Abstract
Objective
To devise and test a self-management course for chronic pain patients based on evidence and underpinned by theory using the Medical Research Council (MRC) framework for developing complex interventions.
Design
We used a mixed method approach. We conducted a systematic review of the effectiveness of components and characteristics of pain management courses. We then interviewed chronic pain patients who had attended pain and self-management courses. Behavioural change theories were mapped onto our findings and used to design the intervention. We then conducted a feasibility study to test the intervention.
Setting
Primary care in the inner city of London, UK.
Participants
Adults (18 years or older) with chronic musculoskeletal pain.
Outcomes
Related disability, quality of life, coping, depression, anxiety, social integration and healthcare resource use.
Results
The systematic reviews indicated that group-based courses with joint lay and healthcare professional leadership and that included a psychological component of short duration (<8 weeks) showed considerable promise. The qualitative research indicated that participants liked relaxation, valued social interaction and course location, and that timing and good tutoring were important determinants of attendance. We used behavioural change theories (social learning theory and cognitive behaviour approaches (CBA)) to inform course content. The course addressed: understanding and accepting pain, mood and pain, unhelpful thoughts and behaviour, problem solving, goal setting, action planning, movement, relaxation and social integration/reactivation. Attendance was 85%; we modified the recruitment of patients, the course and the training of facilitators as a result of testing.
Conclusions
The MRC guidelines were helpful in developing this intervention. It was possible to train both lay and non-psychologists to facilitate the courses and deliver CBA. The course was feasible and well received.
Keywords: PAIN MANAGEMENT, PRIMARY CARE
Strengths and limitations of this study.
The approach enabled us to consider and integrate fidelity assessment.
We were able to modify recruitment processes and the course to accommodate patient needs.
We used the feasibility study to train the team and engage new networks for the main trial
The approach was resource intensive and lengthy but contributed to an efficient trial.
Introduction
Chronic musculoskeletal conditions are costly and burdensome to individuals and the society.1 Point estimates of the prevalence of chronic musculoskeletal pain range from 46% to 76%.2 Despite an increased understanding of the factors contributing to the development of chronic pain, there has been little improvement in how successfully it is treated and managed.3 Treatment centres around pharmaceutical agents and physiotherapy. More complex interventions such as pain management programmes delivered by multidisciplinary teams and self-management courses delivered by lay people with chronic pain are also used to address the complexity of living with and managing chronic pain.4–6 The UK Department of Health and The Health Foundation have invested in the implementation of lay-led (ie, peer-led) self-management training courses through the Expert Patients Programme (EPP)6 7 and the cocreating health initiative that aims to help people help themselves.8 The available evidence, however, suggests that it may not reduce healthcare resource use as expected9–11 and that there are only modest short-term beneficial effects on other outcomes. Very few studies have examined the long-term effects.10 11
In response to the paradox of continued government support of self-management programmes and equivocal evidence of effectiveness, the COping with persistent Pain, Effectiveness Research into Self-management (COPERS) study was commissioned by the UK National Institute of Health Research as a 5-year programme grant to improve the self-management of chronic pain.
Our aim was to design and test a practical and acceptable self-management intervention for chronic musculoskeletal pain.
This study illustrates how the Medical Research Council (MRC) framework for developing complex intervention can be implemented and used to develop interventions.12 We used the recommended approach for developing and designing this new intervention, which consisted of three phases
Identifying the evidence base,
Identifying appropriate theory to inform and model the design of the intervention,
Feasibility testing the intervention.
The first two projects informed the design of a pain self-management course, which we then pilot tested.
Phase I: Identifying the evidence base
We conducted two systematic reviews (SRs) to identify effective components and characteristics of pain management courses (SR1) and predictors, mediators and moderators of outcome in pain management courses (SR2). The methods and results are presented in detail elsewhere.13 14 Additionally, we did a qualitative study (QS) of people living with chronic pain.
We searched relevant databases including: MEDLINE, CINAHL, AHMED and PsychInfo from January 1994 to April 2009 for randomised controlled trials (RCTs) and SRs of self-management interventions. We defined self-management programmes as structured, taught or self-taught courses with distinct components principally aimed at patients (rather than carers) with the goal of improving the participants’ health status or quality of life by teaching them skills to apply to everyday situations. To be considered a ‘programme’ (which implies more than one component), the intervention had to contain at least two of the following components: psychological components (such as behavioural or cognitive therapy), mind-body therapies (such as relaxation, meditation or guided imagery), physical activity (any form of exercise), material on lifestyle (such as dietary advice and sleep management) and pain education (such as understanding their condition and how to take medication effectively).
