |
| High school | 0.89 (0.53, 1.51) | 0.659 | −0.01 (0.06) | 0.874 |
| Some college or more | REF | REF | ||
| Race/Ethnicity | ||||
| Black | 0.78 (0.44, 1.39) | 0.390 | −0.04 (0.07) | 0.576 |
| White | REF | REF | ||
| Hispanic | 1.40 (0.69, 2.85) | 0.338 | 0.03 (0.08) | 0.766 |
| Other/Unknown | 1.69 (0.45, 6.34) | 0.431 | 0.07 (0.15) | 0.632 |
Note: REF=reference category. N=515 for both models. Odds ratios and mean differences are adjusted for center, ventilation type, oxygen level, gestational age, gender, IVH III-IV/cPVL, severe ROP, BPD, corrected age at follow-up, maternal education, and race/ethnicity.
The overall mean (standard deviation) BSID-III scores were 91.83 (14.21) for the cognitive composite and 86.38 (16.32) for the language composite. Children who attained object permanence mastery had significantly higher BSID-III cognitive and language scores after controlling for both medical and socio-economic factors (Table 4). Cognitive scores were 12 points higher and language scores nearly 9 points higher among those with object permanence mastery, adjusted for multiple confounders including maternal education and race/ethnicity. Children who were male and had IVH III-IV/cPVL, severe ROP, or BPD or who were younger at the time of testing (corrected age), had significantly lower cognitive composite scores (Table 4). Children of mothers with high school education or less had significantly lower BSID-III language scores than those whose mothers had some college education or more. Boys and Hispanic children scored significantly lower on the language scale. Children with BPD also had lower language scores.
Table 4.
Regression Models of Bayley III Cognitive and Language Composite Scores by Object Permanence Mastery, Treatment Group and Demographic Characteristics
| Characteristic | Cognitive Composite |
Language Composite |
||
|---|---|---|---|---|
| Adjusted mean difference (SE) | p | Adjusted mean difference (SE) | P | |
| Object Permanence Mastery | 12.03 (1.10) | < 0.001 | 8.75 (1.47) | < 0.001 |
| Ventilation | ||||
| Early Extubation and CPAP | 1.55 (1.04) | 0.144 | 0.81 (1.39) | 0.562 |
| Early Surfactant and Ventilation | REF | REF | ||
| Oxygen level | ||||
| High target SpO2 (91-95%) | 0.09 (1.05) | 0.929 | −0.19 (1.41) | 0.891 |
| Low target SpO2 (85-89%) | REF | REF | ||
| Gestational age | 0.64 (0.54) | 0.246 | 1.04 (0.72) | 0.159 |
| Male | −2.81 (1.01) | 0.008 | −4.25 (1.36) | 0.003 |
| IVH III-IV/cPVL | −4.85 (1.47) | 0.002 | −1.53 (1.95) | 0.439 |
| Severe ROP | 3.94 (1.74) | 0.029 | 2.92 (2.32) | 0.216 |
| BPD | −4.02 (1.19) | 0.002 | −3.58 (1.60) | 0.031 |
| Corrected age at follow-up visit | −0.60 (0.24) | 0.015 | −0.22 (0.33) | 0.509 |
| Education | ||||
| Less than high school | −1.73 (1.39) | 0.220 | −5.35 (1.85) | 0.006 |
| High school | −2.14 (1.24) | 0.091 | −3.99 (1.65) | 0.020 |
| Some college or more | REF | REF | ||
| Race/Ethnicity | ||||
| Black | −0.01 (1.36) | 0.991 | −1.92 (1.83) | 0.300 |
| White | REF | REF | ||
| Hispanic | −0.81 (1.62) | 0.621 | −6.25 (2.18) | 0.007 |
| Other/Unknown | −2.46 (3.07) | 0.428 | −1.25 (4.21) | 0.768 |
Note: REF=reference category. N=511 for cognitive composite model and N=503 for language composite model. Mean differences are adjusted for research center, object permanence mastery, ventilation type, oxygen level, gestational age, gender, IVH III-IV/cPVL, severe ROP, BPD, corrected age at follow-up, maternal education, and race/ethnicity.
