Abstract
Objective
To examine the psychiatric treatment received by primary care patients with anxiety disorders and compare treatment from primary care physicians and psychiatrists.
Method
Primary care patients at 15 U.S. sites were screened for anxiety symptoms at the time of a medical visit. Those screening positive were interviewed to assess for anxiety disorders. Information on psychiatric treatment received and provider of pharmacological treatment was collected.
Results
Of 539 primary care participants with at least one anxiety disorder, almost half (47.3%) were untreated. Nearly 21% were receiving only medication for psychiatric problems, 7.2% received psychotherapy alone, and 24.5% received both medication and psychotherapy. Patients getting psychopharmacologic treatment received similar medications, often at similar dosages, regardless of whether their prescriber was a primary care physician or a psychiatrist. One exception was that patients were less likely to be taking benzodiazepines if their provider was a primary care physician. Those receiving medications from a primary care provider were also less likely to be in psychotherapy. Overall, patients with more functional impairment, more severe symptoms, and comorbid major depression were more likely to receive mental health treatment. Members of racial/ethnic minority groups were less likely to be treated. Frequently endorsed reasons by patients for not receiving pharmacological treatment were that the primary care physician did not recommend it and not believing in taking medication for emotional problems.
Conclusions
Nearly half of primary care patients with anxiety disorders were not treated. However, when treated, care received from primary care physicians and psychiatrists was relatively similar.
Introduction
More than half of patients with a psychiatric problem receive treatment for their symptoms from a primary care physician rather than a mental health specialist (1,2). General medical physicians also facilitate or impede access to mental health specialty services through referral decisions (3, 4). A survey of U.S. adults with depressive and anxiety disorders found that only 1.9% visited a mental health specialist without seeing a primary care physician (5).
Anxiety disorders are among the most common mental health problems presenting in a primary care setting. As much as a third of primary care patients have been found to have significant anxiety symptoms (6). Approximately 15% have a current anxiety disorder, and 24% a lifetime anxiety disorder, as assessed by diagnostic interview (7). Primary care patients with anxiety disorders typically have considerable disability and impairment in functioning (8, 9). They also have high utilization of general medical services, resulting in higher health care costs (10).
Only a few studies have investigated the nature of mental health treatments for primary care patients with anxiety disorders. An analysis of the National Ambulatory Medical Care Survey database from 1985 to 1998 found that, when anxiety was diagnosed, treatment was offered in over 95% of visits to psychiatrists but in only 60% of visits to a primary care physician (11). A World Health Organization-coordinated international study documented the prescribing patterns of primary care physicians in regard to the treatment of psychiatric disorders (12). Of primary care patients with anxiety disorders, 7.7% were found to be treated with antidepressant medications, 34.1% with anxiolytics and hypnotics, and 21.1% with miscellaneous other medications. Use of antidepressants (in 23% of patients with anxiety disorders) was noticeably higher in the U.S. compared to other countries. In the study most similar to our own, primary care patients with anxiety disorders self-reported the treatment they received. Just over half (58.7%) received any psychotropic medication, 35.8% received counseling by their primary care provider, and only 31.3% of patients reported treatment that met the authors' criterion for quality care (13). However, this study did not investigate differences in care received from primary care providers and psychiatrists. In the treatment of depression, when primary care physicians prescribe antidepressants, they use dosages lower than recommended by guidelines and lower than used by psychiatrists (14, 15).
The current study was designed to address the relative lack of information on the type of treatments prescribed to patients with anxiety disorders presenting to primary care settings. The specific goals were to provide descriptive information on the proportion of primary care patients with anxiety disorders who receive mental health treatment and to examine potential differences in treatment received from primary care physicians and psychiatrists. Predictors of receiving treatment for an anxiety disorder were explored in order to ascertain whether mental health treatments are more likely to be initiated for certain subgroups of patients.
Methods
Study Design
Subjects are participants in the Primary Care Anxiety Project (PCAP). PCAP is a longitudinal study of individuals with anxiety disorders in primary care settings (16). Patients with anxiety disorders are assessed at study baseline, 6 and 12 months post-baseline, and then yearly thereafter in follow-up interviews. This report examines baseline data only.
PCAP was conducted across 15 primary care practices in New Hampshire, Massachusetts, Rhode Island, and Vermont. Both internal medicine and family practice offices were involved, including four private practice offices, four university-affiliated clinics, and seven clinics at university teaching hospitals.