We characterised the interventions according to: type of delivery (group, individual, mixed or remote (eg, web based)), type of tutor (healthcare professional, lay or a combination of tutors), setting (medical (ie, hospital, physician office or primary care), community or work based), duration (more or less than 8 weeks) and number of different components.
We examined the following outcomes: pain intensity, physical function, general mental health, depression, anxiety, social function, healthcare use, global health measures, quality of life and self-efficacy, but only examined outcome measures with published evidence of validity and reliability. We grouped outcomes into three follow-up intervals: short term (<4 months), medium term (4–8 months) and long term (>8 months).
We used random effects model meta-analysis to generate standardised mean differences and grouped data according to the presence or absence of course characteristics or components. We looked for patterns of clinically important and statistically significant differences between groupings across different outcomes and follow-up intervals.
Effective components and characteristics of pain management courses (SR1)
Overall, the literature indicated that the strongest evidence for pain outcomes was for group self-management programmes led by healthcare professionals while lay-led courses appeared to benefit participants’ self-efficacy (see table 1).13
Table 1.
Key findings and subsequent recommendations for course design
| Key finding from phases I and II | How this finding influenced course design (influences on main trial shown in brackets) |
|---|---|
| Group delivery appears to be effective (SR1) Networking with others popular feature of SM courses (QS) |
Group intervention |
| Most evidence to support professional tutors (SR1) Mixed professional and lay tutor-led course also effective (SR1) |
Groups to be led by a combination of a lay and a professional tutor |
| Medical and community settings associated with effective courses (SR1) Convenience of courses important to participants (QS) |
Courses to be held in convenient community or health centre settings |
| Courses longer than 8 weeks were no more effective than courses under 8 weeks (SR1) | Shorter duration course |
| SM Interventions with psychological components were more effective than usual care (SR1) Increased number of components were not associated with bigger effect sizes (SR1) |
Principal component of new intervention to be psychological |
| Little evidence to support mind body therapy components (SR1) | Relaxation to be control intervention in main trial. Relaxation was included because participants liked it and to match exposure with the control (QS) |
| Increasing self-efficacy may mediate intervention (SR2) | Course should aim to promote self-efficacy |
| Increasing physical activity may mediate intervention (SR2) Patient resistance to concept of exercise but not general activity (QS) |
We decided against a large physical activity component in the course but include taster activities (possible hobbies) |
| Depression at baseline may be a predictor for poorer outcomes (SR2) | Course covers depression and encourages people who feel they may be depressed to discuss this with their doctor |
| Concerns of attendees about what happens after the course is completed (QS) | Follow-up session at 2 weeks |
| Reduction in activities common in chronic MSK pain patients (QS) | Inclusion of “taster” activity sessions in the course |
| Isolation common in chronic MSK pain patients (QS) | Have plenty of time for socialising |
| Other key considerations influencing course design | |
| Adult educationalists advised that to be interesting and effective the course should employ multiple media and modalities, be delivered in 20-min bites and encourage experiential learning | Inclusion of role play, filmed material, small group exercises, exercises for pairs, active listening exercises, brainstorming, etc |
| Attrition from self-management courses running over 6–8 weeks known to be a problem | Course run over 3 days in a single week |
| Expert professional input may be useful or appealing to participants | Expert professional input delivered by DVD for economy |
| Reproducibility and fidelity of the intervention | Development of a course manual and training package |
MSK, musculoskeletal; QS, qualitative study; SR1, systematic review about components and characteristics of courses; SR2, systematic review about predictors, mediators and moderators of patient outcomes on courses.
The duration of courses did not appear to significantly influence their reported effectiveness and the setting had little impact on the outcome. Interventions including each of the components we tested (except mind body components) showed beneficial effects. Psychological components showed the most benefit. Increasing the number of components did not improve the overall benefit. Overall, our analysis provided some evidence for the use of short, group-delivered courses in convenient settings that have healthcare professional input (more detailed information can be accessed via reference 13).
Predictors, mediators and moderators of outcome in pain management courses (SR2)14
We identified papers that included analyses of predictors, moderators or mediators. We did meta-regression analyses using the standardised mean difference and estimated the precision of associations.15
We found strong evidence that self-efficacy and depression at baseline predicted outcome and strong evidence that self-efficacy and potentially pain-catastrophising and physical activity mediated outcome from self-management programmes for chronic musculoskeletal pain. There were no data on moderators of treatment.14
Qualitative study
We conducted a phenomenological qualitative interview and focus group study. For the interview study, we purposively sampled course participants by gender, age and high-course and low-course attendance from two EEP providers and one pain management course provider, and for the focus groups we recruited a convenience sample of experts from those who had recently published in this field and tutors from two local EPP providers. We carried out in-depth interviews with 16 chronic pain self-management course participants (11 were female, 7 were 45 years or over, 10 were white, 6 were of South Asian origin and 10 people had attended half or more of a course). We convened two focus groups, one with self-management ‘experts’ (n=5) and another with course tutors (n=5). Topics discussed included referrals attendance, course content, course delivery issues and expectations. We used a thematic framework approach to analyse the data and identified key themes and subthemes relevant to devising a new pain self-management course. Participants identified six key areas that they felt their treatment for their chronic pain should address; it describes the participant needs and expectations (table 2). We tried to incorporate these needs and expectations as much as possible into the course. While we could not achieve some things by running a course, we aimed to give participants the skills to realistically assess their needs and show them how to achieve them.
