Abstract
Background
Orthoses are external aids that are often used to treat pain and diseases affecting the spine, such as lumbago, whiplash, and disc herniation. In this review, we assess the effectiveness and complications of orthotic treatment for typical spinal conditions and after spinal surgery. The orthotic treatment of fractures and postural abnormalities are beyond the scope of this article.
Methods
This review is based on a selective search in the Medline database with consideration of controlled trials, systematic reviews, and the recommendations of the relevant medical societies.
Results
Three relevant systematic reviews and four controlled trials were found. Very few controlled trials to date have studied the efficacy of orthotic treatment compared to other conservative treatments and surgery. No definitive evidence was found to support the use of orthoses after surgery, in lumbar radiculopathy, or after whiplash injuries of the cervical spine. In a single trial, short-term immobilization was an effective treatment of cervical radiculopathy. Orthoses are not recommended for nonspecific low back pain. The potential complications of cervical orthoses include pressure-related skin injuries and dysphagia.
Conclusion
No definitive evidence as yet supports the use of orthoses after spinal interventions or in painful conditions of the cervical or lumbar spine. They should, therefore, be used only after individual consideration of the indications in each case.
Orthoses are medical devices classified as prescription-only technical aids in Germany (1). The catalog of technical aids defines them as aids that safeguard function and enclose or fit against the body. Their physical or mechanical properties aim to do one or more of the following: to stabilize, immobilize, mobilize, reduce load, correct, retain, fix, redress, or replace lost bodily functions (1). In addition to custom orthoses, off-the-shelf ready-made orthoses produced in a unit assembly system are also available. Closely related to orthoses are bandages, made from stiff or elastic fabrics only. The posterior portion of a bandage or orthosis may include a pelotte. Pelottes exert a compressing, massaging effect on soft tissues, in order to release muscular tension and reduce pain.
Orthoses are prescribed frequently in normal clinical practice, due to the high prevalence of spinal disease. Approximately 3% to 7% of the population suffers from chronic low back pain (2), and lumbar orthoses and bandages in particular are therefore used for both primary and secondary prevention (3). The frequency of prescription of spinal orthoses and bandages has not yet been systematically collated. Inquiries put to BARMER GEK, a large German statutory health insurance fund, reported that the number of orthoses and bandages for which reimbursement had been provided in 2011 increased by 45% to 97 425 (from 67 211 in 2009 and 72 633 in 2010: personal communication, BARMER press office, June 25, 2012). It is therefore worth asking for which spinal indications there is evidence that orthoses and bandages are effective.
This review article aims firstly to describe how treatment with spinal orthoses and bandages works biomechanically. Next, it gives an overview of the clinical findings from controlled clinical trials and reviews, in order to provide recommendations for the indication of orthotic treatment for the most common acute and chronic diseases of the cervical and lumbar spine. Due to space restrictions, the orthotic treatment of deformities (scoliosis, kyphosis), fractures, vertebral tumors posing a risk of fracture, or the thoracic spine will not be discussed in this article.
Biomechanical aspects
The aim of orthotic treatment is to correct an existing deformity or to prevent progression according to the three point pressure principle (by which two aligned forces oppose a single force placed at the area of deformity or angulation), to stabilize and immobilize weak or damaged spinal segments, to reduce the axial load on the affected sections of the spine, and to control motion (4, 5). Different functional aspects of an orthosis are emphasized for different indications. Secondary effects of orthotic treatment that have been postulated are massage of the soft tissues, warming, and a placebo effect (5). An orthosis should warn the patient to prevent excessive motion and improve posture thanks to tactile stimuli (6). It should also aid the patient in performing occupational therapy or at least help slow down specific movements (4).
Another hypothesis is that orthoses increase intra-abdominal pressure, leading to a reduction in the work performed by the lumbar musculature in upright position (6). A systematic review failed to find evidence for the hypothesis that this reduces the load on the muscles and the axial load on the lumbar spine (6, 7). There is evidence that both soft and rigid lumbar orthoses lead to a significant restriction of flexion and extension and lateral motion. No evidence was found of a significant reduction in rotation, which is considered to be a risk factor for back pain (6). Because some of the findings of biomechanical studies are contradictory, it is not currently possible to give a definitive assessment of the mechanism of action of orthoses (6).