Participant Recruitment and Assessment
Participants in PCAP were recruited from primary care waiting rooms. Inclusion criteria were: a general medical appointment on the day of screening, 18 years of age, English proficiency, and meeting DSM-IV criteria for one or more of 7 intake anxiety disorder diagnoses. Exclusion criteria included active psychosis, the absence of a current address and phone number, and pregnancy.
A research assistant asked all eligible participants in the primary care waiting room if they were interested in participating in a study of different types of stress or nervousness. Interested patients were asked to complete a screening form designed to evaluate the key features of DSM-IV anxiety disorders. Patients who screened positive for anxiety symptoms were offered a full diagnostic interview. After complete description of the study, written consent was obtained from all participants. Institutional Review Boards at each of the sites approved the research protocol. A detailed description of recruitment has been published (17).
Measures
Anxiety screener
A 32-item self-report measure was used to assess the key features of each anxiety disorder. Items were derived from the central features of DSM-IV criteria. In order to avoid excluding potentially eligible participants, the screener was designed to be highly sensitive. A separate validation study conducted on this instrument (16), found that the screening form had a sensitivity of 1.0 and a specificity of .67. No individual in the validation sample screened negative but was found to have a SCID anxiety disorder diagnosis.
Clinical interview
All subjects were diagnosed using the SCID for DSM-IV (18). After the psychotic screen, the SCID anxiety disorders module was administered first. Participants who received an anxiety disorder diagnosis, proceeded to complete the mood, substance use, and eating disorders modules.
Psychosocial Functioning
At the completion of the SCID, the interviewer rated the Global Assessment of Functioning Scale (GAF) that is part of the DSM-IV system (19). This is a measure of functioning and symptom severity. Interviewers also rated the patient on Global Social Adjustment (GSA), as part of the LIFE-base interview (20). This is a 1-5 scale (1 = no impairment and very good functioning, 5 = marked or severe impairment) indicating overall level of current psychosocial functioning.
Non-Psychiatric Medical Problems were assessed using a Medical History Form designed for the study (16). The Medical History Form is an interviewer-administered questionnaire in which participants are asked whether or not they have ever had any of 18 different illnesses or medical problems. For the present study, a dichotomous (yes/no) variable was constructed indicating the presence of a major medical illness. This was coded “yes” for any participant reporting current asthma, cancer, diabetes, epilepsy, heart disease, kidney disease, liver disease, lung or respiratory illness, stroke, and/or thyroid disease.
Treatment Received
Information regarding participant's use of psychotropic medications was captured on the psychotropic treatment section of the LIFE (20). Psychosocial treatment received was measured on the Types of Treatment Form, an interviewer-administered form designed for the present study, and on the Psychosocial Treatment Inventory-Revised (21).
A sub-sample of participants not receiving treatment were interviewed using the Treatment not Received Form, designed for the present study. This is an interviewer-administered measure, examining reasons for not receiving and/or complying with recommended mental health treatment.
Statistical Methods
Descriptive statistics (means, percents) were used to characterize the type of treatment received for the sample as a whole. Comparisons between the type, and dosage, of medications prescribed by primary care physician and psychiatrists were made with chi-square statistics and t-tests, respectively.
Potential predictors of receiving any mental health treatment, and of receiving pharmacotherapy from a psychiatrist versus a primary care physician were examined. The initial pool of potential predictors included age, gender, race/ethnicity, education, insurance type, income, marital status, symptom severity and functioning as measured by the GAF and GSA scales, presence of major depressive disorder (MDD), presence of alcohol/substance use disorder, presence of a major non-psychiatric medical illness, number of anxiety disorders, and anxiety disorder illness age of onset. We reduced this potential pool by examining the univariate relationship between each predictor and each outcome variable. All individual variables related to the outcome variable at p <.05 were entered into a stepwise logistic regression. The final logistic regression models were examined including all remaining variables that entered at a 0.05 level of significance.
Results
Sample Characteristics
A detailed description of recruitment and sample selection, including rates of refusal, has been published (17). 539 primary care patients met criteria for one or more of the following index anxiety disorders and were enrolled in PCAP: posttraumatic stress disorder (n=199, 37%), social phobia (n=182, 34%), panic disorder with agoraphobia (n=150, 28%), generalized anxiety disorder (GAD; n=135, 25%), panic disorder without agoraphobia (n=85, 16%); agoraphobia without history of panic disorder (n=23, 4%), mixed anxiety-depressive disorder (n=10, 2%), or GAD features occurring exclusively within the course of a mood disorder (n=29, 5%). 50.5% of patients had more than one of these anxiety disorders. Comorbid non-anxiety disorders included MDD (41%), alcohol/substance use disorders (10%), and eating disorders (11%).