Table 2.
Qualitative interview study: needs and expectations important to participants
| Functional (practical daily living requirements) | Physical (equipment aids and help) | Emotional (dealing with frustration, anger, boredom, isolation, depression) | Social (social networking, relationships with partners, family and friends) | Economic (financial support, benefits etc, work-related issues) | Medical (pain and drug related) |
| Activities of daily living Being able to cook, shop clean etc. |
Mobility aids Provision of equipment to help move and achieve tasks |
Mood modification Changing and managing feelings better. Dealing with emotions |
Making new friends Meeting new people, finding new friends |
Financial support Benefit payments from the state |
Pain reduction Better knowledge of drugs and how to take them Better prescribing of more effective drugs |
|
Personal hygiene Being able to dress and wash independently |
Home help Physical help from others to do things |
Behavioural change Learning how to do things better within the context of pain |
Improving relationships Communication, understanding, recognition of condition |
Special allowances Disability parking permits |
Reduction in side effects of drugs Nausea, vomiting, diarrhoea and constipation |
|
Looking after others Being able to manage children and partners better |
Pain management Learning new ways to manage pain |
Helping others understand living with pain | Return to work |
Access to ‘non medical’ treatment Massages, acupuncture, gym memberships |
|
| Having someone to listen and talk to | Finding a hobby/distraction from pain | Getting GP support |
GP, general practitioner.
We noted that the patients with chronic musculoskeletal pain whom we interviewed made positive comments about the courses they attended and had particular traits. They were prepared to be socially engaged; they were motivated prior to the course and took up new activities (not necessarily exercise related) after the course. Participants liked the social element and the relaxation components of the course. Good course facilitation and social support cemented their experience. Those with a low mood, poor social skills and unwillingness to change/reflect seemed less likely to engage with these types of courses.
Phase II: Identifying appropriate theory to inform and model the design of the intervention
We searched the literature and spoke to key experts on behavioural change theory and models of persisting pain. We considered the following psychological theoretical models and learning and behaviour modification techniques: social cognitive16 17 and cognitive behavioural theory,18 19 including psychological flexibility (acceptance and commitment therapy, ie, the acceptance of internal experiences or things that cannot be changed countered by behavioural change techniques that are designed to reorientate people towards meaningful activity,20 21 theory of planned behaviour and reasoned action22–24 (including emotional rationalisation) and health belief models. In addition, we looked at attention control techniques25 and physical movement to underpin and inform our intervention. Figure 1 illustrates the relationship between theory and course design.
Figure 1.
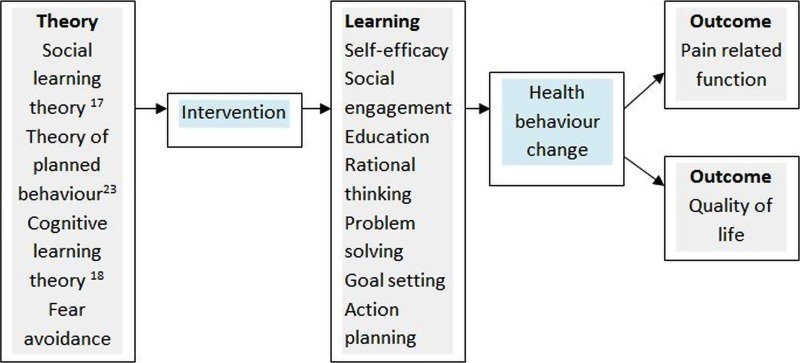
Model of relationship between theory and intervention development.
We established a patient working group to devise an acceptable and appropriate intervention that reflected the evidence we had obtained and the theories we had identified as appropriate.
