Abstract
Acinetobacter baumannii (A. baumannii) is Gram-negative coccobacilli that has emerged as a nosocomial pathogen. Several reports in Indonesia showed the continuous presence of A. baumannii. This study aimed to determine the incidence of A. baumannii bacteremia in neonates in the Neonatal Unit Dr. Cipto Mangunkusumo Hospital (RSCM), Jakarta, Indonesia, and assess its role in blood stream infection using antibiogram and genotyping by pulsed-field gel electrophoresis (PFGE). Subjects were neonates with clinical sepsis. Blood specimens from the neonates and samples of suspected environment within the Neonatal Unit were cultivated. Antimicrobial resistance profiles were classified for analysis purpose. A. baumannii isolates were genotyped by PFGE to determine their similarity. A total of 24 A. baumannii were isolated from 80 neonates and the environment during this period of study. Seven isolates from the neonates showed multiple antimicrobial resistance (MDR), and 82% (n = 17) of the environment isolates were also MDR. Antibiotype “d” seemed to be predominant (62.5%). PFGE analysis showed a very close genetic relationship between the patients and environment isolates (Dice coefficient 0.8–1.0). We concluded that a mode of transmission of environmental microbes to patients was present in the Neonatal Unit of RSCM and thus needed to be overcome.
1. Introduction
Acinetobacter spp. are ubiquitous in the environment, that is, soil and water, and occasionally isolated from mucous membrane, secretion, and skin of hospitalized patients, also on surfaces of hospital environment [1]. This aerobic Gram-negative coccobacilli has emerged as important nosocomial pathogen. Clinical sepsis (CSEP) is included in the blood stream infections (BSI) category and restricted only for infant less than 1 year old [2]. However, in protocols of CDC/NHSN 2013, CSEP criteria are not in the list of BSI group but laboratory-confirmed BSI type 1, 2, and 3 [3].
Multidrug resistance of A. baumannii has caused morbidity, mortality, and increased patients' length of stay in hospital in many countries [4–6]. Mortality of patient with Acinetobacter sp. infection reached 17%–46% [4, 5]. The continuous presence of this environment microorganism from clinical specimens in Jakarta, Indonesia, has been reported [7, 8]. Since Acinetobacter sp. is frequently established as part of skin and respiratory flora of hospitalized patients especially with prolonged periods, assessment of A. baumannii as etiology of disease or colonization is a particular challenge [9]. Bacterial typing either fenotype or genotype would be very useful in indicating HAI cases, as known widely [10, 11]. A case-control study is also recommended to be used in Hospital/Healthcare-acquired infections investigation [12].
Acinetobacter sp. is nonfastidious and easily grows in routine media such as blood agar, MacConkey, and chocolate agar [9, 13]. It looks smooth, opaque, raised, and creamy colony in blood agar and pale or nonlactose fermenter in MacConkey agar [1, 9].
This study aimed to determine the incidence of A. baumannii bacteremia in neonates in Neonatal Unit, Dr. Cipto Mangunkusumo Hospital (RSCM), Jakarta, Indonesia, and assess its role in blood stream infection using antibiogram and genotyping by pulsed-field gel electrophoresis (PFGE) method.
2. Materials and Methods
2.1. Subjects and Specimens
This is a cross-sectional study. Subjects of this study were neonates (0–28 days old; birth weight 1,000–2,000 gram) with clinical sepsis, and within 48 hrs or more of being hospitalized, no clear focal infection was detected, using catheter lines, during 9 months period (June 2010–February 2011). Neonates with birth weight 1,000–2,000 g were in focus because of their viability or being supposed to survive with correct treatment and avoid hospital acquired infection. CDC/NHSN surveillance definition of HAI criteria was used [2]. Two blood specimens from two separate venipunctures drawn simultaneously were cultivated in BACTEC PAED bottles; aseptic procedures were strictly applied as prevention of contamination [2, 9].
All microbiology procedures were carried out at Clinical Microbiology Laboratory of Medical Faculty University of Indonesia (CML-FMUI).
2.2. The Environmental Specimens
Samples from the environment were chosen based on observation of suspected hospital staffs, devices, and patients in the same ward.
