Abstract
Purpose
To evaluate the association of a specific type of lower urinary tract symptom (LUTS) and the depression in community-dwelling elderly Korean men.
Materials and Methods
A total of 392 men aged 65 years or older, who completed urological and psychiatric evaluations as a participant of the Korean Longitudinal Study on Health and Aging, were included. From each subject, an interview on the demographic characteristics and medical history, IPSS, and psychiatric questionnaire were taken. Subjects were divided into two groups; depression and euthymic. Subjects with IPSS subscore more than 3 points was considered 'high' subscore. IPSS subscores were compared between the two groups, and the relationship between depression and LUTS severity was assessed.
Results
The mean age of the subjects was 75, and 6.4% of the subjects were diagnosed to have major depressive disorders. The depression group showed higher IPSS scores than the euthymic group (16.1±9.9 vs. 11.6±8.6, p=0.01). IPSS subscores of question 1 (incomplete empty), question 3 (intermittency), question 4 (urgency) and question 6 (straining to void) were higher in the depression group compared with the euthymic group. Chi-square test revealed subjects with high IPSS 1, 3, 4, and 6 score were associated with depression, but multivariate analysis identified only high IPSS question 4 as a significant prognostic factor for depression.
Conclusions
Elderly population with depression is more likely to have more severe LUTS than population without depression. Among the urinary symptoms, urgency was strongly associated with depression. Patients with moderate to severe LUTS and especially urgency may need their mental health status evaluation.
Keywords: Depression, Longitudinal studies, Lower urinary tract symptoms
INTRODUCTION
Depression is correlated with urological symptoms as well as quality of life. Several studies have illustrated that lower urinary tract symptoms (LUTS) are related to depression [1-3]. Several studies have also shown that a significant correlation exists between incontinence, nocturia, and depression [4-8]. A recent study showed that overactive bladder (OAB) symptoms can also aggravate anxiety and depressive symptoms [9-12]. However, there has been little study of which specific urinary symptoms are more likely to be associated with depression among the various voiding and storage symptoms.
Previously, we reported an association of depression with LUTS in a Korean population-based study [13]. The aim of this study was to evaluate which specific urinary symptoms are more likely to be associated with depression in the Korean population.
MATERIALS AND METHODS
1. Subjects
The data for this study were derived from the Korean Longitudinal Study on Health and Aging (KLoSHA). The detailed procedure was described in a prior article [13]. Among 992 participants, 392 men completed urological and psychiatric evaluations and did not meet the following exclusion criteria: prostate-specific antigen (PSA) level ≥ 10 ng/mL, pyuria, prostate cancer, and history of prostate surgery. All subjects were fully informed of the study protocol and provided written informed consent. The study protocol was approved by the Institutional Review Board of Seoul National University Bundang Hospital (SNUBH).
2. Assessments
Within 2 weeks of the initial contact, an extensive interview was administered to each subject. The Korean version of the International Prostate Symptom Score (IPSS) was administered to male respondents to evaluate urinary symptoms.
The IPSS consists of a total of seven questions that deal with voiding symptoms (incomplete emptying, intermittency, weak stream, and straining to void) and storage symptoms (frequency, urgency, and nocturia). The IPSS voiding subscore was the sum of question 1 (incomplete emptying), question 3 (intermittency), question 5 (weak stream), and question 6 (straining to void). The IPSS storage subscore was the sum of question 2 (frequency), question 4 (urgency), and question 7 (nocturia). Subjects with an IPSS subscore of more than 3 points were considered to have a high IPSS subscore.
Prostate volumes were calculated by using transrectal ultrasonography, and serum prostate-specific antigen levels were determined by using an immunoradioassay. All assessments were performed at SNUBH, which is located in Seongnam.