As recommended by the MRC guidelines, we considered patient pathways through the self-management programme, as well as the likely action and interaction of the different components on outcomes in an attempt to model the impact and effect of our intervention.12 We convened a ‘consensus’ group of two patients, three clinicians (general practitioner (GP) and two clinical psychologists), four researchers and one commissioner to agree on the outcomes we wanted the intervention to affect and the appropriate measurement tools. They were improved function despite pain, ‘better’ healthcare resource use, reactivation into society, more self-confidence in managing pain, better coping and reduced anxiety and depression. The measurement tools were selected and tested in the feasibility study (a sample of which is shown in table 3). We assessed the behavioural change theories relevant to a new intervention and identified individual behavioural change techniques for different learning outcomes and the different components of a course (table 4). We also used a taxonomy of behavioural change techniques developed by Abraham and Michie26 to describe the techniques we adopted to promote positive behavioural change in self-management groups.
Table 3.
Summary baseline data describing the population recruited (mean (SD))
| Data | Pain intensity Scale 0–10 |
EQ5d | PSEQ Scale 0–60 |
HADS Anxiety Scale 1–21 |
HADS Depression Scale 1–21 |
CPAQ Scale 0–120 |
HEIQ Scale 5–20 |
|---|---|---|---|---|---|---|---|
| B'line (n=43) | 6.7 (2.1) | 0.23 (0.4) | 22.5 (12.7) | 11.3 (4.1) | 9.4 (3.8) | 46.7 (17.3) | 12.8 (3.1) |
| F-U (n=25) | 6.3 (2.2) | 0.31 (0.4) | 30.2 (13.1) | 10.2 (3.8) | 8.8 (4.1) | 54.1 (18.02) | 13.1 (3.5) |
Numerical rating scale pain: 0–10=worst pain imaginable, Euroqol—Quality of life indicator (EQ5D), UK norm healthy males/females 40–49 years 0.89/0.87 and 50–59 years 0.8/0.82 (0 death).27 Pain self-efficacy questionnaire (PSEQ) scale: 0–60=completely confident,28 hospital anxiety and depression scale (HADS), scale: 0–7 ‘normal’, 8–10 borderline, 11–21 ‘abnormal’.29 Chronic pain and acceptance questionnaire scale (CPAQ): 120–0=not coping at all,30 Health education involvement questionnaire (HEIQ) Higher scores indicate a better social life.31
Table 4.
Theories, therapies and cognitive and behavioural techniques influencing the design of the course
| Underlying theories and therapies | Influence on course design | Cognitive and behavioural change techniques used throughout the course as determined by the groups and the facilitators |
|---|---|---|
|
Biopsychosocial model of medicine Physiology, psychology and the social environment and society play a part in health |
Whole course | Plan social support/social change Facilitate social comparison Barrier identification/problem solving Devise behavioural goals Action planning Model/demonstrate the behaviour Provide information on where and when to perform behaviour Provide instruction on how to perform the behaviour Provide opportunity to devise ways of performing the behaviour Learn where and when to perform behaviour Learn how to perform the behaviour Prompt generalisation of a target behaviour Provide information on the consequences of behaviour Reflect on the consequences of behaviour Reflect on where and when to perform behaviour Prompt self-monitoring of behaviour Prompt self-monitoring of behaviour outcome Review of behavioural goals and outcomesStress management Prompt self-talkPrompt use of imagery Prompt practice Emotional control training Environmental restructuring Communication skills Provide feedback Prompt focus on past success Environmental restructuring Teach to use prompts/cues Repetition Use of follow-up prompts Prompt anticipated regrets and setbacks Relapse prevention/coping and planning |
|
Acceptance and Commitment Therapy (ACT) Accepting the here and now and living with it |
Pain information Acceptance: the uninvited guest Relaxation and mindfulness |
|
|
Fear avoidance and catastrophising Pain and fear lead to avoidance behaviour which is not always beneficial |
The pain cycle, goal setting and action planning | |
|
Attention management Keeping the brain occupied on things other than pain, reduces pain perception |
Attention control and distraction Relaxation, breathing, visualisation and imagery Taster sessions (eg, art) |
|
|
Social cognitive theory Behaviour may be influenced by interaction between personal, environmental factors and own and others’ behaviour |
Group work/discussion Reflection Listening skills |
|
|
Cognitive therapy Recognising the link between thoughts, emotions and behaviour Theory of planned behaviour Based on beliefs about likely consequences of behaviour Rational emotive principles Logical unemotional rationalisation of events, thoughts, emotions |
Identifying problems, goal setting and action planning Barriers to change—unhelpful thinking Barriers to change—reframing negatives to positives Communicating with your GP Anger, irritability and frustration: managing emotion Follow-up—managing setbacks |
|
|
Mind body therapies Muscle relaxation, biofeedback, visualisation and mindfulness techniques |
Relaxation and breathing Relaxation and visualisation Relaxation and mindfulness of thoughts |
|
|
Physical theory and therapies Alexander technique for posture and physical therapy practice on balance and stretch |
Posture Balance and stretch Stretch |
GP, general practitioner.
The courses also allowed opportunities for people to learn and try new behaviours in an appropriate environment.