Soft cervical bandages (Figure 1a) and rigid orthoses (Figure 1b) are used on the cervical spine. As is logical, soft cervical bandages have little effect on cervical spine mobility (4).
Figure 1.

Cervical orthoses
a) Soft, anatomically-shaped cervical bandage
b) Philadelphia collar

The cervical spine is difficult to immobilize due to the small contact surface area between an orthosis and the occiput, the mandible, and the clavicle, as well as the limited possibility of compressing the soft tissues of the throat. As a result, there is a certain amount of mobility in the cervical spine during chewing and shoulder movement (8). Even a rigid Philadelphia collar allows considerable motion: 29% for flexion and extension, 44% for rotation, and 66% for lateral inclination (4).
Clinical indications
Whiplash
Approximately 200 000 whiplash injuries occur in Germany every year (9). The main clinical symptoms are neck pain (88% to 100%) and headaches (54% to 66%) (9). After skeletal injury has been ruled out, a soft cervical bandage is often prescribed. A systematic review determined the efficacy of various conservative forms of treatment with the primary parameters pain, global perceived effect, and participation in daily activities (9). Five of the eleven trials included in the review compared immobilization using cervical bandages to an active, mobilizing therapy regimen (9). Mobilization was superior to immobilization in four of these trials (10– 13), while one found no difference (14). Based on the low methodical quality of the included trials, the authors of the systematic review concluded that active intervention tended to be more effective than immobilization.
Cervical radiculopathy
Cervical radiculopathy often occurs in the context of degenerative processes (e.g. prolapsed disc, spondylarthritis) and is characterized by neck pain with dermatomal radiation to the upper extremity. In general, where there are acute symptoms and surgery is not indicated (in the absence of high-grade paresis) initial treatment is conservative, using analgesics and immobilization or physiotherapy. A positive effect is observed after 3 to 6 months in 80% to 90% of patients (15, 16).
A three-armed randomized controlled trial (RCT) compared immobilization using a semirigid orthosis, physiotherapy, and analgesics alone in patients with acute-onset, neurologically confirmed cervical radiculopathy (n = 207, length of complaint <1 month, visual analog scale (VAS) and neck disability index) (17). At six weeks, immobilization using semirigid orthosis and physiotherapy (twice weekly) were shown to be superior to analgesics alone. At six months there were no significant differences between the groups. The authors recommended immobilization on the grounds that it was more economical than physiotherapy. Other than this trial there are no high-quality trials comparing immobilization to other conservative forms of treatment. The question of whether patients with acute cervicobrachialgia and no neurological limitations also benefit from immobilization remains open.
In a three-armed RCT in patients with chronic radiculopathy (defined as lasting more than three months, median 21 months), Persson et al. determined at four months that surgical treatment was superior to physiotherapy and the use of rigid orthoses (worn for three months) in terms of pain and neurological deficit (18). There were no significant differences between the conservative treatment arms after four months, or between all the treatment groups at one year.
Acute and chronic low back pain
Lumbar and lumbosacral orthoses are often used to treat acute and chronic pain and for prevention. Priority treatment aims are faster mobilization and improvement of symptoms. A 2001 Cochrane Review on the use of lumbar orthoses and bandages to prevent and treat low back pain analyzed 13 controlled trials (5). Only four trials were of good methodical quality; information on the orthoses used and on patient compliance was often lacking. The authors determined that there was no strong evidence (level 1) either for or against the efficacy of lumbar orthoses in the prevention or treatment of low back pain. There was moderate evidence (level 2) against the efficacy of lumbar orthoses in primary prevention. There is no evidence to date on secondary prevention (level 4). The trials’ findings on efficacy in treating low back pain are controversial. There is poor evidence (level 3) that some rigid orthoses are more effective than bandages. Overall, the authors of the review come to the conclusion that lumbar orthoses are not suitable for primary prevention or for treatment of lumbar pain. In the latest Cochrane Review, dating from 2008, the authors came to a similar conclusion and therefore concluded that further high-quality randomized controlled trials assessing the efficacy of orthoses were necessary (19).
