Abstract
Objective
This study examined whether serum levels of GFAP breakdown products (GFAP-BDP) were elevated in mild and moderate TBI compared to controls and if they were associated with traumatic intracranial lesions on CT scan (+CT) and having a neurosurgical intervention (NSI).
Methods
This prospective cohort study enrolled adult patients presenting to three Level 1 Trauma Centers following blunt head trauma with loss of consciousness, amnesia, or disorientation and a GCS 9–15. Control groups included normal uninjured controls and trauma controls presenting to the ED with orthopedic injuries or an MVC without TBI. Blood samples were obtained in all patients within 4 hours of injury and measured by ELISA for GFAP-BDP (ng/ml).
Results
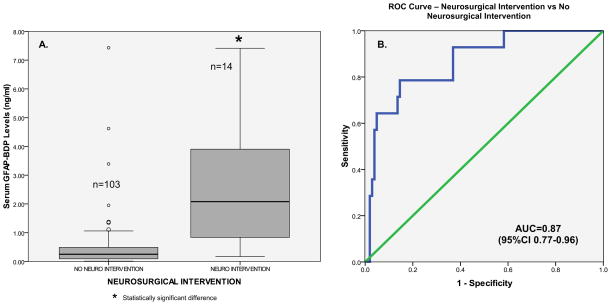
Of the 307 patients enrolled, 108 were TBI patients (97 with GCS 13–15, and 11 with GCS 9–12) and 199 were controls (176 normal controls and 16 MVC controls and 7 orthopedic controls). ROC curves demonstrated that early GFAP-BDP levels were able to distinguish TBI from uninjured controls with an AUC of 0.90 (95%CI 0.86–0.94) and differentiated TBI with a GCS 15 with an AUC 0.88 (95%CI 0.82–0.93). Thirty two TBI patients (30%) had lesions on CT. The AUC for discriminating those patients with CT lesions versus those without CT lesions was 0.79 (95%CI 0.69–0.89). Moreover, the ROC curve for distinguishing NSI from no NSI yielded an AUC of 0.87 (95%CI 0.77–0.96).
Conclusions
GFAP-BDP is detectable in serum within an hour of injury and is associated with measures of injury severity including the GCS score, CT lesions and neurosurgical intervention. Further study is required to validate these findings before clinical application.
Keywords: Traumatic Brain Injury, head injury, trauma, human, biomarkers, proteomics, diagnostic, Serum, Computed Tomography, neurosurgical intervention, sensitivity, specificity
INTRODUCTION
Background
Traumatic brain injury (TBI) is a significant cause of death and disability in the United States1 with 52,000 annual deaths and 5.3 million impaired by its effects. Each year in the United States there are at least 1.7 million people who sustain a TBI with1.4 million of these treated and released from emergency departments across the country.2 Traumatic brain injury is a leading cause of combat casualty with an estimated 15–25% of all injuries sustained in 20th century conflicts being to the head.3–5 Tools to diagnose and triage brain injury victims would be useful in both civilian and military settings. Accurate diagnosis in acute care environments is critical to patient outcome. Such decisions include performing Computed Tomography (CT) scans of the brain, seeking neurosurgical consultation, admitting or transferring to a higher level of care, returning to play or duty, and averting the consequences of “second impact syndrome,”6, 7 when repeated concussions in a short period become potentially debilitating or fatal.
Importance
Conventionally, early risk stratification of brain injury is based on CT scanning.8–10 According to recent estimates, 62 million CT scans are performed annually in the US.11 While increasing CT use has improved diagnostic capabilities and reduced hospital admissions,12 it has also raised concern over unnecessary exposure to ionizing radiation.13–17 Some studies suggest that CT scans of the head may be among the largest contributors to radiation exposure due to the frequency with which they are performed.18, 19 Moreover, in the United States there is a very high rate of ordering CT scans for mild TBI (also known as concussion) that is fostered by the nature of ED practice: high case volumes, brief physician-patient contact, uncertain follow-up, and fear of medicolegal repercussions.20 Yet, emergency departments with a high ordering rate of head CT scans can still miss intracranial injuries.21, 22 Furthermore, more subtle lesions or diffuse injury may not be evident on CT acutely.23–26
Unlike other organ-based diseases, such as myocardial ischemia, where rapid serum-based biomarkers prove invaluable to guide diagnosis and treatment, there are no such rapid, definitive diagnostic neurochemical markers for TBI that quantify the gravity of the injury. There have been a number of biomarkers assessed in TBI.27 The most extensively studied among these include glial protein S-100 beta(β)28–32, neuron-specific enolase (NSE)33–36, and myelin basic protein (MBP)37–40 Although some of these published studies suggest that these biomarkers correlate with degree of injury; there are conflicting results.41–46
Glial Fibrillary Acidic Protein (GFAP) is a monomeric intermediate protein found in astroglial skeleton that was first isolated by Eng et al. in 1971.47 GFAP is found in white and gray brain matter and is strongly upregulated during astrogliosis.48 Current evidence indicates that serum GFAP might be a useful marker for various types of brain damage from neurodegenerative disorders49, 50 and stroke51 to severe traumatic brain injury.52–57 Recently, Vos et al. described serum GFAP profile in severe and moderate TBI (GCS <12)31 but there are no published studies on profiling serum GFAP levels following mild TBI.
Goals of This investigation
Recently we became aware that GFAP appears highly vulnerable to proteolytic modifications in vitro and in vivo and confirmed that the form of GFAP in biofluids is likely to be breakdown product (BDP) of GFAP.58–60 This study examined whether GFAP-BDP was significantly elevated in the serum of mild and moderate TBI patients compared to controls. Additionally, this study examined the relationship between GFAP-BDP levels and measures of acute injury severity such as GCS, traumatic intracranial lesions on CT scan and neurosurgical intervention.
MATERIALS AND METHODS
Study Design
This prospective controlled cohort study enrolled a convenience sample of adult patients with suspected TBI following blunt head trauma presenting to the emergency department within 4 hours of injury with a GCS of 9 to 15. Trauma control patients were enrolled simultaneously.
Setting
Study sites included the Emergency Departments (ED) of three Level I Trauma Centers; Shands at University of Florida in Gainesville, Florida; Orlando Regional Medical Center in Orlando, Florida; and Washington University in St. Louis, Missouri. This study was approved by the respective Institutional Review Boards (IRB) of each institution. Written informed consent was obtained from patients and/or legal authorized representatives prior to enrollment. In the event the patient was unable to consent for themselves and a legal authorized representative was not present or reachable, the IRB granted permission to collect initial samples using delayed 24-hour consent. Consent was required within 24 hours of being deemed eligible. Delayed consent was rarely required.
Selection of Participants
Eligibility for suspected mild TBI was determined by the treating physician based on the history of blunt head trauma followed by either loss of consciousness, amnesia, or disorientation61 and presenting to the emergency department within 4 hours of injury with a GCS of 9 to 15. Head CT Scans were performed at the discretion of the treating physician. Patients were excluded if: 1) they were less than 18 years old; 2) there was no history of trauma as their primary event (e.g. syncope or seizure); 3) they had known dementia, chronic psychosis or active CNS pathology; or 4) were pregnant.
There were two control groups: 1) normal adult volunteers without any acute injuries who responded to advertisements in a local flyer; 2) non-head injured patients presenting to the emergency department with either a single limb orthopedic injury or following a motor vehicle collision without blunt head trauma. The mechanisms of injury for the orthopedic controls included falls, crush injuries, or direct impact to a limb resulting in a single limb fracture and/or dislocation. There could be no other concomitant injuries. Orthopedic controls could be exposed to significant forces but could not be in a motorized vehicle.
Trauma control patients had a normal mental status at the time of enrollment and had no evidence of acute brain injury or hemodynamic instability and were enrolled during the same period as TBI patients were enrolled. These controls were carefully screened to ensure they had no blunt head trauma and no symptoms of brain injury, including no loss of consciousness, no amnesia and no alteration in sensorium at any time after injury. The purpose of including non-head injured trauma controls was to examine biomarker levels in patients who were exposed to the acceleration and deceleration forces without blunt trauma.
