Abstract
Pancreatic exocrine insufficiency is an important cause of maldigestion and a major complication in chronic pancreatitis. Normal digestion requires adequate stimulation of pancreatic secretion, sufficient production of digestive enzymes by pancreatic acinar cells, a pancreatic duct system without significant outflow obstruction and adequate mixing of the pancreatic juice with ingested food. Failure in any of these steps may result in pancreatic exocrine insufficiency, which leads to steatorrhea, weight loss and malnutrition-related complications, such as osteoporosis. Methods evaluating digestion, such as fecal fat quantification and the 13C-mixed triglycerides test, are the most accurate tests for pancreatic exocrine insufficiency, but the probability of the diagnosis can also be estimated based on symptoms, signs of malnutrition in blood tests, fecal elastase 1 levels and signs of morphologically severe chronic pancreatitis on imaging. Treatment for pancreatic exocrine insufficiency includes support to stop smoking and alcohol consumption, dietary consultation, enzyme replacement therapy and a structured follow-up of nutritional status and the effect of treatment. Pancreatic enzyme replacement therapy is administered in the form of enteric-coated minimicrospheres during meals. The dose should be in proportion to the fat content of the meal, usually 40-50000 lipase units per main meal, and half the dose is required for a snack. In cases that do not respond to initial treatment, the doses can be doubled, and proton inhibitors can be added to the treatment. This review focuses on current concepts of the diagnosis and treatment of pancreatic exocrine insufficiency.
Keywords: Chronic pancreatitis, Pancreatic exocrine insufficiency, Pancreatic enzyme replacement therapy
Core tip: This is a review on the diagnosis and treatment of pancreatic exocrine insufficiency. The review includes a discussion of the definition of pancreatic exocrine insufficiency, a pragmatic approach to its diagnosis and current concepts of indications for treatment with pancreatic enzyme replacement therapy, including measures to optimize the effect.
INTRODUCTION
Pancreatic exocrine insufficiency (PEI) can be defined as a reduction in pancreatic enzyme activity in the intestinal lumen to a level that is below the threshold required to maintain normal digestion. This concept is crucial for the understanding of PEI and has several important consequences for the diagnosis and treatment of this condition. First, pancreatic exocrine secretion can be significantly reduced without PEI being present. In a landmark paper four decades ago, DiMagno et al[1] demonstrated that steatorrhea does not occur until pancreatic lipase output is reduced to 5%-10% of normal output. Hence, the demonstration of moderately reduced bicarbonate or enzyme output in sensitive tests of pancreatic secretion, such as the secretin/cholecystokinin-stimulation test, is a reliable indicator of chronic pancreatitis (CP) but does not necessarily indicate PEI. Second, any pathology, including extrapancreatic conditions, that interrupt the chain of events required for the normal digestion of ingested food by pancreatic digestive enzymes may cause PEI. Thus, “pancreatic exocrine insufficiency” is a denomination that, from a semantic point of view, is too narrow for this condition; “pancreatic maldigestion” could be an alternative and probably more correct term. Diseases of the pancreatic parenchyma, such as CP, cystic fibrosis and status post necrotizing acute pancreatitis, are the most common causes of PEI. However, PEI may also be caused by obstruction of the pancreatic duct system due to a tumor or a stricture, by reduced stimulatory capacity in the intestine secondary to untreated celiac disease[2] or Crohn’s disease, by increased intraluminal inactivation of pancreatic enzymes in Zollinger-Ellison syndrome[3] or by impaired mixing of ingested food and the pancreatic juice after upper gastrointestinal surgery[4] (Figure 1).
Figure 1.
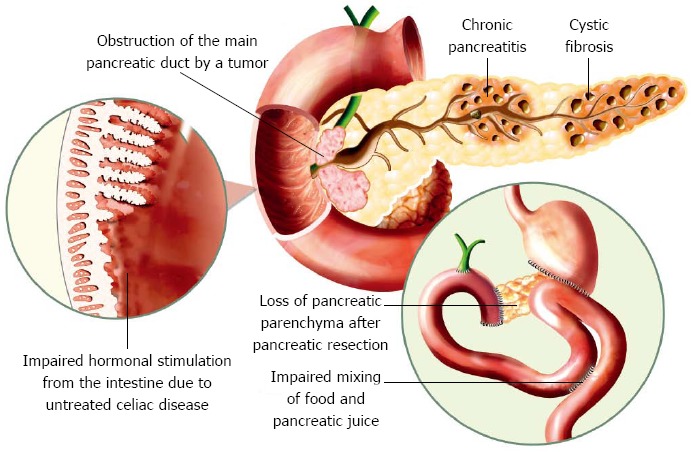
Different causes of pancreatic exocrine insufficiency.
The pancreatic juice plays a pivotal role in the digestion and absorption of nutrients[5]. Pancreatic enzyme secretion is stimulated during the cephalic[6] and gastric[7] phases to a certain degree, but the most important stimulation occurs during the intestinal phase, when chyme enters the duodenum. The presence of fatty acids, amino acids and gastric acid in the duodenum is the most potent stimulator of exocrine pancreatic secretion[8]. Vagal and neural reflexes stimulate pancreatic secretion during the cephalic and gastric phases[6,7]. During the intestinal phase, cells in the duodenal mucosa release CCK, which stimulates the secretion of pancreatic enzymes from acinar cells[9], and secretin, which elicits water and bicarbonate secretion from ductal cells[10,11].
The pancreatic juice consists of bicarbonate and water secreted by ductal cells and several enzymes, secreted by acinar cells, with the specific capacity to digest proteins, carbohydrates and fat. In situations with reduced exocrine pancreatic function, the ability to digest fat is the determining factor that causes the most important symptoms and clinical complications because lipase, the major lipolytic enzyme of the pancreatic juice, is the pancreatic digestive enzyme with the poorest stability in the gastrointestinal lumen. The destruction of lipase is even more rapid when the pH is below 4, which is often the situation in CP, in which the buffering of gastric acid is insufficient due to low bicarbonate excretion by the pancreas[12]. Furthermore, there is minimal extrapancreatic lipolytic enzyme production, as opposed to the extrapancreatic capacity to digest carbohydrates provided by salivary amylase and intestinal oligosaccharidoses or the proteolytic capacity provided by gastric pepsinogen.
PEI is one of the major complications in CP and should be considered in all CP patients. The prevalence of PEI in CP increases with disease duration, and approximately half of patients will have developed PEI by 12 years after disease onset[13]. There are no reliable estimates of the prevalence of PEI in the general population.
Patients with untreated PEI not only suffer from impaired quality of life due to steatorrhea, weight loss, abdominal discomfort and other PEI-related symptoms but are also highly likely to develop deficiencies of micronutrients and lipid-soluble vitamins[14]. These deficiencies in turn place patients at risk of malnutrition-related complications, such as osteoporosis[15,16]. Hence, an early and accurate diagnosis of PEI is of high clinical importance.