All respondents were administered the Korean version of the Mini International Neuropsychiatric Interview to diagnose depression. To evaluate depression, researchers used questionnaires, including the revised Korean version of the Geriatric Depression Scale, the Korean version of the Center for Epidemiologic Studies Depression Scale, and the 17-item Hamilton Depression Rating Scale. Depression diagnoses were made by a panel of 4 neuropsychiatrists according to the DSM-IV on the basis of the data collected through the questionnaires.
The subjects were divided into two groups according to the presence of depression: the depression group and the euthymic group, who did not have depression. The total IPSS, IPSS voiding subscore, IPSS storage subscore, and scores on each question were compared between the subjects with depression (depression group) and those without depression (euthymic group) and the relationship between depression and LUTS severity was assessed.
3. Statistical analysis
We compared the clinical variables between the subjects with depression (depression group) and those without depression (euthymic group) by using Student t-tests. Chi-square analysis was used for categorical variables, and variables in the univariate analysis with p<0.05 were included in the multivariate analysis. Multiple logistic regression analyses were conducted to estimate the odds ratio with a 95% confidence interval for high IPSS subscore and presence of depression. Statistical analyses were conducted by using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA), and p-values of <0.05 were considered significant.
RESULTS
The mean age of the subjects was 75 years, and 6.4% of the subjects were diagnosed as having major depressive disorders. There were no statistically significant differences in prostate volume, serum PSA level, or the prevalence of comorbidities such as diabetes or hypertension between the depression group and the euthymic group. The detailed characteristics of the study subjects are described in the previous publication [13].
The depression group showed higher total IPSSs than did the euthymic group (16.1±9.9 vs. 11.6±8.6, p=0.01). The IPSS voiding subscore and the IPSS storage subscore were also higher in the depression group (Table 1). Among the 7 questions on the IPSS questionnaire, IPSS subscores for question 1 (incomplete emptying), question 3 (intermittency), question 4 (urgency), and question 6 (straining to void) were higher in the depression group than in the euthymic group (Fig. 1).
TABLE 1.
The difference in International Prostate Symptom Score (IPSS) between the euthymic group and the depression group
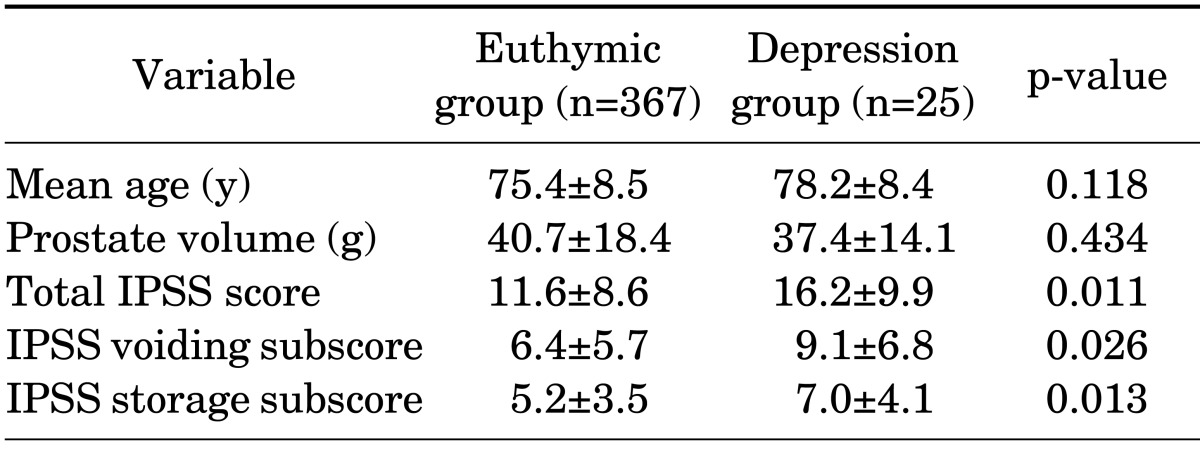
Values are presented as mean±standard deviation.
FIG. 1.