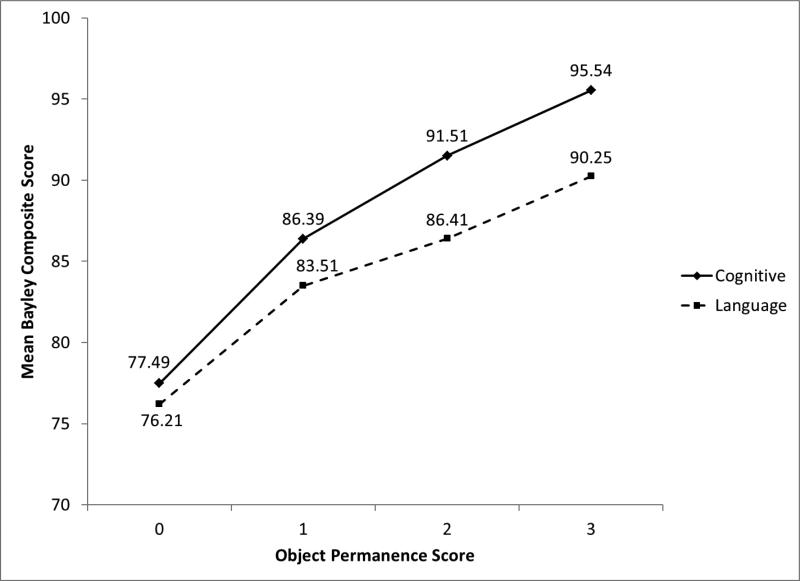
Results found in the models using object permanence score rather than object permanence mastery were comparable (Table 5). Higher object permanence score was associated with higher cognitive and language composite scores (p < 0.001). Boys and children with IVH III-IV/cPVL, severe ROP, or BPD or lower corrected age at time of testing had significantly lower object permanence scores. Boys, children with BPD, and those who had mothers with lower educations had significantly lower language composite scores. Model-adjusted mean BSID-III cognitive and language scores for each possible object permanence score are shown in Figure 2.
Table 5.
Regression Models of Bayley III Cognitive and Language Composite Scores by Object Permanence Score, Treatment Group and Demographic Characteristics
| Characteristic | Cognitive Composite |
Language Composite |
||
|---|---|---|---|---|
| Adjusted mean difference (SE) | p | Adjusted mean difference (SE) | P | |
| Object Permanence Score | 5.80 (0.45) | < 0.001 | 4.42 (0.62) | < 0.001 |
| Ventilation | ||||
| Early Extubation and CPAP | 1.14 (1.01) | 0.264 | 0.53 (1.36) | 0.701 |
| Early Surfactant and Ventilation | REF | REF | ||
| Oxygen level | ||||
| High target SpO2 (91-95%) | 0.27 (1.01) | 0.794 | −0.12 (1.38) | 0.929 |
| Low target SpO2 (85-89%) | REF | REF | ||
| Gestational age | 0.56 (0.52) | 0.293 | 0.99 (0.71) | 0.170 |
| Male | −2.81 (0.97) | 0.006 | −4.17 (1.34) | 0.003 |
| IVH III-IV/cPVL | −3.87 (1.42) | 0.009 | −0.86 (1.94) | 0.660 |
| Severe ROP | 4.52 (1.67) | 0.010 | 3.18 (2.28) | 0.170 |
| BPD | −3.68 (1.15) | 0.003 | −3.34 (1.57) | 0.040 |
| Corrected age at follow-up visit | −0.74 (0.23) | 0.002 | −0.34 (0.33) | 0.301 |
| Education | ||||
| Less than high school | −1.68 (1.34) | 0.216 | −5.23 (1.81) | 0.006 |
| High school | −2.36 (1.19) | 0.055 | −4.10 (1.61) | 0.015 |
| Some college or more | REF | REF | ||
| Race/Ethnicity | ||||
| Black | −0.23 (1.32) | 0.862 | −2.18 (1.79) | 0.231 |
| White | REF | REF | ||
| Hispanic | −0.54 (1.57) | 0.733 | −6.15 (2.13) | 0.006 |
| Other/Unknown | −2.36 (2.96) | 0.431 | −1.13 (4.12) | 0.785 |
Note: REF=reference category. N=511 for cognitive composite model and N=503 for language composite model. Mean differences are adjusted for research center, object permanence score, ventilation type, oxygen level, gestational age, gender, IVH III-IV/cPVL, severe ROP, BPD, corrected age at follow-up, maternal education, and race/ethnicity.
Figure 2.