Germany’s National Disease Management Guideline on Low Back Pain (20) recommends that orthoses should not be used to treat acute or chronic nonspecific low back pain (grade of recommendation A). Data from 10 of a total of 54 identified trials were examined to analyze the evidence for this recommendation. Of these, four trials of moderate methodological quality and one with good methodological quality found no positive efficacy for orthoses versus either other nonpharmacological forms of treatment or no intervention. Five trials that found evidence of a positive effect for orthoses were of moderate methodological quality; the trials with a negative conclusion were therefore rated as being of higher quality.
Spondylodiscitis
A further indication for orthotic treatment is conservative therapy for spondylodiscitis if there is no high-grade destruction of the vertebral body and surgery is not urgently indicated (21). At the thoracolumbar and lumbar level, a stable, custom polyethylene bodice can immobilize the affected spinal segment and reduce the load on the anterior section of the vertebrae thanks to a reclining position (22). Most authors recommend treatment for 6 to 10 weeks using a hard corset combined with antibiotic therapy (23, 24).
Cervical spondylodiscitis is often treated surgically. If the patient is eligible for conservative treatment, immobilization using a rigid orthosis is recommended (21).
To date there are no data from controlled trials concerning rare and heterogeneous-onset spondylodiscitis.
Postoperative orthotic treatment
In an international survey, 61% of spinal surgeons answered that they prescribed orthoses for between one and eight weeks after surgery on the cervical spine, while 49% answered that they prescribed this for surgery on the lumbar spine (25). The main reason given was restriction of patients’ activities as a result of orthotic treatment.
To date there are no data from controlled trials on the efficacy of orthoses following stability-maintaining procedures such as decompression or intervertebral disc surgery on the lumbar spine. Neither is there any consensus on how rigid an orthosis should be, the type of orthosis, or duration of treatment. In our hospital, in line with the judgment of the surgeon, a Hohmann bridging bodice (Figure 2) is prescribed for the first six weeks postsurgically following multisegmental decompression and when there is a risk of instability (4).
Figure 2.
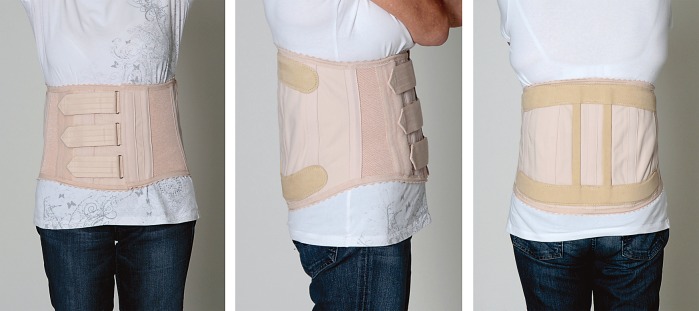
Custom Hohmann bridging bodice
For instrumented screw-and-rod lumbar spinal arthrodesis, fusion rates of between 46% and 100% can be achieved after two years, depending on the underlying disease (26). The use of orthoses in such cases is controversial (27).
One RCT investigated the significance of postoperative corset treatment following lumbar spinal arthrodesis using a posterior screw-and-rod system and autologous iliac crest grafting in degenerative diseases of the lumbar spine (28). Patients in the intervention group (n = 46) were asked to wear a stable, custom corset for eight weeks following surgery, 24 hours a day (except during personal hygiene and examinations), and to undertake physical exercise for a further four weeks. The patients in the control group (n = 44) were mobilized with no orthoses. After two years, there were no significant differences between the two groups in terms of the clinical parameters measured (Dallas Pain Questionnaire and SF-36), postoperative complication rate, or the rate of subsequent lumbar spinal operations. This trial found neither an advantage nor a disadvantage for corset use following lumbar spinal arthrodesis.
The frequent postoperative use of orthoses on the cervical spine may be due to the high mobility of this section of the spine and the frequency of surgical fusion. Most fusions are performed without plate osteosynthesis using intervertebral implants. Orthoses are used to reduce the mobility of and load on the segment upon which surgery is performed and thereby improve the fusion rate. Using modern, synthetic (polyetheretherketone) or titanium alloplastic interbody cages instead of bone cages makes the need for postoperative immobilization questionable in the absence of evidence. In a randomized pilot trial, during the first six weeks following fusion using an interbody cage, patients benefited from immobilization in terms of the neck disability index and a reduction in pain (29).