Table 4 shows our rationale for mapping and modelling theory to behavioural change techniques and the methods used by facilitators throughout the courses. The final column describes the behavioural change techniques that were used throughout the courses. While some sessions required facilitators to employ techniques focusing on providing feedback, other sessions provided instruction to promote behavioural change and yet others allowed participants to try out techniques within the ‘safety’ of the learning environment and the group. The techniques employed by facilitators were often dependent on the needs of the participants and the groups and therefore are utilised as necessary and when required in each individual session. No negative or coercive behavioural change techniques were recommended or used as part of the courses. We decided that the components of the course should include: psychological concepts using cognitive behavioural (http://www.babcp.com/) approaches to managing chronic pain (these covered: acceptance, attention control, goal setting and action planning, recognising unhelpful thinking and behaviours); the course also covered communication skills, relationships, promoting better sleep, medical education, social networking, hobbies and activities, posture and movement, breathing, relaxation and visualisation and guided imagery. Our QS indicated that patient understanding about pain was limited, so we therefore decided to include an educational DVD with a pain consultant answering common questions from patients with chronic pain. The structure of the course we piloted is shown in table 5.
Table 5.
Pilot course overview and final course
| Day | Sessions | Content of sessions |
|---|---|---|
| 1 Living and dealing with pain |
1. Introduction and understanding pain and acceptance |
Session 1: Introduction Session 2: Pain information Session 3: Acceptance: the uninvited guest |
| Lunch | ||
| Taster activity | Art | |
| 2. Mind, mood and pain | Session 4: Pain, when is it bearable and when is it not? Session 5: The pain cycle |
|
| 3. Movement and posture and relaxation | Session 6: Movement and posture Session 7: Breathing and relaxation (focusing the mind) |
|
| 2 Doing something about your life with pain |
4. Dealing with unhelpful, negative thoughts and barriers to change | Session 8: Reflections from day one Session 9: Identifying problems, goal setting and action planning Session 10: Unhelpful thinking and automatic thoughts |
| Lunch | ||
| Taster activity | Hand massage | |
| 5. Making pain more manageable | Session 11: Barriers to change, challenging unhelpful thoughts. Pros and cons of chronic pain and reframing Session 12: Attention control and distraction Session 13: Identifying things that make pain more manageable |
|
| 6. Movement and Relaxation | Session 14: Movement and balance Session 15: Breathing, relaxation and visualisation |
|
| 3 Communication and relationships |
7. Communication skills and relationships |
Session 16: Reflections from day 2 Session 17: Communication with health professionals Session 18: Communication and listening Session 19: Anger, irritability, frustration Session 20: Intimacy (rejected after testing) |
| Lunch | Introduce idea of ‘buddying’ (rejected after testing) | |
| Taster activity | Craft (rejected after testing; added volunteering instead) | |
| 9. Movement and relaxation | Session 21: Movement and stretch Session 22: Relaxation and guided imagery |
|
| 4 Follow-up |
10. The future | Session 23: Reflections Session 24: Managing setbacks |
Course
The findings from the SRs and the QS informed the design of the new intervention (table 1). The final course structure and content included a mix of theoretical concepts and psychological, behavioural, educational and physical techniques. Our qualitative research and evidence reviews identified a variety of components, characteristics and functions to accommodate in the self-management course, hence the eclectic design.
We designed a group course to be facilitated by a healthcare professional (a psychologist, physiotherapist, chiropractor, osteopath, occupational therapist or GP) and a lay person with chronic pain with prior experience in small group facilitation (eg, a course facilitator on the EPP). The course was structured to be delivered over three short days in 1 week (10:00–14:45), with a 2 h follow-up session 2 weeks later. We also designed a 2-day training programme for all potential facilitators. All courses were to be held in a convenient, accessible location for study participants.
Phase III: assessing the feasibility of the intervention (COPERS trial ISRCTN 24426731)
Method
We used an uncontrolled pilot study approach to test the feasibility of delivering the intervention and the receipt of the intervention.
Participants
Adults (18 years and over) included those with persistent musculoskeletal pain (pain in their muscles or joints lasting longer than the normal expected healing time of 3 months) who were physically and mentally able to attend a community-based group course. We excluded those who had any other more serious comorbidity than their pain (such as terminal illness, cancer, uncontrolled addictions or other mental health issues).
All patients were required to be fluent in English as this was a group-based course reliant on discussion and interaction.
Sample size
We estimated that six courses of 8–10 people would be sufficient to evaluate the course; we aimed to recruit around 60–80 participants allowing for dropouts.