DIAGNOSIS OF PANCREATIC EXOCRINE INSUFFICIENCY
The gold standard for the diagnosis of PEI is three-day fecal fat quantification and determination of the coefficient of fat absorption[17]. A major drawback of fecal fat quantification is that the test is cumbersome and unpleasant for both the patient and laboratory personnel. The patient is required to keep a strict diet, with 100 g of fat per day for five days, and to collect the complete volume of feces for three days. Laboratory personnel need to handle large volumes of feces. Therefore, this test is very rarely performed in daily clinical practice and is only available at few specialized centers. Several alternative methods for the diagnosis of PEI have been proposed.
Diagnosis based on symptoms, blood tests and imaging
Symptoms in patients with PEI vary, depending on the degree and etiology of PEI. The classical clinical picture is a patient presenting with foul-smelling, loose stools, weight loss, muscle wasting; and flatulence. Advanced tests of pancreatic exocrine function can usually be avoided in patients with a well-established CP diagnosis based on morphological findings and a clear clinical picture of PEI. A trial of pancreatic enzyme replacement therapy (PERT) based only on the clinical picture is recommended by several national societies when the clinical presentation is strongly suggestive of PEI[18,19]. However, only relying on symptoms may lead to both the over- and under-diagnosis of PEI. Diarrhea and weight loss may be due to conditions other than PEI, and PEI can also be present in the absence of overt steatorrhea.
In addition to explaining and treating clinical symptoms, the second rationale for the early diagnosis of PEI is to prevent complications of malnutrition. It is reasonable to assume that such malnutrition-related complications will be preceded by deficiencies of macro- or micronutrients detectable by routine blood tests. Hence, from a theoretical point of view, serum nutritional markers could be used to support the diagnosis of PEI. Deficiencies of several nutrients in blood tests have been demonstrated in CP, including apolipoproteins[20,21], total cholesterol[22], magnesium[22,23], lipid-soluble vitamins[24-26], retinol-binding protein[26], calcium, zinc and selenium[25], but the majority of these studies have not taken the exocrine function status of patients into consideration. Studies investigating the association between nutritional markers and PEI in CP patients have demonstrated that deficiencies of lipid-soluble vitamins are associated with an increased probability of PEI[15,26], as opposed to B12 and folate levels, which are not associated with PEI[14,27]. The possibility of diagnosing PEI based on nutritional markers in the blood was recently studied in a cohort of 114 patients with CP, of whom 38 suffered from PEI[14]. Hemoglobin, albumin, prealbumin and retinol-binding protein levels below the lower limit of normal magnesium levels below 2.05 mg/dL; and HbA1C levels above the upper limit of normal were all significantly associated with PEI. No PEI patient in this study presented with normal values for all of these parameters. The central conclusion that can be drawn from this study is that a normal panel of serum nutritional markers can exclude PEI with a high negative predictive value.
The probability of PEI in CP can also be estimated based on pancreatic imaging findings in the absence of more advanced tests of pancreatic function[28]. Notably, ductal changes on endoscopic retrograde pancreatography, computerized tomography (CT)[29] and endoscopic ultrasound (EUS) have been associated with decreased exocrine pancreatic function. The diagnosis of CP by EUS is based on the demonstration of several different parenchymal (hyperechoic foci, hyperechoic strands, parenchymal lobularity and cysts) and ductal (pancreatic duct dilatation, irregular pancreatic duct contour, hyperechoic pancreatic duct margin, dilated side branches and intraductal calcifications) abnormalities defined in the Rosemont classification[30]. A recent study demonstrated a clear correlation between the number of EUS criteria met and the probability of PEI. Calcifications and main pancreatic duct dilatation were independently associated with PEI in a multivariate analysis, and the probability of PEI was > 80% if these features were present[28].
Fecal elastase 1
Pancreatic elastase 1 is an enzyme of the pancreatic juice that is highly stable during passage through the gastrointestinal tract[31]. The concentration of elastase 1 can be measured in feces using a simple enzyme-linked immunosorbent assay [fecal elastase 1 (FE-1)] on a spot fecal sample[32,33]. FE-1 levels have been demonstrated to correlate with more sensitive tests of pancreatic secretion, such as the secretin test[32,34]. Low FE-1 levels have also been demonstrated to correlate with morphological tests for CP, such as endoscopic retrograde pancreatography[35] and magnetic resonance cholangiopancreatography[36]. However, as opposed to the relatively large number of studies evaluating FE-1 assessment as a test for the diagnosis of CP, studies evaluating the role of FE-1 testing in the detection of PEI in CP are scarce. Recently, Benini et al[37] investigated FE-1 and fecal fat in patients with CP or pancreatic resection. Three important conclusions can be drawn from this study. First, an FE-1 concentration of < 15 μg/g feces detects PEI with high sensitivity and specificity in patients with CP without prior pancreatic surgery. Second, intermediate FE-1 values (15-200 μg/g feces) are more difficult to interpret and likely warrant testing with more sensitive methods. Third, FE-1 assessment is not a reliable test for PEI in patients post-pancreatic resection. The fecal fat concentration was consistently higher in relation to FE-1 levels in operated compared with non-operated cases[37]. This finding was not unexpected; inadequate mixing of food with the pancreatic juice and other factors not related to pancreatic secretory capacity are likely to contribute to the pathogenesis of PEI after pancreatic resections.
13C-mixed triglycerides breath test
The 13C-mixed triglycerides (13C-MTG) breath test was introduced by Vantrappen et al[38]. The test directly measures the clinically most relevant end-effect of exocrine pancreatic function: the degradation of triglycerides. This makes this test preferable to tests that measure exocrine pancreatic secretion, such as the secretin test and the FE-1 assay. For the 13C-MTG test, the patient ingests a small amount of 13C-marked triglycerides (2-octanoyl (1-13C)-1,3 distearoyl glycerol), together with butter on a piece of toasted bread, after an overnight fast. In the presence of normal lipase activity, 13C-triglycerides will be degraded in the intestinal lumen, and 13C-marked fatty acids will then be absorbed. These fatty acids will in turn be metabolized in the liver, and 13CO2 can finally be measured in exhaled air. Subjects with PEI have decreased lipase activity, which can be detected as a decreased recovery of 13CO2 in exhaled air. Currently, there is no general agreement on the optimal design of the test and several different protocols have been proposed[39-43]. The protocol developed by Domínguez-Muñoz et al[44] has been adopted by several groups, including our institution, and this protocol is described in Table 1[44]. Values below 29% are considered as pathological, and the test detects fat maldigestion with a sensitivity of > 90%[40].