The average age of participants was 39 years old. The majority were female (76%) and Caucasian (83%). Of the 91 participants who were members of a minority group, 41 were African-American, 20 Hispanic, 9 Native American, 7 Asian, and 14 Other. Half of all participants were married, the majority had at least a high school education (67%), and 40% were employed full-time.
Overall Treatment of Anxiety Disorders in Primary Care
Of the total 539 primary care patients with an anxiety disorder, 52.7% (N=284) were receiving treatment for psychiatric problems. One hundred-thirty-two patients (24.5%) were receiving both psychopharmacological treatment and psychotherapy, 113 (21.0%) were receiving only medication, and just 39 (7.2%) were receiving only psychotherapy.
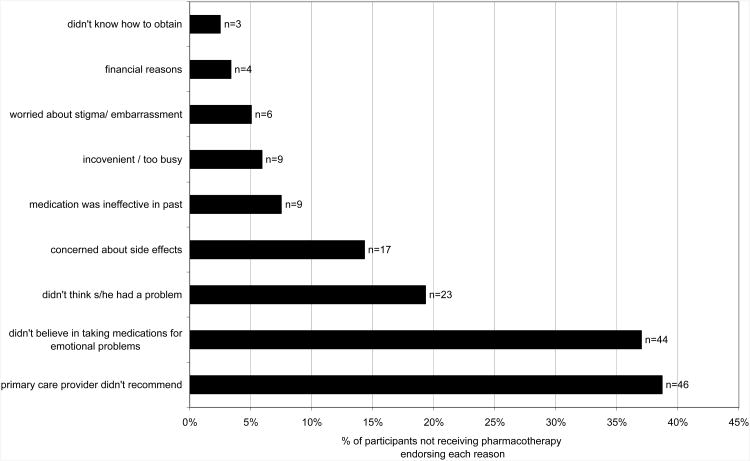
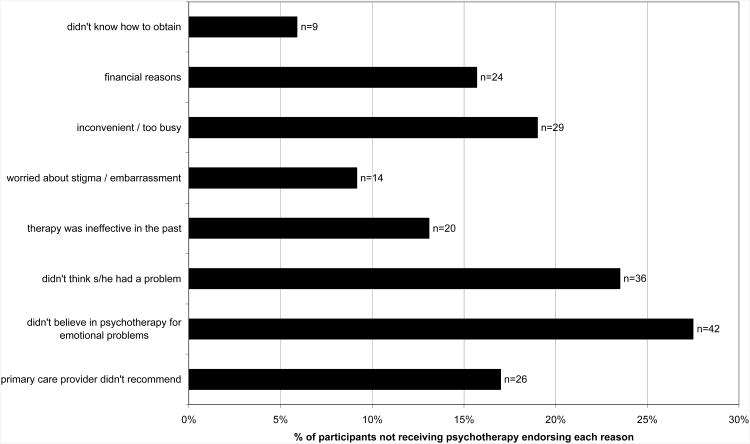
Reasons given by participants for not receiving pharmacotherapy are shown in figure 1 and for not receiving psychotherapy are in figure 2. Among the top two most frequently endorsed reasons for not getting both types of treatment was that the patient didn't believe in treatment for emotional problems. The most commonly endorsed reason for not receiving pharmacotherapy was that the primary care provider didn't recommend this treatment (38.7%). This was also endorsed by 17% of those not getting psychotherapy. Additionally, not realizing that he or she had a treatable, emotional problem was the third most common reason for not receiving pharmacotherapy (endorsed by 19.3%) and the second most common reason for not getting psychotherapy (23.5%). Barriers related to treatment access, such as cost, convenience, and knowing how to obtain care were commonly endorsed as reasons for not receiving psychotherapy, but rarely given as barriers to pharmacotherapy.
Figure 1. Reasons given for not receiving pharmacotherapy (N=119).
Figure 2. Reasons given for not receiving psychotherapy (N=153).