Data Collection and Processing
All initial patient assessments were made by board certified emergency medicine physicians trained by a formal one-hour session on evaluating patient eligibility. At the time of enrollment, the study team carefully reassessed every patient to ensure each patient met inclusion criteria and verified any exclusions. Any finding of loss of consciousness, amnesia or disorientation had to be documented in the medical record for the patient to be enrolled. Blood samples were obtained from each TBI and non-head injured trauma control shortly after arrival to the ED and within 4 hours of the reported time of injury. There was only one serum GFAP-BDP biomarker level analyzed per patient in the 4-hour post-injury period. A single vial of approximately 5mL of blood was collected and placed in clot tubes with a serum separator and allowed to clot at room temperature. The blood was centrifuged within 30 minutes and the serum was placed in bar-coded aliquot containers and stored in a freezer at −70 degrees Celsius until it was transported to a central laboratory (Banyan Biomarkers Inc.). There, the samples were analyzed in batches using a sandwich enzyme-linked immunosorbent assay (ELISA) to GFAP-BDP. Reports of the assay results were sent after the lab had received a given quota. After assessment and treatment in the emergency department, patients were either discharged home or admitted to hospital based on severity of their injuries and patient management was not altered by the study. Blood sampling and handling in uninjured normal controls was conducted in the same manner.
Patients underwent standard CT scan of the head according to the judgment of the treating physician. The CT scan ordering pattern at the participating Level I trauma centers is such that most patients with blunt head injury with subsequent symptoms have a head CT scan performed as part of usual care. In some instances, physicians ordered CT scans of the head on trauma controls based on mechanism or clinical circumstances. CT examinations of each TBI patient were interpreted by board-certified radiologists who recorded location, extent and type of brain injury. Radiologists were blinded to the study protocol but had the usual clinical information. Lab personnel running the samples were blinded to the clinical data.
Biomarker Analysis
When a full length purified recombinant human GFAP is subjected to in vitro treatment with calpain, it is processed to mainly 42kD and 38kD breakdown products (BDPs).59, 60 To construct a GFAP-BDP specific sandwich ELISA, many mouse monoclonal antibodies (Mab) raised against GFAP and it BDP’s were actively screened. Full length GFAP was almost undetected, as determined by probing with human GFAP in cell lysate with or without calpain digestion in vitro. However, one identified Mab IgG (clone 2H12) detected GFAP breakdown products (BDP’s) and this antibody was used as the capture antibody for the ELISA. In contrast, a rabbit polyclonal antibody (Pab) raised against the midsection of full length GFAP detected both full length human GFAP (50K) and its major BDP’s (42K, 38K) with high affinity. Since the capture Mab 2H12 provided the required specificity for GFAP-BDP, the Pab served as the detection antibody, Using this antibody pair and denatured recombinant GFAP as BDP-mimic, a GFAP-BDP specific ELSIA was constructed. The intra-assay Coefficient of Variance (CV) was 4.3% to 7.8% while the inter-assay CV was 7.8% to 14.3% from high to low concentration. The limit of detection (LOD) within the linear dynamic range was determined to be 0.020 ng/mL. Samples with undetectable (ND) levels of GFAP-BDP were assigned a value of 50% of the lower limit of detection (i.e. ND=0.010 ng/mL). Any samples yielding a signal over the quantification range was diluted and re-assayed.
Outcome measures
The primary outcome measure tested the ability of GFAP-BDP to distinguish patients with mild and moderate TBI from those without TBI (normal uninjured controls) and assessed the relationship to non-head injured trauma controls. The secondary outcome measures tested the ability of GFAP-BDP to distinguish between different levels of injury severity. These severity measures included: 1) Glascow Coma Score (GCS) scores 62, 63 obtained at presentation to the emergency department; 2) the presence of intracranial lesions on initial CT scan; and 3) having a neurosurgical intervention. Intracranial lesions on CT included any acute traumatic intracranial lesions visualized on CT scan. Neurosurgical intervention was defined as either death within 7 days secondary to head injury or the need for any of the following procedures within 7 days: craniotomy, elevation of skull fracture, intracranial pressure monitoring, or intubation for head injury.64, 65
Primary Data Analysis
Descriptive statistics with means and proportions were used to describe the data. For statistical analysis, biomarker levels were treated as continuous data, measured in ng/ml and expressed as means (±95%CI). Data were assessed for equality of variance and distribution. Logarithmic transformations were conducted on non-normally distributed data. Group comparisons for different GCS Scores were performed using analysis of variance with multiple comparisons using Games-Howell post-hoc test. Receiver Operating Characteristics (ROC) curves were created to explore the ability of the biomarker to distinguish between controls and TBI patients within 4 hours of injury, as well as for intracranial lesions on CT scan and neurosurgical intervention. Estimates of the area under these curves (AUC) were obtained (AUC=0.5 indicates no discrimination and an AUC=1.0 indicates a perfect diagnostic test). GFAP-BDP cutpoints were selected to maximize the sensitivity and correctly identify as many patients with CT lesions and neurosurgical intervention as possible. Classification performance was assessed by sensitivity, specificity, positive and negative predictive values with 95% confidence intervals. All analyses were performed using the statistical software package PASW 17.0 (IBM Corporation®, Somers NY).
A pilot study provided preliminary data to calculate a sample size for distinguishing TBI patients with a positive CT versus a negative CT. A sample of 28 from the positive CT group and 28 from the negative CT group achieve 80% power to detect a difference of 0.10 between the area under the ROC curve AUC0 (for GFAP) under the null hypothesis of 0.89 and an AUC1 (for standard CT) under the alternative hypothesis of 0.99 using a two-sided z-test at a significance level of 0.05.
RESULTS
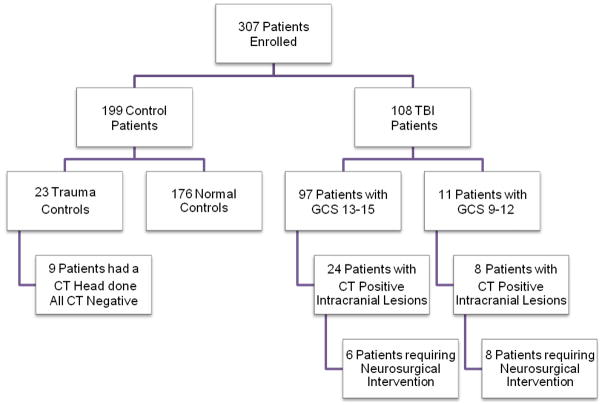
A total of 307 patients were enrolled in the study and had serum samples drawn within 4 hours of injury for analysis. There were 108 TBI patients: 97 with GCS 13–15 and 11 with GCS 9–12; and 199 controls: 176 normal controls with no injuries and 23 trauma controls who had peripheral injuries without TBI (16 MVC controls and 7 orthopedic controls). The flow diagram in Figure 1 describes the distribution of enrolled patients. CT scan of the head was performed in all TBI patients and traumatic intracranial lesions on CT scan were evident in 32 (30%): 24 (75%) of patients presented with a GCS 13–15 and 8 (25%) with GCS 9–12. A CT scan was also performed in 9 trauma control patients despite the patients’ lack of signs or symptoms of TBI – no blunt trauma, no loss of consciousness, no amnesia and no alteration in sensorium at any time after injury. These CT’s were performed at the discretion of the treating physician based on mechanism or clinical circumstances and none of them showed any signs of traumatic intracranial lesions. Neurosurgical intervention was performed on 14 patients (13%), 6 (43%) presented with a GCS 13–15 and 8 (57%) with GCS 9–12.
Figure 1. Flow diagram of enrolled patients.
Flow diagram showing the number of all TBI and control patients enrolled.
There were 25 TBI subjects enrolled from the University of Florida, 53 from Orlando Regional Medical Center and 30 from Washington University. The distribution of clinical characteristics for each site is presented in Table 1. There were no statistically significant differences in the demographic characteristics of the controls (normal and trauma) and TBI patients for age or gender (Table 1).
Table 1. Demographic and clinical data for all subjects included in the study.