2.3. Cultivation and Identification
Blood specimens were cultured using BACTEC PAED. Gram stain were carried out on positive bottles and followed by inoculation on to blood agar and MacConkey. Identification was conducted using coagulase, catalase, mannitol, API STREP, and API STAPH for Gram positive bacteria. While for the Gram negative the tests were oxidase, API 20E, and API 20NE [9]. Incubation at 44°C was also performed to distinguish A. baumannii from A. calcoaceticus [1, 9].
2.4. Antimicrobial Susceptibility Testing
Antimicrobial susceptibility tests using disk diffusion method were performed for each isolate. Clinical and Laboratory Standards Institute (CLSI) apply as reference [14]. Antibiotics tested were as follow: ceftazidime, amikacin, trimethoprim-sulfamethoxazole, ampicillin-sulbactam, ofloxacin, levofloxacin, meropenem, imipenem, amoxicillin-clavulanic acid, ceftriaxone, cefotaxime, gentamicin, tobramycin, tetracycline, ciprofloxacin, aztreonam, cefepime, piperacillin-tazobactam, and ticarcillin.
Antibiotype was determined as described by Tega et al., 2007 [11], and marked as a lowercase letter. Differences in one or two antibiotics susceptibility were grouped in the same antibiotypes.
2.5. Storage
All of the isolates were stored in nutrient broth containing glycerol 7.5% (v/v) and kept in −80°C. A. baumannii isolates were subcultured on blood agar prior to genotyping.
2.6. Genotyping
Plugs containing bacterial pellets were prepared prior to ApaI (Vivantis) enzyme digestion. The procedures were conducted as described by Suwanto and Kaplan [15]. Electrophoresis was carried out using CHEF-DR II apparatus (Bio-Rad Laboratories, CA, USA) in TBE buffer 0.5x at 14°C. Initial and final time of electrophoresis was 5.3–34.9 seconds; running time was 19.5 hours. Rhodobacter sphaeroides 2.4.1. was used as molecular marker [15]. Analysis was conducted using Unweighted Pair Group Means Method (UPGMA) as described by Seifert et al., 2005, to determine the isolates' pulsotypes [16].
3. Results
3.1. Subjects and Specimens
Out of 80 neonates included in this study, 28 neonates (35%) were diagnosed with sepsis as confirmed by blood culture results. Among these, 5 neonates had A. baumannii bacteremia. Thirty-seven isolates obtained from positive blood cultures were Gram-negative bacteria (see Table 1). A total of 7 A. baumannii isolates were found.
Table 1.
Spectrum of microorganisms isolated from blood culture of neonates with sepsis.
| Microorganisms | Number of isolates* | Number of neonates |
|---|---|---|
| Acinetobacter baumannii | 7 | 5 |
| Pseudomonas aeruginosa | 4 | 3 |
| Staphylococcus epidermidis | 3 | 3 |
| Enterobacter asburiae | 4 | 2 |
| Staphylococcus aureus | 3 | 2 |
| Stenotrophomonas maltophilia | 2 | 2 |
| Candida tropicalis | 2 | 1 |
| Enterobacter cloacae | 2 | 1 |
| Mould | 2 | 1 |
| Candida albicans | 1 | 1 |
| Candida sp. | 1 | 1 |
| Citrobacter freundii | 1 | 1 |
| Candida parapsilosis | 1 | 1 |
| Enterobacter amnigenus 2 | 1 | 1 |
| Enterobacter aerogenes | 1 | 1 |
| Klebsiella pneumoniae | 1 | 1 |
| Serratia marcescens | 1 | 1 |
|
| ||
| Total | 37 | 28 |
*One neonate might experience more than 1 episode of sepsis.
3.2. Specimens from Environment
A variety of microbes were isolated from the environment. Over 50 suspected surfaces and devices located in the ward were examined. Seventeen isolates of A. baumannii were isolated from 17 locations. The following were the origins of those isolates: buttons of ventilator, perineum and gluteus area of different neonates, arm (hand and wrist) area of different neonates, hand of nurse, hand of doctors, plastics covered in porthole of infant incubator, bogota bag on patient who had colostomy, and tap water (see Table 2).
Table 2.