To understand the clinical and demographic characteristics associated with a greater likelihood of receiving treatment for psychiatric problems, stepwise logistic regression was conducted. After prescreening variables (as described above), the following variables were eligible for examination of receiving/not receiving any treatment: income, ethnicity/race, receiving medicare or public assistance, GAF, number of current anxiety disorders, and currently in episode of MDD. Results of a forward selection step-wise logistic regression analysis revealed that four variables entered the predictive model at p < 0.05 (Table 1). Primary care patients with anxiety disorders who received mental health treatment were significantly more likely to have poorer functioning and more severe symptoms, as measured by the GAF, have a concurrent MDD diagnosis, be receiving medicare or public assistance, and to not be a member of a minority group.
Table 1. Predictors of Receiving Any Mental Health Treatment Among Primary Care Patients with Anxiety Disorders.
| Odds Ratio (90% CI) | Wald χ2 | DF | P-value | |
|---|---|---|---|---|
| Receiving Medicaid or Public Assistance | 1.7 (1.2 – 2.5) | 5.7 | 1 | 0.017 |
| Nonwhite | 0.29 (0.18 – 0.46) | 19.5 | 1 | < 0.0001 |
| Current Major Depressive Disorder | 2.0 (1.4 – 2.9) | 10.6 | 1 | 0.01 |
| GAF | 0.94 (0.92 – 0.96) | 19.0 | 1 | < 0.0001 |
Results from final model including all variables that entered at 0.05 or better are given.
We ran posthoc analyses to better understand the finding that patients with medicare were more likely to receive treatment. We found that participants with medicare were more likely to be receiving treatment (67%), than either participants with no insurance (42% in treatment) (χ2=9.73, df=1, p<.01) or those with private insurance (49% in treatment) (χ2=12.58, df=1, p<.001). There was no difference in treatment rates between participants with no insurance and those with private insurance (χ2=0.93, df=1, p=0.33).
Comparisons of Treatment Received from Psychiatrists and Primary Care Physicians
Psychopharmacological Treatment Received
Of the 244 participants who were receiving medication treatment, 100 (41.0%) obtained their medication from their primary care physician, 98 (40.2%) from their psychiatrist, and 7 (2.9%) from other sources (e.g., from their gynecologist or were taking a family member's prescription). These data were missing or the source was unknown for 39 (16.0%) individuals. Among those who received their medication from primary care providers or psychiatrists, 60.4% (119/197) of participants received selective serotonin/norepinephrine reuptake inhibitors (SSRI/SNRIs), 34.5% (68/197) received benzodiazepines, 11.7% (23/197) received tricyclic antidepressants, 14.7% (29/197) received trazadone, and 3% (6/197) received buspirone.
Patients of primary care physicians, compared to psychiatrists, were significantly less likely to receive benzodiazepines (24.0% [24/100] vs. 45.4% [44/97]; χ2 = 9.9, DF = 1, p = 0.0016). There were no significant differences in the rates of receiving SSRI/SNRIs (66.0%% [66/100] vs. 54.6% [53/97], respectively), tricyclic antidepressants, (10.0% [10/100] vs. 13.4% [13/97]), or trazadone (15.0% [15/100] vs. 14.4% [14/97]). Few patients reported taking buspirone, prescribed from either primary care physicians (n=1 patient) or psychiatrists (n=5 patients).
An examination of mean doses of SSRI/SRNI medications reported by primary care patients revealed there were no significant differences between the two types of providers. However, when their prescriber was a psychiatrist, as compared to a primary care physician, patients reported taking somewhat higher doses of sertraline (110 ± 74 [n=15] vs. 70 ± 40 [n=25]mg/day, respectively; t = 1.9, DF = 19.1 [separate variance test], p = 0.068) and fluoxetine (35 ± 26 [n=17] vs. 22 ± 9 [n=18] mg/day; t = 1.99, df = 19.9 [separate variance test], p =0.06). Dosages of paroxetine were similar (19 ± 14 mg/day, n=14 for psychiatrists; 23 ± 20 mg/day, n = 23 for primary care physicians). Only one patient received venlafaxine from his/her primary care provider (dosage = 75 mg/day compared to an average of 191 ± 142 mg/day for 8 patients treated by psychiatrists). No patient received citalopram from a primary care physician (enrollment overlapped its introduction in the Unites States).