The table describes data from patients enrolled overall and at each center.
| TBI | CONTROL | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Characteristics | Total N=108 |
University of Florida N=25 |
Orlando Regional Medical Center N=53 |
Washington University N=30 |
Normal Controls N=176 |
Trauma Controls N=23 |
|
| ||||||
| Mean age (yrs±SD) | 39 (±15) | 35 (±15) | 39 (±15) | 44 (±16) | 37 (±14) | 44 (±17) |
|
| ||||||
| Range | (18–89) | (18–61) | (19–70) | (19–89) | (18–65) | (19–83) |
|
| ||||||
| Gender (%) Male | 70 (65) | 16 (64) | 34 (64) | 20 (67) | 93 (53) | 16 (70) |
|
| ||||||
| GCS Score in ED (%) | ||||||
| GCS 9–12 | 11 (10) | 5 (20) | 3 (6) | 3 (10) | 0 (0) | 0 (0) |
| GCS 13–15 | 97 (90) | 20 (80) | 50 (94) | 27 (90) | 176 (100) | 23 (100) |
|
| ||||||
| Mechanism of Injury | ||||||
| Motor Vehicle Crash | 45 (42) | 15 (60) | 25 (47) | 5 (17) | 0 (0) | 16 (70) |
| Fall | 24 (22) | 3 (12) | 7 (13) | 14 (46) | 0 (0) | 2 (9) |
| Motorcycle | 14 (14) | 2 (8) | 11 (21) | 1 (3) | 0 (0) | 0 (0) |
| Pedestrian Struck | 7 (7) | 2 (8) | 3 (6) | 2 (7) | 0 (0) | 1 (4) |
| Bicycle | 6 (6) | 0 (0) | 4 (7) | 2 (7) | 0 (0) | 0 (0) |
| Hit with blunt object | 4 (3) | 0 (0) | 1 (2) | 3 (10) | 0 (0) | 0 (0) |
| Assault | 4 (3) | 0 (0) | 2 (4) | 2 (7) | 0 (0) | 0 (0) |
| Sports/Other | 4 (3) | 3 (12) | 0 (0) | 1 (3) | 0 (0) | 4 (17) |
|
| ||||||
| Loss of Consciousness (%) | ||||||
| Yes | 77 (71) | 16 (64) | 43 (81) | 18 (60) | 0 (0) | 0 (0) |
| No | 25 (23) | 6 (24) | 10 (19) | 9 (30) | 176 (100) | 23 (100) |
| Unknown | 6 (6) | 3 (12) | 0 (0) | 3 (10) | 0 (0) | 0 (0) |
|
| ||||||
| Amnesia (%) | 43 (40) | 9 (36) | 23 (43) | 11 (37) | 0 (0) | 0 (0) |
|
| ||||||
| Admitted to Hospital (%) | 66 (61) | 23 (92) | 27 (51) | 16 (53) | 0 (0) | 10 (43) |
|
| ||||||
| Intoxicated (Alcohol or Drugs) | 13 (12) | 7 (28) | 4 (8) | 2 (7) | - | 1 (4) |
|
| ||||||
| Neurosurgical Intervention | 14 (13) | 5 (20) | 8 (15) | 1 (3) | - | 0 (0) |
|
| ||||||
| Traumatic Intracranial Lesions on CT Scan of Head | 32 (30) | 10 (40) | 12 (23) | 10 (33) | - | 0 (0) |
|
| ||||||
| Lesion Types on CT Head | ||||||
| Epidural hematoma | 3 (9) | 1 (10) | 1 (8) | 1 (10) | 0 (0) | |
| Subdural hematoma | 7 (22) | 0 (0) | 1 (8) | 6 (60) | 0 (0) | |
| Subarachnoid hemorrhage | 8 (25) | 3 (30) | 3 (25) | 2 (20) | - | 0 (0) |
| Contusion | 3 (9) | 3 (30) | 0 (0) | 0 (0) | 0 (0) | |
| Intracerebral hemorrhage | 1 (3) | 0 (0) | 1 (8) | 0 (0) | 0 (0) | |
| Pneumocephalus | 2 (7) | 0 (0) | 2 (2) | 0 (0) | 0 (0) | |
| Combination of lesions | 8 (25) | 3 (10) | 4 (33) | 1 (10) | 0 (0) | |
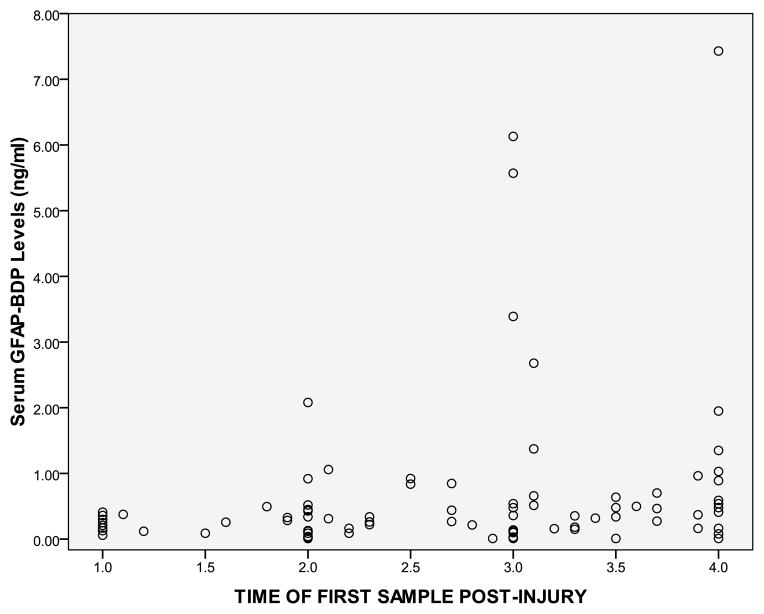
Both the TBI and trauma controls had serum samples drawn within 4 hours of injury with the average time from injury to serum sample collection at 2.7 hours (95%CI 2.5–2.9). The average time to serum collection for TBI patients was 2.6 hours (95%CI 2.4–2.9); for orthopedic controls it was 2.5 hours (95%CI 1.9–3.2); and for MVC controls it was 3.2 (95%CI 2.7–3.7). The temporal profile of GFAP-BDP in TBI patients within 4 hours post-injury is shown in Figure 2. GFAP-BDP demonstrated a rapid appearance in serum post-injury with levels detectible within an hour of injury. Some of the higher levels were seen starting at approximately 2 hours post-injury. There was a significant difference in the levels of GFAP-BDP between all TBI patients and all controls. A comparison of mean, median and log transformed serum levels of GFAP-BDP between various control groups and TBI groups are presented in Table 2.
Figure 2. Temporal profile of GFAP-BDP in TBI patients within 4 hours of injury.
The dots represent levels of GFAP-BDP (ng/ml) at different times post-injury. GFAP-BDP demonstrated a rapid appearance in serum post-injury with levels detectible within an hour of injury.
Table 2. Description of GFAP-BDP levels in the different groups.
Description of median, mean, and log transformed mean of serum GFAP-BDP levels in the different groups.
| Median [IQR] (ng/ml) | Mean (95%CI) (ng/ml) | SD (ng/ml) | Log transformed Mean (95%CI) | |
|---|---|---|---|---|
|
| ||||
| All TBI | 0.316 [0.600] | 0.893 (0.573, 1.213) | 1.677 | −1.300 (−1.618, −0.982) |
|
| ||||
| All Controls | 0.010 [0.060] | 0.057 (0.044, 0.071) | 0.098 | −3.72 (−3.889,−3.554) |
|
| ||||
| TBI | ||||
| GCS 15 (n=77) | 0.268 [0.420] | 0.5331 (0.259, 0.807) | 1.206 | −1.614 (−1.961, −1.266) |
| GCS 14 (n=18) | 0.223 [1.132] | 1.130 (0.147, 2.113) | 1.976 | −1.080 (−1.887, −0.273) |
| GCS 13 (n=2) | 0.510 | 0.510 (0, 5.465) | 0.552 | −1.113 (−13.91, 11.69) |
| GCS 12 (n=2) | 0.455 | 0.455 (0, 5.982) | 0.615 | −2.014 (−26.13, 22.10) |
| GCS 11 (n=1) | - | 7.41 | - | 2.003 |
| GCS 10 (n=0) | - | - | - | - |
| GCS 9 (n=8) | 2.923 [3.467] | 3.208 (1.586, 4.830) | 1.940 | 0.948 (0.291, 1.606) |
|
| ||||
| Uninjured Controls | 0.010 [0.050] | 0.038 (0.029, 0.047) | 0.059 | −3.902 (−4.054, −3.750) |
|
| ||||
| Ortho Controls | 0.216 [0.275] | 0.203 (0.048, 0.357) | 0.167 | −2.274 (−3.776, −0.771) |
|
| ||||
| MVC Controls | 0.122 [0.373] | 0.204 (0.102, 0.306) | 0.191 | −2.371 (−3.196, −1.546) |
In Figure 3a levels of GFAP-BDP in normal and trauma controls are shown relative to 3 groups of GCS score divided as GCS 15, GCS 13–14, and GCS 9–12. There were statistically significant differences between each of the groups relative to the uninjured controls (as noted by the asterisks). In particular, when patients with an ED GCS score of 15 were isolated from the TBI group, early serum GFAP-BDP levels were significantly different between patients with a GCS 15 versus trauma controls (Figure 3b). When we dichotomized the GCS score into the traditional GCS 13–15 versus GCS 9–12 there were significant differences between the groups (Figure 3c). Additionally, when we dichotomized the GCS score into GCS 14–15 versus GCS 9–13 there were also statistically important differences between the groups (Figure 3d).