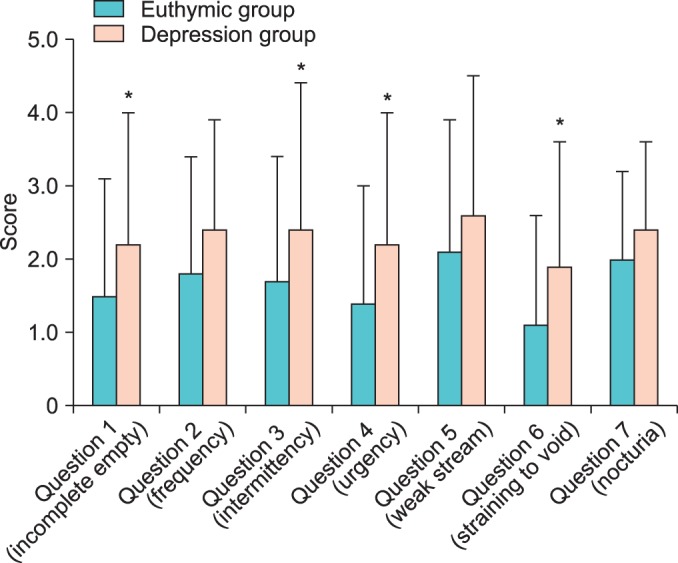
The difference in International Prostate Symptom Score subscores between the euthymic group and the depression group. Data are expressed as mean±standard deviation. *p <0.05, depression group vs. euthymic group.
Chi-square tests showed that high scores on IPSS questions 1, 3, 4, and 6 were associated with depression, but the multivariate analysis identified only a high score on IPSS question 4 (urgency) as a significant prognostic factor for depression. Subjects who had a high urgency IPSS had a 1.33 increased odds of having major depressive disorders compared with those with low or no urgency symptoms (p=0.01) (Table 2).
TABLE 2.
Analysis of lower urinary tract symptoms as a risk factor for depression
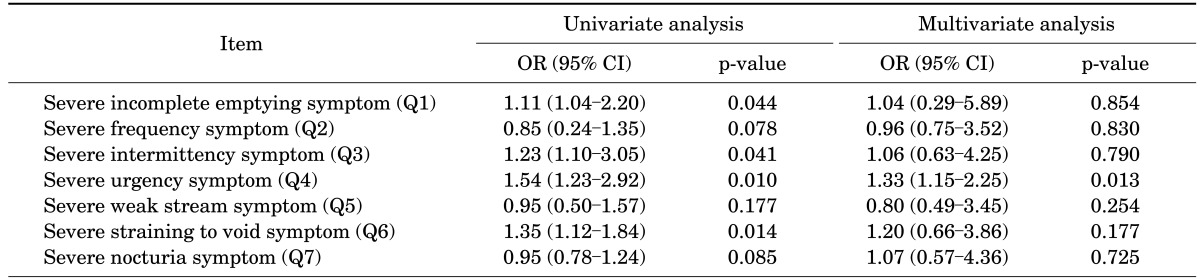
Q, item on the International Prostate Symptom Score questionnaire; OR, odds ratio; CI, confidence interval.
DISCUSSION
Depressive disorders are a very common group of diseases, with an overall prevalence of 2% to 17.1% [14-16]. Depression can have a severe impact on overall health and plays an important role in the pathogenesis of many chronic diseases, such as chronic obstructive pulmonary disease, inflammatory bowel disease, arthritis, asthma, diabetes, and congestive heart failure [17-25]. This relationship also exists between depression and many urological symptoms, such as urinary incontinence and other LUTS.