Model-Adjusted Mean Bayley-III Cognitive and Language Composite Scores by Object Permanence Scores
DISCUSSION
In this prospective, multicenter study we found that object permanence as a measure of early working memory was significantly related to measures of cognition and language, but not associated with race/ethnicity or maternal education. This confirms our previous findings in regards to object permanence and cognition as measured by the BSID-II,18 and provides additional evidence that object permanence is a culturally neutral measure of early working memory. This is an important finding, as tests of cognition are influenced by race/ethnicity,19 maternal education, and parental stress.20 The controversy related to biases inherent in measures of intelligence, especially related to race/ethnic factors, is not new,21 but we continue to use them as the main measure of morbidity and indicator of improvement in medical care.
Interest in studying executive functioning, including early working memory, inhibition, and reasoning, have been increasing over the past decade;9 however, these skills are difficult to measure in young children.22 We used object permanence, a skill described by Piaget23 as one of the earliest measures of early working memory,24 a skill that is related to early white matter injury5 and development of dorsolateral prefrontal regions.25 Our finding that object permanence was associated with cognition and language scores on the BSID-III indicates that it could potentially augment research by providing an additional measure of development that is potentially free of socio-economic and racial/ethnic biases.18 Better understanding of early executive functioning in extremely preterm children could lead to earlier diagnosis and improved interventions for children born preterm. In conjunction with the BSID-III cognitive score, a measure of object permanence may improve our detection of ongoing problems with executive function at 18–22 months, which is highly related to learning difficulties later in life. Early childhood intervention results in significant improvements in cognitive, academic, and social outcomes,26 and tasks that specifically work on early working memory can be developed to potentially enhance executive functioning skills in young children.27
We also found that children with IVH, ROP and BPD had significantly lower object permanence scores. These findings are similar to those in the Trial of Indomethacin Prophylaxis in Preterms (TIPP) study as IVH, ROP, and BPD were also associated with adverse developmental outcomes at 18-month in children born extremely-low birth weight.28 Schmidt and associates found that children who had IVH had the greatest odds of poor long-term outcome followed by those children with severe ROP or BPD.28 Our findings that boys did more poorly on measures of object permanence are consistent with other outcome studies of children born preterm.9,22,28 Corrected age at time of testing also impacted object permanence mastery which is consistent with Piaget's findings that this is a skill that is developmental in nature.23 It is important to take into account the age of the child when using this type of a task.
A limitation of this study is that the object permanence items used were selected from the cognitive scale of the BSID-III. Since we also administered the BSID-III cognitive scale in the study, using these items in both measures could result in a degree of correlation between the scales. However, our findings for object permanence were significantly different from the BSID-III cognitive scale when race/ethnicity was taken into account. Another limitation of this study is that this cohort may not be a representative sample of extremely low birth weight infants and therefore caution should be used in generalizing these findings.29 A strength of our study was the utilization of the NICHD NRN, which includes a large number of children from a variety of race, ethnic and socio-economic backgrounds.
In conclusion, our study supports the hypothesis that our measure of object permanence is free of influence from race, ethnic and socio-economic factors. We suggest that this can be used to detect early deficits in working memory in children born extremely low birth weight. Adding this simple task to our current clinical practice would allow us to detect early executive function difficulties in young children. Further investigation of ways to identify specific intervention techniques to enhance early executive skills would be beneficial.
ACKNOWLEDGEMENTS
The National Institutes of Health, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), and the National Heart, Lung, and Blood Institute (NHLBI) provided grant support for the Neonatal Research Network's SUPPORT Trial.
Data collected at participating sites of the NICHD Neonatal Research Network (NRN) were transmitted to RTI International, the data coordinating center (DCC) for the network, which stored, managed and analyzed the data for this study. On behalf of the NRN, Drs. Abhik Das (DCC Principal Investigator) and Carla Bann (DCC Statistician) had full access to all the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis.
We are indebted to our medical and nursing colleagues and the infants and their parents who agreed to take part in this study.
FUNDING SOURCES
The National Institutes of Health and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) provided grant support for the Neonatal Research Network Follow-up studies
APPENDIX
The following investigators, in addition to those listed as authors, participated in this study:
NRN Steering Committee Chair: Michael S. Caplan, MD, University of Chicago, Pritzker School of Medicine (2006-2011).