Figures 3a, 3b, 3c, & 3d.
Figure 3a. A comparison of serum levels of GFAP-BDP drawn within 4 hours of injury in TBI patients with different GCS scores versus normal and trauma controls. GCS scores were divided as GCS 15, GCS 13–14, and GCS 9–12. There are 3 control groups: i- non-injured, ii- non-head injured orthopedic controls, and iii- non-head injured controls from motor vehicle collisions. There are statistically significant differences between the uninjured controls and each of the groups (indicated by the asterisk “*”) and serum levels of GFAP-BDP increased incrementally with worsening GCS scores. Boxplots represent medians in ng/ml and interquartile ranges.
Figure 3b. A comparison of serum levels of GFAP-BDP drawn within 4 hours of injury in TBI patients with GCS 15 versus trauma controls. When TBI patients with an ED GCS score of 15 are isolated from the TBI group early GFAP-BDP levels demonstrate significant differences between patients with a GCS 15 versus trauma controls. Boxplots represent medians in ng/ml and interquartile ranges.
Figure 3c. A comparison of serum levels of GFAP-BDP in TBI patients with GCS dichotomized into GCS 13–15 versus GCS 9–12. When TBI patients are dichotomized into the traditional GCS 13–15 versus GCS 9–12, early GFAP-BDP levels are significantly different between the 2 groups. Boxplots represent medians in ng/ml and interquartile ranges.
Figure 3d. A comparison of serum levels of GFAP-BDP in TBI patients with GCS dichotomized into GCS 14–15 versus GCS 9–13. When TBI patients are dichotomized into the more recently suggested dichotomy of GCS 14–15 versus GCS 9–13, early GFAP-BDP levels are significantly different between the 2 groups. Boxplots represent medians in ng/ml and interquartile ranges.
* Statistically significant difference
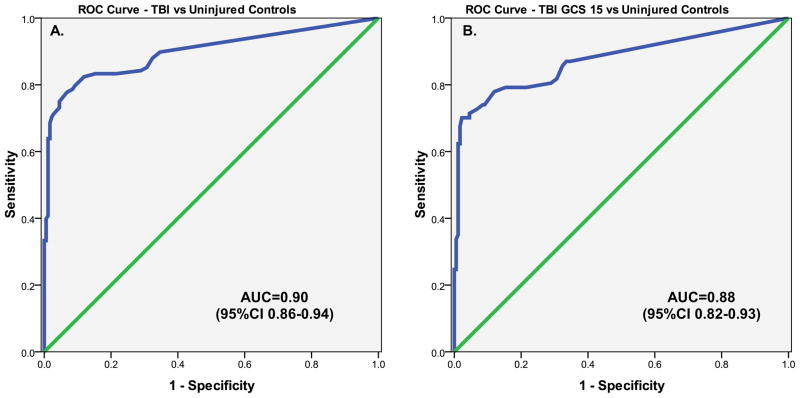
Area under the curve (AUC) was calculated from the ROC curves constructed to assess the performance of early GFAP-BDP levels in TBI versus control patients. ROC curves demonstrated that early GFAP-BDP levels were able to distinguish TBI from uninjured controls with an AUC of 0.90 (95%CI 0.86–0.94)(Figure 4a). More specifically, GFAP-BDP was able to differentiate TBI patients with a GCS 15 from normal controls with an AUC 0.88 (95%CI 0.82–0.93)(Figure 4b).
Figures 4a & 4b.
Figure 4a. ROC Curve for distinguishing TBI versus uninjured controls. The area under the ROC curve (AUC) demonstrates that early GFAP-BDP levels are able discriminate between patients without injuries from patients with TBI with an AUC 0.90 (95%CI 0.86–0.94).
Figure 4b. ROC Curve for distinguishing TBI patients with a GCS 15 versus uninjured controls. TBI Patients with a GCS 15 are isolated from the group and compared to uninjured controls. Early GFAP-BDP levels are able discriminate between patients without injuries from TBI patients with a GCS 15 with an AUC 0.88 (95%CI 0.82–0.93).
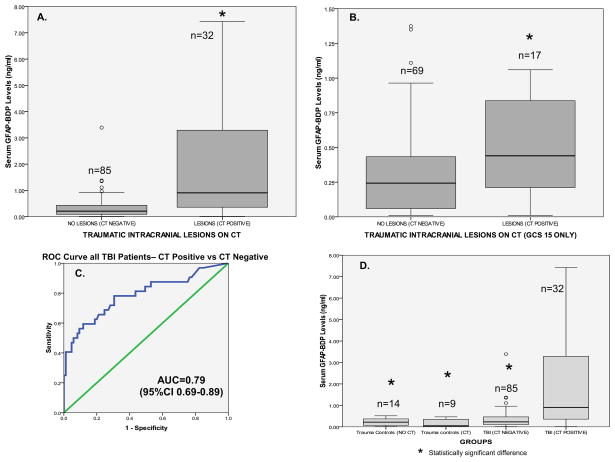
When serum levels of GFAP-BDP were compared in patients with traumatic intracranial lesions on CT scan (CT positive) to those without CT lesions (CT negative), levels were significantly higher in those with lesions on CT scan (Figure 5a). Patients with GCS 15 were assessed independently and serum GFAP-BDP levels were significantly more elevated in those with CT scan lesions than those without (Figure 5b). The area under the curve for discriminating between CT scan positive and CT scan negative intracranial lesions was 0.79 (95%CI 0.69–0.89)(Figure 5c). Figure 5d shows GFAP-BDP levels in the 16 trauma controls having no CT performed versus the 9 trauma control patients who had CT scans of the head ordered by their treating physician despite lack of TBI symptoms. There was no difference in GFAP-BDP levels between the trauma controls who did or did not have CT scans performed. TBI patients with a negative CT had significantly higher levels of GFAP-BDP than trauma controls with a negative CT. Most notable was that GFAP-BDP levels were significantly elevated in patients with traumatic intracranial lesions on CT (CT positive) than those without CT lesions (CT negative) (significantly different from each group) regardless of whether they were trauma controls or TBI.
Figures 5a, 5b & 5c.
Figure 5a. Boxlplot comparing serum GFAP-BDP levels drawn within 4 hours of injury in patients with and without traumatic intracranial lesions on CT. Levels of serum GFAP-BDP are significantly higher in patients with traumatic intracranial lesions on CT (CT positive) than those without CT lesions (CT negative). Bars represent medians in ng/ml and interquartile ranges.
Figure 5b. Boxplot comparing serum GFAP-BDP levels drawn within 4 hours of injury in patients with and without traumatic intracranial lesions on CT in TBI patients with GCS 15. In a subset of TBI patients with a GCS 15 levels of serum GFAP-BDP are significantly higher in those with traumatic intracranial lesions on CT (CT positive) than those without CT lesions (CT negative). Bars represent medians in ng/ml and interquartile ranges.
Figure 5c. ROC Curve for distinguishing CT positive versus CT negative patients. The area under the ROC curve (AUC) demonstrates that early GFAP-BDP levels are able discriminate between patients with and without traumatic intracranial lesions on CT (AUC 0.79; 95%CI 0.69–0.89).
Figure 5d. Boxplot comparing serum GFAP-BDP levels drawn within 4 hours of injury in patients with and without traumatic intracranial lesions on CT in both TBI and trauma controls. GFAP-BDP levels are significantly higher in patients with traumatic intracranial lesions on CT (CT positive) than those without CT lesions (CT negative) regardless of whether they are trauma controls or TBI. Bars represent medians in ng/ml and interquartile ranges.
* Statistically significant difference
Additionally, we compared serum levels of GFAP-BDP in patients who had a neurosurgical intervention versus those who received no such intervention. Substantially higher serum levels were detected in those who had a neurosurgical intervention (Figure 6a). The ROC curve for discriminating between those having and not having a neurosurgical intervention yielded an AUC of 0.87 (95%CI 0.77–0.96)(Figure 6b).
Figures 6a, 6b.
Figure 6a. Boxplot comparing serum GFAP-BDP levels drawn within 4 hours of injury in patients with neurosurgical intervention versus those without intervention. Levels of serum GFAP-BDP are significantly higher in patients with who had neurosurgical intervention versus those who did not. Bars represent medians in ng/ml and interquartile ranges.
Figure 6b. ROC Curve for distinguishing those who had a neurosurgical intervention versus those who did not. The area under the ROC curve (AUC) demonstrates that early GFAP-BDP levels are able discriminate between patients with who required neurosurgical intervention versus those who did not (AUC 0.87; 95%CI 0.77–0.96).