The relationship of LUTS and depression has been reported in several studies. Wong et al. [26] showed a significant association between moderate-to-severe LUTS and clinically relevant depressive disorders in a large study that included 1980 men aged 65 to 92 years. Rom et al. [1] investigated LUTS and depression in a homogeneous cohort of 673 healthy men and reported a significant effect of IPSS on depression measured by use of the Beck Depression Inventory score. We reported similar results in the previous KLoSHA study, in which depression was associated with a 5.8-fold increased odds of having moderate to severe LUTS [13]. Although several studies have shown an association of LUTS and depression, there are few studies regarding the effects of subcategories of LUTS, such as nocturia and urgency, on depression. Nocturia was reported to be strongly associated with depression in some studies [7,27-29]. In one study, depressed men had a 6.5-fold increased risk of nocturia [29]. Conversely, Johnson et al. [27] reported that patients with 5 or more episodes of nocturia per night experienced a 6.5-fold increased risk of depression compared with patients without nocturia.
OAB symptoms also affect depression. Recent study results from EpiLUTS showed that men and women with OAB were more likely to have worse scores on anxiety and depression assessments [30].
In the present study, to investigate the effect of subcategories of LUTS, we used the IPSS questionnaire and analyzed the effect of IPSS subscores on depression. Although both storage and voiding symptoms, including incomplete emptying, intermittency, urgency, and straining to void, were higher in the depression group; urgency was the only significant risk factor for depression in the multivariate analysis. A 1-point increase in urgency score was associated with 1.33 increased odds of having major depressive disorders.
The association between urgency and depression could be attributable to several different mechanisms. Obviously, moderate and severe OAB decrease quality of life in many ways and urgency is the key symptom of OAB. Quality of life is sometimes decreased to such an extent that a patient can develop depressive moods. Although there is no question item on the IPSS questionnaire that addresses urgency incontinence, the urgency subscore can represent the OAB status in the population.
A limitation of this study is that the data were cross-sectional and do not provide information regarding the temporal cause-effect relationship between urgency symptoms and depression. Also, we used one IPSS questionnaire to evaluate the LUTS of a population. More specific questionnaires evaluating OAB symptoms would be more informative for revealing the relationship of OAB symptoms and depression. Also, the cause of depression that would be related to LUTS was not analyzed. Finally, the small number of subjects in the depression group and interactions between factors, such as answers on the questionnaire, are limitations of this study, especially in the statistical analysis. The prevalence of depression was not so high that a larger study population will be needed to prove the definite correlation of urgency and depression. Despite these limitations, it is meaningful that this study showed a relationship of urgency and depression in a population-based study.
CONCLUSIONS
Our population-based study showed that older men with depression are more likely to have more severe LUTS than a population without depression. Among the various urinary symptoms, urgency was strongly associated with having depression. Patients who have moderate to severe LUTS and especially urgency may need an evaluation of their mental health status.
ACKNOWLEDGMENTS
This work was supported by an Independent Research Grant (IRG) from Pfizer Global Pharmaceuticals (Grant No. 06-05-039) and the Grant for Developing Seongnam Health Promotion Program for the Elderly from Seongnam City Government in Korea (grant No. 800-20050211).
Footnotes
The authors have nothing to disclose.
