Abstract
Purpose
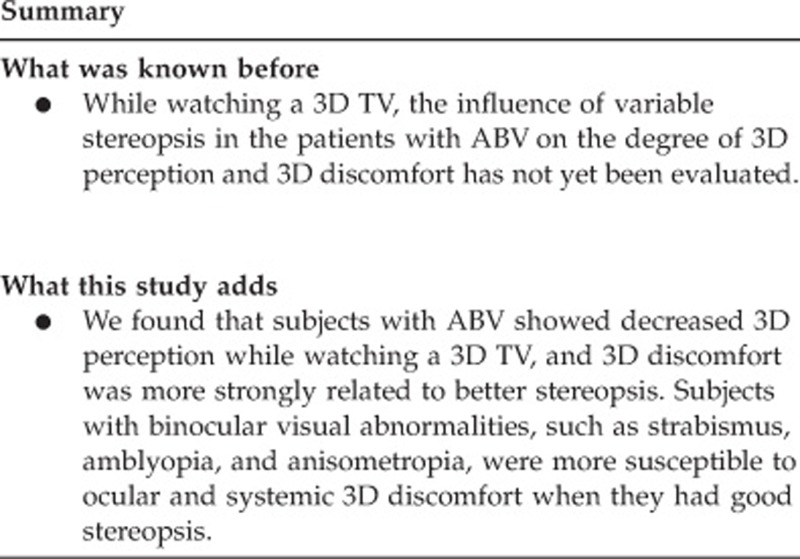
To evaluate the degree of three-dimensional (3D) perception and ocular and systemic discomfort in patients with abnormal binocular vision (ABV), and their relationship to stereoacuity while watching a 3D television (TV).
Methods
Patients with strabismus, amblyopia, or anisometropia older than 9 years were recruited for the ABV group (98 subjects). Normal volunteers were enrolled in the control group (32 subjects). Best-corrected visual acuity, refractive errors, angle of strabismus, and stereoacuity were measured. After watching 3D TV for 20 min, a survey was conducted to evaluate the degree of 3D perception, and ocular and systemic discomfort while watching 3D TV.
Results
One hundred and thirty subjects were enrolled in this study. The ABV group included 49 patients with strabismus, 22 with amblyopia, and 27 with anisometropia. The ABV group showed worse stereoacuity at near and distant fixation (P<0.001). Ocular and systemic discomfort was, however, not different between the two groups. Fifty-three subjects in the ABV group and all subjects in the control group showed good stereopsis (60 s of arc or better at near), and they reported more dizziness, headache, eye fatigue, and pain (P<0.05) than the other 45 subjects with decreased stereopsis. The subjects with good stereopsis in the ABV group felt more eye fatigue than those in the control group (P=0.031). The subjects with decreased stereopsis showed more difficulty with 3D perception (P<0.001).
Conclusions
The subjects with abnormal stereopsis showed decreased 3D perception while watching 3D TV. However, ocular and systemic discomfort was more closely related to better stereopsis.
Keywords: abnormal binocular vision, asthenopia, depth perception
Introduction
With the progression of the three-dimensional (3D) technology industry, 3D displays are becoming pervasive. 3D theaters as well as 3D television (TV) and computers are widely used. There has also been a noticeable increase in exposure to 3D images. Although watching 3D images is known to induce more ocular and systemic fatigue and discomfort, which can be referred to as ‘3D asthenopia', than watching two-dimensional (2D) images,1, 2, 3, 4, 5 the influence of 3D images on the eyes or other parts of the body and the related mechanisms are not thoroughly understood. In addition, there are no safety guidelines for watching a 3D display.