Setting
Inner London urban community in East London. We recruited patients from two local general practices, the Tower Hamlets Persistent Pain Service and the musculoskeletal physiotherapy service at Mile End Hospital. Participants were identified by clinicians from known regular patients and ad hoc from face-to-face consultations. We delivered the courses in community-based venues convenient for participants.
Outcomes
We used a number of outcome measures to test completion rates and acceptability. Questionnaire instruments are shown in table 3.
Follow-up
Participants completed postal questionnaires at a baseline and at 3 months.
Fidelity and facilitator training: adherence and competence
We trained 15 facilitators to deliver the course. They underwent a 2-day training course and included six lay people with chronic pain and nine healthcare professionals (one chiropractor, three osteopaths, two physiotherapists, one psychologist, one occupational therapist and one GP). Three of these trained healthcare professionals were unable to facilitate courses due to work pressures.
We observed all the courses and wrote extensive field notes. In addition to collecting our outcome data, we asked for written feedback about the courses from the facilitators and the participants and also interviewed 13 participants. We collected data about attendance for every component of the course and reasons for non-attendance and non-participation.
Results
We sent 518 invitation letters to people with chronic pain (335 were female); 68 people agreed to participate (13% response rate), 8 withdrew without accepting a place, and 60 accepted a place on a course (33 were female). In 4 months, we delivered six courses with an average of seven participants per course. Overall, participants attended 85% of all sessions.
Participant feedback
The overall satisfaction score (0–5 with five indicating most satisfied) was 4.2. The interview data revealed that participants most liked meeting other people with chronic pain and the relaxation sessions. Participants who attended few sessions (less than 1 day), or did not attend, reported that work commitments and being in a group were an issue, and that some poor facilitation affected their learning and pleasure. Some participants mentioned that they thought the intimacy session was too personal and they did not want to disclose this type of information to people they did not know well.
Facilitator feedback
This centred on the need for preparation and experience in facilitation and handling difficult situations. Observer feedback identified that there were some modules that needed to be amended, and that the intimacy session did not work well due to the reluctance of participants to discuss issues. In addition, the facilitators felt that the ‘buddying-up’ system (the facilitators created and provided the opportunity and time for group members to exchange contact details) should be instigated and initiated by the group themselves, not the facilitators, as some group members found the concept of buddying too intrusive. More handouts were suggested and facilitators needed more training in facilitation to make sure that they were confident. However, all facilitators felt that they improved as they progressed through the courses.
No serious adverse events occurred as a result of the intervention.
Quantitative data
Descriptive results from the baseline questionnaire showed that 53% (23/43) of participants were female, modal age range was 41–50 years (15 participants). Twenty-one people (49%) regarded themselves as unemployed or as unable to work due to pain, 12 were employed, 5 were retired and 4 were looking after family at home.
Baseline
Overall, the profile of the participants at baseline suggested that they had above average pain (6.7 on a scale of 0–10) and rated their quality of life as low; also, they had high anxiety scores and were not coping well (table 3).
Follow-up
The follow-up response rate was 58%. Participant, facilitator and researcher feedback suggested that the follow-up questionnaire length (94 questions) was too burdensome and therefore unacceptable for the main trial.
Findings and recommendations to optimise the intervention and a trial protocol
The course was feasible, acceptable to participants and deliverable. Participants were positive about the course and the content appeared to be meaningful to them. Attrition was very low over the three main days: participants attended an average 85% of the course. Attrition has been reported as an issue in other trials; one such trial (intervention arm n=313) using expert patient programmes over a 6-week period showed a loss of 26% participants between referral and course attendance and 40% of participants attended three or less sessions overall, that is, 50% or less of the course sessions.11
The facilitation and group process may have optimised the learning process as discussion embedded participant thinking. All the course evaluation material suggested that good facilitation skills were crucial for positive participant perception. Comprehensive facilitator training is essential for courses to run effectively.
Recruitment to the study was difficult and conversion rates from invitation to course attendance were lower than we had hoped (∼13% of those invited), but were in line with other studies of this nature recruiting patients from primary care with chronic conditions.32–34 Despite this, we had sufficient interest from patients to run six courses and this feasibility study showed that there was a demand for learning about non-pharmacological approaches to managing pain. Procedures for future recruitment can be enhanced by increasing the number of invitations and devising and testing a comprehensive and inclusive electronic search strategy for patients with chronic pain.35 It is also quite likely that recruitment to the intervention would be higher outside the context of a research study.
Recruitment needs to be timed with the delivery of the intervention (ie, course dates which had to be planned in advance due to facilitator and accommodation availability). We estimated that an average lead time from identification of participant, screening for suitability by GP, sending invitation, receiving enquiries and interest, sending out and returning baseline questionnaires, randomisation and booking on a course takes around 8 weeks. Building rapport with participants from the outset is crucial to reduce loss of potential participants prior to being enroled, randomised and/or booked on a course.