A multicenter RCT with a follow-up time of 24 months concluded that cervical orthosis is not necessary following monosegmental anterior fusion using plate osteosynthesis (30). Cervical supports did not improve clinical outcome according to the neck disability index, SF-36, or the Numerical Rating Scale (NRS); they also failed to improve the radiological fusion rate.
Complications of orthotic treatment
Treating physicians and patients often believe that wearing an orthosis for longer periods weakens the trunk muscles. Research on this subject yields controversial data, some of which show that these muscles become stronger (31, 32), some that they become weaker (33), and some no difference (34). A study of the isokinetic and isometric strength of healthy subjects showed no significant differences following 21-day use of a lumbar bandage (35).
Excessive pressure exerted by the orthosis on the skin and exposed anatomical structures may lead to ulcers. The use of orthoses should therefore be limited to patients who can perceive such pain stimuli and react to them appropriately.
Depending on the length of time for which they are worn, rigid cervical orthoses can lead to pressure sores on the mandible and the occiput in 6.8% of patients (36, 37). Cervical orthoses can cause dysphagia as result of narrowing of the pharynx, deglutition alterations (38), and an unusually upright head position when eating.
In general, therefore, it is recommended that orthotic treatment should be prescribed and monitored by a physician, with the aim of the shortest possible treatment duration and early patient mobilization.
Key Messages.
Cervical and lumbar orthoses significantly restrict the motion of the treated section of the spine but do not immobilize it completely.
There is no evidence that orthotic treatment for cervical radiculopathy, for whiplash, or following surgery is beneficial to the spine.
According to Germany’s National Disease Management Guideline on Low Back Pain, orthotic treatment of nonspecific back pain cannot be recommended.
Physicians should monitor the duration of orthotic treatment and ensure that orthoses fit well, as incorrect use of orthoses can affect their effectiveness and lead to complications.
Despite the widespread clinical use of orthoses, for many spinal indications there are no high-quality controlled trials demonstrating that they are effective.
Acknowledgments
Translated from the original German by Caroline Devitt, M.A.
Footnotes
Conflict of interest statement
Dr. Zarghooni and Prof. Eysel have received payment for a research project they themselves initiated from Bauerfeind AG in Zeulenroda-Triebes.
Dr. Beyer and Dr. Siewe declare that no conflict of interest exists.
References
- 1.Spitzenverband G. Hilfsmittelverzeichnis 2012. Available from: https://hilfsmittelgkv-spitzenverband.de/home.action. 2012 Last accessed on 26 November. [Google Scholar]
- 2.Anderson G. The epidemiology of spinal disorders. In: Frymeyer JW, editor. The adult spine: principle and practice. 2nd ed. Philadelphia: Lippincott-Raven Publishers; 1997. pp. 93–141. [Google Scholar]
- 3.Dillingham TR. Lumbar supports for prevention of low back pain in the workplace. JAMA. 1998;279:1826–1828. doi: 10.1001/jama.279.22.1826. [DOI] [PubMed] [Google Scholar]
- 4.Agabegi SS, Asghar FA, Herkowitz HN. Spinal orthoses. J Am Acad Orthop Surg. 2010;18:657–667. doi: 10.5435/00124635-201011000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Jellema P, van Tulder MW, van Poppel MN, Nachemson AL, Bouter LM. Lumbar supports for prevention and treatment of low back pain: A systematic review within the framework of the cochrane back review group. Spine (Phila Pa 1976) 2001;26:377–386. doi: 10.1097/00007632-200102150-00014. [DOI] [PubMed] [Google Scholar]