Antimicrobial Susceptibility patterns of 24 Acinetobacter baumannii isolates.
| No | Source | AMX | CAZ | CFP | AMK | K | C | TMP/SXT | SAM | OFX | FOS | LVX | MEM | IPM | AMC | CXM | CRO | CTX | CN | TOB | TE | CIP | ATM | FEP | TZP | CSL | TIC | Antibiotype |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Blood | R | R | R | S | R | R | R | S | R | R | R | R | R | R | R | R | R | R | R | R | R | I | R | R | I | R | a |
| 2 | Blood | R | R | R | R | R | R | R | R | I | R | R | S | S | R | R | R | R | R | R | R | R | R | R | R | S | R | b |
| 3 | Blood | R | R | R | S | R | R | R | R | R | R | R | R | R | R | R | R | R | R | S | R | R | R | R | R | I | R | c |
| 4 | Skin (arm) of neonate | R | R | R | I | R | R | R | R | R | R | I | R | R | R | R | R | R | R | R | R | R | I | R | R | I | R | d |
| 5 | Skin (arm) of neonate | S | R | I | S | S | S | R | S | R | S | I | S | S | S | R | I | R | S | S | S | S | I | R | S | I | I | e |
| 6 | Skin (arm) of neonate | R | R | R | S | R | R | S | S | I | R | S | S | S | R | R | R | R | R | R | R | R | R | R | I | S | R | f |
| 7 | Skin (arm) of neonate | R | R | R | I | R | I | R | R | R | R | I | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | d |
| 8 | Buttons of ventilator | R | R | R | I | R | R | R | I | R | R | I | R | R | R | R | R | R | R | R | R | R | I | R | R | I | R | d |
| 9 | Skin (perineum, gluteal) of neonate | R | R | R | R | R | R | R | R | R | R | S | R | R | R | R | R | R | R | R | R | R | R | R | R | I | R | g |
| 10 | Skin (perineum, gluteal) of neonate | R | R | R | I | R | R | R | I | R | R | I | R | R | R | R | R | R | R | R | R | R | I | R | R | I | R | d |
| 11 | Skin (perineum, gluteal) of neonate | R | R | R | R | R | R | R | I | I | R | I | R | R | R | R | R | R | R | R | R | R | R | R | R | I | R | d |
| 12 | Blood | R | R | R | R | R | R | R | R | R | R | I | R | R | R | R | R | R | R | R | R | R | I | R | R | I | R | d |
| 13 | Skin (perineum, gluteal) of neonate | R | R | R | I | R | R | R | I | I | R | I | R | R | R | R | R | R | R | R | R | R | R | R | R | I | R | d |
| 14 | Skin (hand) of doctor | R | R | R | R | R | R | R | I | R | R | I | R | R | R | R | R | R | R | S | R | R | R | R | R | I | R | h |
| 15 | Blood | R | R | R | R | R | R | R | I | R | R | I | R | R | R | R | R | R | R | R | R | R | I | R | R | I | R | d |
| 16 | Blood | R | R | R | I | R | R | R | R | I | R | I | R | R | R | R | R | R | R | R | R | R | I | R | R | I | R | d |
| 17 | Blood | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | I | R | d |
| 18 | Plastics covered in porthole of infant incubator | R | R | R | R | R | R | R | I | R | R | I | R | R | R | R | R | R | R | R | R | R | R | R | R | I | R | d |
| 19 | Skin (arm) of neonate | R | R | R | I | R | R | R | I | I | R | S | R | R | R | R | R | R | R | R | R | R | I | I | R | I | R | g |
| 20 | Skin (hand) of nurse | R | R | R | I | R | R | R | I | R | R | I | R | R | R | R | R | R | R | R | R | R | R | R | R | I | R | d |
| 21 | Bogota bag | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | R | d |
| 22 | Skin (hand) of doctor | R | R | R | I | R | R | R | I | R | R | I | R | R | R | R | R | R | R | R | R | R | R | R | R | I | R | d |
| 23 | Tap water | S | S | I | S | S | R | S | S | S | S | S | S | S | S | I | I | I | S | S | S | S | I | S | S | S | S | i |
| 24 | Skin (perineum, gluteal) of neonate | R | R | R | R | R | R | R | I | R | R | I | R | R | R | R | R | R | R | R | R | R | R | R | R | I | R | d |
CAZ: ceftazidime, CFP: cefoperazone, AMK: amikacin, K: kanamycin, C: chloramphenicol, TMP/SXT: trimethoprim-sulfamethoxazole, OFX: ofloxacin, FOS: fosfomycin, LVX: levofloxacin, MEM: meropenem, IPM: imipenem, AMC: amoxicillin-clavulanic acid, CXM: cefuroxime, CRO: ceftriaxone, CTX: cefotaxime, CN: gentamicin, TOB: tobramycin, TE: tetracycline, CIP: ciprofloxacin, ATM: aztreonam, FEP: cefepime, TZP: piperacillin-tazobactam, CSL: cefoperazone-sulbactam, and TIC: ticarcillin.