To perceive a 3D image as a stereoscopic one, a fusional mechanism should be used6. With normal binocular vision, one can perceive 3D images with motor and sensory fusion. However, patients with abnormal binocular vision (ABV), including strabismus, amblyopia, and anisometropia, may have a variable range of fusional ability. Some patients cannot use a fusional mechanism at all, whereas some patients can use a fusional mechanism to a normal degree with an additive effort to obtain it. This kind of additive effort can increase fatigue while watching 3D images. In addition, the degree of ABV, which can be measured with a stereopsis test, can affect the degree of 3D perception. We have reported that the presence of exophoria might be a risk factor for 3D asthenopia in otherwise healthy subjects.7 Yet, the degree of 3D perception and ocular and systemic discomfort in patients with ABV with variable stereoacuity have not been evaluated. The purpose of this study is to evaluate the degree of 3D perception and ocular and systemic discomfort in patients with ABV, including strabismus, amblyopia, and anisometropia, and their relationship to stereoacuity while watching a 3D TV.
Materials and methods
Patients aged 9 years or older who had at least one abnormal binocular condition that included strabismus, anisometropia, or amblyopia were recruited for the ABV group. Normal subjects were included in the control group. Anisometropia was defined as a difference in the spherical equivalent (SEQ) in refractive error between eyes >2 diopters. Amblyopia was diagnosed when the best-corrected visual acuity was <16/20, or when the difference between eyes was more than two lines of Snellen acuity. The subjects were diagnosed with strabismus when there was any refixating eye movement on the alternate cover test. We performed cover/uncover test to differentiate phoria from tropia.
The ABV group was divided into three subgroups according to the etiology of ABV. When a patient had strabismic or anisometropic amblyopia, he or she was included in the amblyopia subgroup for analysis. Informed consent was obtained from all of the volunteers following the study protocol, which was reviewed and approved by the Institutional Review Board of Korea University Medical Center and adhered to the tenets of the Declaration of Helsinki. Volunteers with a history of other ophthalmological diseases, including glaucoma and retinal disease, and with systemic diseases, such as cerebral palsy and delayed maturation, were excluded.
The best-corrected visual acuity and refractive errors were measured. The angle of ocular deviation was obtained with the alternate prism-cover test while the subject was fixating the accommodative target at 6 m. Stereoacuity was examined with the Stereo Fly test (Stereo Optical Co., Chicago, IL, USA) for near and with the Frisby–Davis distance stereotest (FD2; Stereotest, Sheffield, UK) for distant stereopsis, according to a previously reported method.8, 9 The photographs of fundus, taken with a fundus camera, were also examined for retinal abnormalities.
The 3D video, which was produced by the national broadcasting system for 3D test-run broadcasts in South Korea, was shown for 20 min on a 3D high-definition TV (3D TV), sized 139 cm diagonally. Both types of 3D TV using shutter glasses and polarized glasses were used in this study. The illuminance of the room was 5 lx. The viewing distance was 2.8 m.
After watching the 3D TV, the participants were surveyed to evaluate the degree of 3D perception and subjective symptoms of ocular and systemic discomfort (Supplementary Table 1). The questionnaire comprised 13 items, which included the degree of 3D perception and the most frequently reported ocular and non-ocular symptoms after watching 3D images.10, 11, 12, 13, 14, 15 Each item was answered onto a five-category scale (0–4). A score of 0 corresponded to no symptom. Score 1 meant mild symptoms, which were tolerable, and score 2 meant moderate symptoms, which sometimes caused an inconvenience while watching 3D TV. A score of 3 indicated severe symptoms, which caused a disturbance during 3D viewing, and a score of 4 corresponded to extremely severe symptoms as a result of which people had to discontinue watching 3D images. The degree of 3D perception and subjective ocular and systemic discomfort were compared between the two groups.
The stereoacuity results were grouped as either ‘good' (60 s of arc or better), ‘moderate' (>60 and ≤800 s of arc), or ‘poor' (>800 s of arc to nil) stereopsis according to the near stereoacuity. The degree of 3D perception and ocular and systemic symptoms were compared among the stereoacuity groups. These were also compared between the subjects who showed normal stereopsis in the ABV group and in the control group.