In this pilot, participants reported poor quality of life, low self-efficacy to manage their chronic pain, relatively high levels of social isolation, poor coping and a tendency to anxiety and depression. Thus, secondary outcome measures need to reflect these health and social states. Our descriptive baseline data may explain why the ‘buddying system’ and the ‘Intimacy session’ from the course were too difficult for some participants to deal with. It may be that depression should be addressed with patients prior to, or in conjunction with, attending these types of courses.
The theory underpinning the decisions to include the variety of sessions and behavioural change techniques worked within the group learning environment; this has also been shown to be effective in other studies of chronic pain.33 36 The learning sequence we adopted enabled each session to build on the previous session, and in many cases the participants were able to predict the next phase of learning in advance. The learning and flow of information was pitched at a level where participants could follow the structure and understand the content. This was shown in the daily feedback sheets where we asked participants what they had learnt; their learning mapped well onto the learning objectives. The quotes below illustrate some of this.
it was shocking to think there is no cure for my pain but I suppose there isn't, otherwise I would have been given it by now
the ‘unhelpful thinking’…they were all me, I will look out for these now, I've stuck them (the list of automatic thoughts) on my fridge door
the relaxation and the breathing really help me
I spend all day trying not to think about my pain but that's the worst thing I can do
The best part was meeting everyone
The participants valued the social interaction on the course highly; for some participants, it appeared to have an impact on self-esteem and confidence, for example, self comparison with others in less fortunate circumstances, perspective on life, distraction, laughter and release from boredom and isolation in some cases.
We found that it was possible to train both lay and non-psychologists to facilitate the courses and deliver cognitive behaviour approach. Delivery styles did vary and there is value in thorough training and evaluation of training and subsequent delivery of courses, embedding fidelity assessment from the outset to measure the adherence and competence of those delivering the intervention. We found that the course stood up to the inexperience of our facilitators to deliver an entirely new course; the content in terms of the discussions, information and handouts was robust enough to make an impression regardless of the delivery style. We recommend that inexperienced personnel are partnered with experienced personnel initially.
A by-product of testing the programme was staff training and development based on their experience of conducting the pilot. We also found that we built valuable networks and contacts, which was helpful for the main trial.
Conclusion
The MRC guidance for developing complex interventions enabled us to develop and test an evidence-based and theory-informed pain self-management course. The process enhanced the intervention and gave the study team confidence in the modified intervention and trial procedures and processes necessary to run a full effectiveness and cost effectiveness RCT efficiently.37
Supplementary Material
Footnotes
Contributors: DC wrote the first draft of the paper and managed all the development phases of the study. KH worked on all phases of the development and has contributed to and commented on the manuscript. MU and SJCT are the principal investigators on the project and provided oversight and guidance in all stages of the research and contributed to the manuscript. TP was involved in the systematic reviews and the theoretical development of the programme and has commented on the paper. AR developed and delivered the education component of the course and has commented on this paper.
Funding: This paper presents independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research scheme (RP-PG-0707–10189). The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Competing interests: None.
Ethics approval: Ethics approval was granted by the East London and The City Research Ethics Committee Alpha (10//H0704/7). ISRCTN: 24426731 COPERS trial.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All additional data pertaining to this study will be published in a full NIHR report published by the funder.