S: sensitive, I: intermediate, and R: resistant.
Intermediate result is assumed as resistant result.
3.3. Antimicrobial Susceptibility
A total of 24 A. baumannii were tested for their susceptibility to antibiotics. Overall, susceptibility of A. baumannii to antibiotics was very low ranging between 0% and 21%. Susceptibility to ceftazidime was 4%, amikacin 21%, trimetoprim-sulfamethoxazole 8%, ampicillin-sulbactam 16%, ofloxacin 4%, levofloxacin 16%, meropenem 16%, imipenem 16%, amoxicillin-clavulanic acid 8%, ceftriaxone 16%, cefotaxime 0%, gentamicin 16%, tobramycin 16%, tetracycline 16%, ciprofloxacin 16%, aztreonam 0%, cefepime 4%, piperacillin-tazobactam 8%, and ticarcillin 4% (Figure 1). All isolates originated from blood showed multiple antimicrobial resistant (MDR), while of the environmental isolates, 82% were MDR.
Figure 1.

Susceptibility pattern of A. baumannii isolates (n = 24) to various antibiotics.
Of all A. baumannii isolates tested, 9 distinct antibiotypes (“a”–“i”) were determined (Table 2). Predominant antibiotype was “d,” which is composed of 4 isolates that originated from blood and eleven from environment. Thus, 62.5% of the isolates were identical based on their antibiogram profile.
3.4. PFGE
ApaI digested genomic DNA of all 24 A. baumannii strains that revealed 11–13 fragments DNA with molecular weight ranges between 63 and 1,100 kb. Estimated genome size varied from 1,663 up to 3,392 kb (Figure 2). The electrophoresis results were transformed into binary data and analyzed by UPGMA software. Seven distinct PFGE types (pulsotype “A”–“G”) were identified (Figure 3). Twenty-three isolates (96%) showed a high degree of similarity with Dice coefficient 0.8–1.0 (pulsotype “A”–“F”); therefore these isolates were very closely related. Of these, 7 isolates were originated from blood and 16 from the environment.
Figure 2.
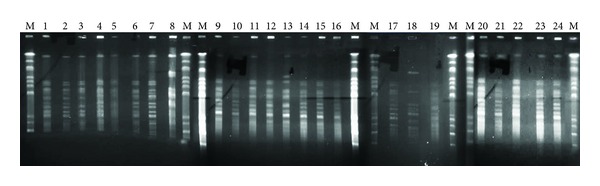
PFGE (Schizotype) profile from A. baumannii (n = 24) digested by ApaI restriction enzyme. Running condition: agarose gel 1.2% in TBE 0.5x, buffer TBE 0.5x, temperature 14°C, ramping pulse 5.3–34.9 second, and run time: 19.5 hours.
Figure 3.
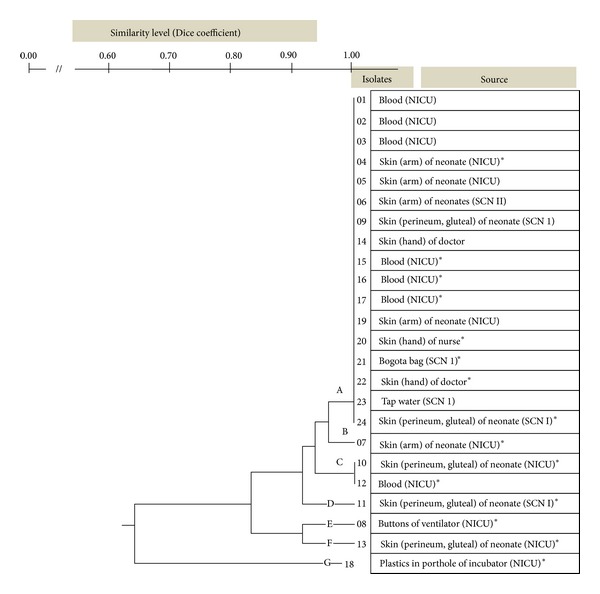
Phenogram of A. baumannii isolates. Seven pulsotypes (“A”–“G”) were identified. Twenty-three isolates (96%) showed a high degree of similarity with Dice coefficient 0.8–1.0, that is, pulsotype “A”–“F”. *Identical antibiotypes.