For statistical analysis, the Kruskal–Wallis and the Mann–Whitney U-tests were used with SPSS 12.0K for Windows (SPSS Inc., Chicago, IL, USA). For multiple testing problems, P-values were adjusted with the Bonferroni correction. The χ2-test was used to compare the distribution of the subjects in the near stereoacuity subgroups.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Results
One hundred and thirty subjects were enrolled in this study, 98 in the ABV group, and 32 in the control group. The mean age of the subjects was 13.0±4.87 years. Seventy-five (57.7%) were women. The ABV group included 49 patients with strabismus, 22 with amblyopia, and 27 with anisometropia. Among the strabismic patients, 34 had an exodeviation, 11 had an esodeviation, and 4 had a hyperdeviation. The mean deviation angles (prism diopters) among those patients were 11.6±6.74, 7.7±14.72, and 5.5±5.74, respectively. In the patients with exodeviation, 8 patients had intermittent exotropia, 1 constant exotropia, and 25 exophoria. In the patients with esodeviation, five had infantile esotropia and six had accommodative or partially accommodative esotropia. The diagnosis, angle of deviation, and stereoacuity of subjects with strabismus are presented in Supplementary Table 2. In amblyopic patients, the mean Snellen acuity of the worse eye was 0.58±0.27. In anisometropic patients, the mean difference in SEQ between the eyes was 2.71±1.58 diopters.
The mean distant stereoacuity was 14.06±9.79 s of arc in the control group and 34.85±16.32 s of arc in the ABV group (P<0.001). There was no subject or control with distant stereopsis worse than 800 s of arc. For near stereoacuity, 53 patients in the ABV group had normal stereopsis, 33 showed moderate, and the remaining 12 had poor stereopsis, whereas all subjects in the control group showed normal stereopsis. Thus, there was a significant difference in the distribution of near stereoacuity between the two groups (P<0.001).Within the ABV group, the mean distant stereopsis (seconds of arc) was 31.02±16.99 in the strabismus subgroup, 45.00±11.95 in the amblyopia subgroup, and 33.52±15.12 in the anisometropia subgroup (P<0.001). The distant stereoacuity of the amblyopia subgroup was poorer than that of the strabismus (P=0.006) and anisometropia subgroups (P=0.012). There was no difference between the strabismus and anisometropia subgroups with regard to distance stereoacuity (P=0.556). Table 1 shows the distribution of near stereoacuity in the ABV group. The distribution was not significantly different among subgroups (P=0.126).
Table 1. The near stereoacuity of subjects in the ABV group according to its etiology.
| ABV group |
Near stereoacuity (seconds of arc) |
Total | |||
|---|---|---|---|---|---|
| Good (60 or better) | Moderate (60< and ≤800) | Poor (worse than 800) | |||
| Subgroups | Strabismus | 31 | 13 | 5 | 49 |
| Amblyopia | 7 | 10 | 5 | 22 | |
| Anisometropia | 15 | 10 | 2 | 27 | |
| Total | 53 | 33 | 12 | 98 | |
Abbreviation: ABV, abnormal binocular vision.
Table 2 shows the results of the survey in the ABV and control groups. The ocular and systemic discomfort was not different between the two groups. The survey results were compared among subgroups of ABV group in Table 3. There was no difference in the ocular and systemic discomfort among the subgroups. However, there was a difference in the degree of subjective 3D perception (P=0.010). Subgroup analysis revealed that the subjects with amblyopia showed a greater decrease in 3D perception than those with anisometropia (P=0.004), strabismus (P=0.049), and the control group (P=0.004). There was no difference between subjects with strabismus or anisometropia and the control group.