Using the same initial pool of variables given above, the following were eligible for the regression analysis: marital status, race/ethnicity, GSA, GAF, and medicare/public assistance. Step-wise logistic regression (N=194) predicting whether a patient received medication treatment from their primary care physician or a psychiatrist revealed only one significant predictor: patient's global social adjustment (GSA) (Wald χ2= 12.3., DF = 1, p < 0.001; odds ratio = 1.8). Primary care patients with anxiety disorders who received medication from a psychiatrist had poorer psychosocial functioning as measured by GSA.
Psychotherapy Received
Of the 198 patients receiving psychotropic medications from either a psychiatrist or a primary care physician, those individuals whose pharmacotherapy was prescribed by a psychiatrist were significantly more likely to receive conjunctive psychotherapy (χ2 = 36.01, DF = 1, p < .0001). Thirty-three (33%) of patients getting medications from a primary care provider and 74 (76%) of patients whose medications were prescribed by a psychiatrist reported also receiving psychotherapy.
Discussion
Several findings emerged from the current study that are relevant to the quality of care provided to patients with anxiety disorders who present to primary care settings. First, only about half of primary care patients with anxiety disorders were currently receiving any mental health treatment. Second, patients taking psychotropic medications were equally likely to be receiving the prescription from their primary care provider as from a psychiatrist. Third, SSRIs/SNRIs were the most commonly prescribed psychotropic medication, by both primary care providers and psychiatrists. Fourth, patients were less likely to be taking benzodiazepines prescribed by primary care physicians than by psychiatrists. Fifth, individuals receiving psychotropic medication from a primary care physician were less likely than those getting pharmacotherapy from a psychiatrist to also be receiving psychotherapy. Sixth, members of ethnic minority groups were less likely to be receiving mental health treatment. Seventh, individuals with more impairment and more severe symptoms, as evidenced by lower GAF scores, or with a concurrent major depressive disorder, were more likely to receive mental health treatment. Eighth, primary care patients who were not receiving pharmacotherapy for their anxiety disorders stated that two of the main reasons for not being treated included that their doctor never recommended treatment (38.7%) and that they did not believe in medication for emotional problems (37%). The most frequently endorsed reasons for not receiving psychotherapy were that 27.5% did not believe in psychotherapy and 23.8% of patients didn't know they had a problem.
The fact that only about half of primary care patients with an anxiety disorder were receiving mental health treatment is consistent with the National Ambulatory Medical Care Survey that reported treatment was offered at 60% of the primary care office visits for patients with anxiety (11). These data suggest that there remains substantial room for further improvement in reducing the burden of anxiety disorders on society.
Although only about half of patients with anxiety disorders received any treatment, when pharmacological treatment was implemented, rates of receiving antidepressants (SSRI/SNRIs) from primary care physicians were as high as those from psychiatrists, suggesting that many primary care physicians are aware of new developments in pharmacotherapy for anxiety disorders. Similar to our data, a multinational study of prescribing patterns in primary care found that, in the United States, 23% of patients with an anxiety problem received a prescription for an antidepressant (12). Patients were less likely to receive benzodiazepines from primary care physicians, compared to psychiatrists, perhaps due to primary care physician concern for the variety of adverse events and abuse liability that may be associated with these agents (22; 23). We also found that the only significant predictor of receiving medication from a psychiatrist versus a primary care physician was severity of functional impairment. Therefore, it may be that psychiatrists prescribe more benzodiazepines than do primary care physicians, because psychiatrists are treating a more severely impaired population. In terms of dosing, there was no significant difference between dosages reported by patients prescribed their medication by primary care physicians and psychiatrists. However, the difference in dosages for sertraline and fluoxetine fell just short of statistical significance. Sample sizes were too small to detect anything but large differences, so this issue needs further investigation.
Our study did not directly evaluate the physician's viewpoint on why treatment was not implemented for many patients with anxiety disorders. Analyses of demographic and clinical predictors suggest the possibility that primary care physicians have a high threshold for recognition and/or treatment of anxiety disorders. This may also be the reason why patients on public assistance were more likely to be receiving treatment than their counterparts with private insurance. Patients with public insurance may have had worse functioning and appeared more severely ill. When patients had more severe symptoms, worse functioning, or comorbid depression, primary care physicians were perhaps more likely to recognize that a psychiatric disorder was present and consequently implement treatment, or refer patients to a psychiatrist for treatment. Whether the primary care physicians are not aware of the anxiety disorder when functioning is higher, or whether they are hesitant to treat higher functioning patients with anxiety disorders, is not clear. Our data do indicate that many patients report that they were unaware of having a problem or that their primary care doctor did not recommend treatment, suggesting at the least a lack of communication between the primary care physician and the patient. Further research is needed to understand how often primary care physicians recognize anxiety disorders but decide not to communicate their diagnoses with patients and not to treat such disorders, or whether primary care physicians are continuing to not recognize such disorders when impairment is less severe, as has been documented in the past (24; 6).