- 6.van Poppel MN, de Looze MP, Koes BW, Smid T, Bouter LM. Mechanisms of action of lumbar supports: A systematic review. Spine (Phila Pa 1976) 2000;25:2103–2113. doi: 10.1097/00007632-200008150-00016. [DOI] [PubMed] [Google Scholar]
- 7.Perkins MS, Bloswick DS. The use of back belts to increase intraabdominal pressure as a means of preventing low back injuries: A survey of the literature. Int J Occup Environ Health. 1995;1:326–335. doi: 10.1179/oeh.1995.1.4.326. [DOI] [PubMed] [Google Scholar]
- 8.Chin KR, Auerbach JD, Adams SB, Sodl JF, Riew KD. Mastication causing segmental spinal motion in common cervical orthoses. Spine (Phila Pa 1976) 2006;31:430–434. doi: 10.1097/01.brs.0000200218.52384.8b. [DOI] [PubMed] [Google Scholar]
- 9.Peeters GG, Verhagen AP, de Bie RA, Oostendorp RA. The efficacy of conservative treatment in patients with whiplash injury: A systematic review of clinical trials. Spine (Phila Pa 1976) 2001;26:e64–e73. doi: 10.1097/00007632-200102150-00006. [DOI] [PubMed] [Google Scholar]
- 10.Borchgrevink GE, Kaasa A, McDonagh D, Stiles TC, Haraldseth O, Lereim I. Acute treatment of whiplash neck sprain injuries. A randomized trial of treatment during the first 14 days after a car accident. Spine (Phila Pa 1976) 1998;23:25–31. doi: 10.1097/00007632-199801010-00006. [DOI] [PubMed] [Google Scholar]
- 11.Giebel GD, Edelmann M, Huser R. Die Distorsion der Halswirbelsäule: fruhfunktionelle vs. ruhigstellende Behandlung [Sprain of the cervical spine: Early functional vs. Immobilization treatment] Zentralbl Chir. 1997;122:517–521. [PubMed] [Google Scholar]
- 12.McKinney LA. Early mobilisation and outcome in acute sprains of the neck. BMJ. 1989;299:1006–1008. doi: 10.1136/bmj.299.6706.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mealy K, Brennan H, Fenelon GC. Early mobilization of acute whiplash injuries. Br Med J (Clin Res Ed) 1986;292:656–657. doi: 10.1136/bmj.292.6521.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pennie BH, Agambar LJ. Whiplash injuries. A trial of early management. J Bone Joint Surg Br. 1990;72:277–279. doi: 10.1302/0301-620X.72B2.2312568. [DOI] [PubMed] [Google Scholar]
- 15.Persson LC, Carlsson CA, Carlsson JY. Long-lasting cervical radicular pain managed with surgery, physiotherapy, or a cervical collar. A prospective, randomized study. Spine (Phila Pa 1976) 1997;22:751–758. doi: 10.1097/00007632-199704010-00007. [DOI] [PubMed] [Google Scholar]
- 16.Saal JS, Saal, Yurth EF. Nonoperative management of herniated cervical intervertebral disc with radiculopathy. Spine (Phila Pa 1976) 1996;21:1877–1883. doi: 10.1097/00007632-199608150-00008. [DOI] [PubMed] [Google Scholar]
- 17.Kuijper B, Tans JT, Beelen A, Nollet F, de Visserc M. Cervical collar or physiotherapy versus wait and see policy for recent onset cervical radiculopathy: Randomised trial. BMJ. 2009;339 doi: 10.1136/bmj.b3883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Persson LC, Moritz U, Brandt L, Carlsson CA. Cervical radiculopathy: Pain, muscle weakness and sensory loss in patients with cervical radiculopathy treated with surgery, physiotherapy or cervical collar. A prospective, controlled study. Eur Spine J. 1997;6:256–266. doi: 10.1007/BF01322448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Duijvenbode IC, Jellema P, van Poppel MN, van Tulder MW. Lumbar supports for prevention and treatment of low back pain. Cochrane Database Syst Rev. 2008;(2) doi: 10.1002/14651858.CD001823.pub3. CD001823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bundesärztekammer (BÄK) Kassenärztliche Bundesvereinigung (KBV), Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF) Nationale VersorgungsLeitlinie Kreuzschmerz - Langfassung. Version 4, 2010. Last revised: August 2013. Available from: www.kreuzschmerz.versorgungsleitlinien.de. last accessed on 9 September 2013.