One environmental A. baumannii strain, which was isolated from plastics covered in porthole of infant incubator, was not in a close similarity with the other (Dice coefficient 0.667) (Figure 3).
4. Discussions
A. baumannii is known as environmental microorganism; however it has been found as commensal in human skin, perineum, and digestive system in hospitalized patients. Our findings were in agreement with other reports [15, 17]. Most of A. baumannii isolates from the environment in this study derived from skin of the patients themselves indicated that colonization of A. baumannii played an important role in the occurrence of hospital infections. The other microbes such as Staphylococcus aureus, Enterobacter asburiae, and Pseudomonas aeruginosa found as colonization on neonates' skin, plastics covered portholes of incubator, syringe pump, humidifier liquid attached to incubator, and so forth (data not shown), could also give risks of infection when aseptic and antiseptic techniques in invasive procedures were not done properly [13].
Most of A. baumannii isolated in the study were multidrug resistant (MDR). According to Abbo et al., 2005, MDR criteria were defined when resistant to all of studied antibiotics, that is, piperacillin-tazobactam, cefepime, ceftazidime, aztreonam, ciprofloxacin, gentamicin, and tobramycin, but could be sensitive to amikacin, ampicillin-sulbactam, imipenem, meropenem, and minocycline [18]. Several reports showed that the usage of broad spectrum antibiotics affected normal flora and induced MDR A. baumannii [19, 20]. The same situation occurred in the unit where this study was conducted; broad spectrum antibiotics such as Carbapenem, Piperacillin-Tazobactam, Cefepime, combined with Aminoglycoside, and Amikacin were widely used.
In this study, genetic relationship of A. baumannii isolates was assessed using antibiogram and genotyping, while other investigators used only antibiogram for interspecies differentiation, although it was not confirmative [2]. Genotyping by pulsed-field gel electrophoresis has been shown to give better differentiation within species [17, 18]. Our results showed that more than 50% of A. baumannii isolates with antibiotype “d” had identical genome profile (pulsotype “A”).
5. Conclusions
All A. baumannii isolated from blood of neonates with sepsis showed very close genetic relationship to those of environment. We concluded that there was transmission of environmental microbes to patients through contaminated hands of medical staffs and medical equipments. Tracking the agent of nosocomial infection using molecular approach is very fruitful to shed a light on the transmission and resources and therefore would give benefit to infection control.
Acknowledgments
This study is funded by RSCM, Jakarta, Indonesia. The authors would like to thank Tjahjono D. Gondhowiardjo, M.D., Ph.D., for the funding by the institution.