Of particular concern is the finding that members of minority groups were less likely to receive mental health treatment. This is consistent with results of a recent primary care study, which found that ethnic minorities were less likely to receive appropriate antianxiety medications (13). Another previous study failed to find any differences in the prescribing of antidepressants to non-Latino white patients and Latino patients in primary care (25). Further studies are needed to determine if the ethnic disparity found in our study is unique to anxiety disorders, or unique to the sites, or geographic area, of the current study. Additionally, it is important to note that our study measured treatment received, as reported by the patient, rather than treatment prescribed, as reported by the physician. Therefore, an important agenda for future research is to sort out whether barriers to minorities receiving treatment for anxiety disorders are related more to physician behavior or cultural attitudes towards medication or therapy among patients.
For some primary care physicians, failure to adequately treat anxiety disorders may be related to a belief that the anxiety is secondary to a non-psychiatric medical disorder. However, in the present study we found that the presence of a major non-psychiatric medical illness was not related to the likelihood of receiving treatment.
Our data also suggests that some of the barriers to effective treatment lie within the patient, rather than the primary care doctor. One of the most common reasons for not receiving pharmacotherapy was not believing in medication for emotional problems, and the most common reason for not receiving psychotherapy was not believing in psychotherapy. These findings indicate that efforts to improve treatment of anxiety disorders in primary care must involve patient education, not solely interventions directed at providers. In the treatment of major depressive disorder, an intervention that focused on counseling primary care patients about medication treatment was found to improve adherence and enhance outcomes among those receiving higher dosages, relative to treatment as usual (31). The value of patient education about anxiety disorders and their treatment needs also to be investigated.
Limitations of the current study include the fact that all of the primary care sites were in one geographic area of the United States. Research involving a broader range of sites across the U.S., including sites with larger populations of minorities served, would be important to examine the generalizability of our findings. Further, our investigation is not an epidemiological study in that we did not systematically interview all members of the available population, and in that by asking patients if they were interested in participating in a study about “stress or nervousness” we may have biased the sample toward those with anxiety disorders. Thus, this data is not meant as a report of anxiety disorder prevalence rates in primary care. Additionally, this study did not examine the frequency of visits to psychiatrists and primary care physicians to monitor anxiety and treatment. A potential unreported difference in care between these provider types may be the follow-up received, especially after prescribing a new medication. The current data is also limited in that it provides only a single “snap shot” about the treatment of anxiety disorders after such patients have presented to a primary care setting. Some primary care physicians might take a “watchful waiting” approach with anxiety disorders in order to see if symptoms resolve over time without treatment. If anxiety symptoms persist over time, primary care physicians might be compelled to implement treatment, or refer for specialty care. Longitudinal follow-up data would provide such information on whether the rate of treatment increases if symptoms are persistent. The PCAP study is currently tracking the patient cohort described herein, with assessments at 6 and 12 months post-intake and then yearly thereafter. Thus, we will eventually be able to address the issue of how treatments, or lack of treatment, changes over time for patients with anxiety disorders.
Acknowledgments
Funding for this study was provided by an Unrestricted Grant from Pfizer Pharmaceuticals, Inc. The first author's time and effort was supported in part, through a Mentored Patient Oriented Research Career Development Award from the National Institute of Mental Health, K23 MH069595.
Footnotes
Portions of this data were presented at the annual meeting of the North American Primary Care Research Group, Nova Scotia, Canada, 2001, the annual meeting of the American Psychiatric Association, San Francisco, CA, 2003, the Primary Care Anxiety Conference of the Anxiety Disorders Association of America, Warrenton, VA, 2004, and the Annual Meeting of the Anxiety Disorders Association of America, Miami, FL, 2006.