- 21.Sobottke R, Seifert H, Fatkenheuer G, Schmidt M, Gossmann A, Eysel P. Current diagnosis and treatment of spondylodiscitis. Dtsch Arztebl Int. 2008;105:181–187. doi: 10.3238/arztebl.2008.0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zarghooni K, Rollinghoff M, Sobottke R, Eysel P. Treatment of spondylodiscitis. Int Orthop. 2012;36:405–411. doi: 10.1007/s00264-011-1425-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bettini N, Girardo M, Dema E, Cervellati S. Evaluation of conservative treatment of non specific spondylodiscitis. Eur Spine J. 2009;18:143–150. doi: 10.1007/s00586-009-0979-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Di Martino A, Papapietro N, Lanotte A, Russo F, Vadala G, Denaro V. Spondylodiscitis: Standards of current treatment. Curr Med Res Opin. 2012;28:689–699. doi: 10.1185/03007995.2012.678939. [DOI] [PubMed] [Google Scholar]
- 25.Bible JE, Biswas D, Whang PG, Simpson AK, Rechtine GR, Grauer JN. Postoperative bracing after spine surgery for degenerative conditions: A questionnaire study. Spine J. 2009;9:309–316. doi: 10.1016/j.spinee.2008.06.453. [DOI] [PubMed] [Google Scholar]
- 26.Lee CS, Hwang CJ, Lee DH, Kim YT, Lee HS. Fusion rates of instrumented lumbar spinal arthrodesis according to surgical approach: A systematic review of randomized trials. Clin Orthop Surg. 2011;3:39–47. doi: 10.4055/cios.2011.3.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Connolly PJ, Grob D. Bracing of patients after fusion for degenerative problems of the lumbar spine-yes or no? Spine (Phila Pa 1976) 1998;23:1426–1428. doi: 10.1097/00007632-199806150-00024. [DOI] [PubMed] [Google Scholar]
- 28.Yee AJ, Yoo JU, Marsolais EB, et al. Use of a postoperative lumbar corset after lumbar spinal arthrodesis for degenerative conditions of the spine. A prospective randomized trial. J Bone Joint Surg Am. 2008;90:2062–2068. doi: 10.2106/JBJS.G.01093. [DOI] [PubMed] [Google Scholar]
- 29.Abbott A, Halvorsen M, Dedering A. Is there a need for cervical collar usage post anterior cervical decompression and fusion using interbody cages? A randomized controlled pilot trial. Physiother Theory Pract. 2013;29(4):290–300. doi: 10.3109/09593985.2012.731627. [DOI] [PubMed] [Google Scholar]
- 30.Campbell MJ, Carreon LY, Traynelis V, Anderson PA. Use of cervical collar after single-level anterior cervical fusion with plate: Is it necessary? Spine (Phila Pa 1976) 2009;34:43–48. doi: 10.1097/BRS.0b013e318191895d. [DOI] [PubMed] [Google Scholar]
- 31.Kawaguchi Y, Gejo R, Kanamori M, Kimura T. Quantitative analysis of the effect of lumbar orthosis on trunk muscle strength and muscle activity in normal subjects. J Orthop Sci. 2002;7:483–489. doi: 10.1007/s007760200084. [DOI] [PubMed] [Google Scholar]
- 32.Holmstrom E, Moritz U. Effects of lumbar belts on trunk muscle strength and endurance: A follow-up study of construction workers. J Spinal Disord. 1992;5:260–266. doi: 10.1097/00002517-199209000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Eisinger DB, Kumar R, Woodrow R. Effect of lumbar orthotics on trunk muscle strength. Am J Phys Med Rehabil. 1996;75:194–197. doi: 10.1097/00002060-199605000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Walsh NE, Schwartz RK. The influence of prophylactic orthoses on abdominal strength and low back injury in the workplace. Am J Phys Med Rehabil. 1990;69:245–250. doi: 10.1097/00002060-199010000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Fayolle-Minon I, Calmels P. Effect of wearing a lumbar orthosis on trunk muscles: Study of the muscle strength after 21 days of use on healthy subjects. Joint Bone Spine. 2008;75:58–63. doi: 10.1016/j.jbspin.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 36.Powers J, Daniels D, McGuire C, Hilbish C. The incidence of skin breakdown associated with use of cervical collars. J Trauma Nurs. 2006;13:198–200. doi: 10.1097/00043860-200610000-00016. [DOI] [PubMed] [Google Scholar]
- 37.Plaisier B, Gabram SG, Schwartz RJ, Jacobs LM. Prospective evaluation of craniofacial pressure in four different cervical orthoses. J Trauma. 1994;37:714–720. doi: 10.1097/00005373-199411000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Stambolis V, Brady S, Klos D, Wesling M, Fatianov T, Hildner C. The effects of cervical bracing upon swallowing in young, normal, healthy volunteers. Dysphagia. 2003;18:39–45. doi: 10.1007/s00455-002-0083-2. [DOI] [PubMed] [Google Scholar]