Table 1.
The 13C-mixed triglycerides breath test according to Domínguez-Muñoz et al[44]
| The patient fasts from midnight |
| Twenty minutes before the test, 10 mg of metoclopramide is ingested |
| A baseline breath sample is taken |
| At time 0, 250 mg of 13C-mixed triglycerides mixed with 16 g of fat on a piece of toasted bread is ingested, together with a glass (200 mL) of water |
| Breath samples are taken every 15 (or 30) min for 6 h |
| Finally, 13CO2/12CO2 is measured in collected breath samples by mass spectrometry or isotope-selective nondispersive infrared spectrometry |
Test based on analysis of pancreatic juice after secretin/cerulein stimulation
Exocrine pancreatic function can be measured by so-called direct pancreatic function tests. In these tests, pancreatic secretion is stimulated by secretin and/or cerulein[45] or by the ingestion of a standard test meal[46]. After stimulation, samples of the pancreatic juice are aspirated from a tube that has been placed in the duodenum, and the concentrations of pancreatic digestive enzymes and bicarbonate are measured. A peak bicarbonate concentration in pancreatic secretion significantly below normal values (a cut-off value of 80 mEq has been advocated by most authorities) in the secretin test has long been considered as the most sensitive test for early CP. A drawback of the direct function tests is that they require the placement of a large-bore tube in the duodenum during the complete duration of the test, which is poorly tolerated by patients. It is also important to keep in mind that a mild reduction in pancreatic exocrine function, occasionally called “exocrine pancreatic dysfunction” or “mild pancreatic exocrine insufficiency”, is not equivalent to clinically significant PEI. PEI, based on its definition, is a reduction in exocrine pancreatic function to a level that results in maldigestion. Since the introduction of highly sensitive pancreatic imaging methods, such as MRI, modern CT and endoscopic ultrasound, the need to rely on pancreatic function testing for the diagnosis of CP has diminished, and most centers have abandoned the classic secretin test.
Recently, an endoscopic direct pancreatic function test was developed, with a simplified protocol for pancreatic fluid collection through an endoscope. A good correlation between the endoscopic pancreatic function test and standard direct tests has been demonstrated[47,48]. Exocrine pancreatic secretion can also be evaluated based on the degree of duodenal filling on MRI after secretin stimulation, which has been demonstrated to correlate with a combination of the FE-1 assay, the 13C-MTG breath test and fecal fat testing[49] and the endoscopic pancreatic function test[50]. Further studies are needed to evaluate the role of the endoscopic function test and secretin-enhanced MRI in the diagnosis of PEI. It should be noted that all tests of pancreatic secretion share the drawback of ignoring other factors that may alter the effect of pancreatic enzymes in the intestine. Thus, tests of pancreatic secretion are irrelevant in situations in which factors other than the secretory capacity of the pancreas may contribute to PEI.
Integrated use of methods to diagnose PEI
The optimal test for the diagnosis of PEI is a test that can detect the maldigestion of fat with high sensitivity and specificity. Fecal fat quantification and the 13C-MTG breath test are recommended for the accurate diagnosis of PEI because these two tests best fit this description. However, due to the limited availability of these tests and the odious nature of fecal fat quantification, there is a need for a simplified way to estimate the probability of PEI based on generally available clinical parameters. In Figure 2, a proposal for a diagnostic algorithm to estimate the probability of PEI based on routine blood tests, FE-1 assessment and standard imaging is presented. The algorithm is designed to have a high negative predictive value for PEI and integrates knowledge from recent studies[14,28,37]. However, it should be stressed that this algorithm provides only an estimation of the probability of PEI and that the algorithm has not been scientifically validated.
Figure 2.
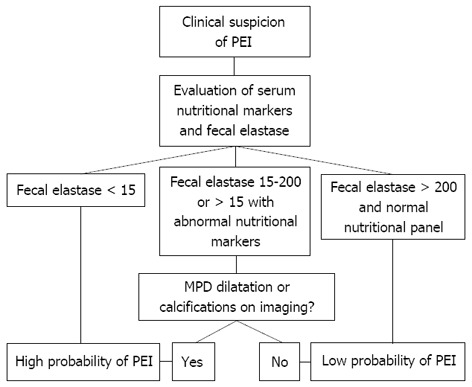
Evaluation of the probability of pancreatic exocrine insufficiency in the absence of advanced tests for maldigestion, such as fecal fat quantification and the 13C-mixed triglycerides breath test. PEI: Pancreatic exocrine insufficiency; MPD: Main pancreatic duct.
TREATMENT OF PANCREATIC EXOCRINE INSUFFICIENCY
Cornerstones in the treatment of PEI are PERT, support to cease smoking and alcohol consumption, consultation with a dietitian and a systematic follow-up to assure optimal treatment effect (Figure 3). The goal of this treatment concept is to normalize digestion, alleviate PEI-related symptoms and prevent malnutrition-related morbidity and mortality and disease progression.
Figure 3.
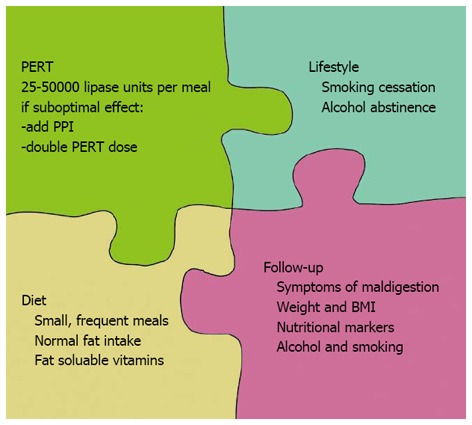
Fundamental aspects in the care of patients with pancreatic exocrine insufficiency. PERT: Pancreatic enzyme replacement therapy; PPI: Proton pump inhibitors.
Diet, smoking and drinking
Historically, a low-fat diet has been recommended in PEI to reduce steatorrhea. This recommendation has been abandoned in modern dietary counseling in PEI due to the risk of aggravating PEI-related weight loss and deficiencies of lipid-soluble vitamins[18,51]. By optimization of the PERT dose and supportive treatment with PPI, most PEI patients will tolerate a normal-fat diet. Dietary consultation should include advice for sufficient caloric intake and normal fat content. Small, frequent meals are usually better tolerated than large, high-caloric meals. Deficiencies of fat-soluble vitamins are very common in PEI patients, and vitamin supplementation therapy should be given if necessary[15]. Support for alcohol abstinence should be offered to all patients with alcohol-related CP. In addition to the general health benefits of alcohol withdrawal, this withdrawal has also been demonstrated to slow the further deterioration of pancreatic exocrine function[52]. Smoking is a risk factor for pancreatic cancer, acute pancreatitis and CP[53], and is also associated with an increased probability of reduced pancreatic exocrine function based on the endoscopic pancreatic function test in cases with CP[54]. Continued smoking has been associated with earlier development of calcifications in patients with CP[55]. Smoking cessation should be encouraged in all patients with CP with or without PEI.