References
- 1.Price D, Beck A, Nimmer C, Bensen S. The treatment of anxiety disorders in a primary care setting. Psychiatr Q. 2000;7:31–45. doi: 10.1023/a:1004662600803. [DOI] [PubMed] [Google Scholar]
- 2.Shear MK, Schulberg HC. Anxiety disorders in primary care. Bull Menninger Clin. 1995;59(suppl A):A73–A85. [PubMed] [Google Scholar]
- 3.Beardsley RS, Gardocki GJ, Larson DB, Hidalgo J. Prescribing of psychotropic medication by primary care physicians and psychiatrists. Arch Gen Psychiatry. 1988;45:1117–1119. doi: 10.1001/archpsyc.1988.01800360065009. [DOI] [PubMed] [Google Scholar]
- 4.Weiller E, Bisserbe JC, Maier W, Lecrubier Y. Prevalence and recognition of anxiety syndromes in five European primary care settings. Br J Psychiatry. 1998;173(suppl. 34):18–23. [PubMed] [Google Scholar]
- 5.Young AS, Klap R, Sherbourne CD, Wells KB. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001;58:55–61. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]
- 6.Fifer SK, Mathias SD, Patrick DL, Mazonson PD, Lubeck DP, Buesching DP. Untreated anxiety among adult primary care patients in a Health Maintenance Organization. Arch Gen Psychiatry. 1994;51:740–750. doi: 10.1001/archpsyc.1994.03950090072010. [DOI] [PubMed] [Google Scholar]
- 7.Nisenson LG, Pepper CM, Schwenk TL, Coyne JC. The nature and prevalence of anxiety disorders in primary care. Gen Hosp Psychiatry. 1998;20:21–28. doi: 10.1016/s0163-8343(97)00096-0. [DOI] [PubMed] [Google Scholar]
- 8.Roy-Byrne PP, Stein MB, Russo J, Mercier E, Thomas R, McQuaid J, Katon WJ, Craske MG, Bystritsky A, Sherbourne CD. Panic disorder in the primary care setting: comorbidity, disability, service utilization, and treatment. J Clin Psychiatry. 1999;60:492–499. doi: 10.4088/jcp.v60n0713. [DOI] [PubMed] [Google Scholar]
- 9.Sherbourne CD, Wells KB, Meredith LS, Jackson CA, Camp P. Comorbid anxiety disorder and the functioning and well-being of chronically ill patients of general medical providers. Arch Gen Psychiatry. 1996;53:889–895. doi: 10.1001/archpsyc.1996.01830100035005. [DOI] [PubMed] [Google Scholar]
- 10.Simon G, Ormel J, VonKorff M, Barlow W. Health care costs associated with depressive and anxiety disorders in primary care. Am J Psychiatry. 1995;152:353–357. doi: 10.1176/ajp.152.3.352. [DOI] [PubMed] [Google Scholar]
- 11.Harman JS, Rollman BL, Hanusa BH, Lenze EJ, Shear MK. Physician office visits of adults for anxiety disorders in the United States, 1985-1998. J Gen Intern Med. 2002;17:165–172. doi: 10.1046/j.1525-1497.2002.10409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Linden M, Lecrubier Y, Bellantuono C, Benkert O, Kisely S, Simon G. The prescribing of psychotropic drugs by primary care physicians: an international collaborative study. J Clin Psychopharmacol. 1999;19:132–140. doi: 10.1097/00004714-199904000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Stein MB, Sherbourne CD, Craske MG, Means-Christensen A, Bystritsky A, Katon W, Sullivan G, Roy-Byrne PP. Quality of care for primary care patients with anxiety disorders. Am J Psychiatry. 2004;161:2230–2237. doi: 10.1176/appi.ajp.161.12.2230. [DOI] [PubMed] [Google Scholar]
- 14.McManus P, Mant A, Mitchell P, Britt H, Dudley J. Use of antidepressants by general practitioners and psychiatrists in Australia. Aust N Z J Psychiatry. 2003;37:184–189. doi: 10.1046/j.1440-1614.2003.01132.x. [DOI] [PubMed] [Google Scholar]
- 15.Donoghue JM, Tylee A. The treatment of depression: prescribing patterns of antidepressants in primary care in the UK. Br J Psychiatry. 1996;168:164–168. doi: 10.1192/bjp.168.2.164. [DOI] [PubMed] [Google Scholar]