* Statistically significant difference
Cutoff points for GFAP-BDP were derived from the ROC Curves for detecting intracranial lesions on CT scan and having a neurosurgical intervention. The aim of this exploratory analysis was to maximize the sensitivity and correctly classify all CT positive lesions and all those with a neurosurgical intervention. Classification performance for detecting intracranial lesions on CT at a GFAP-BDP cutoff level of 0.035 ng/ml yielded a sensitivity of 97% (95%CI 82–100), a specificity of 18% (95%CI 11–28) and a negative predictive value of 94% (95%CI 68–100)(Table 3a). Classification performance for predicting neurosurgical intervention at a GFAP-BDP cutoff level of 0.17 ng/ml yielded a sensitivity of 100% (95%CI 73–100), a specificity of 42% (95%CI 32–52) and a negative predictive value of 100% (95%CI 90–100)(Table 3b).
Table 3a. & 3b.
Contingency table and Classification Performance of Serum GFAP-BDP in detecting Intracranial Lesions on CT and Contingency table and Classification Performance of Serum GFAP-BDP in detecting Need for Neurosurgical Intervention
| CT positive | CT negative | Sensitivity | 97% (82–100) | |
|---|---|---|---|---|
| GFAP-BDP positive ≥0.035 ng/ml | 31 | 70 | Specificity | 18% (11–28) |
| GFAP-BDP negative <0.035 ng/ml | 1 | 15 | NPV | 94% (68–100) |
| PPV | 31% (22–41) |
| Neurosurgical Intervention | No Neurosurgical Intervention | Sensitivity | 100% (73–100) | |
|---|---|---|---|---|
| GFAP-BDP positive ≥0.17 ng/ml | 14 | 60 | Specificity | 42% (32–52) |
| GFAP-BDP negative <0.17 ng/ml | 0 | 43 | NPV | 100% (90–100) |
| PPV | 19% (11–30) |
LIMITATIONS
While these data are encouraging, the authors recognize there are limitations to this study. The current study was performed in a limited cohort of patients with mild and moderate TBI, a disease that tends to be heterogeneous in nature. Patients were enrolled as a convenience sample because research team members could not be on duty 24/7. Despite this, patients were recruited consecutively when research assistants were on duty including on weekends and nights so a representative sample could be enrolled.
We used very strict criteria for defining suspected TBI subjects and control subjects. This may have limited the clinical applicability of our findings in trauma patients. Our definition specified that the patient had to have blunt head trauma followed by either loss of consciousness, amnesia, or disorientation. However, there were nine control patients who physicians felt sufficiently concerned about to order a head CT on, despite the lack of clinical signs and symptoms of TBI. We attempted to adjust for this by adding these nine trauma controls to our analysis of CT and neurosurgical intervention in order to reflect actual practice and improve the clinical applicability of our findings. Future studies should consider testing the biomarker in its intended setting which includes any patient with suspected TBI following trauma based on the judgment of the treating physician.
At this time we cannot confirm that GFAP-BDP is entirely CNS specific and not released from other organs. However, its ability to distinguish between TBI and controls is encouraging. Injured controls were exposed to significant non-trivial trauma and they served as robust comparators for the TBI patients. Current studies of patients with multi-trauma will further address the effect of extracranial injuries on GFAP-BDP values. Additionally, analysis on the biokinetics and temporal profile of GFAP-BDP are being conducted that will give insight into pattern of release of GFAP-BDP over time and during different clinical circumstances. This will also help characterize the optimal timing of sampling after injury.
This study addressed severity of injury in the acute care setting and did not describe long-term outcome in these patients. Outcome data will be assessed as these data become available in our ongoing studies.
DISCUSSION
Although there are studies assessing GFAP in serum, these studies have looked primarily at patients with severe TBI.53–56 This clinical study is among the first to systematically assess early levels of GFAP-BDP in human serum in TBI patients with GCS 9–15. We elected to study both mild and moderate injury because initial GCS scores in the ED in this population can be surprisingly deceptive. The classification of a TBI as a mild or a moderate can change based on neuroimaging results and the presence of factors altering mental status such as intoxication, medications and other injuries. A patient with a GCS of 15 who has an acute bleed on CT scan can be classified as moderate. Conversely, a patient with a GCS of 11 who has no evidence of intracranial injury on CT scan can be classified as a mild. Although we studied TBI patients from GCS 9–15 we included focused analyses of those with a GCS score of 15.
Our group recently discovered that GFAP appears highly vulnerable to proteolytic modifications in vitro and in vivo and confirmed that the form of GFAP in biofluids is likely to be breakdown product (BDP) of GFAP.59, 60 GFAP has previously been studied rather limitedly as a possible protease substrate. Following TBI GFAP-BDP is likely a product of calpain over-activation, leading to its release from injured or degenerative glia cells. Therefore, it appears that GFAP-BDP’s are not only released during gliosis subacutely but appears within hours after glial damage from TBI. Thus, in addition to the clinical correlations this new biochemical finding adds to the significance of the interpretation of these biomarker levels after brain injury.
Much of the previous work on biomarkers in mild TBI has been limited by factors such as wide variations in sample collection times and inadequate control groups. When we designed the study we carefully considered these limitations. To overcome the sample schedule shortfall we restricted sample collection to within 4 hours of injury to reflect actual clinical practice and measure GFAP-BDP as soon after injury as possible. Additionally, we incorporated three different control groups in this study. Uninjured controls represented the general population and non-head injured trauma controls had either orthopedic injuries or exposure to the forces of motor vehicle crashes. This allowed for a robust comparison of the biomarker levels between TBI and various controls and reflects how it would be used in a real-time clinical setting for trauma patients. Many trauma controls were exposed to significant trauma including the acceleration-deceleration vectors of motor vehicle crashes and falls from heights over 5 feet. Their injuries paralleled TBI patients except for their lack of both blunt head trauma and TBI symptoms. The fact that trauma controls had significantly higher levels of GFAP-BDP’s than uninjured controls may reflect the force of the mechanism. To our advantage, in nine trauma patients the mechanism was so significant that physicians actually ordered head CT’s as part of their clinical care despite the lack of blunt head injury and the lack of signs and symptoms of brain injury. This allowed us to assess levels of GFAP-BDP in CT negative trauma controls against trauma controls without CT and CT negative TBI patients. TBI patients with a negative CT had higher levels than trauma controls, regardless of having a CT done. More importantly, the largest elevation in GFAP-BDP occurred in those with traumatic intracranial lesions on CT, regardless of GCS or the type of trauma control.
This provides a unique glimpse of GFAP-BDP levels in clinically apparent TBI from non-TBI trauma or, at least, non-clinically apparent TBI. Ongoing studies by our group are assessing long-term outcomes in these patients which will ultimately determine the true impact of the TBI on patient outcome. A large number of normal controls were included to facilitate the development of appropriate normative data.
Also unique to this study is that the majority of serum samples were obtained very early post-injury when patients first arrived in the emergency department. GFAP-BDP demonstrated a rapid appearance in serum post-injury with levels detectible in less than an hour of injury. Levels rose incrementally with severity of injury. They were either undetectable or in very low levels in normal controls, slightly higher in trauma controls, significantly elevated in TBI patients with a GCS 15 and were seen in its highest levels in TBI subjects with a positive CT.
Such acute elevations of this biomarker can make it a potentially useful clinical tool for determining injury severity early in the course after injury. Potential applications could include influencing the decision to image patients who are intoxicated or sedated, determining the degree brain injury in a multiple trauma victim, seeking neurosurgical consultation or making transport decisions about transfer to a neurosurgical facility.
Concerns over exposure to ionizing radiation from CT scans13–17 has led to calls for judicious use of such tests.66, 67 Evidently, high GFAP-BDP levels were associated with traumatic intracranial lesions on CT scan (CT positive), a finding which held true for patients with a GCS of 15 as well. If these findings can be validated, GFAP-BDP’s association with the presence of intracranial lesions on CT scans could help emergency and trauma physicians reduce the number CT’s they perform. Accordingly, GFAP-BDP could be incorporated into guidelines for neuroimaging decisions and decisions to transfer patients to neurosurgical facilities.
CONCLUSION
This study is among the first to systematically assess GFAP-BDP in human serum following mild and moderate TBI. We confirmed that the GFAP-BDP is present in human serum and that its levels are significantly elevated in this population using ELISA analysis, including those presenting with a GCS 15. GFAP-BDP is detectable in serum within a few hours of injury and is associated with measures of injury severity including the GCS score, CT lesions and neurosurgical intervention. This present work extends findings from studies in severe TBI. Further study is required to validate these findings before clinical application.