Pancreatic enzyme replacement therapy
Pancreatic digestive enzymes can be administered orally, together with meals, in patients with PEI to compensate for the lack of endogenous enzyme secretion. Modern pancreatic enzyme preparations are extracts from the porcine pancreas (pancrelipase) that are administered as enteric-coated minimicrospheres. Several different preparations are commercially available, with minor differences in particle size and pH-related release kinetics[56]. PEI with steatorrhea and/or weight loss is an undisputed indication for PERT. Several studies have demonstrated an improved coefficient of fat absorption[57-60], decreased maldigestion-related symptoms[57,59-61] and even improved quality of life[61,62]. The need for PERT in PEI without symptoms is a matter of debate, and randomized clinical trials on this issue are lacking. Nevertheless, certain collateral evidence supports PERT, even in the absence of overt steatorrhea and weight loss: (1) A longitudinal study in patients with CP demonstrated that patients with no clinical symptoms of steatorrhea but an abnormal steatocrit who did not receive PERT lost more weight than not only CP patients with a normal steatocrit but also patients with an abnormal steatocrit and symptoms of steatorrhea who were treated with PERT[63]; (2) Laboratory signs of malnutrition have been demonstrated in a large proportion of patients with CP and asymptomatic steatorrhea who were not under treatment with PERT[64]. The clinical relevance of such deficiencies has not been specifically investigated in CP and PEI, but an increased risk of complications that are generally associated with malnutrition can be assumed[65]; and (3) Based on observational studies in CP, it is well known that malnutrition-related diseases and findings, such as osteoporosis-related fractures[16], decreased bone mineral density[15,66,67] and deficiencies of fat-soluble vitamins[15], are common in CP.
As evidence for nutritional deficiencies in patients with PEI with and without symptoms has increased in recent years, PERT is now increasingly regarded as a treatment for maldigestion rather than a way to suppress diarrhea in patients with CP[65]. The goal of PERT is stated to be the elimination of maldigestion in the Australasian Pancreatic Club recommendations[18]. Meanwhile, the Spanish Pancreatic Club regards any clinical or nutritional deficiency in a CP patient as an indication for PERT[68], and the Italian Association for the Study of the Pancreas states in its guidelines that PEI is an indication for PERT[19].
The safety and efficacy of PERT for the treatment of PEI in CP has been investigated in four randomized, double-blinded, placebo-controlled clinical trials including up to 72 patients over study periods of 1-2 wk[57-60]. Significant improvements in the coefficient of fat absorption[57-60], the coefficient of nitrogen absorption[58-60], stool fat content[60] and stool weight[60] have been documented. Two of these trials have also reported results from open-label extension periods of 6 and 12 mo[62,69]. Continuous improvement during treatment, with a steady-state reached at week 13, was observed for most symptom variables[62]. In these clinical trials, PERT has been well tolerated, and no serious adverse events have been reported. Fibrosing colonopathy is the only serious complication that has been associated with PERT. In the vast majority of reported cases, this rare condition has been observed in patients with cystic fibrosis using high doses of PERT[70]. The pathophysiology of this condition is unknown, but factors related to cystic fibrosis disease per se, the dosing of PERT and possibly agents in the enteric coating of the pancrelipase preparations may play a role[71].
There are no studies investigating the long-term effects of PERT on morbidity and mortality from PEI, which should be kept in mind if patients with no or minimal symptoms of PEI are considered for PERT.
Dosing of pancreatic enzyme replacement therapy
The concept of PERT is to induce a lipolytic capacity that corresponds to the amount of ingested fat at every meal. Therefore, higher doses are necessary for large, high-fat meals, and lower doses are sufficient for snacks and lean meals. The optimal dose of PERT in CP has not been investigated systematically in clinical trials. Recommendations from different national societies range from 20-40000 lipase units per main meal, as recommended by the German Society of Digestive and Metabolic Diseases[72], to 25-40000 lipase units per main meal, as recommended by the Australasian Pancreatic Club[18] and the Italian Association for the Study of the Pancreas[19], to 40-50000 lipase units per mail mean, as recommended by The Spanish Pancreatic Club[68]. In general, half of the dose is recommended for snacks and minor meals. Recent randomized clinical trials have used higher doses (72000 USP units[59] and 80000 Ph.Eur.U units[60] per main meal). It is noteworthy that even in a study using 80000 lipase units per main meal, only 26% of the patients had a normalized coefficient of fat absorption at the end of the 51-wk open-label extension of the study[62].
There is no consensus on the definition of treatment success in PERT. If the elimination of maldigestion is accepted as the aim of the treatment, fecal fat quantification or an indirect test of maldigestion, such as the 13C-MTG breath test, would be the most appropriate examination for verifying treatment success. However, this approach is rarely feasible in clinical practice. Most guidelines recommend a reevaluation of symptoms and weight and a reevaluation of serum tests of malnutrition.
In fact, it is highly likely that many patients with PEI today are receiving PERT that is suboptimal. A recent study from the Netherlands has indicated that as many as 70% of patients with CP report steatorrhea-related symptoms despite PERT[73] and that persistent deficits in blood nutritional parameters despite PERT are common in PEI[15,64]. What measures can be taken to optimize the result of PERT? First, it is of utmost importance to ensure that the patient is taking the prescribed dose correctly. Capsules should be administered with meals (as opposed to before or after) for optimal effect[74]. If signs or symptoms of maldigestion persist, the PERT dose can be increased, and proton pump inhibitors can be added[44,75,76]. The rational for adjuvant treatment with proton pump inhibitors is that bicarbonate secretion is impaired in CP, resulting in insufficient buffering of the gastric chyme when it enters the small bowel. This phenomenon may in turn compromise the effect of PERT because lipase is rapidly degraded at a low pH and because enzyme release from microspheres is pH dependent. If PERT is ineffective despite an increased dose and adjuvant treatment with PPI, the diagnosis of PEI should be revised, and possible coexisting and/or alternative reasons for maldigestion, such as small intestinal bacterial overgrowth, should be considered. A summary of PERT concepts in clinical practice is presented in Table 2.
Table 2.
Pancreatic enzyme replacement therapy: How we do it
| PERT is started at 50000 lipase units per main meal and 25000 lipase units per snack |
| The basic concepts of the pathophysiology of PEI and how PERT works are explained to the patient. It is emphasized that PERT should be taken with meals and that the dose should be adjusted to the fat content of the meal |
| If maldigestion persists, proton pump inhibitors can be added, and the dose is increased to 80000 lipase units per main meal and 40000 lipase units per snack |
| If PERT is still ineffective, despite the optimization described above, small intestinal bacterial overgrowth is considered, and the evidence for a diagnosis of PEI is revised |
PEI: Pancreatic exocrine insufficiency; PERT: Pancreatic enzyme replacement therapy.