- 16.Weisberg RB, Bruce SE, Machan JT, Kessler RC, Culpepper L, Keller MB. Nonpsychiatric illness among primary care patients with trauma histories and post-traumatic stress disorder. Psychiatr Serv. 2002;53:848–854. doi: 10.1176/appi.ps.53.7.848. [DOI] [PubMed] [Google Scholar]
- 17.Weisberg RB, Maki KM, Culpepper L, Keller MB. Is anyone really M.A.D? The occurrence and course of mixed anxiety-depressive disorder in a sample of primary care patients. J Nerv Ment Dis. 2005;193:223–230. doi: 10.1097/01.nmd.0000158379.14063.cd. [DOI] [PubMed] [Google Scholar]
- 18.First MB, Spitzer RL, Gibbon M, Williams JBW. Biometrics Research Department. New York State Psychiatric Institute; 1996. Structured clinical interview for the DSM-IV Axis I Disorders. [Google Scholar]
- 19.Diagnostic and Statistical Manual of Mental Disorders. 4th. Washington, DC: 1994. American Psychiatric Association. [Google Scholar]
- 20.Keller MB, Warshaw MG, Dyck I, Dolan RT, Shea MY, Riley K, Shapiro R. LIFE-IV: The Longitudinal Interval Follow-up Evaluation for DSM-IV. Providence, RI: Department of Psychiatry and Human Behavior, Brown University; 1997. [Google Scholar]
- 21.Steketee G, Perry JC, Goisman RM, Warshaw MG, Massion AO, Peterson LG, Langford L, Weinshenker N, Farreras IG, Keller MB. The Psychosocial Treatments Interview for Anxiety Disorders: a method for assessing psychotherapeutic procedures in anxiety disorders. J Psychother Pract Res. 1997;6:194–210. [PMC free article] [PubMed] [Google Scholar]
- 22.Rickels K, Schweizer E, Lucki I. Benzodiazepine side effects. In: Hales RE, Frances AJ, editors. Amer Psychiatric Association Annual Review vol 6. Washington: American Psychiatric Press, Inc; 1987. pp. 781–801. [Google Scholar]
- 23.Woods JH, Katz JL, Winger G. Benzodiazepines: use, abuse, and consequences. Pharmacol Rev. 1992;44(2):151–347. [PubMed] [Google Scholar]
- 24.Borus JF, Howes MJ, Devins NP, Rosenberg R, Livingston WW. Primary health care providers' recognition and diagnosis of mental disorders in their patients. Gen Hosp Psychiatry. 1988;10:317–321. doi: 10.1016/0163-8343(88)90002-3. [DOI] [PubMed] [Google Scholar]
- 25.Sleath BL, Rubin RH, Huston SA. Antidepressant prescribing to Hispanic and non-Hispanic white patients in primary care. Ann Pharmacother. 2001;35:419–423. doi: 10.1345/aph.10245. [DOI] [PubMed] [Google Scholar]
- 26.Van der Feltz-Cornelis CM, Lyons JS, Huyse FJ, Campos R, Fink P, Slaets JP. Health services research on mental health in primary care. Int J Psychiatry Med. 1997;27:1–21. doi: 10.2190/YLPG-RV5E-MCPW-FKTM. [DOI] [PubMed] [Google Scholar]
- 27.Culpepper L. Use of algorithms to treat anxiety in primary care. J Clin Psychiatry. 2003;64(suppl. 2):30–33. [PubMed] [Google Scholar]
- 28.Sherbourne CD, Wells KB, Duan N, Miranda J, Unutzer J, Jaycox L, Schoenbaum M, Meredith LS, Rubenstein LV. Long-term effectiveness of disseminating quality improvement for depression in primary care. Arch Gen Psychiatry. 2001;58:696–703. doi: 10.1001/archpsyc.58.7.696. [DOI] [PubMed] [Google Scholar]
- 29.Andersen SM, Harthorn BH. Changing the psychiatric knowledge of primary care physicians. The effects of a brief intervention on clinical diagnosis and treatment. Gen Hosp Psychiatry. 1990;12:177–190. doi: 10.1016/0163-8343(90)90077-p. [DOI] [PubMed] [Google Scholar]
- 30.Katon W, Von Korff M, Lin E, Simon G, Walker E, Unutzer J, Bush T, Russo J, Ludman E. Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiatry. 1999;56:1109–15. doi: 10.1001/archpsyc.56.12.1109. [DOI] [PubMed] [Google Scholar]
- 31.Peveler R, George C, Kinmonth AL. Effect of antidepressant drug counselling and information leaflets on adherence to drug treatment in primary care: randomised controlled trial. BMJ. 319:1999. 612–615. doi: 10.1136/bmj.319.7210.612. [DOI] [PMC free article] [PubMed] [Google Scholar]