Acknowledgments
Grant Support
This study was supported in part by Department of Defense Award number DoD W81XWH-06-1-0517. Material has been reviewed by the Walter Reed Army Institute of Research. There is no objection to its presentation and/or publication. The opinions or assertions contained herein are the private views of the authors, and are not to be construed as official, or as reflecting true views of Department of the Army or Department of Defense.
The project described was supported in part by Award Number R01NS057676 from the National Institute of Neurological Disorders and Stroke. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders And Stroke or the National Institutes of Health.
A special thanks to Michael Walker, PhD for statistical advice and guidance on this manuscript.
Footnotes
Author Disclosure Statement
Drs. Papa, Brophy and Demery are consultants of Banyan Biomarkers, Inc. but receive no stocks or royalties from the company and will not benefit financially from this publication. Drs. Liu, Mo, Zhang, Mondello and Ms Akinyi are employees of Banyan Biomarkers, Inc. Drs. Wang and Hayes own stock, receive royalties from, and are officers of Banyan Biomarkers Inc., and as such may benefit financially as a result of the outcomes of this research or work reported in this publication.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Linda Papa, Email: lpstat@aol.com, Director of Academic Clinical Research, Orlando Health, Adjunct Professor, Department of Emergency Medicine, University of Florida, Associate Professor, Florida State University, College of Medicine, Associate Professor, University of Central Florida, College of Medicine, Attending Emergency Physician, Department of Emergency Medicine, Orlando Regional Medical Center, 86 W. Underwood (S-200), Orlando, Florida, 32806, Tel.: 407-237-6329, Fax: 407-649-3083.
Lawrence M. Lewis, Email: lewisl@wusm.wustl.edu, Associate Professor of Emergency Medicine and Medicine, Washington University School of Medicine, Division of Emergency Medicine, 660 South Euclid Avenue, Campus Box 8072, St. Louis, MO 63110, Tel.: (314) 758-6787, Fax: (314) 362-0478.
Jay L. Falk, Email: Jay.Falk@orlandohealth.com, Chief Academic Medical Officer, Orlando Health, Attending Emergency Physician, Orlando Regional Medical Center, 86 W. Underwood (S-200), Orlando, Florida, 32806, Tel.: 407-237-6324, Fax: 321-843-6058.
Zhiqun Zhang, Email: zzhang@banyanbio.com, Center of Innovative Research, Banyan Biomarkers Inc., 12085 Research Dr. Alachua, FL 32615, Tel.: (386) 518-6757, Fax: (386) 518-6811.
Salvatore Silvestri, Email: Sal.Silvestri@orlandohealth.com, Program Director, Emergency Medicine Residency, Attending Emergency Physician, Orlando Regional Medical Center, 86 W. Underwood (S-200), Orlando, Florida, 32806, Tel.: 407-237-6324, Fax: 321-843-6058.
Philip Giordano, Email: Philip.Giordano@orlandohealth.com, Corporate Director, Research Operations, Orlando Health, Attending Emergency Physician, Orlando Regional Medical Center, 86 W. Underwood (S-200), Orlando, Florida, 32806, Tel.: 407-237-6324, Fax: 321-843-6058.
Gretchen M. Brophy, Email: gbrophy@vcu.edu, Professor of Pharmacotherapy & Outcomes Science and Neurosurgery, Virginia Commonwealth University, Medical College of Virginia Campus, 410 N. 12th Street, PO Box 980533, Richmond, VA 23298-0533, Tel.: (804) 828-1201, Fax: (804) 828-8359.
Jason Demery, Email: jasondemery@gmail.com, Assistant Professor of Psychiatry, University of Florida Forensic Institute, Licensed Psychologist & Forensic Neuropsychologist, UF Springhill Health Center, 8491 NW 39th Ave., Gainesville, Florida 32606, Tel.: (352) 265-3284, Fax: (352) 265-3285.
Neha K. Dixit, Email: nehakdixit@gmail.com, NF/SG Veteran’s Health System, Psychology Service, 1601 SW Archer Road, Gainesville, FL 32610, Phone: 352-376-1611 Ext. 4820, Fax: 352-248-0260.
Ian Ferguson, Washington University School of Medicine, Division of Emergency Medicine, 660 South Euclid Avenue, Campus Box 8072, St. Louis, MO 63110, Tel.: (314) 362-9119, Fax: (314) 362-0419.
Ming Cheng Liu, Email: mcliu@banyanbio.com, Center of Innovative Research, Banyan Biomarkers Inc., 12085 Research Dr. Alachua, FL 32615, Tel.: (386) 518-6757, Fax: (386) 518-6811.
Jixiang Mo, Email: jmo@banyanbio.com, Center of Innovative Research, Banyan Biomarkers Inc., 12085 Research Dr. Alachua, FL 32615, Tel.: (386) 518-6757, Fax: (386) 518-6811.
Linnet Akinyi, Email: lakinyi@banyanbio.com, Center of Innovative Research, Banyan Biomarkers Inc., 12085 Research Dr. Alachua, FL 32615, Tel.: (386) 518-6757, Fax: (386) 518-6811.
Kara Schmid, Email: Kara.Schmid@us.army.mil, Walter Reed Army Institute of Research, Department of Applied Neurobiology, Division of Psychiatry and Neuroscience, Silver Spring, Maryland 20910, Tel.: (301) 319-9376.
Stefania Mondello, Email: smondello@banyanbio.com, Fellow, Center of Innovative Research, Banyan Biomarkers Inc., 13400 Progress Blvd., Alachua, FL 32615, Tel.: (386) 518-6713, Fax: (386) 518-6776, Alachua, Florida.
Claudia S. Robertson, Email: claudiar@bcm.tmc.edu, Professor, Department of Critical Care and Neurosurgery, Baylor College of Medicine, One Baylor Plaza, Houston, Texas 77030, Tel.: (713) 873-2792, Fax: (713) 798-8063.
Frank C. Tortella, Email: FRANK.C.TORTELLA@US.ARMY.MIL, Walter Reed Army Institute of Research, Department of Applied Neurobiology, Division of Psychiatry and Neuroscience, Silver Spring, Maryland 20910, Tel.: (301) 319-9687.
Ronald L. Hayes, Email: rhayes@banyanbio.com, Banyan Biomarkers Inc., 13400 Progress Blvd., Alachua, FL 32615, Tel.: (386) 518-6713, Fax: (386) 518-6776.
Kevin K. W. Wang, Email: kwang@banyanbio.com, Banyan Biomarkers Inc., 12085 Research Dr., Alachua, FL 32615, Tel.: (386) 518-6757, Fax: (386)-518-6811.