Table 2. The comparison of survey results between the control and ABV groups.
| Control group | ABV group | Pa | |
|---|---|---|---|
| Dizzy | 0.94±0.98 | 0.84±0.95 | 0.598 |
| Headache | 0.44±0.56 | 0.61±0.82 | 0.489 |
| Nausea | 0.28±0.73 | 0.20±0.61 | 0.689 |
| Eye fatigue | 0.75±0.92 | 0.92±0.98 | 0.394 |
| Eye pain | 0.84±1.17 | 0.68±1.01 | 0.259 |
| Tearing | 0.38±1.13 | 0.20±0.72 | 0.492 |
| Eye dryness | 0.38±0.94 | 0.40±0.74 | 0.400 |
| Blurred vision | 0.28±0.58 | 0.28±0.70 | 0.623 |
| Difficulty in focusing | 0.34±0.90 | 0.42±0.79 | 0.303 |
| Double vision | 0.34±0.90 | 0.32±0.86 | 0.949 |
| Transient visual dimness after watching TV | 0.22±0.55 | 0.24±0.70 | 0.881 |
| Could not feel stereoscopic vision | 0.47±0.84 | 0.91±1.32 | 0.118 |
| Difficulty in eye tracking the motion on TV | 0.16±0.45 | 0.28±0.62 | 0.358 |
Abbreviation: ABV, abnormal binocular vision.
The Mann–Whitney U-test.
Table 3. The subgroup comparison of survey results in ABV groups.
|
ABV group |
Pa | |||
|---|---|---|---|---|
| Strabismus (n=49) | Amblyopia (n=22) | Anisometropia (n=27) | ||
| Dizzy | 1.04±1.00 | 0.55±0.74 | 0.70±0.95 | 0.088 |
| Headache | 0.73±0.93 | 0.41±0.59 | 0.56±0.75 | 0.453 |
| Nausea | 0.22±0.67 | 0.09±0.29 | 0.26±0.66 | 0.761 |
| Eye fatigue | 1.10±1.12 | 0.59±0.67 | 0.85±0.86 | 0.232 |
| Eye pain | 0.71±1.19 | 0.64±1.05 | 0.67±1.00 | 0.989 |
| Tearing | 0.22 ±0.80 | 0.23±0.69 | 0.15±0.60 | 0.765 |
| Eye dryness | 0.43±0.82 | 0.36±0.49 | 0.37±0.79 | 0.755 |
| Blurred vision | 0.24±0.60 | 0.41±0.80 | 0.22±0.80 | 0.509 |
| Difficulty in focusing | 0.47±0.79 | 0.50±0.74 | 0.26±0.81 | 0.179 |
| Double vision | 0.39±1.02 | 0.27±0.46 | 0.22±0.80 | 0.424 |
| Transient visual dimness after watching TV | 0.24±0.75 | 0.27±0.63 | 0.22±0.70 | 0.806 |
| Could not feel stereoscopic vision | 0.84±1.21 | 1.59±1.62 | 0.48±1.05 | 0.010 |
| Difficulty in eye tracking the motion on TV | 0.35±0.72 | 0.32±0.57 | 0.11±0.42 | 0.185 |
Abbreviation: ABV, abnormal binocular vision.
The Kruskal–Wallis test.
The ocular and systemic discomfort was compared according to stereoacuity. The subjects with good stereopsis on the Titmus stereofly test (53 in the ABV group and all 32 in the control group) reported more dizziness, headache, eye fatigue, and pain (P<0.05) than the 45 subjects with decreased stereopsis (worse than 60 s of arc; Table 4). The subjects with decreased stereopsis showed more difficulty with 3D perception (P<0.001).
Table 4. The comparison of the survey results between the subjects with normal and moderate-to-poor streoacuity.