References
- 1.Brooks GF, Carroll KC, Butel JS, Morse SA, Mietzner TA. Pseudomonads, acinetobacters & uncommon gram-negative bacteria. In: Brooks G, Carroll KC, Butel J, Morse S, Mietzner T, editors. Jawetz, Melnick and Adelberg, Medical Microbiology. 25th edition. chapter 16 2010. [Google Scholar]
- 2.Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. American Journal of Infection Control. 2008;36(5):309–332. doi: 10.1016/j.ajic.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 3.CDC/NHSN protocol corrections, clarification and addition for surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. 2013. [DOI] [PubMed]
- 4.Kilic A, Li H, Mellmann A, et al. Acinetobacter septicus sp. nov. association with a nosocomial outbreak of bacteremia in a neonatal intensive care unit. Journal of Clinical Microbiology. 2008;46(3):902–908. doi: 10.1128/JCM.01876-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vandenbroucke-Grauls CMJE, Kerver AJH, Rommes JH, Jansen R, den Dekker C, Verhoef J. Endemic Acinetobacter anitratus in a surgical intensive care unit: mechanical ventilators as reservoir. European Journal of Clinical Microbiology and Infectious Diseases. 1988;7(4):485–489. doi: 10.1007/BF01962597. [DOI] [PubMed] [Google Scholar]
- 6.Charnot-Katsikas A, Dorafshar AH, Aycock JK, David MZ, Weber SG, Frank KM. Two cases of necrotizing fasciitis due to Acinetobacter baumannii . Journal of Clinical Microbiology. 2009;47(1):258–263. doi: 10.1128/JCM.01250-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moehario LH, Tjoa E. Isolation of environmental microorganisms from clinical specimens: a report of the occurence of Acinetobacter anitratus in blood of hospitalized patients in Jakarta in a 7 year period. Medical Journal of Indonesia. 2009;18(4):227–232. [Google Scholar]
- 8.Moehario LH, Tjoa E, Kiranasari A, Ningsih I, Rosana Y, Karuniawati A. Trends in antimicrobial susceptibility of gram-negative bacteria isolated from blood in Jakarta from 2002 to 2008. Journal of Infection in Developing Countries. 2009;3(11):843–848. doi: 10.3855/jidc.85. [DOI] [PubMed] [Google Scholar]
- 9.Forbes BA, Sahm DF, Weissfeld AS. Bailey & Scott’s Diagnostic Microbiology. 12th edition 2007. [Google Scholar]
- 10.Tenover FC, Arbeit RD, Goering RV, et al. Interpreting chromosomal DNA restriction patterns produced by pulsed- field gel electrophoresis: criteria for bacterial strain typing. Journal of Clinical Microbiology. 1995;33(9):2233–2239. doi: 10.1128/jcm.33.9.2233-2239.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tega L, Raieta K, Ottaviani D, Russo GL, Blanco G, Carraturo A. Catheter-related bacteremia and multidrug-resistant Acinetobacter lwoffii . Emerging Infectious Diseases. 2007;13(2):355–356. doi: 10.3201/eid1302.060858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sehulster L, Chinn RYW. Guidelines for environmental infection control in health-care facilities. Recommendations of CDC and the Health Care Infection Control Practices Advisory Committee (HICPAC) Morbidity and Mortality Weekly Report. 2003;52(RR10):1–42. [PubMed] [Google Scholar]
- 13.Murray PR, Rosenthal KS, Pfaller MA. Medical Microbiology. 5th edition. 2005. Pseudomonas and related organisms; pp. 357–365. [Google Scholar]
- 14.Performance standards for antimicrobial susceptibility testing, twentieth international supplement. Clinical and Laboratory Standards Institute. 2010;30(1) [Google Scholar]
- 15.Suwanto A, Kaplan S. Physical and genetic mapping of the Rhodobacter sphaeroides 2.4.1 genome: genome size, fragment identification, and gene localization. Journal of Bacteriology. 1989;171(11):5840–5849. doi: 10.1128/jb.171.11.5840-5849.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seifert H, Dolzani L, Bressan R, et al. Standardization and interlaboratory reproducibility assessment of pulsed-field gel electrophoresis-generated fingerprints of Acinetobacter baumannii . Journal of Clinical Microbiology. 2005;43(9):4328–4335. doi: 10.1128/JCM.43.9.4328-4335.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ku SC, Hsueh PR, Yang PC, Luh KT. Clinical and microbiological characteristics of bacteremia caused by Acinetobacter lwoffii . European Journal of Clinical Microbiology and Infectious Diseases. 2000;19(7):501–505. doi: 10.1007/s100960000315. [DOI] [PubMed] [Google Scholar]
- 18.Abbo A, Navon-Venezia S, Hammer-Muntz O, Krichali T, Siegman-Igra Y, Carmeli Y. Multidrug-resistant Acinetobacter baumannii . Emerging Infectious Diseases. 2005;11(1):22–29. doi: 10.3201/eid1101.040001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agustí C, Pujol M, Argerich MJ, et al. Short-term effect of the application of selective decontamination of the digestive tract on different body site reservoir ICU patients colonized by multi-resistant Acinetobacter baumannii . Journal of Antimicrobial Chemotherapy. 2002;49(1):205–208. doi: 10.1093/jac/49.1.205. [DOI] [PubMed] [Google Scholar]
- 20.Camp C, Tatum OL. A review of Acinetobacter baumannii as a highly successful pathogen in times of war. Laboratory Medicine. 2010;41(11):649–657. [Google Scholar]