References
- 1.Rom M, Schatzl G, Swietek N, Rucklinger E, Kratzik C. Lower urinary tract symptoms and depression. BJU Int. 2012;110(11 Pt C):E918–E921. doi: 10.1111/j.1464-410X.2012.11552.x. [DOI] [PubMed] [Google Scholar]
- 2.Coyne KS, Wein AJ, Tubaro A, Sexton CC, Thompson CL, Kopp ZS, et al. The burden of lower urinary tract symptoms: evaluating the effect of LUTS on health-related quality of life, anxiety and depression: EpiLUTS. BJU Int. 2009;103(Suppl 3):4–11. doi: 10.1111/j.1464-410X.2009.08371.x. [DOI] [PubMed] [Google Scholar]
- 3.Johnson TV, Abbasi A, Ehrlich SS, Kleris RS, Owen-Smith A, Raison CL, et al. IPSS quality of life question: a possible indicator of depression among patients with lower urinary tract symptoms. Can J Urol. 2012;19:6100–6104. [PubMed] [Google Scholar]
- 4.Zorn BH, Montgomery H, Pieper K, Gray M, Steers WD. Urinary incontinence and depression. J Urol. 1999;162:82–84. doi: 10.1097/00005392-199907000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Nygaard I, Turvey C, Burns TL, Crischilles E, Wallace R. Urinary incontinence and depression in middle-aged United States women. Obstet Gynecol. 2003;101:149–156. doi: 10.1016/s0029-7844(02)02519-x. [DOI] [PubMed] [Google Scholar]
- 6.Melville JL, Katon W, Delaney K, Newton K. Urinary incontinence in US women: a population-based study. Arch Intern Med. 2005;165:537–542. doi: 10.1001/archinte.165.5.537. [DOI] [PubMed] [Google Scholar]
- 7.Asplund R, Henriksson S, Johansson S, Isacsson G. Nocturia and depression. BJU Int. 2004;93:1253–1256. doi: 10.1111/j.1464-410X.2004.04835.x. [DOI] [PubMed] [Google Scholar]
- 8.van der Vaart CH, Roovers JP, de Leeuw JR, Heintz AP. Association between urogenital symptoms and depression in community-dwelling women aged 20 to 70 years. Urology. 2007;69:691–696. doi: 10.1016/j.urology.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 9.Steers WD. Overactive bladder (OAB): what we thought we knew and what we know today. Eur Urol Suppl. 2002;1:3–10. [Google Scholar]
- 10.Tubaro A. Defining overactive bladder: epidemiology and burden of disease. Urology. 2004;64(6 Suppl 1):2–6. doi: 10.1016/j.urology.2004.10.047. [DOI] [PubMed] [Google Scholar]
- 11.Yoo ES, Kim BS, Kim DY, Oh SJ, Kim JC. The impact of overactive bladder on health-related quality of life, sexual life and psychological health in Korea. Int Neurourol J. 2011;15:143–151. doi: 10.5213/inj.2011.15.3.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Milsom I, Kaplan SA, Coyne KS, Sexton CC, Kopp ZS. Effect of bothersome overactive bladder symptoms on health-related quality of life, anxiety, depression, and treatment seeking in the United States: results from EpiLUTS. Urology. 2012;80:90–96. doi: 10.1016/j.urology.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 13.Park HK, Paick SH, Kim HG, Lho YS, Byun SS, Lee SB, et al. Effect of depression on the risk and severity of lower urinary tract symptoms in community-dwelling elderly Korean men. Low Urin Tract Symptoms. 2012;4:63–67. doi: 10.1111/j.1757-5672.2011.00113.x. [DOI] [PubMed] [Google Scholar]
- 14.Blazer DG, Kessler RC, McGonagle KA, Swartz MS. The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry. 1994;151:979–986. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- 15.Ayuso-Mateos JL, Vazquez-Barquero JL, Dowrick C, Lehtinen V, Dalgard OS, Casey P, et al. Depressive disorders in Europe: prevalence figures from the ODIN study. Br J Psychiatry. 2001;179:308–316. doi: 10.1192/bjp.179.4.308. [DOI] [PubMed] [Google Scholar]