| Normal stereopsis (60 arcsec or better) | Moderate-to-poor stereopsis (worse than 60 arcsec) | Pa | |
|---|---|---|---|
| Dizzy | 1.04±1.02 | 0.53±0.73 | 0.007 |
| Headache | 0.66±0.80 | 0.40±0.69 | 0.050 |
| Nausea | 0.28±0.73 | 0.11±0.38 | 0.212 |
| Eye fatigue | 1.05±1.03 | 0.56±0.72 | 0.009 |
| Eye pain | 0.79±1.05 | 0.60±1.23 | 0.042 |
| Tearing | 0.20±0.75 | 0.33±0.98 | 0.400 |
| Eye dryness | 0.35±0.78 | 0.47±0.81 | 0.291 |
| Blurred vision | 0.25±0.60 | 0.33±0.90 | 0.698 |
| Difficulty in focusing | 0.36±0.80 | 0.47±0.84 | 0.348 |
| Double vision | 0.28±0.84 | 0.40±0.91 | 0.214 |
| Transient visual dimness after watching TV | 0.22±0.61 | 0.27±0.78 | 0.547 |
| Could not feel stereoscopic vision | 0.45±0.81 | 1.47±1.59 | <0.001 |
| Difficulty in eye tracking the motion on TV | 0.26±0.62 | 0.22±0.52 | 0.956 |
The Mann–Whitney U-test.
There was no difference in the ocular and systemic discomfort between the subjects with moderate stereopsis and those with poor stereopsis. The subjects with poor stereoacuity had more difficulty in 3D perception than those with moderate stereoacuity (P=0.006). Among the subjects with good stereopsis, those in the ABV group felt more eye fatigue than those in the control group (P=0.031; Table 5); those subjects also experienced more headaches than the control group to a nearly significant degree (P=0.076).
Table 5. The comparison of the survey results in the subjects with normal stereopsis of the control and ABV group.
|
Subjects with good stereopsis |
Pa | ||
|---|---|---|---|
| From control group (n=32) | From ABV group (n=53) | ||
| Dizzy | 0.93±0.98 | 1.12±1.04 | 0.457 |
| Headache | 0.44±0.56 | 0.81±0.89 | 0.076 |
| Nausea | 0.28±0.73 | 0.29±0.75 | 0.881 |
| Eye fatigue | 0.75±0.92 | 1.25±1.06 | 0.031 |
| Eye pain | 0.84±1.17 | 0.77±0.98 | 0.865 |
| Tearing | 0.38±1.13 | 0.10±0.36 | 0.240 |
| Eye dryness | 0.38±0.94 | 0.35±0.68 | 0.601 |
| Blurred vision | 0.28±0.58 | 0.23±0.61 | 0.485 |
| Difficulty in focusing | 0.34±0.90 | 0.38±0.75 | 0.435 |
| Double vision | 0.34±0.90 | 0.25±0.81 | 0.519 |
| Transient visual dimness after watching TV | 0.22±0.55 | 0.23±0.65 | 0.904 |
| Could not feel stereoscopic vision | 0.47±0.84 | 0.44±0.80 | 0.977 |
| Difficulty in eye tracking the motion on TV | 0.16±0.45 | 0.33±0.71 | 0.287 |
Abbreviation: ABV, abnormal binocular vision.
The Mann–Whitney U-test.
Discussion
When images with horizontal disparity are located on the corresponding retina in each eye simultaneously, stereopsis occurs. The fusion of such disparate images results in single stereoscopic vision with depth perception. This is how 3D displays work: they function by showing images with horizontal disparity to each eye simultaneously. Thus, a normal binocular visual system with intact fusional mechanism is necessary to properly experience a 3D display. We defined the patients with ABV as having difficulties in achieving and maintaining normal binocular single vision. Among these conditions, strabismus, anisometropia, and amblyopia are typical; hence, the patients with those diseases with variable degree of stereopsis were included in the ABV group in this study.
In this study, there was no difference in ocular and systemic discomfort between the ABV and control groups. The presence of abnormalities in binocular vision itself did not have an important role in symptom development after watching 3D images. However, the ABV group showed variable stereopsis. Forty-five subjects in the ABV group showed moderate-to-poor near stereoacuity, but the other 53 in the ABV group showed normal near stereoacuity. When ocular and systemic discomfort was evaluated according to stereoacuity, the subjects with normal stereopsis experienced more discomfort than those with moderate-to-poor stereopsis, although they perceived the stereoscopic images better. We believe that the subjects with moderate-to-poor stereopsis had difficulty in fusion while watching 3D images. This might have made the 3D images appear to be no different from 2D images for these individuals, and they did not experience more ocular and systemic symptoms.