References
- 1.Consensus conference. Rehabilitation of persons with traumatic brain injury. NIH Consensus Development Panel on Rehabilitation of Persons With Traumatic Brain Injury. Jama. 1999;282(10):974–983. [PubMed] [Google Scholar]
- 2.Faul M, Xu L, Wald MM, Coronado VG. Emergency Department Visits, Hospitalizations and Deaths 2002–2006. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2010. [Accessed November 11, 2010]. Traumatic Brain Injury in the United States. http://www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf. [Google Scholar]
- 3.Carey ME. Analysis of wounds incurred by U.S. Army Seventh Corps personnel treated in Corps hospitals during Operation Desert Storm, February 20 to March 10, 1991. J Trauma. 1996 Mar;40(3 Suppl):S165–169. doi: 10.1097/00005373-199603001-00036. [DOI] [PubMed] [Google Scholar]
- 4.Sapsford W. Penetrating brain injury in military conflict: does it merit more research? J R Army Med Corps. 2003 Mar;149(1):5–14. doi: 10.1136/jramc-149-01-02. [DOI] [PubMed] [Google Scholar]
- 5.Okie S. Traumatic brain injury in the war zone. N Engl J Med. 2005 May 19;352(20):2043–2047. doi: 10.1056/NEJMp058102. [DOI] [PubMed] [Google Scholar]
- 6.Cantu RC. Return to play guidelines after a head injury. Clin Sports Med. 1998 Jan;17(1):45–60. doi: 10.1016/s0278-5919(05)70060-0. [DOI] [PubMed] [Google Scholar]
- 7.Erlanger DM, Kutner KC, Barth JT, Barnes R. Neuropsychology of sports-related head injury: Dementia Pugilistica to Post Concussion Syndrome. Clin Neuropsychol. 1999 May;13(2):193–209. doi: 10.1076/clin.13.2.193.1963. [DOI] [PubMed] [Google Scholar]
- 8.Jagoda AS, Bazarian JJ, Bruns JJ, Jr, et al. Clinical policy: neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. J Emerg Nurs. 2009 Apr;35(2):e5–40. doi: 10.1016/j.jen.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Stein SC, Fabbri A, Servadei F, Glick HA. A critical comparison of clinical decision instruments for computed tomographic scanning in mild closed traumatic brain injury in adolescents and adults. Ann Emerg Med. 2009 Feb;53(2):180–188. doi: 10.1016/j.annemergmed.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Gallagher CN, Hutchinson PJ, Pickard JD. Neuroimaging in trauma. Curr Opin Neurol. 2007 Aug;20(4):403–409. doi: 10.1097/WCO.0b013e32821b987b. [DOI] [PubMed] [Google Scholar]
- 11.Mettler FA, Jr, Thomadsen BR, Bhargavan M, et al. Medical radiation exposure in the U.S. in 2006: preliminary results. Health Phys. 2008 Nov;95(5):502–507. doi: 10.1097/01.HP.0000326333.42287.a2. [DOI] [PubMed] [Google Scholar]
- 12.Wardlaw JM, Keir SL, Seymour J, et al. What is the best imaging strategy for acute stroke? Health Technol Assess. 2004 Jan;8(1):iii, ix–x, 1–180. doi: 10.3310/hta8010. [DOI] [PubMed] [Google Scholar]
- 13.Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007 Nov 29;357(22):2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 14.Fayngersh V, Passero M. Estimating radiation risk from computed tomography scanning. Lung. 2009 May-Jun;187(3):143–148. doi: 10.1007/s00408-009-9143-9. [DOI] [PubMed] [Google Scholar]
- 15.Hall EJ, Brenner DJ. Cancer risks from diagnostic radiology. Br J Radiol. 2008 May;81(965):362–378. doi: 10.1259/bjr/01948454. [DOI] [PubMed] [Google Scholar]
- 16.Heilbrun ME, Chew FS, Tansavatdi KR, Tooze JA. The role of negative CT of the abdomen and pelvis in the decision to admit adults from the emergency department after blunt trauma. J Am Coll Radiol. 2005 Nov;2(11):889–895. doi: 10.1016/j.jacr.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 17.Livingston DH, Loder PA, Koziol J, Hunt CD. The use of CT scanning to triage patients requiring admission following minimal head injury. J Trauma. 1991 Apr;31(4):483–487. discussion 487–489. [PubMed] [Google Scholar]
- 18.Berrington de Gonzalez A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009 Dec 14;169(22):2071–2077. doi: 10.1001/archinternmed.2009.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brenner DJ. Slowing the increase in the population dose resulting from CT scans. Radiat Res. Dec;174(6):809–815. doi: 10.1667/RR1859.1. [DOI] [PubMed] [Google Scholar]
- 20.Long AE. Radiographic decision-making by the emergency physician. Emerg Med Clin North Am. 1985;3:437–446. [PubMed] [Google Scholar]
- 21.Stiell IG, Wells GA, Vandemheen K, et al. Variation in ED use of computed tomography for patients with minor head injury. Ann Emerg Med. 1997 Jul;30(1):14–22. doi: 10.1016/s0196-0644(97)70104-5. [DOI] [PubMed] [Google Scholar]
- 22.Ryu WH, Feinstein A, Colantonio A, Streiner DL, Dawson D. Regional variability in the use of CT for patients with suspected mild traumatic brain injury. Can J Neurol Sci. 2009 Jan;36(1):42–46. doi: 10.1017/s0317167100006296. [DOI] [PubMed] [Google Scholar]
- 23.Mac Donald CL, Johnson AM, Cooper D, et al. Detection of blast-related traumatic brain injury in U.S. military personnel. N Engl J Med. 2011 Jun 2;364(22):2091–2100. doi: 10.1056/NEJMoa1008069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mirvis SE, Shanmuganathan K. Trauma radiology: Part IV. Imaging of acute craniocerebral trauma. J Intensive Care Med. 1994 Nov-Dec;9(6):305–315. doi: 10.1177/088506669400900605. [DOI] [PubMed] [Google Scholar]
- 25.Lobato RD, Gomez PA, Alday R, et al. Sequential computerized tomography changes and related final outcome in severe head injury patients. Acta Neurochir (Wien) 1997;139(5):385–391. doi: 10.1007/BF01808871. [DOI] [PubMed] [Google Scholar]
- 26.Gaetz M. The neurophysiology of brain injury. Clin Neurophysiol. 2004 Jan;115(1):4–18. doi: 10.1016/s1388-2457(03)00258-x. [DOI] [PubMed] [Google Scholar]
- 27.Papa L, Robinson G, Oli M, et al. Use of Biomarkers for Diagnosis and Management of Traumatic Brain Injury Patients. Expert Opinion on Medical Diagnostics. 2008;2(8):937–945. doi: 10.1517/17530059.2.8.937. [DOI] [PubMed] [Google Scholar]
- 28.Woertgen C, Rothoerl RD, Holzschuh M, Metz C, Brawanski A. Comparison of serial S-100 and NSE serum measurements after severe head injury. Acta Neurochir (Wien) 1997;139(12):1161–1164. doi: 10.1007/BF01410977. discussion 1165. [DOI] [PubMed] [Google Scholar]
- 29.Romner B, Ingebrigtsen T, Kongstad P, Borgesen SE. Traumatic brain damage: serum S-100 protein measurements related to neuroradiological findings. J Neurotrauma. 2000 Aug;17(8):641–647. doi: 10.1089/089771500415391. [DOI] [PubMed] [Google Scholar]
- 30.Korfias S, Stranjalis G, Boviatsis E, et al. Serum S-100B protein monitoring in patients with severe traumatic brain injury. Intensive Care Med. 2007 Feb;33(2):255–260. doi: 10.1007/s00134-006-0463-4. [DOI] [PubMed] [Google Scholar]
- 31.Vos PE, Jacobs B, Andriessen TM, et al. GFAP and S100B are biomarkers of traumatic brain injury: an observational cohort study. Neurology. 2010 Nov 16;75(20):1786–1793. doi: 10.1212/WNL.0b013e3181fd62d2. [DOI] [PubMed] [Google Scholar]
- 32.Berger RP, Pierce MC, Wisniewski SR, Adelson PD, Kochanek PM. Serum S100B concentrations are increased after closed head injury in children: a preliminary study. J Neurotrauma. 2002 Nov;19(11):1405–1409. doi: 10.1089/089771502320914633. [DOI] [PubMed] [Google Scholar]
- 33.de Kruijk JR, Leffers P, Menheere PP, Meerhoff S, Twijnstra A. S-100B and neuron-specific enolase in serum of mild traumatic brain injury patients. A comparison with health controls. Acta Neurol Scand. 2001 Mar;103(3):175–179. doi: 10.1034/j.1600-0404.2001.103003175.x. [DOI] [PubMed] [Google Scholar]
- 34.Raabe A, Grolms C, Seifert V. Serum markers of brain damage and outcome prediction in patients after severe head injury. Br J Neurosurg. 1999 Feb;13(1):56–59. doi: 10.1080/02688699944195. [DOI] [PubMed] [Google Scholar]
- 35.Ross SA, Cunningham RT, Johnston CF, Rowlands BJ. Neuron-specific enolase as an aid to outcome prediction in head injury. Br J Neurosurg. 1996 Oct;10(5):471–476. doi: 10.1080/02688699647104. [DOI] [PubMed] [Google Scholar]