Alpert Medical School of Brown University and Women & Infants Hospital of Rhode Island (U10 HD27904) – Abbot R. Laptook, MD; William Oh, MD; Angelita M. Hensman, RN BSN; Bonnie E. Stephens, MD; Barbara Alksninis, PNP; Dawn Andrews, RN; Kristen Angela, RN; Susan Barnett, RRT; Bill Cashore, MD; Melinda Caskey, MD; Kim Francis, RN; Dan Gingras, RRT; Regina A. Gargus, MD FAAP; Katharine Johnson, MD; Shabnam Lainwala, MD; Theresa M. Leach, MEd CAES; Martha R. Leonard, BA BS; Sarah Lillie, RRT; Kalida Mehta; James R. Moore, MD; Lucy Noel; Suzy Ventura; Rachel V. Walden; Victoria E. Watson, MS CAS.
Case Western Reserve University, Rainbow Babies & Children's Hospital (U10 HD21364, M01 RR80) – Michele C. Walsh, MD MS; Avroy A. Fanaroff, MD; Nancy S. Newman, RN; Bonnie S. Siner, RN; Arlene Zadell RN; Julie DiFiore, BS; Monika Bhola, MD; Harriet G. Friedman, MA; Gulgun Yalcinkaya, MD.
Duke University School of Medicine, University Hospital, Alamance Regional Medical Center, and Durham Regional Hospital (U10 HD40492, M01 RR30) – Ronald N. Goldberg, MD; C. Michael Cotten, MD MHS; Patricia Ashley, MD; Kathy J. Auten, MSHS; Kimberley A. Fisher, PhD FNP-BC IBCLC; Katherine A. Foy, RN; Sharon F. Freedman, MD; Sandra Grimes, RN BSN; Kathryn E. Gustafson, PhD; Melody B. Lohmeyer, RN MSN; William F. Malcolm, MD; David K. Wallace, MD MPH.
Emory University, Children's Healthcare of Atlanta, Grady Memorial Hospital, and Emory Crawford Long Hospital (U10 HD27851, RR25008, M01 RR39) – Barbara J. Stoll, MD; Susie Buchter, MD;
Anthony J. Piazza, MD; David P. Carlton, MD; Linda Black, MD; Ann M. Blackwelder, RNC BS MS; Sheena Carter, PhD; Elisabeth Dinkins, PNP; Sobha Fritz, PhD; Ellen C. Hale, RN BS CCRC; Amy K. Hutchinson, MD; Maureen Mulligan LaRossa, RN; Gloria V. Smikle, PNP MSN.
Eunice Kennedy Shriver National Institute of Child Health and Human Development – Stephanie Wilson Archer, MA.
Indiana University, University Hospital, Methodist Hospital, Riley Hospital for Children, and Wishard Health Services (U10 HD27856, M01 RR750) – Brenda B. Poindexter, MD MS; James A. Lemons, MD; Leslie D. Wilson, BSN CCRC; Faithe Hamer, BS; Ann B. Cook, MS; Dianne E. Herron, RN; Carolyn Lytle, MD MPH; Heike M. Minnich, PsyD HSPP.
National Heart, Lung, and Blood Institute – Mary Anne Berberich, PhD; Carol J. Blaisdell, MD; Dorothy B. Gail, PhD; James P. Kiley, PhD.
RTI International (U10 HD36790) – W. Kenneth Poole, PhD; Marie G. Gantz, PhD; Jamie E. Newman, PhD MPH; Jeanette O'Donnell Auman, BS; Carolyn Petrie Huitema, MS; James W. Pickett II, BS; Dennis Wallace, PhD; Kristin M. Zaterka-Baxter, RN BSN.
Stanford University, Lucile Packard Children's Hospital (U10 HD27880, UL1 RR25744, M01 RR70) – Krisa P. Van Meurs, MD; David K. Stevenson, MD; M. Bethany Ball, BS CCRC; Barbara Bentley, PsychD MSEd; Maria Elena DeAnda, PhD; Anne M. DeBattista, RN, PNP; Jean G. Kohn, MD MPH; Renee P. Pyle, PhD; Nicholas H. St. John, PhD; Hali E. Weiss, MD.
Tufts Medical Center, Floating Hospital for Children (U10 HD53119, M01 RR54) – Ivan D. Frantz III, MD; John M. Fiascone, MD; Anne Furey, MPH; Brenda L. MacKinnon, RNC; Ellen Nylen, RN BSN; Ana Brussa, MS OTR/L; Cecelia Sibley, PT MHA.