Among the subjects with normal stereopsis in both groups, the subjects in the ABV group had more ocular fatigue than those in the control group. They experienced more headaches than did patients in the normal group, and the difference was marginally significant. We think that those subjects may have to make additional efforts, such as fusional vergence and accommodation, to maintain fusion while watching 3D images. Fusional vergence is needed to perceive two images with horizontal disparity as a stereoscopic one when watching a 3D display. Accommodation is accompanied by convergent eye movements, which is unnecessary, because the distance between the eyes and the 3D display screen did not change. This vergence–accommodation conflict was reported as an important factor in so-called 3D fatigue.1, 3, 16, 17, 18, 19 Emoto et al5 reported that fusional amplitude showed a greater decrease in stereoscopic viewing than in viewing conventional TV because of the strain on the vergence eye movement system. The ABV patients with normal stereopsis would need more effort than normal people to maintain fusion. The image blurring in amblyopia, asymmetric refractive error in anisometropia, and the ocular misalignment in strabismus would be obstacles to overcome for ABV patients to maintain binocular single vision and achieve normal stereopsis. We believe that ABV patients with normal stereopsis would have to make this additional effort while watching 3D TV, causing more discomfort.
Our study has some limitations. We used questionnaire-based grading, which is a rather subjective method, to assess the severity of ocular or systemic discomfort, as objective method that correlates with such subjective symptoms has not been well established yet. Further study to find the appropriate objective method to measure the severity of 3D discomfort would be necessary. Another limitation is that a 2D-viewing condition was absent in this study. It might be possible that an ABV patient with normal stereopsis might also report more fatigue when viewing 2D TV. However, the aim of this study was to evaluate 3D perception and discomfort while watching 3D TV in patients with ABV; hence, we did not perform any tests under a 2D control testing condition. It would be necessary to compare discomfort experienced while watching 2D TV with that experienced while viewing 3D TV in these patients in future studies. In addition, because the degree of strabismus, anisometropia, and corrected visual acuity in subjects with amblyopia and stereopsis were variable in the ABV group, we were unable to evaluate other factors such as the type and angle of strabismus, fusional amplitude, and the differences in refractive error and visual acuity between eyes, which could potentially affect 3D discomfort. Further study in a larger number of subjects with each etiology and having a similar degree of stereopsis is necessary.
In conclusion, subjects with ABV showed decreased 3D perception, and ocular and systemic discomfort were more strongly related to better stereopsis. Subjects with binocular visual abnormalities, such as strabismus, amblyopia, and anisometropia, were more susceptible to ocular and systemic 3D discomfort when they had good stereopsis.