In conclusion, PEI is a state of maldigestion that is the result of a reduction of pancreatic enzyme activity in the intestinal lumen to a level that is below the threshold required to maintain normal digestion. CP is the most common cause of PEI, but several other pancreatic and extrapancreatic diseases can lead to PEI. The diagnosis of PEI is best established by tests that directly measure digestion, such as fecal fat quantification or the 13C-MTG breath test. If these tests are not available, clinical and biochemical signs of malnutrition; pancreatic imaging findings; and tests that measure pancreatic secretion, such as the FE-1 assay, can be used to estimate the probability of PEI. The treatment of PEI relies on the elimination of risk factors for disease progression, such as smoking and alcohol consumption; consultation with a dietitian; PERT; and a systematic follow-up of the treatment effect on nutritional status and symptoms. If required, PERT can be optimized by dose augmentation and the addition of proton pump inhibitors.
Footnotes
P- Reviewers: Du YQ, Fernandez-Zapico ME, Wassef W, Zhang JX S- Editor: Wen LL L- Editor: A E- Editor: Liu XM
References
- 1.DiMagno EP, Go VL, Summerskill WH. Relations between pancreatic enzyme ouputs and malabsorption in severe pancreatic insufficiency. N Engl J Med. 1973;288:813–815. doi: 10.1056/NEJM197304192881603. [DOI] [PubMed] [Google Scholar]
- 2.Leeds JS, Hopper AD, Hurlstone DP, Edwards SJ, McAlindon ME, Lobo AJ, Donnelly MT, Morley S, Sanders DS. Is exocrine pancreatic insufficiency in adult coeliac disease a cause of persisting symptoms? Aliment Pharmacol Ther. 2007;25:265–271. doi: 10.1111/j.1365-2036.2006.03206.x. [DOI] [PubMed] [Google Scholar]
- 3.Kingham JG, Levison DA, Fairclough PD. Diarrhoea and reversible enteropathy in Zollinger-Ellison syndrome. Lancet. 1981;2:610–612. doi: 10.1016/s0140-6736(81)92746-x. [DOI] [PubMed] [Google Scholar]
- 4.Domínguez-Muñoz JE. Pancreatic enzyme replacement therapy: exocrine pancreatic insufficiency after gastrointestinal surgery. HPB (Oxford) 2009;11 Suppl 3:3–6. doi: 10.1111/j.1477-2574.2009.00132.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keller J, Layer P. Human pancreatic exocrine response to nutrients in health and disease. Gut. 2005;54 Suppl 6:vi1–v28. doi: 10.1136/gut.2005.065946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anagnostides A, Chadwick VS, Selden AC, Maton PN. Sham feeding and pancreatic secretion. Evidence for direct vagal stimulation of enzyme output. Gastroenterology. 1984;87:109–114. [PubMed] [Google Scholar]
- 7.White TT, Mcalexander RA, Magee DF. The effect of gastric distension on duodenal aspirates in man. Gastroenterology. 1963;44:48–51. [PubMed] [Google Scholar]
- 8.Watanabe S, Shiratori K, Takeuchi T, Chey WY, You CH, Chang TM. Release of cholecystokinin and exocrine pancreatic secretion in response to an elemental diet in human subjects. Dig Dis Sci. 1986;31:919–924. doi: 10.1007/BF01303211. [DOI] [PubMed] [Google Scholar]
- 9.Pandol SJ. Neurohumoral control of exocrine pancreatic secretion. Curr Opin Gastroenterol. 2003;19:443–446. doi: 10.1097/00001574-200309000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Schaffalitzky de Muckadell OB, Fahrenkrug J, Nielsen J, Westphall I, Worning H. Meal-stimulated secretin release in man: effect of acid and bile. Scand J Gastroenterol. 1981;16:981–988. doi: 10.3109/00365528109181015. [DOI] [PubMed] [Google Scholar]
- 11.Schaffalitzky de Muckadell OB, Fahrenkrug J, Watt-Boolsen S, Worning H. Pancreatic response and plasma secretin concentration during infusion of low dose secretin in man. Scand J Gastroenterol. 1978;13:305–311. doi: 10.3109/00365527809179825. [DOI] [PubMed] [Google Scholar]
- 12.DiMagno EP, Malagelada JR, Go VL, Moertel CG. Fate of orally ingested enzymes in pancreatic insufficiency. Comparison of two dosage schedules. N Engl J Med. 1977;296:1318–1322. doi: 10.1056/NEJM197706092962304. [DOI] [PubMed] [Google Scholar]
- 13.Layer P, Yamamoto H, Kalthoff L, Clain JE, Bakken LJ, DiMagno EP. The different courses of early- and late-onset idiopathic and alcoholic chronic pancreatitis. Gastroenterology. 1994;107:1481–1487. doi: 10.1016/0016-5085(94)90553-3. [DOI] [PubMed] [Google Scholar]
- 14.Lindkvist B, Domínguez-Muñoz JE, Luaces-Regueira M, Castiñeiras-Alvariño M, Nieto-Garcia L, Iglesias-Garcia J. Serum nutritional markers for prediction of pancreatic exocrine insufficiency in chronic pancreatitis. Pancreatology. 2012;12:305–310. doi: 10.1016/j.pan.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 15.Sikkens EC, Cahen DL, Koch AD, Braat H, Poley JW, Kuipers EJ, Bruno MJ. The prevalence of fat-soluble vitamin deficiencies and a decreased bone mass in patients with chronic pancreatitis. Pancreatology. 2013;13:238–242. doi: 10.1016/j.pan.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 16.Tignor AS, Wu BU, Whitlock TL, Lopez R, Repas K, Banks PA, Conwell D. High prevalence of low-trauma fracture in chronic pancreatitis. Am J Gastroenterol. 2010;105:2680–2686. doi: 10.1038/ajg.2010.325. [DOI] [PubMed] [Google Scholar]
- 17.Van De Kamer JH, Ten Bokkel Huinink H, Weyers HA. Rapid method for the determination of fat in feces. J Biol Chem. 1949;177:347–355. [PubMed] [Google Scholar]
- 18.Toouli J, Biankin AV, Oliver MR, Pearce CB, Wilson JS, Wray NH. Management of pancreatic exocrine insufficiency: Australasian Pancreatic Club recommendations. Med J Aust. 2010;193:461–467. doi: 10.5694/j.1326-5377.2010.tb04000.x. [DOI] [PubMed] [Google Scholar]