References
- 1.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study. Lancet 2010;380:2224–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parsons S, Breen A, Foster NE, et al. Prevalence and comparative troublesomeness by age of musculoskeletal pain in different body locations. Fam Pract 2007;24:308–16 [DOI] [PubMed] [Google Scholar]
- 3.Croft P. Is life becoming more of a pain? BMJ 2000;320:1552–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wanless D. Securing our future health: taking a long-term view—the Wanless Report. Department of Health, Stationery Office, 2002. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4009293 [Google Scholar]
- 5.Donaldson L. Expert patients usher in a new era of opportunity for the NHS. BMJ 2003;326:1279–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Department of Health The expert patient: a new approach to chronic disease management for the 21st century. Department of Health, Stationery Office, 2001. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyandGuidance/DH_4006801 [Google Scholar]
- 7.Expert patient programme. http://www.expertpatients.co.uk/ (accessed 17 Jun 2013)
- 8.Health foundation UK, co-creating health initiative. http://www.health.org.uk/areas-of-work/programmes/co-creating-health/ (accessed 17 Jun 2013)
- 9.Griffiths C, Foster G, Ramsay J, et al. How effective are expert patient (lay led) education programmes for chronic disease? BMJ 2007;334:1254–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Foster G, Taylor SJ, Eldridge SE, et al. Self-management education programmes by lay leaders for people with chronic conditions. Cochrane Database Syst Rev 2007;(4):CD005108. [DOI] [PubMed] [Google Scholar]
- 11.Kennedy A, Reeves D, Bower P, et al. The effectiveness and cost effectiveness of a national lay-led self care support programme for patients with long-term conditions: a pragmatic randomised controlled trial. J Epidemiol Community Health 2007;61:254–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: new guidance. Medical Research Council, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carnes D, Homer KE, Miles CL, et al. Effective delivery styles and content for self-management interventions for chronic musculoskeletal pain: a systematic literature review. Clin J Pain 2012;28:344–54 [DOI] [PubMed] [Google Scholar]
- 14.Miles CL, Pincus T, Carnes D, et al. Can we identify how programmes aimed at promoting self-management in musculoskeletal pain work and who benefits? A systematic review of sub-group analysis within RCTs. Eur J Pain 2011;15:775.e1–11 [DOI] [PubMed] [Google Scholar]
- 15.Upton G, Cook I. Oxford dictionary of statistics. Oxford: Oxford University Press, 2002 [Google Scholar]
- 16.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191–215 [DOI] [PubMed] [Google Scholar]
- 17.Bandura A. Social foundations of thought and action: a social cognitive theory. Pearson Education, 1986 [Google Scholar]
- 18.Beck JS. Cognitive therapy. The Guildford Press, 1995 [Google Scholar]
- 19.Leahy R. Cognitive therapy techniques: a practitioner's guide. New York: Guildford Press, 2003 [Google Scholar]
- 20.Hayes SC, Smith SX. Get out of your mind and into your life: the new acceptance and commitment therapy. Oakland, CA: New Harbinger Publications, 2005 [Google Scholar]
- 21.Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: an experiential approach to behavior change. New York: Guilford Press, 2004 [Google Scholar]
- 22.Ajzen I, Fishbein M. Belief, attitude, intention and behaviour: an introduction to theory and research (Addison-Wesley series in social psychology). Longman Higher Education, 1976 [Google Scholar]
- 23.Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Pearson Education, 1980 [Google Scholar]
- 24.Kuhl J, Beckman J. eds. Action control: from cognition to behavior (Springer series in social psychology). Berlin: Springer-Verlag; and Heidelberg: GmbH & Co, 1985 [Google Scholar]
- 25.Morley S, Shapiro DA, Biggs J. Developing a treatment manual for attention management in chronic pain. Cogn Behav Ther 2004;33:1–11 [DOI] [PubMed] [Google Scholar]
- 26.Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008;27:379–87 [DOI] [PubMed] [Google Scholar]
- 27.Kind P, Hardman G, Macran S. UK population norms for EQ-5D. Discussion paper 172. University of York, Centre for Health Economics, 1999 [Google Scholar]
- 28.Nicholas MK. The pain self-efficacy questionnaire: taking pain into account. Eur J Pain 2007;11:153–63 [DOI] [PubMed] [Google Scholar]
- 29.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70 [DOI] [PubMed] [Google Scholar]
- 30.McCracken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: component analysis and a revised assessment method. Pain 2004;107:159–66 [DOI] [PubMed] [Google Scholar]
- 31.University of Melbourne . Health Education Impact Questionnaire. http://www.crd.unimelb.edu.au/heiq/ [Google Scholar]
- 32.UK BEAM Trial Team United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: effectiveness of physical treatments for back pain in primary care. BMJ 2004;329:1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lamb SE, Hansen Z, Lall R, et al. Group cognitive behavioural treatment for low-back pain in primary care: a randomised controlled trial and cost-effectiveness analysis. Lancet 2010;375:916–23 [DOI] [PubMed] [Google Scholar]
- 34.Johnson RE, Jones GT, Wiles NJ, et al. Active exercise, education, and cognitive behavioral therapy for persistent disabling low back pain: a randomized controlled trial. Spine 2007;32:1578–85 [DOI] [PubMed] [Google Scholar]
- 35.Foell J, Carnes D, Homer K, et al. Developing and implementing electronic search strategies to recruit patients with chronic musculoskeletal pain in primary care databases. Primary Health Care Res Dev 2013;May 24:1–10.10.1017/S1463423613000248 [DOI] [PubMed] [Google Scholar]
- 36.Ostelo R, van Tulder MW, Vlaeyen JWS, et al. Behavioural treatment for chronic low-back pain. Cochrane Database Syst Rev 2005;(1):CD002014. [DOI] [PubMed] [Google Scholar]
- 37.Carnes D, Underwood M, Homer K, et al. Effectiveness and cost effectiveness of a novel, group self-management course for adults with chronic musculoskeletal pain: study protocol for a multi-centre, randomised controlled trial (COPERS). BMJ Open 2013;3:e002492. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