Acknowledgments
We thank Soon-Young Hwang, PhD, who is a biostatistician at the Korea University College of Medicine, Department of Biostatistics, for her help with the statistical analysis performed in this study. This study was supported by research grants from the Korea Communications Commission (KCC) and was conducted as a part of research suggesting guidelines for the safety of 3D broadcast viewing.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on Eye website (http://www.nature.com/eye)
Supplementary Material
References
- Yano S, Ide S, Mitsuhashi T, Thwaites H. A study of visual fatigue and visual comfort for 3D HDTV/HDTV images. Displays. 2002;23 (4:191–201. [Google Scholar]
- Schor CM, Tsuetaki TK. Fatigue of accommodation and vergence modifies their mutual interactions. Invest Ophthalmol Vis Sci. 1987;28 (8:1250–1259. [PubMed] [Google Scholar]
- Lambooij M, Ijsselsteijn W, Fortuin M, Heynderickx I. Visual discomfort and visual fatigue of stereoscopic displays: a review. J Imaging Sci Technol. 2009;53 (3:030201–030214. [Google Scholar]
- Hoffman DM, Girshick AR, Akeley K, Banks MS. Vergence-accommodation conflicts hinder visual performance and cause visual fatigue. J Vis. 2008;8 (3:33. 1–30. doi: 10.1167/8.3.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emoto M, Nojiri Y, Okano F. Changes in fusional vergence limit and its hysteresis after viewing stereoscopic TV. Displays. 2004;25 (3-4:67–76. [Google Scholar]
- Von Noorden GK, Campos EC.Examination of the patinet-VIn: Von Noorden GK, Campos EC (eds.)Binocular Vision And Ocular Motility: Theory And Management Of Strabismus6th ed.Mosby: St Louis, MO, USA; 2002298–307. [Google Scholar]
- Kim SH, Suh YW, Song JS, Park JH, Kim YY, Huh K, et al. Clinical research on the ophthalmic factors affecting 3D asthenopia. J Pediatr Ophthalmol Strabismus. 2012;49 (4:248–253. doi: 10.3928/01913913-20120207-03. [DOI] [PubMed] [Google Scholar]
- Adams WE, Hrisos S, Richardson S, Davis H, Frisby JP, Clarke MP. Frisby Davis distance stereoacuity values in visually normal children. Br J Ophthalmol. 2005;89 (11:1438–1441. doi: 10.1136/bjo.2005.071761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong SW, Park SC. Development of distant stereoacuity in visually normal children as measured by the Frisby-Davis distance stereotest. Br J Ophthalmol. 2008;92 (9:1186–1189. doi: 10.1136/bjo.2008.138362. [DOI] [PubMed] [Google Scholar]
- Ames SL, Wolffsohn JS, McBrien NA. The development of a symptom questionnaire for assessing virtual reality viewing using a head-mounted display. Optom Vis Sci. 2005;82 (3:168–176. doi: 10.1097/01.opx.0000156307.95086.6. [DOI] [PubMed] [Google Scholar]
- Mon-Williams M, Wann JP, Rushton S. Binocular vision in a virtual world: visual deficits following the wearing of a head-mounted display. Ophthalmic Physiol Opt. 1993;13 (4:387–391. doi: 10.1111/j.1475-1313.1993.tb00496.x. [DOI] [PubMed] [Google Scholar]
- Howarth PA, Costello PJ. The occurrence of virtual simulation sickness symptoms when an HMD was used as a personal viewing system. Displays. 1997;18 (2:107–116. [Google Scholar]
- Wilson JR. Effects of participating in virtual environments - A review of current knowledge. Safety Sci. 1996;23 (1:39–51. [Google Scholar]
- Regan EC, Price KR. The frequency of occurrence and severity of side-effects of immersion virtual-reality. Aviat Space Envir Md. 1994;65 (6:527–530. [PubMed] [Google Scholar]
- Mon-Williams M, Wann JP. Binocular virtual reality displays: when problems do and don't occur. Hum Factors. 1998;40 (1:42–49. [Google Scholar]
- Kooi FL, Toet A. Visual comfort of binocular and 3D displays. Displays. 2004;25 (2-3:99–108. [Google Scholar]
- Rushton SK, Riddell PM. Developing visual systems and exposure to virtual reality and stereo displays: some concerns and speculations about the demands on accommodation and vergence. Appl Ergon. 1999;30 (1:69–78. doi: 10.1016/s0003-6870(98)00044-1. [DOI] [PubMed] [Google Scholar]
- Howarth PA. Potential hazards of viewing 3-D stereoscopic television, cinema and computer games: a review. Ophthalmic Physiol Opt. 2011;31 (2:111–122. doi: 10.1111/j.1475-1313.2011.00822.x. [DOI] [PubMed] [Google Scholar]
- Bando T, Iijima A, Yano S. Visual fatigue caused by stereoscopic images and the search for the requirement to prevent them: a review. Displays. 2012;33 (2:76–83. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