- 19.Frulloni L, Falconi M, Gabbrielli A, Gaia E, Graziani R, Pezzilli R, Uomo G, Andriulli A, Balzano G, Benini L, et al. Italian consensus guidelines for chronic pancreatitis. Dig Liver Dis. 2010;42 Suppl 6:S381–S406. doi: 10.1016/S1590-8658(10)60682-2. [DOI] [PubMed] [Google Scholar]
- 20.Hartmann D, Felix K, Ehmann M, Schnölzer M, Fiedler S, Bogumil R, Büchler M, Friess H. Protein expression profiling reveals distinctive changes in serum proteins associated with chronic pancreatitis. Pancreas. 2007;35:334–342. doi: 10.1097/mpa.0b013e3180cac723. [DOI] [PubMed] [Google Scholar]
- 21.Montalto G, Soresi M, Carroccio A, Scafidi E, Barbagallo CM, Ippolito S, Notarbartolo A. Lipoproteins and chronic pancreatitis. Pancreas. 1994;9:137–138. doi: 10.1097/00006676-199401000-00021. [DOI] [PubMed] [Google Scholar]
- 22.Sobral-Oliveira MB, Faintuch J, Guarita DR, Oliveira CP, Carrilho FJ. Nutritional profile of asymptomatic alcoholic patients. Arq Gastroenterol. 2011;48:112–118. doi: 10.1590/s0004-28032011000200006. [DOI] [PubMed] [Google Scholar]
- 23.Schnitzler CM, Mesquita JM, Shires R. Cortical and trabecular bone microarchitecture and turnover in alcohol-induced chronic pancreatitis: a histomorphometric study. J Bone Miner Metab. 2010;28:456–467. doi: 10.1007/s00774-009-0151-x. [DOI] [PubMed] [Google Scholar]
- 24.Kalvaria I, Labadarios D, Shephard GS, Visser L, Marks IN. Biochemical vitamin E deficiency in chronic pancreatitis. Int J Pancreatol. 1986;1:119–128. doi: 10.1007/BF02788444. [DOI] [PubMed] [Google Scholar]
- 25.Twersky Y, Bank S. Nutritional deficiencies in chronic pancreatitis. Gastroenterol Clin North Am. 1989;18:543–565. [PubMed] [Google Scholar]
- 26.Marotta F, Labadarios D, Frazer L, Girdwood A, Marks IN. Fat-soluble vitamin concentration in chronic alcohol-induced pancreatitis. Relationship with steatorrhea. Dig Dis Sci. 1994;39:993–998. doi: 10.1007/BF02087550. [DOI] [PubMed] [Google Scholar]
- 27.Glasbrenner B, Malfertheiner P, Büchler M, Kuhn K, Ditschuneit H. Vitamin B12 and folic acid deficiency in chronic pancreatitis: a relevant disorder? Klin Wochenschr. 1991;69:168–172. doi: 10.1007/BF01665861. [DOI] [PubMed] [Google Scholar]
- 28.Domínguez-Muñoz JE, Alvarez-Castro A, Lariño-Noia J, Nieto L, Iglesias-García J. Endoscopic ultrasonography of the pancreas as an indirect method to predict pancreatic exocrine insufficiency in patients with chronic pancreatitis. Pancreas. 2012;41:724–728. doi: 10.1097/MPA.0b013e31823b5978. [DOI] [PubMed] [Google Scholar]
- 29.Domínguez-Muñoz JE, Manes G, Pieramico O, Büchler M, Malfertheiner P. Effect of pancreatic ductal and parenchymal changes on exocrine function in chronic pancreatitis. Pancreas. 1995;10:31–35. doi: 10.1097/00006676-199501000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Catalano MF, Sahai A, Levy M, Romagnuolo J, Wiersema M, Brugge W, Freeman M, Yamao K, Canto M, Hernandez LV. EUS-based criteria for the diagnosis of chronic pancreatitis: the Rosemont classification. Gastrointest Endosc. 2009;69:1251–1261. doi: 10.1016/j.gie.2008.07.043. [DOI] [PubMed] [Google Scholar]
- 31.Sziegoleit A, Krause E, Klör HU, Kanacher L, Linder D. Elastase 1 and chymotrypsin B in pancreatic juice and feces. Clin Biochem. 1989;22:85–89. doi: 10.1016/s0009-9120(89)80003-7. [DOI] [PubMed] [Google Scholar]
- 32.Löser C, Möllgaard A, Fölsch UR. Faecal elastase 1: a novel, highly sensitive, and specific tubeless pancreatic function test. Gut. 1996;39:580–586. doi: 10.1136/gut.39.4.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leeds JS, Oppong K, Sanders DS. The role of fecal elastase-1 in detecting exocrine pancreatic disease. Nat Rev Gastroenterol Hepatol. 2011;8:405–415. doi: 10.1038/nrgastro.2011.91. [DOI] [PubMed] [Google Scholar]
- 34.Stein J, Jung M, Sziegoleit A, Zeuzem S, Caspary WF, Lembcke B. Immunoreactive elastase I: clinical evaluation of a new noninvasive test of pancreatic function. Clin Chem. 1996;42:222–226. [PubMed] [Google Scholar]
- 35.Hardt PD, Marzeion AM, Schnell-Kretschmer H, Wüsten O, Nalop J, Zekorn T, Klör HU. Fecal elastase 1 measurement compared with endoscopic retrograde cholangiopancreatography for the diagnosis of chronic pancreatitis. Pancreas. 2002;25:e6–e9. doi: 10.1097/00006676-200207000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Bilgin M, Bilgin S, Balci NC, Momtahen AJ, Bilgin Y, Klör HU, Rau WS. Magnetic resonance imaging and magnetic resonance cholangiopancreatography findings compared with fecal elastase 1 measurement for the diagnosis of chronic pancreatitis. Pancreas. 2008;36:e33–e39. doi: 10.1097/mpa.0b013e318150e557. [DOI] [PubMed] [Google Scholar]
- 37.Benini L, Amodio A, Campagnola P, Agugiaro F, Cristofori C, Micciolo R, Magro A, Gabbrielli A, Cabrini G, Moser L, et al. Fecal elastase-1 is useful in the detection of steatorrhea in patients with pancreatic diseases but not after pancreatic resection. Pancreatology. 2013;13:38–42. doi: 10.1016/j.pan.2012.11.307. [DOI] [PubMed] [Google Scholar]
- 38.Vantrappen GR, Rutgeerts PJ, Ghoos YF, Hiele MI. Mixed triglyceride breath test: a noninvasive test of pancreatic lipase activity in the duodenum. Gastroenterology. 1989;96:1126–1134. doi: 10.1016/0016-5085(89)91632-6. [DOI] [PubMed] [Google Scholar]
- 39.Bożek M, Jonderko K, Piłka M. On a refinement of the ¹³C-mixed TAG breath test. Br J Nutr. 2012;107:211–217. doi: 10.1017/S0007114511002881. [DOI] [PubMed] [Google Scholar]