- 16.Steffens DC, Skoog I, Norton MC, Hart AD, Tschanz JT, Plassman BL, et al. Prevalence of depression and its treatment in an elderly population: the Cache County study. Arch Gen Psychiatry. 2000;57:601–607. doi: 10.1001/archpsyc.57.6.601. [DOI] [PubMed] [Google Scholar]
- 17.Di Marco F, Verga M, Reggente M, Maria Casanova F, Santus P, Blasi F, et al. Anxiety and depression in COPD patients: The roles of gender and disease severity. Respir Med. 2006;100:1767–1774. doi: 10.1016/j.rmed.2006.01.026. [DOI] [PubMed] [Google Scholar]
- 18.Light RW, Merrill EJ, Despars JA, Gordon GH, Mutalipassi LR. Prevalence of depression and anxiety in patients with COPD: relationship to functional capacity. Chest. 1985;87:35–38. doi: 10.1378/chest.87.1.35. [DOI] [PubMed] [Google Scholar]
- 19.Kurina LM, Goldacre MJ, Yeates D, Gill LE. Depression and anxiety in people with inflammatory bowel disease. J Epidemiol Community Health. 2001;55:716–720. doi: 10.1136/jech.55.10.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Addolorato G, Capristo E, Stefanini GF, Gasbarrini G. Inflammatory bowel disease: a study of the association between anxiety and depression, physical morbidity, and nutritional status. Scand J Gastroenterol. 1997;32:1013–1021. doi: 10.3109/00365529709011218. [DOI] [PubMed] [Google Scholar]
- 21.Dickens C, McGowan L, Clark-Carter D, Creed F. Depression in rheumatoid arthritis: a systematic review of the literature with meta-analysis. Psychosom Med. 2002;64:52–60. doi: 10.1097/00006842-200201000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Janson C, Bjornsson E, Hetta J, Boman G. Anxiety and depression in relation to respiratory symptoms and asthma. Am J Respir Crit Care Med. 1994;149(4 Pt 1):930–934. doi: 10.1164/ajrccm.149.4.8143058. [DOI] [PubMed] [Google Scholar]
- 23.Blazer DG, Moody-Ayers S, Craft-Morgan J, Burchett B. Depression in diabetes and obesity: racial/ethnic/gender issues in older adults. J Psychosom Res. 2002;53:913–916. doi: 10.1016/s0022-3999(02)00314-8. [DOI] [PubMed] [Google Scholar]
- 24.Jiang W, Alexander J, Christopher E, Kuchibhatla M, Gaulden LH, Cuffe MS, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161:1849–1856. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- 25.Havranek EP, Ware MG, Lowes BD. Prevalence of depression in congestive heart failure. Am J Cardiol. 1999;84:348–350. A9. doi: 10.1016/s0002-9149(99)00293-3. [DOI] [PubMed] [Google Scholar]
- 26.Wong SY, Hong A, Leung J, Kwok T, Leung PC, Woo J. Lower urinary tract symptoms and depressive symptoms in elderly men. J Affect Disord. 2006;96:83–88. doi: 10.1016/j.jad.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 27.Johnson TV, Abbasi A, Ehrlich SS, Kleris RS, Raison CL, Master VA. Nocturia associated with depressive symptoms. Urology. 2011;77:183–186. doi: 10.1016/j.urology.2010.04.048. [DOI] [PubMed] [Google Scholar]
- 28.Foley DJ, Vitiello MV, Bliwise DL, Ancoli-Israel S, Monjan AA, Walsh JK. Frequent napping is associated with excessive daytime sleepiness, depression, pain, and nocturia in older adults: findings from the National Sleep Foundation '2003 Sleep in America' Poll. Am J Geriatr Psychiatry. 2007;15:344–350. doi: 10.1097/01.JGP.0000249385.50101.67. [DOI] [PubMed] [Google Scholar]
- 29.Asplund R, Johansson S, Henriksson S, Isacsson G. Nocturia, depression and antidepressant medication. BJU Int. 2005;95:820–823. doi: 10.1111/j.1464-410X.2005.05408.x. [DOI] [PubMed] [Google Scholar]
- 30.Coyne KS, Sexton CC, Kopp ZS, Ebel-Bitoun C, Milsom I, Chapple C. The impact of overactive bladder on mental health, work productivity and health-related quality of life in the UK and Sweden: results from EpiLUTS. BJU Int. 2011;108:1459–1471. doi: 10.1111/j.1464-410X.2010.10013.x. [DOI] [PubMed] [Google Scholar]