University of Alabama at Birmingham Health System and Children's Hospital of Alabama (U10 HD34216, M01 RR32) – Waldemar A. Carlo, MD; Namasivayam Ambalavanan, MD; Monica V. Collins, RN BSN MaEd; Shirley S. Cosby, RN BSN. Vivien A. Phillips, RN BSN; Kirstin J. Bailey, PhD; Fred J. Biasini, PhD; Maria Hopkins, PhD; Kristen C. Johnston, MSN CRNP; Sara Krzywanski, MS; Kathleen G. Nelson, MD; Cryshelle S. Patterson, PhD; Richard V. Rector, PhD; Leslie Rodriguez, PhD; Amanda Soong, MD; Sally Whitley, MA OTR-L FAOTA; Sheree York, PT DPT MS PCS.
University of California – San Diego Medical Center and Sharp Mary Birch Hospital for Women (U10 HD40461) – Neil N. Finer, MD; Maynard R. Rasmussen, MD; Paul R. Wozniak, MD; Kathy Arnell, RNC; Rene Barbieri-Welge; Ayala Ben-Tall; Renee Bridge, RN; Clarence Demetrio, RN; Martha G. Fuller, RN MSN; Elaine Ito; Meghan Lukasik; Wade Rich, RRT; Deborah Pontillo; Donna Posin, OTR/L MPA; Cheryl Runyan; James Wilkes; Paul Zlotnik.
University of Iowa Children's Hospital (U10 HD53109, UL1 RR24979, M01 RR59) – Edward F. Bell, MD; John A. Widness, MD; Jonathan M. Klein, MD; Tarah T. Colaizy, MD MPH; Karen J. Johnson, RN BSN; Diane L. Eastman, RN CPNP MA.
University of New Mexico Health Sciences Center (U10 HD53089, M01 RR997) – Robin K. Ohls, MD; Julie Rohr, MSN RNC CNS; Conra Backstrom Lacy, RN; Rebecca Montman, BSN.
University of Texas Southwestern Medical Center at Dallas, Parkland Health & Hospital System,
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST STATEMENT
The coauthors have no conflicts of interests relevant to this manuscript.
REFERENCES
- 1.Lehto JE, Juujarvi P, Kooistra L, Pulkkinen L. Dimensions of executive functioning evidence from children. Br J Dev Psychol. 2003;21:59–80. [Google Scholar]
- 2.Lezak MD. Neuropsychological Assessment. Oxford University Press; New York: 2004. [Google Scholar]
- 3.Sun J, Rao N. Scaffolding Interactions with Preschool Children: comparisons between Chinese mothers and teachers across different tasks. Merrill-Palmer quarterly. 2012;58(1):110–140. [Google Scholar]
- 4.Diamond A. The early development of executive function. In: Bialystok E, Craik FIM, editors. Lifespan cognition: Mechanisms of change. Oxford University press; New York: 2006. pp. 70–95. [Google Scholar]
- 5.Woodward LJ, Edgin JO, Thompson D, Inder TE. Object working memory deficits predicted by early brain injury and development in the preterm infant. Brain. 2005;128:2578–2587. doi: 10.1093/brain/awh618. [DOI] [PubMed] [Google Scholar]
- 6.Orchinik LJ, Taylor HG, Espy KA, et al. Cognitive outcomes for extremely preterm/extremely low birth weight children in kindergarten. J Int Neuropsychol Soc. 2011;17(6):1067–79. doi: 10.1017/S135561771100107X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson PJ, Doyle LW. Cognitive and educational deficits in children born extremely preterm. Semin Perinatol. 2008;32(1):51–58. doi: 10.1053/j.semperi.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 8.Aarnoudse-Moens CS, Weisglas-Kuperus N, van Goudoever JB, Oosterlaan J. Development of preschool and academic skills in children born very preterm. J Pediatr. 2011;158:51–6. doi: 10.1016/j.jpeds.2010.06.052. [DOI] [PubMed] [Google Scholar]
- 9.Mulder H, Pitchford NJ, Hagger MS, Marlow N. Development of executive function and attention in preterm children: A systematic review. Dev Neuropsychol. 2009;34(4):393–421. doi: 10.1080/87565640902964524. [DOI] [PubMed] [Google Scholar]
- 10.Bayless S, Stevenson J. Executive functions in school-age children born very prematurely. Early Hum Dev. 2007;83(4):247–254. doi: 10.1016/j.earlhumdev.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 11.Bayley N. Bayley Scales of Infant Development. Harcourt Assessment; New York: 1969. [Google Scholar]