- 40.Iglesias-Garcia J, Vilarino M, Iglesias-Rey M, Lourido V, Dominguez-Munoz E. Accuracy of the optimized 13C-mixed triglyceride breath test for the diagnosis of steatorrhea in clinical practice. Gastroenterology. 2003;124 Supp 1:A631. [Google Scholar]
- 41.Boedeker C, Goetze O, Pfaffenbach B, Luypaerts A, Geypens B, Adamek RJ. 13C mixed-triglyceride breath test: isotope selective non-dispersive infrared spectrometry in comparison with isotope ratio mass spectrometry in volunteers and patients with chronic pancreatitis. Scand J Gastroenterol. 1999;34:1153–1156. doi: 10.1080/003655299750024977. [DOI] [PubMed] [Google Scholar]
- 42.Löser C, Brauer C, Aygen S, Hennemann O, Fölsch UR. Comparative clinical evaluation of the 13C-mixed triglyceride breath test as an indirect pancreatic function test. Scand J Gastroenterol. 1998;33:327–334. doi: 10.1080/00365529850170946. [DOI] [PubMed] [Google Scholar]
- 43.Keller J, Brückel S, Jahr C, Layer P. A modified ¹³C-mixed triglyceride breath test detects moderate pancreatic exocrine insufficiency. Pancreas. 2011;40:1201–1205. doi: 10.1097/MPA.0b013e318220ad98. [DOI] [PubMed] [Google Scholar]
- 44.Domínguez-Muñoz JE, Iglesias-García J, Vilariño-Insua M, Iglesias-Rey M. 13C-mixed triglyceride breath test to assess oral enzyme substitution therapy in patients with chronic pancreatitis. Clin Gastroenterol Hepatol. 2007;5:484–488. doi: 10.1016/j.cgh.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 45.Burton P, Evans DG, Harper AA, Howath T, Oleesky S, Scott JE, Varley H. A test of pancreatic function in man based on the analysis of duodenal contents after administration of secretin and pancreozymin. Gut. 1960;1:111–124. doi: 10.1136/gut.1.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Borgstrom B, Dahlqvist A, Lundh G. On the site of absorption of fat from the human small intestine. Gut. 1962;3:315–317. doi: 10.1136/gut.3.4.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stevens T, Conwell DL, Zuccaro G, Van Lente F, Lopez R, Purich E, Fein S. A prospective crossover study comparing secretin-stimulated endoscopic and Dreiling tube pancreatic function testing in patients evaluated for chronic pancreatitis. Gastrointest Endosc. 2008;67:458–466. doi: 10.1016/j.gie.2007.07.028. [DOI] [PubMed] [Google Scholar]
- 48.Stevens T, Conwell DL, Zuccaro G, Van Lente F, Purich E, Khandwala F, Fein S. A randomized crossover study of secretin-stimulated endoscopic and dreiling tube pancreatic function test methods in healthy subjects. Am J Gastroenterol. 2006;101:351–355. doi: 10.1111/j.1572-0241.2006.00407.x. [DOI] [PubMed] [Google Scholar]
- 49.Schneider AR, Hammerstingl R, Heller M, Povse N, Murzynski L, Vogl TJ, Caspary WF, Stein J. Does secretin-stimulated MRCP predict exocrine pancreatic insufficiency?: A comparison with noninvasive exocrine pancreatic function tests. J Clin Gastroenterol. 2006;40:851–855. doi: 10.1097/01.mcg.0000225652.00308.a2. [DOI] [PubMed] [Google Scholar]
- 50.Balci NC, Smith A, Momtahen AJ, Alkaade S, Fattahi R, Tariq S, Burton F. MRI and S-MRCP findings in patients with suspected chronic pancreatitis: correlation with endoscopic pancreatic function testing (ePFT) J Magn Reson Imaging. 2010;31:601–606. doi: 10.1002/jmri.22085. [DOI] [PubMed] [Google Scholar]
- 51.Domínguez-Muñoz JE. Pancreatic exocrine insufficiency: diagnosis and treatment. J Gastroenterol Hepatol. 2011;26 Suppl 2:12–16. doi: 10.1111/j.1440-1746.2010.06600.x. [DOI] [PubMed] [Google Scholar]
- 52.Gullo L, Barbara L, Labò G. Effect of cessation of alcohol use on the course of pancreatic dysfunction in alcoholic pancreatitis. Gastroenterology. 1988;95:1063–1068. doi: 10.1016/0016-5085(88)90184-9. [DOI] [PubMed] [Google Scholar]
- 53.Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144:1252–1261. doi: 10.1053/j.gastro.2013.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Law R, Parsi M, Lopez R, Zuccaro G, Stevens T. Cigarette smoking is independently associated with chronic pancreatitis. Pancreatology. 2010;10:54–59. doi: 10.1159/000225927. [DOI] [PubMed] [Google Scholar]
- 55.Maisonneuve P, Lowenfels AB, Müllhaupt B, Cavallini G, Lankisch PG, Andersen JR, Dimagno EP, Andrén-Sandberg A, Domellöf L, Frulloni L, et al. Cigarette smoking accelerates progression of alcoholic chronic pancreatitis. Gut. 2005;54:510–514. doi: 10.1136/gut.2004.039263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Löhr JM, Hummel FM, Pirilis KT, Steinkamp G, Körner A, Henniges F. Properties of different pancreatin preparations used in pancreatic exocrine insufficiency. Eur J Gastroenterol Hepatol. 2009;21:1024–1031. doi: 10.1097/MEG.0b013e328328f414. [DOI] [PubMed] [Google Scholar]
- 57.Safdi M, Bekal PK, Martin S, Saeed ZA, Burton F, Toskes PP. The effects of oral pancreatic enzymes (Creon 10 capsule) on steatorrhea: a multicenter, placebo-controlled, parallel group trial in subjects with chronic pancreatitis. Pancreas. 2006;33:156–162. doi: 10.1097/01.mpa.0000226884.32957.5e. [DOI] [PubMed] [Google Scholar]
- 58.Toskes PP, Secci A, Thieroff-Ekerdt R. Efficacy of a novel pancreatic enzyme product, EUR-1008 (Zenpep), in patients with exocrine pancreatic insufficiency due to chronic pancreatitis. Pancreas. 2011;40:376–382. doi: 10.1097/MPA.0b013e31820b971c. [DOI] [PubMed] [Google Scholar]