- 36.Naeimi ZS, Weinhofer A, Sarahrudi K, Heinz T, Vecsei V. Predictive value of S-100B protein and neuron specific-enolase as markers of traumatic brain damage in clinical use. Brain Inj. 2006 May;20(5):463–468. doi: 10.1080/02699050600664418. [DOI] [PubMed] [Google Scholar]
- 37.Berger RP, Adelson PD, Pierce MC, Dulani T, Cassidy LD, Kochanek PM. Serum neuron-specific enolase, S100B, and myelin basic protein concentrations after inflicted and noninflicted traumatic brain injury in children. J Neurosurg. 2005 Jul;103(1 Suppl):61–68. doi: 10.3171/ped.2005.103.1.0061. [DOI] [PubMed] [Google Scholar]
- 38.Wang KK, Ottens AK, Liu MC, et al. Proteomic identification of biomarkers of traumatic brain injury. Expert Rev Proteomics. 2005 Aug;2(4):603–614. doi: 10.1586/14789450.2.4.603. [DOI] [PubMed] [Google Scholar]
- 39.Berger RP, Beers SR, Richichi R, Wiesman D, Adelson PD. Serum biomarker concentrations and outcome after pediatric traumatic brain injury. J Neurotrauma. 2007 Dec;24(12):1793–1801. doi: 10.1089/neu.2007.0316. [DOI] [PubMed] [Google Scholar]
- 40.Yamazaki Y, Yada K, Morii S, Kitahara T, Ohwada T. Diagnostic significance of serum neuron-specific enolase and myelin basic protein assay in patients with acute head injury. Surg Neurol. 1995 Mar;43(3):267–270. doi: 10.1007/978-4-431-68231-8_86. discussion 270–261. [DOI] [PubMed] [Google Scholar]
- 41.Piazza O, Storti MP, Cotena S, et al. S100B is not a reliable prognostic index in paediatric TBI. Pediatr Neurosurg. 2007;43(4):258–264. doi: 10.1159/000103304. [DOI] [PubMed] [Google Scholar]
- 42.Martens P. Serum neuron-specific enolase as a prognostic marker for irreversible brain damage in comatose cardiac arrest surviviors. Acad Emerg Med. 1996;3:126–131. doi: 10.1111/j.1553-2712.1996.tb03399.x. [DOI] [PubMed] [Google Scholar]
- 43.Rainey T, Lesko M, Sacho R, Lecky F, Childs C. Predicting outcome after severe traumatic brain injury using the serum S100B biomarker: results using a single (24h) time-point. Resuscitation. 2009 Mar;80(3):341–345. doi: 10.1016/j.resuscitation.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 44.Bazarian JJ, Zemlan FP, Mookerjee S, Stigbrand T. Serum S-100B and cleaved-tau are poor predictors of long-term outcome after mild traumatic brain injury. Brain Inj. 2006 Jun;20(7):759–765. doi: 10.1080/02699050500488207. [DOI] [PubMed] [Google Scholar]
- 45.Watt SE, Shores EA, Baguley IJ, Dorsch N, Fearnside MR. Protein S-100 and neuropsychological functioning following severe traumatic brain injury. Brain Inj. 2006 Sep;20(10):1007–1017. doi: 10.1080/02699050600909698. [DOI] [PubMed] [Google Scholar]
- 46.Morochovic R, Racz O, Kitka M, et al. Serum S100B protein in early management of patients after mild traumatic brain injury. Eur J Neurol. 2009 Oct;16(10):1112–1117. doi: 10.1111/j.1468-1331.2009.02653.x. [DOI] [PubMed] [Google Scholar]
- 47.Eng LF, Vanderhaeghen JJ, Bignami A, Gerstl B. An acidic protein isolated from fibrous astrocytes. Brain Res. 1971 May 7;28(2):351–354. doi: 10.1016/0006-8993(71)90668-8. [DOI] [PubMed] [Google Scholar]
- 48.Duchen LW. General pathology of neurons and neuroglia. In: Adams JA, Corsellis JAN, Duchen LW, editors. Greenfield’s Neuropathology. London: Edward Arnold; 1984. pp. 1–52. [Google Scholar]
- 49.Baydas G, Nedzvetskii VS, Tuzcu M, Yasar A, Kirichenko SV. Increase of glial fibrillary acidic protein and S-100B in hippocampus and cortex of diabetic rats: effects of vitamin E. Eur J Pharmacol. 2003 Feb 21;462(1–3):67–71. doi: 10.1016/s0014-2999(03)01294-9. [DOI] [PubMed] [Google Scholar]
- 50.Mouser PE, Head E, Ha KH, Rohn TT. Caspase-mediated cleavage of glial fibrillary acidic protein within degenerating astrocytes of the Alzheimer’s disease brain. Am J Pathol. 2006 Mar;168(3):936–946. doi: 10.2353/ajpath.2006.050798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Herrmann M, Vos P, Wunderlich MT, de Bruijn CH, Lamers KJ. Release of glial tissue-specific proteins after acute stroke: A comparative analysis of serum concentrations of protein S-100B and glial fibrillary acidic protein. Stroke. 2000 Nov;31(11):2670–2677. doi: 10.1161/01.str.31.11.2670. [DOI] [PubMed] [Google Scholar]
- 52.Missler U, Wiesmann M, Wittmann G, Magerkurth O, Hagenstrom H. Measurement of glial fibrillary acidic protein in human blood: analytical method and preliminary clinical results. Clin Chem. 1999 Jan;45(1):138–141. [PubMed] [Google Scholar]
- 53.Pelinka LE, Kroepfl A, Leixnering M, Buchinger W, Raabe A, Redl H. GFAP versus S100B in serum after traumatic brain injury: relationship to brain damage and outcome. J Neurotrauma. 2004 Nov;21(11):1553–1561. doi: 10.1089/neu.2004.21.1553. [DOI] [PubMed] [Google Scholar]
- 54.Pelinka LE, Kroepfl A, Schmidhammer R, et al. Glial fibrillary acidic protein in serum after traumatic brain injury and multiple trauma. J Trauma. 2004 Nov;57(5):1006–1012. doi: 10.1097/01.ta.0000108998.48026.c3. [DOI] [PubMed] [Google Scholar]
- 55.van Geel WJ, de Reus HP, Nijzing H, Verbeek MM, Vos PE, Lamers KJ. Measurement of glial fibrillary acidic protein in blood: an analytical method. Clin Chim Acta. 2002 Dec;326(1–2):151–154. doi: 10.1016/s0009-8981(02)00330-3. [DOI] [PubMed] [Google Scholar]
- 56.Nylen K, Ost M, Csajbok LZ, et al. Increased serum-GFAP in patients with severe traumatic brain injury is related to outcome. J Neurol Sci. 2006 Jan 15;240(1–2):85–91. doi: 10.1016/j.jns.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 57.Mondello S, Papa L, Buki A, et al. Neuronal and glial markers are differently associated with computed tomography findings and outcome in patients with severe traumatic brain injury: a case control study. Crit Care. 2011 Jun 24;15(3):R156. doi: 10.1186/cc10286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.DeArmond SJ, Fajardo M, Naughton SA, Eng LF. Degradation of glial fibrillary acidic protein by a calcium dependent proteinase: an electroblot study. Brain Res. 1983 Mar 7;262(2):275–282. doi: 10.1016/0006-8993(83)91018-1. [DOI] [PubMed] [Google Scholar]
- 59.Zhang Z, Yang B, Glushakova O, et al. Alterations in the expression of glial fibrillary acidic protein and fragmentation in the subacute phase of brain injury [Abstract]. J Neurotrauma; The 28th National Neurotrauma Society Symposium; Las Vegas, Nevada. 2010. Vol suppl. [Google Scholar]
- 60.Zhang Z, Yang B, Glushakova O, et al. Expression patterns of glial fibrillary acidic protein (GFAP) in the sub-acute phase of brain injury [Abstract]. Annual Advanced Technology Applications for Combat Casualty Care (ATACCC); St. Petersburg, Florida. 2010. [Google Scholar]
- 61.Medicine MTBICACoR. Definition of Mild Traumatic Brain Injury. J Head Trauma Rehabil 1993. 1993;8(3):86–87. [Google Scholar]
- 62.Teasdale G, Jennett B. Assessment and prognosis of coma after head injury. Acta Neurochir (Wien) 1976;34(1–4):45–55. doi: 10.1007/BF01405862. [DOI] [PubMed] [Google Scholar]
- 63.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974 Jul 13;2(7872):81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 64.Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA. 2005 Sep 28;294(12):1511–1518. doi: 10.1001/jama.294.12.1511. [DOI] [PubMed] [Google Scholar]
- 65.Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001 May 5;357(9266):1391–1396. doi: 10.1016/s0140-6736(00)04561-x. [DOI] [PubMed] [Google Scholar]
- 66.Dula K, Mini R, van der Stelt PF, Lambrecht JT, Schneeberger P, Buser D. Hypothetical mortality risk associated with spiral computed tomography of the maxilla and mandible. Eur J Oral Sci. 1996 Oct-Dec;104(5–6):503–510. doi: 10.1111/j.1600-0722.1996.tb00133.x. [DOI] [PubMed] [Google Scholar]
- 67.Macgregor DM, McKie L. CT or not CT--that is the question. Whether ‘tis better to evaluate clinically and x ray than to undertake a CT head scan! Emerg Med J. 2005 Aug;22(8):541–543. doi: 10.1136/emj.2004.017160. [DOI] [PMC free article] [PubMed] [Google Scholar]