- 12.Bayley N. Manual for the Bayley scales of infant development. 2nd edition The Psychological Corporation; San Antonio (TX): 1993. [Google Scholar]
- 13.Bayley N. Bayley scales of infant and toddler development. 3rd edition Harcourt Assessment; San Antonio (TX): 2006. [Google Scholar]
- 14.Hack M, Taylor G, Drotar D, et al. Poor predictive validity of the Bayley Scales of Development for cognitive function of extremely low birth weight children at school age. Pediatrics. 2005;116:333–341. doi: 10.1542/peds.2005-0173. [DOI] [PubMed] [Google Scholar]
- 15.Lowe J, Erickson SE, MacLean P, Duvall SW. Early working memory and maternal communication in toddlers born very low birth weight. Acta Paediatr. 2009;98:660–663. doi: 10.1111/j.1651-2227.2008.01211.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Finer NN, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. 2010 doi: 10.1056/NEJMoa0911783. DOI: 10.1056/NEJMoa0911783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carlo WA, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Target ranges of oxygen saturation in extremely preterm infants. N Engl J Med. 2010 doi: 10.1056/NEJMoa0911781. DOI: 10.1056/NEJMoa0911781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lowe J, MacLean P, Shaffer ML, Watterberg K. Early working memory in children born with extreme low birth weight: assessed by object permanence. J Child Neurol. 2009;24:410–415. doi: 10.1177/0883073808324533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duncan AF, Watterberg KL, Nolen TL, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Effect of Ethnicity and Race on Cognitive and Language Testing at Age 18-22 Months in Extremely Preterm Infants. J Pediatr. 2012 Jun;160(6):966–71. doi: 10.1016/j.jpeds.2011.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brummelte S, Grunau RE, Synnes AR, Whitfeld MF, Petrie-Thomas J. Declining cognitive development from 8 to 18 months in preterm children predicts persisting higher parenting stress. Early Hum Dev. 2011;87:273–280. doi: 10.1016/j.earlhumdev.2011.01.030. [DOI] [PubMed] [Google Scholar]
- 21.Jensen AR. How much can we boost I.Q. and scholastic achievement? Harv Educ Rev. 1969;33:1–123. [Google Scholar]
- 22.Carlson SM. Developmentally sensitive measures of executive function in preschool children. Dev Neuropsychol. 2005;28(2):595–616. doi: 10.1207/s15326942dn2802_3. [DOI] [PubMed] [Google Scholar]
- 23.Piaget J. The origins of intelligence in children. International Universities Press; New York, NY: 1952. [Google Scholar]
- 24.Diamond A. Development of the ability to use recall to guide action, as indicated by infants’ performance on ABBAR. Child Dev. 1985;56(4):868–883. [PubMed] [Google Scholar]
- 25.Goldman-Rakic P. Functional development of the prefrontal cortex in early life and the problem of neuronal plasticity. Exp Neurol. 1971;32:366–387. doi: 10.1016/0014-4886(71)90005-7. [DOI] [PubMed] [Google Scholar]
- 26.Ramey CT, Campbell FA, Burchinal M, Skinner ML, Gardner DM, Ramey SL. Persistent effects of early childhood education on high-risk children and their mothers. Appl Dev Sci. 2000;4(1):2–14. [Google Scholar]
- 27.Diamond A, Barnett WS, Thomas J, Munro S. Preschool program improves cognitive control. Science. 2007;318:1387–1388. doi: 10.1126/science.1151148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schmidt B, Asztalos EV, Roberts RS, Robertson CM, Sauve RS, Whitfield MF. Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months. JAMA. 2004;289(9):1124–1129. doi: 10.1001/jama.289.9.1124. [DOI] [PubMed] [Google Scholar]
- 29.Rich W, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Enrollment of extremely low birth weight infants in a clinical research study may not be representative. Pediatrics. 2012;129:480–484. doi: 10.1542/peds.2011-2121. [DOI] [PMC free article] [PubMed] [Google Scholar]