- 59.Whitcomb DC, Lehman GA, Vasileva G, Malecka-Panas E, Gubergrits N, Shen Y, Sander-Struckmeier S, Caras S. Pancrelipase delayed-release capsules (CREON) for exocrine pancreatic insufficiency due to chronic pancreatitis or pancreatic surgery: A double-blind randomized trial. Am J Gastroenterol. 2010;105:2276–2286. doi: 10.1038/ajg.2010.201. [DOI] [PubMed] [Google Scholar]
- 60.Thorat V, Reddy N, Bhatia S, Bapaye A, Rajkumar JS, Kini DD, Kalla MM, Ramesh H. Randomised clinical trial: the efficacy and safety of pancreatin enteric-coated minimicrospheres (Creon 40000 MMS) in patients with pancreatic exocrine insufficiency due to chronic pancreatitis--a double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2012;36:426–436. doi: 10.1111/j.1365-2036.2012.05202.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Czakó L, Takács T, Hegyi P, Prónai L, Tulassay Z, Lakner L, Döbrönte Z, Boda K, Lonovics J. Quality of life assessment after pancreatic enzyme replacement therapy in chronic pancreatitis. Can J Gastroenterol. 2003;17:597–603. doi: 10.1155/2003/515848. [DOI] [PubMed] [Google Scholar]
- 62.Ramesh H, Reddy N, Bhatia S, Rajkumar JS, Bapaye A, Kini D, Kalla M, Thorat V. A 51-week, open-label clinical trial in India to assess the efficacy and safety of pancreatin 40000 enteric-coated minimicrospheres in patients with pancreatic exocrine insufficiency due to chronic pancreatitis. Pancreatology. 2013;13:133–139. doi: 10.1016/j.pan.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 63.Dumasy V, Delhaye M, Cotton F, Deviere J. Fat malabsorption screening in chronic pancreatitis. Am J Gastroenterol. 2004;99:1350–1354. doi: 10.1111/j.1572-0241.2004.30661.x. [DOI] [PubMed] [Google Scholar]
- 64.Domínguez-Muñoz JE, Iglesias-García J. Oral pancreatic enzyme substitution therapy in chronic pancreatitis: is clinical response an appropriate marker for evaluation of therapeutic efficacy? JOP. 2010;11:158–162. [PubMed] [Google Scholar]
- 65.Domínguez-Muñoz JE. Chronic pancreatitis and persistent steatorrhea: what is the correct dose of enzymes? Clin Gastroenterol Hepatol. 2011;9:541–546. doi: 10.1016/j.cgh.2011.02.027. [DOI] [PubMed] [Google Scholar]
- 66.Morán CE, Sosa EG, Martinez SM, Geldern P, Messina D, Russo A, Boerr L, Bai JC. Bone mineral density in patients with pancreatic insufficiency and steatorrhea. Am J Gastroenterol. 1997;92:867–871. [PubMed] [Google Scholar]
- 67.Haaber AB, Rosenfalck AM, Hansen B, Hilsted J, Larsen S. Bone mineral metabolism, bone mineral density, and body composition in patients with chronic pancreatitis and pancreatic exocrine insufficiency. Int J Pancreatol. 2000;27:21–27. doi: 10.1385/IJGC:27:1:21. [DOI] [PubMed] [Google Scholar]
- 68.de-Madaria E, Abad-González A, Aparicio JR, Aparisi L, Boadas J, Boix E, de-Las-Heras G, Domínguez-Muñoz E, Farré A, Fernández-Cruz L, et al. The Spanish Pancreatic Club’s recommendations for the diagnosis and treatment of chronic pancreatitis: part 2 (treatment) Pancreatology. 2013;13:18–28. doi: 10.1016/j.pan.2012.11.310. [DOI] [PubMed] [Google Scholar]
- 69.Gubergrits N, Malecka-Panas E, Lehman GA, Vasileva G, Shen Y, Sander-Struckmeier S, Caras S, Whitcomb DC. A 6-month, open-label clinical trial of pancrelipase delayed-release capsules (Creon) in patients with exocrine pancreatic insufficiency due to chronic pancreatitis or pancreatic surgery. Aliment Pharmacol Ther. 2011;33:1152–1161. doi: 10.1111/j.1365-2036.2011.04631.x. [DOI] [PubMed] [Google Scholar]
- 70.FitzSimmons SC, Burkhart GA, Borowitz D, Grand RJ, Hammerstrom T, Durie PR, Lloyd-Still JD, Lowenfels AB. High-dose pancreatic-enzyme supplements and fibrosing colonopathy in children with cystic fibrosis. N Engl J Med. 1997;336:1283–1289. doi: 10.1056/NEJM199705013361803. [DOI] [PubMed] [Google Scholar]
- 71.Nakajima K, Oshida H, Muneyuki T, Kakei M. Pancrelipase: an evidence-based review of its use for treating pancreatic exocrine insufficiency. Core Evid. 2012;7:77–91. doi: 10.2147/CE.S26705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hoffmeister A, Mayerle J, Beglinger C, Büchler MW, Bufler P, Dathe K, Fölsch UR, Friess H, Izbicki J, Kahl S, et al. [S3-Consensus guidelines on definition, etiology, diagnosis and medical, endoscopic and surgical management of chronic pancreatitis German Society of Digestive and Metabolic Diseases (DGVS)] Z Gastroenterol. 2012;50:1176–1224. doi: 10.1055/s-0032-1325479. [DOI] [PubMed] [Google Scholar]
- 73.Sikkens EC, Cahen DL, van Eijck C, Kuipers EJ, Bruno MJ. Patients with exocrine insufficiency due to chronic pancreatitis are undertreated: a Dutch national survey. Pancreatology. 2012;12:71–73. doi: 10.1016/j.pan.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 74.Domínguez-Muñoz JE, Iglesias-García J, Iglesias-Rey M, Figueiras A, Vilariño-Insua M. Effect of the administration schedule on the therapeutic efficacy of oral pancreatic enzyme supplements in patients with exocrine pancreatic insufficiency: a randomized, three-way crossover study. Aliment Pharmacol Ther. 2005;21:993–1000. doi: 10.1111/j.1365-2036.2005.02390.x. [DOI] [PubMed] [Google Scholar]
- 75.Bruno MJ, Rauws EA, Hoek FJ, Tytgat GN. Comparative effects of adjuvant cimetidine and omeprazole during pancreatic enzyme replacement therapy. Dig Dis Sci. 1994;39:988–992. doi: 10.1007/BF02087549. [DOI] [PubMed] [Google Scholar]
- 76.Regan PT, Malagelada JR, DiMagno EP, Glanzman SL, Go VL. Comparative effects of antacids, cimetidine and enteric coating on the therapeutic response to oral enzymes in severe pancreatic insufficiency. N Engl J Med. 1977;297:854–858. doi: 10.1056/NEJM197710202971603. [DOI] [PubMed] [Google Scholar]


